Abstract
Background:
Optic nerve sheath fenestration (ONSF) longitudinal outcomes remain unclear and are vital in the assessment of vision failure in patients with raised intracranial pressure (ICP). Furthermore, limited observational data exists regarding its use in other causes of raised ICP.
Objective:
To determine the efficacy and safety of ONSF for idiopathic intracranial hypertension (IIH), cerebral venous sinus thrombosis (CVST), and other indications.
Method:
Multicentre study from a tertiary hospital and specialty eye referral hospital in Melbourne, Australia, from July 2000 to December 2020. A total of 116 eyes from 70 patients undergoing ONSF were retrospectively reviewed with patient demographics, surgery indications, visual acuity (VA), visual fields, fundus photos of optic discs, retinal nerve fibre layer (RNFL) thickness, average thickness of optic discs on optical coherence tomography (OCT), and complications recorded. Parametric tests were used to compare the treatment groups pre- and post-operatively.
Results:
A total of 116 eyes from 70 patients underwent ONSF, which involved 92 eyes with IIH, 9 eyes with CVST, and 15 eyes with other aetiologies (‘Other’). Post ONSF, there was a best corrected visual acuity (BCVA) improvement or stabilisation in 84% of patients in all groups, with 50% achieving a BCVA of 6/6 or better at the final follow-up. RNFL, visual fields, and fundus grades all trended towards improvement, with most improvement noted by day 360. Common complications included transient diplopia (n = 29, 25%) and worsening of visual function requiring further cerebrospinal fluid (CSF) diversion procedures (n = 20, 17%). Complications were most significant in the ‘Other’ group with 1/3 of eyes requiring further CSF diversion procedures.
Conclusion:
Our data demonstrates effectiveness in the use of ONSF in papilloedema with visual failure due to IIH or CVST and when other CSF diversion procedures or medical therapies have failed.
Keywords: cerebral venous sinus thrombosis, idiopathic intracranial hypertension, optic nerve sheath fenestration
Introduction
Optic nerve sheath fenestration (ONSF) was first described in 1872, to relieve the effects of papilloedema through surgical decompression. Raised intracranial pressure (ICP) is thought to be mechanically transmitted through the optic nerve sheath, resulting in optic nerve fibre damage via intraneuronal ischaemia 1 This can ultimately lead to irreversible nerve fibre damage and subsequent vision loss.2–4 Current surgical techniques include direct visualisation of the optic nerve to create a window in the bulbous part of the meningeal covering of the retrolaminar optic nerve. Its use is indicated in any cause of raised ICP where there is a threat to visual function.
Idiopathic intracranial hypertension (IIH) is a syndrome of raised ICP in the absence of an identifiable aetiology. 5 Current treatment options aim to minimise symptoms and preserve visual function. Medical management with acetazolamide, weight loss, and close observation, is the most common therapeutic intervention. Surgical options are indicated when there is a threat to visual acuity (VA) in the setting of intolerance/refractory to medical management. Insertion of a ventriculoperitoneal shunt is the most common surgical intervention, likely due to local expertise.6,7 ONSF is shown to reduce papilloedema, maintain or improve visual function, reduce headaches, and is one of few surgical procedures to be considered in the setting of acute visual deterioration in the setting of IIH.5,8–10
The treatment of secondary causes of raised ICP focuses on the underlying cause. The incidence of persistent and rapidly progressive visual dysfunction in these settings is not known, with limited efficacy and safety data available on using ONSF in this setting. 11 Recent observational data demonstrated efficacy in the use of ONSF in cerebral venous sinus thrombosis (CVST) with stability/improvement achieved in 80% of eyes. 12 Case literature reports of ONSF as an intervention in multiple secondary processes associated with raised ICP includes central nervous system masses, optic nerve sheath meningoceles, post-operative subarachnoid haemorrhage of the optic nerve, acute retinal necrosis syndrome, non-arteritic ischaemic optic neuropathy, and central retinal vein occlusion.13–15
In this retrospective analysis, we aimed to report the longitudinal outcomes of ONSF for patients with IIH, CVST, and other aetiologies with regard to visual function.
Method
Data extraction
A retrospective analysis was performed using patient notes undergoing ONSF at the Royal Melbourne Hospital and Royal Victorian Eye and Ear Hospital, Melbourne, Australia, between July 2000 and December 2020.
