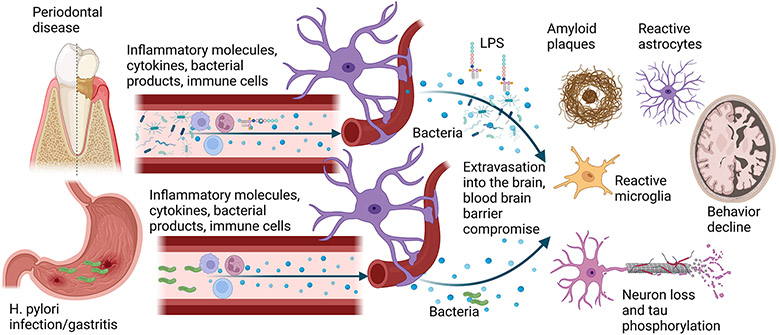
Fig. 2. Possible mechanisms of brain and stomach communication to the brain to potentiate AD pathophysiology.
Periodontitis, characterized by chronic gingival inflammation and bone and tooth loss, increases the risk for AD and dementia. Periodontitis is also positively correlated with increased amyloid plaque load, gliosis, and neuron loss. Increased immune cell activation and circulating cytokines associated with periodontitis may infiltrate through the blood-brain barrier to directly influence disease pathophysiology. Similarly, periodontal pathogens and their components, such as LPS, have been reported to be elevated in AD brains. Rodent studies of oral pathogen infection support the human disease findings by stimulating increased brain cytokines and LPS, memory dysfunction, neuron loss, elevated Aβ, and increased phospho-tau levels. In addition to the inflammatory contributions of changing oral health to the brain in AD, several studies demonstrate that the peripheral inflammatory changes associated with gastric infection and gastritis also induce AD-like changes in rodents, including elevated brain cytokines and altered behavior. This notion is supported by human studies demonstrating an increased association of H. pylori infection with AD patients compared to controls and improved behavior with eradication therapy.