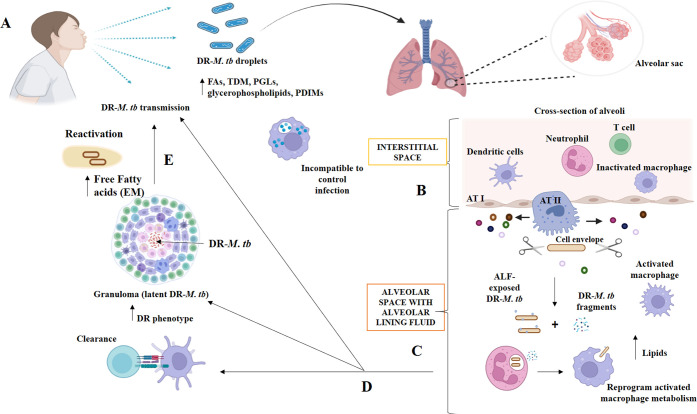
Figure 3.
Interactions between drug-resistant Mycobacterium tuberculosis and the host at various stages of infection in the pulmonary microenvironment. Copyright [2021] [Allué-Guardia, García and Torrelles).11 (A) Inhaling drug-resistant Mycobacterium tuberculosis-containing droplets from a TB patient can cause infection. Drug-resistant Mycobacterium tuberculosis bacilli have altered cell envelope lipids. Drug-resistant Mycobacterium tuberculosis will reach the alveoli after bypassing upper respiratory tract barriers. The alveolar space has resident phagocytes called alveolar macrophages (AMs), while the interstitial space around the alveoli has IMs, DCs, neutrophils (N), and T cells. (B) Hydrolases (represented as scissors) in the alveolar lining fluid (ALF) can cleave and modify the Mycobacterium tuberculosis cell envelope, releasing cell envelope fragments into the alveolar space. This interaction occurs when drug-resistant Mycobacterium tuberculosis bacteria enter the alveolar space. (C) ALF-modified Drug-resistant Mycobacterium TB bacilli then engage with AMs, ATs, and other host’s innate immune cells (e.g., neutrophils, DCs). Drug-resistant Mycobacterium TB pieces are immunogenic and may draw neutrophils to the infection site, which may help resident resting AMs eliminate the infection. (D) These initial interactions will result in ALF-exposed drug-resistant Mycobacterium tuberculosis clearance, a successful infection driving primary active TB disease, or a latent infection defined by persisters in granulomas. This niche protects against anti-TB drugs, increasing the phenotype. Surrounding mesenchymal stem cells (MSCs) can decrease immune responses and offer a protective intracellular environment for M. tuberculosis B persistence. (E) Failure of granulomas to retain drug-resistant Mycobacterium tuberculosis can lead to reactivation and progression to active TB disease, with the development of drug-resistant Mycobacterium tuberculosis occurring extracellularly and causing lung tissue degradation and cavity formation. In this setting, an extracellular matrix (EM) composed of free fatty acids may be secreted by drug-resistant Mycobacterium tuberculosis, providing additional protection from TB medications.