Only cases that met the Modified Dandy criteria were included in the IIH group. 5 All cases of IIH had either failed maximal medical therapy or had rapid progressive visual loss requiring ONSF. CVST diagnosis was confirmed with computed tomography brain venography or magnetic resonance venography showing evidence of thrombosis in the cerebral venous sinuses. In the setting of compression of the dural veins secondary to malignancy with subsequent thrombosis formation, this was attributed to the ‘Other’ diagnoses. ‘Other’ diagnoses that underwent ONSF were diagnosed on history, physical exam, CT or MRI imaging, histology of optic nerve sheath, relevant blood tests, cerebrospinal fluid (CSF) analysis, and opening pressures when appropriate. All had evidence of visual impairment in either VA, visual fields, or subjectively, and had clear evidence of papilloedema.
We identified patients from medical records via surgical item numbers and reviewed all relevant case notes. Data capture included: indication for surgery, body mass index, co-morbidities, medication history, treatment pre- and post-operation, complications, best-corrected visual acuity (BCVA), mean deviation (MD) on automated visual fields, Frisen fundus papilloedema grading, and optical coherence tomography (OCT) measurement of retinal nerve fibre layer (RNFL).
Visual fields were assessed with standard automated perimetry using an Allergan Humphrey Visual Field analyser using the 30-2 program. OCT imaging of the RNFL using a Zeiss OCT stratus prior to November 2011, and Heidelberg Spectral-Domain OCT thereafter, was collected.
Surgical procedure
A medial conjunctival peritomy approach transconjunctival orbitotomy was performed in all cases, sometimes with lateral canthotomy. The vertical recti were slung on a large silk suture, and the medial rectus muscle was disinserted on an absorbable suture. Using malleable retractors, the retrobulbar optic nerve was visualised directly, typically with the use of the operating microscope. The dural sheath was then exposed and incision of the dura performed with CSF release observed. An approximate 3 mm × 5 mm window was then excised from the sheath, haemostasis was achieved, followed by re-attachment of the medial rectus to the globe and closure of the conjunctiva. This method as outlined by Galbraith and Sullivan 16 was performed in all but one of the eyes. One ONSF was a redo operation with an upper lid skin crease approach. All operations were performed by a consultant orbital surgeon or orbital fellow under direct supervision.
Outcome targets
The primary VA outcome was defined as a BCVA equal to 6/6 or better, with initial VA worse than 6/6. We also defined a secondary VA outcome of better than or equal to 6/12, with initial VA worse than 6/12. Snellen VA was converted to logarithm of the minimum angle of resolution (logMAR). Improvement or worsening was defined as a logMAR change of ±0.1. The visual field MD improvement cut-off was −2.0. 17
Data was analysed for each surgical outcome per eye. These outcome measures were recorded at days 10, 30, 90, 180, 360, and >360 post the ONSF procedure. Due to the non-uniform follow-up times, the time points were categorised as follows: day 0–20 as day 10, day 21–55 as day 30, day 56–135 as day 90, day 136–270 as day 180, and day 271–360 as day 360.
Statistical analysis
All analyses were performed in the R software (version 3.6.3; R Core Team 18 ). Normative data was described as mean and standard deviation. Paired t-tests were used for statistical comparisons. Due to the low samples in the CVST and other groups, statistical analysis was limited to descriptive analyses.
Results
Clinical characteristics
Clinical characteristics of the ONSFs in 116 eyes from 70 patients, 46 bilateral and 24 unilateral procedures, are shown in Table 1. Patients with IIH formed the majority of all ONSFs performed with a total of 92 eyes. 8.6% of patients had CSF diversion procedures prior to the ONSF, with the majority of these patients within the IIH subgroup. The ‘other’ cohort had a higher mean age and comprised predominantly male patients compared to the other subgroups. The mean timepoint for pre-operative recordings occurred 7.2 days prior to the ONSF.
Table 1.
Patient and eye characteristics of optic nerve sheath fenestrations (ONSF). Age, weight, and height are represented as mean (standard deviation). Continuous variables are presented as mean (standard deviation). Categorical variables are presented as N (percentage). Percentages in the overall column are as a column percentage of the total (vertical). Percentages in the subgroups are as a row percentage of the overall (horizontal).
| Aetiology | Overall | IIH | CVST | Other |
|---|---|---|---|---|
| Characteristics | ||||
| Eyes | ||||
| Total – eyes | 116 | 92 (79.3%) | 9 (7.7%) | 15 (12.9%) |
| Gender | ||||
| Male | 16 (13.8%) | 5 (31.3%) | 1 (0.6%) | 10 (62.5%) |
| Female | 100 (86.2%) | 87 (87%) | 8 (8%) | 5 (5%) |
| Age (years) | 29.8 (11.1) | 29.9 (10.7) | 25.8 (4.2) | 39 (15.7) |
| Type of ONSF | ||||
| Bilateral | 46 (79.3%) | 37 (80.4%) | 4 (8.7%) | 5 (10.9%) |
| Unilateral | 24 (20.7%) | 18 (75%) | 1 (4.2%) | 5 (20.8%) |
| Pre-operative measurements (days prior) Follow-up (days) | 7.6 (12.2) | 7.6 (10.7) | 8.4 (15.2) | 2.3 (1.2) |
| Mean | 324.7 (421.7) | 373 (454.5) | 213 (154.8) | 77 (57.5) |
| Min | 1 | 1 | 17 | 3 |
| Max | 2399 | 2399 | 412 | 193 |
| Patients | ||||
| Total | 70 | 55 (78.6%) | 5 (7.1%) | 10 (14.3%) |
| Gender | ||||
| Male | 13 (18.6%) | 5 (38.5%) | 1 (7.7%) | 7 (53.8%) |
| Female | 57 (81.4%) | 50 (87.7%) | 4 (7.0%) | 3 (5.3%) |
| Age (years) | 30.9 (11.8) | 29.9 (10.7) | 25.8 (4.2) | 39.0 (15.7) |
| Weight (kg) | 94.5 (26) | 95.2 (27.4) | 85.3 (21.6) | 93.4 (9.7) |
| Height (cm) | 170 (10) | 163 (11) | 168 (7) | 172 (9) |
| Diabetes | 3 (4.3%) | 2 (66.6%) | 0 | 1 (33.3%) |
| Hypertension | 6 (8.6%) | 4 (66.6%) | 1 (16.7%) | 1 (16.7%) |
| Smoking | 11 (15.7%) | 10 (90.9%) | 1 (9.1%) | 0 |
| Oral contraceptive | 8 (11.4%) | 5 (62.5%) | 3 (37.5%) | 0 |
| Anti-depressant | 9 (12.9%) | 7 (77.8%) | 0 | 2 (22.2%) |
| Treatment prior | ||||
| Acetazolamide | 53 (75.7%) | 46 (86.8%) | 4 (7.5%) | 3 (5.7%) |
| Topiramate | 8 (11.4%) | 7 (87.5%) | 1 (12.5%) | 0 |
| Corticosteroids | 9 (12.9%) | 4 (44.4%) | 4 (44.4%) | 1 (11.1%) |
| CSF diversion | 6 (8.6%) | 5 (83.3%) | 0 | 1 (16.7%) |
cm, centimetre; CVST, cerebral venous sinus thrombosis; IIH, idiopathic intracranial hypertension; kg, kilograms.
Surgical complications
The most frequent complications following ONSF surgery included transient diplopia found in 25% (23/92) of IIH eyes, 44% (4/9) of CVST eyes, and 13% (2/15) of other eyes. CSF diversion therapy with either a ventriculo-peritoneal or lumbo-peritoneal shunt was required in a majority of the other subgroup (33%) on comparison to the IIH and CVST groups (Table 2).
Table 2.
Complications following optic nerve sheath fenestration procedure, whereby the complications are not mutually exclusive. Percentages in the overall column are as a column percentage of the total. Percentages in the subgroups are as a row percentage of the overall.
| Complication | Total (n = 116) | IIH (n = 92) | CVST (n = 9) | Other (n = 15) |
|---|---|---|---|---|
| Transient diplopia | 29 (25%) | 23 (79.3%) | 4 (13.7%) | 2 (6.9%) |
| Diplopia requiring surgical fixation | 2 (1.7%) | 2 (100%) | 0 | 0 |
| Transient visual deterioration | 2 (1.7%) | 2 (100%) | 0 | 0 |
| Repeat ONSF | 2 (1.7%) | 2 (100%) | 0 | 0 |
| CSF diversion therapy secondary to worsening VA | 20 (17.2%) | 13 (65%) | 2 (10%) | 5 (25%) |
| Corneal Dellen | 1 (0.8%) | 1 (100%) | 0 | 0 |
| Transient ptosis | 4 (3.4%) | 4 (100%) | 0 | 0 |
CSF, cerebral sinus fluid; CVST, cerebral venous sinus thrombosis; IIH, idiopathic intracranial hypertension; VA, visual acuity.
VA
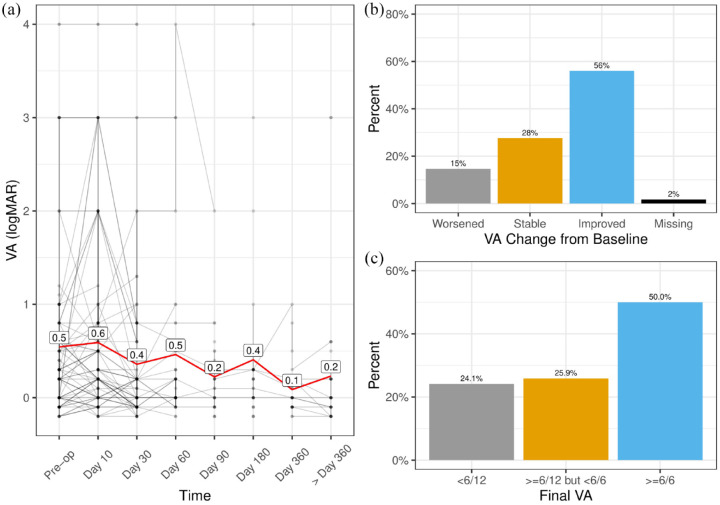
VA improved in the overall ONSF and IIH groups (Figure 1). However, a comparison of the pre-operative VA and VA at >360 days was not significant (p = 0.096).
Figure 1.
Visual acuity of all optic nerve sheath fenestration eyes. (a) Longitudinal VA (logMAR) with pre- and post-operative recordings, (b) VA changes from baseline to last follow-up, (c) best corrected visual acuity at final follow-up.
VA, visual acuity.
We compared the pre-operative VA and the last recorded VA during follow-up (mean = 324.7 ± 421.7 days). The VA of the overall group worsened in 15%, stabilised in 28%, and improved in 56% of eyes [Figure 1(a)]. There was no difference in the distribution of changes in VA for eyes, on comparison of unilateral versus bilateral procedures (p = 0.2). 50% of patients achieved a last recorded VA of 6/6 or better, 25.9% achieved a VA of between 6/6 and 6/12, and 24.1% achieved a VA worse than 6/12 [Figure 1(b)].
Clinical and demographic characteristics between patients with a stable/improved VA and those with a worsened VA are shown in Supplemental Table 1. A worse pre-operative VA and fundus grading was significantly associated with a worse VA post-operatively (Supplemental Table 1).
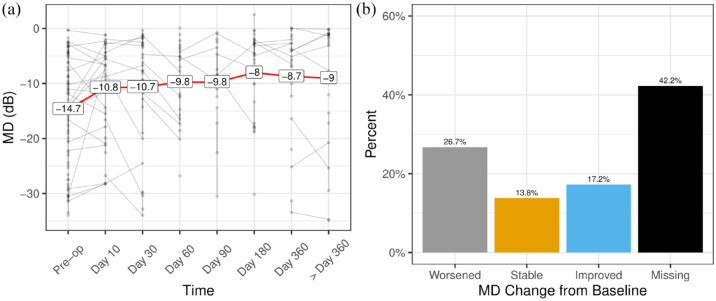
Visual field MD
Visual field MD improved significantly between pre-operative and >360 days in both the total ONSF and IIH subgroup (p = 0.001) [Figure 2(a) and (b)]. In the overall ONSF group, the MD score worsened in 26.7% of eyes, improved in 13.8%, and was stable in 17.2% [Figure 2(b)]. There was no difference in the distribution of changes in MD for eyes, on comparison of unilateral versus bilateral procedures (p = 0.69). 42% of the post-op visual fields were unable to be included due to lack of access to results or the fields’ results being classed as unreliable [Figure 2(b)].
Figure 2.
Visual field MD of (a) Overall ONSF group over time and (b) proportions of patients with improvements in MD from baseline.
IIH, idiopathic intracranial hypertension; MD, mean deviation; ONSF, optic nerve sheath fenestration.
Patient characteristics were compared between those patients whose VA was stable/improved versus worsened (Supplemental Table 2). This demonstrated that a worse pre-operative VA is associated with a worse MD post-operatively (p < 0.05).
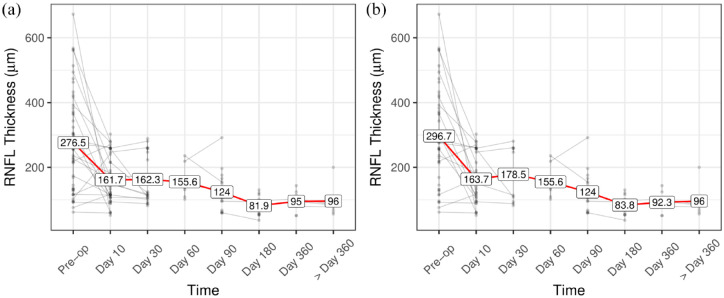
OCT measurements and clinical papilloedema ratings
The average RNFL of the overall ONSF and IIH subgroup demonstrated a trend to improvement [Figure 3(a) and (b)]. A significant difference was noted between the pre-operative and >360 days RNFL values for the overall group [mean difference (95% CI) = 182.9 (104.6–261.2), p = 0.001] and the IIH subgroup [mean difference (95% CI) = 196.4 (117.1–275.6), p = 0.001].
Figure 3.
Peripapillary RNFL of (a) overall ONSF group over time and (b) subgroup of IIH patients, whereby the values depicted are the mean measured in micrometers.
IIH, idiopathic intracranial hypertension; ONSF, optic nerve sheath fenestration; RNFL, retinal nerve fibre layer.
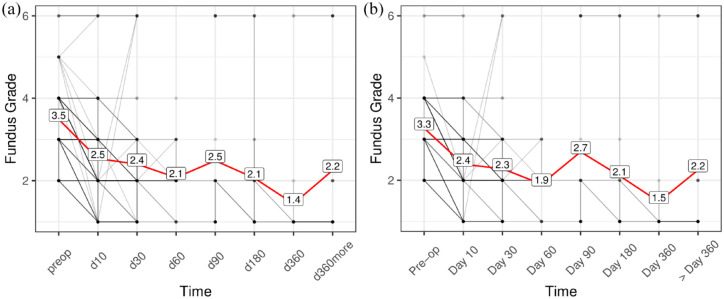
Similarly, significant improvements in fundus gradings were observed [Figure 4(a) and (b)]. Furthermore, significant differences were noted between the pre-operative and >360 days fundus ratings for the overall group [mean difference (95% CI) = 0.9 (0.3–1.6), p = 0.006] and the IIH subgroup [mean difference (95% CI) = 0.9 (0.3–1.6), p = 0.006].
Figure 4.
Fundus grading of (a) overall ONSF group over time and (b) fundus gradings in the IIH patients, whereby the values depicted on the plot are the mean.
IIH, idiopathic intracranial hypertension; ONSF, optic nerve sheath fenestration.
CVST eyes
A total of nine eyes with CVST and ongoing visual deterioration underwent ONSF (Table 3). Eyes five and six represented a severe case of visual loss secondary to CVST and demonstrated no light perception pre- and post-operatively. However, all other eyes demonstrated either stability or improvements in their VA. Minimal recordings for visual field MD and RNFL were available. The available visual field MD of the three eyes demonstrated improvements, and the two RNFL results demonstrated improvement at last follow-up.
Table 3.
Each eye with ONSF performed in patients with a CVST. Clinical and OCT measurements are shown from pre-operative assessment (pre) to the last recorded value coinciding on the day of the last follow-up (last).
| Eye | VA (pre) | VA (last) | MD (pre) | MD (last) | RNFL (pre) | RNFL (last) | Fundus (pre) | Fundus (last) | Follow-up (days) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 0.4 | 0.2 | – | – | – | – | 5 | 1 | 412 |
| 2 | 0.3 | 0.2 | – | – | – | – | 5 | 1 | 412 |
| 3 | 0.2 | 0 | – | – | – | – | – | – | 180 |
| 4 | 0.2 | 0.2 | – | – | – | – | – | – | 180 |
| 5 | 4 | 4 | – | – | – | – | 4 | 1 | 28 |
| 6 | 4 | 4 | – | – | – | – | 4 | 1 | 28 |
| 7 | 0 | −0.1 | −4.50 | −2.01 | 324 | 115 | – | – | 330 |
| 8 | −0.1 | −0.1 | −4.98 | −1.12 | 132 | 99 | – | – | 330 |
| 9 | 1 | 0.6 | −10.19 | −6.72 | – | – | 4 | 1 | 17 |
CVST, cerebral venous sinus thrombosis; MD, mean deviation; OCT, optical coherence tomography; ONSF, optic nerve sheath fenestration; RNFL, retinal nerve fibre layer; VA, visual acuity in logMAR.
Other eyes
The ‘other’ group included a total of eight cases (15 eyes, 5 bilateral procedures) that underwent ONSF for aetiologies other than IIH or CVST. The aetiologies are as listed in Table 4. Of note, 50% of the cases were in the setting of a recent resection of a brain tumour. Eyes 8 and 9, 12 and 13 did not have recorded opening pressures. All had evidence of visual failure and marked papilloedema, and the VA in two eyes worsened, eight were stable, and five improved. The available MD results demonstrated either improvement or stability in all but one eye, whereas the RNFL values improved in all patients whereby the RNFL is recorded.
Table 4.
Each eye with ONSF performed secondary to other aetiologies. Parameters are depicted as their pre-operative value (pre) and their last recorded value (last).
| Eyes | Etiology | VA (pre) | VA (last) | MD (pre) | MD (last) | RNFL (pre) | RNFL (last) | Fundus (pre) | Fundus (last) | Follow-up (days) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Post-excision of right petrous meningioma with narrowed right transverse sinus with arachnoid granulation in left transverse sinus | −0.1 | −0.1 | – | – | 264 | 117 | 3 | 2 | 48 |
| 2 | 0 | 0 | – | – | 226 | 125 | 3 | 2 | 48 | |
| 3 | Post-excision of large olfactory groove meningioma | 2 | 2 | – | – | – | – | 4 | 1 | 126 |
| 4 | 2 | 4 | – | – | – | – | 4 | 1 | 126 | |
| 5 | Paraneoplastic optic neuropathy in setting of disseminated small cell lung cancer | 0.3 | 0.3 | −24.5 | −10.0 | 95 | 57 | 5 | 3 | 193 |
| 6 | 0.3 | 0.3 | −22.5 | −12.3 | 103 | 95 | 5 | 2 | 193 | |
| 7 | Left transverse sinus thrombosis post excision of left glomus jugulare | 0.8 | −0.2 | – | – | – | – | 3 | 1 | 80 |
| 8 | Widespread leucoencephalopathy possibly due to SLE | 1 | 0.3 | – | – | – | – | 5 | 1 | 46 |
| 9 | 0.2 | 0 | – | – | – | – | 5 | 1 | 46 | |
| 10 | Metastatic prostate Ca involving orbital walls and optic foramen | 0.7 | 0.6 | – | – | – | – | 4 | 4 | 71 |
| 11 | 0.5 | 0.5 | – | – | – | – | – | – | 3 | |
| 12 | Obstructive hydrocephalus of unknown cause and steroid-responsive optic neuropathy | 1 | 1 | −25.4 | −30.4 | 283 | 106 | Pale | Pale | 42 |
| 13 | 0 | 0.2 | −13.9 | −10.1 | 174 | 107 | Pale | Pale | 30 | |
| 14 | Post-excision of large left vestibular schwannoma and LP shunt insertion | 3 | 2 | −34.0 | −34.0 | 137 | 102 | 5 | Pale | 31 |
| 15 | 0.8 | 0.8 | −28.3 | −29.7 | 117 | 87 | 5 | Pale | 31 |
LP, lumboperitoneal; MD, mean deviation; ONSF, optic nerve sheath fenestration; RNFL, retinal nerve fibre layer; SLE, systemic lupus erythematosus; VA, visual acuity.
Discussion
ONSF performed in the appropriate setting is a recognised treatment to preserve visual function in IIH and CVST.12,13 However, little is known about the outcomes of ONSF used for other disease processes, and the natural history over time following the procedure. 13 This retrospective analysis aimed to elucidate the natural history of outcomes following ONSF over various time intervals, as well as providing insights into indications other than IIH and CVST.
ONSF is shown to improve VA, with a total of 27% improving and 59% achieving stability (Figure 1). These values are consistent with previous retrospective analysis’ in the literature, with a recent systematic review indicating improvement in 44.1% of a total collated 962 cases. 19 Additionally, 50% of patients achieved a VA better than or equal to 6/6 at last follow-up, which indicates not only stability following surgery, but good visual outcomes. There was no difference in the distribution of VA outcomes (improvement/stability/worsening) on comparison of unilateral versus bilateral procedures: noting that this was calculated from eye level data and was not a primary outcome. It has been noted previously that unilateral procedures of ONSF do have a positive effect on visual outcomes of both eyes in IIH. 20 Hence in our cohort any difference between the unilateral versus bilateral procedures may require a larger sample size to be observed. Furthermore, a worse VA or fundus grading pre-operatively was found to be associated with a worsening VA post-operatively at last follow-up (Supplemental Table 1), hence indicating urgent assessment and therapeutic decisions in these patients upon presentation/during close follow-up. When considered in patients with ‘other’ indications, the VA either improved or was stable in all except for one eye. With only two eyes in the ‘other’ cohort experiencing transient diplopia as the predominant complication (Table 2), ONSF can be considered a safe treatment for other conditions. 12
The automated visual field perimetry MD scores demonstrated improvement on comparison between the pre-operative and >360 day values in both the overall and IIH subgroup (Figure 2). The improvements noted in our series (improvement in 13.8% of eyes; stability in 17.2%) is lower than the reported 65.2% improvement noted in a recent review. 19 Additionally, as demonstrated in Figure 2(b), 42% of the post-op visual fields were unable to be included, which highlights the importance of standardised visual field practices between hospitals. Interpretation of visual field improvement in the ‘other’ subgroup was limited by missing evaluations and may indicate less rigorous ophthalmological assessment and follow-up of this cohort.
We noted significant improvement in papilloedema as measured by both peripapillary RNFL thickness and papilloedema grades. A similar improvement was noted in the CVST and other subgroups, indicating a similar effect in these cohorts, which has been demonstrated in prior observational studies in CVST patients. 12 The rapid lowering of peripapillary RNFL measurements post-ONSF is objective evidence of successful surgery through local release of pressure and reduction of ICP. This is also supported by prior studies demonstrating that OCT can also be used to non-invasively measure ICP in IIH. 21 However, it may be confounded by optic nerve head atrophy secondary to chronically raised ICP, which may represent a progression of the disease process. Furthermore, prior medical or surgical treatment of IIH can make the interpretation of the peripapillary RNFL outcomes difficult. 22 Monitoring of disease progression in patients with visual failure in the setting of raised pressures includes a combination of visual field perimetry, and OCT. In the setting of rapid deterioration, further urgent neuroimaging (magnetic resonance imaging with venogram) is repeated with the addition of further lumbar punctures to assess opening pressures.
The lack of a comparator group limited our ability to comment and/or recommend ONSF against other treatment modalities. As the aim of the study was to elucidate the visual outcomes following ONSF, we did not exclude patients with previous CSF diversion procedures. This may have had a confounding result on the outcomes with a potential increased apparent effectiveness. Additionally, with regards to interpretation of our Frisen grading, we did not have a blind analysis conducted by separate assessors, hence making the interpretation of these results less reliable. This lack of uniform assessment can be seen in the wide variability of gradings in the Figure 4 plots. Furthermore, there was both incomplete and non-uniform follow-up data available at each time point, especially for the CVST and other groups.
Conclusion
ONSF demonstrated trends of improvement in VA documented over time, with a large proportion of our eyes demonstrating stability/improvement. Furthermore, significant improvements were seen with regard to MD, RNFL, and Frisen grading. Our data demonstrates effectiveness of ONSF in aetiologies other than IIH and CVST when there is raised ICP, papilloedema, and visual failure, particularly when other CSF diversion procedures or medical therapies have failed or are unsuitable.
Supplemental Material
Supplemental material, sj-docx-1-tan-10.1177_17562864231197994 for A 20-year multicentre retrospective review of optic nerve sheath fenestration outcomes by Shaddy El-Masri, Matthew Wilson, Jonathan Goh, Paul Sanfilippo, Anthony Fok, Thomas Hardy, Rahul Chakrabarti and Anneke Van Der Walt in Therapeutic Advances in Neurological Disorders
Acknowledgments
None.
Footnotes
ORCID iDs: Shaddy El-Masri  https://orcid.org/0000-0002-5264-5885
https://orcid.org/0000-0002-5264-5885
Anneke Van Der Walt  https://orcid.org/0000-0002-4278-7003
https://orcid.org/0000-0002-4278-7003
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Shaddy El-Masri, Royal Melbourne Hospital, Hospital City Campus, Grattan Street, Parkville, VIC 3050, Australia; Royal Adelaide Hospital, Adelaide, SA, Australia.
Matthew Wilson, Royal Victorian Eye and Ear Hospital, Melbourne, VIC, Australia.
Jonathan Goh, Royal Victorian Eye and Ear Hospital, Melbourne, VIC, Australia.
Paul Sanfilippo, Neuroscience Department, The Alfred Hospital, Melbourne, VIC, Australia.
Anthony Fok, Royal Melbourne Hospital, Parkville, VIC, Australia.
Thomas Hardy, Royal Victorian Eye and Ear Hospital, Melbourne, VIC, Australia.
Rahul Chakrabarti, Royal Victorian Eye and Ear Hospital, Melbourne, VIC, Australia.
Anneke Van Der Walt, Royal Victorian Eye and Ear Hospital, Melbourne, VIC, Australia; Neuroscience Department, The Alfred Hospital, Melbourne, VIC, Australia.
Declarations
Ethics approval and consent to participate: This study was approved by the Royal Victorian Eye and Ear Hospital human research ethics committee (approval number 19/1416HL). Participant consent was not required according to local legislation, as this was a retrospective study.
Consent for publication: Not applicable.
Author contributions: Shaddy El-Masri: Conceptualization; Investigation; Methodology; Project administration; Resources; Writing – original draft; Writing – review & editing.
Matthew Wilson: Conceptualization; Data curation; Methodology; Validation; Visualization.
Jonathan Goh: Conceptualization; Data curation; Writing – review & editing.
Paul Sanfilippo: Conceptualization; Formal analysis; Investigation; Validation; Visualization; Writing – review & editing.
Anthony Fok: Conceptualization; Methodology; Supervision; Validation.
Thomas Hardy: Investigation; Methodology; Supervision; Writing – review & editing.
Rahul Chakrabarti: Conceptualization; Investigation; Methodology; Supervision; Writing – review & editing.
Anneke Van Der Walt: Conceptualization; Investigation; Methodology; Project administration; Supervision; Validation; Writing – review & editing.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of data and materials: The datasets generated during and/or analysed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
- 1. Hayreh SS. Pathogenesis of optic disc edema in raised intracranial pressure. Prog Retin Eye Res 2016; 50: 108–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dewecker L. An incision of the optic nerve in cases of neuroretinitis. First Ophthalmol Congress Rep 1872; 4: 11–14. [Google Scholar]
- 3. Acheson JF. Optic nerve disorders: role of canal and nerve sheath decompression surgery. Eye (Lond) 2004; 18: 1169–1174. [DOI] [PubMed] [Google Scholar]
- 4. Wall M. Idiopathic intracranial hypertension: mechanisms of visual loss and disease management. Semin Neurol 2000; 20: 89–95. [PubMed] [Google Scholar]
- 5. Mollan SP, Davies B, Silver NC, et al. Idiopathic intracranial hypertension: consensus guidelines on management. J Neurol Neurosurg Psychiatr 2018; 89: 1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wall M. Idiopathic intracranial hypertension. Neurol Clin 2010; 28: 593–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hamedani AG, Thibault DP, Revere KE, et al. Trends in the surgical treatment of pseudotumor cerebri syndrome in the United States. JAMA Netw Open 2020; 3: e2029669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Acheson JF, Green WT, Sanders MD. Optic nerve sheath decompression for the treatment of visual failure in chronic raised intracranial pressure. J Neurol Neurosurg Psychiatry 1994; 57: 1426–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Alsuhaibani AH, Carter KD, Nerad JA, et al. Effect of optic nerve sheath fenestration on papilledema of the operated and the contralateral nonoperated eyes in idiopathic intracranial hypertension. Ophthalmology 2011; 118: 412–414. [DOI] [PubMed] [Google Scholar]
- 10. Nithyanandam S, Manayath GJ, Battu RR. Optic nerve sheath decompression for visual loss in intracranial hypertension: report from a tertiary care center in South India. Indian J Ophthalmol 2008; 56: 115–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Murdock J, Tzu JH, Schatz NJ, et al. Optic nerve sheath fenestration for the treatment of papilledema secondary to cerebral venous thrombosis. J Neuroophthalmol 2014; 34: 67–69. [DOI] [PubMed] [Google Scholar]
- 12. Li Z, Cheng L, Xu Y, et al. Optic nerve sheath fenestration for progressive visual loss in cerebral venous sinus thrombosis: a long-term retrospective observational study. Neurol Ther 2023; 12: 441–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chen H, Zhang Q, Tan S, et al. Update on the application of optic nerve sheath fenestration. Restor Neurol Neurosci 2017; 35: 275–286. [DOI] [PubMed] [Google Scholar]
- 14. Moreau A, Lao KC, Farris BK. Optic nerve sheath decompression: a surgical technique with minimal operative complications. J Neuroophthalmol 2014; 34: 34–38. [DOI] [PubMed] [Google Scholar]
- 15. Morello A, Bianconi A, Cogoni M, et al. Bilateral idiopathic optic nerve sheath meningocele: a case report and literature review. J Neurosci Rural Pract 2022; 13: 781–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Galbraith JE, Sullivan JH. Decompression of the perioptic meninges for relief of papilledema. Am J Ophthalmol 1973; 76: 687–692. [DOI] [PubMed] [Google Scholar]
- 17. Yaqub M. Visual fields interpretation in glaucoma: a focus on static automated perimetry. Commun Eye Health 2012; 25: 1–8. [PMC free article] [PubMed] [Google Scholar]
- 18. R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing V, Austria, https://www.R-project.org/ (2020, accessed 20 December 2020).
- 19. Kalyvas A, Neromyliotis E, Koutsarnakis C, et al. A systematic review of surgical treatments of idiopathic intracranial hypertension (IIH). Neurosurg Rev 2021; 44: 773–792. [DOI] [PubMed] [Google Scholar]
- 20. Hagen SM, Wegener M, Toft PB, et al. Unilateral optic nerve sheath fenestration in idiopathic intracranial hypertension: a 6-month follow-up study on visual outcome and prognostic markers. Life (Basel) 2021; 11: 778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Vijay V, Mollan SP, Mitchell JL, et al. Using optical coherence tomography as a surrogate of measurements of intracranial pressure in idiopathic intracranial hypertension. JAMA Ophthalmol 2020; 138: 1264–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Skau M, Yri H, Sander B, et al. Diagnostic value of optical coherence tomography for intracranial pressure in idiopathic intracranial hypertension. Graefes Arch Clin Exp Ophthalmol 2013; 251: 567–574. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-tan-10.1177_17562864231197994 for A 20-year multicentre retrospective review of optic nerve sheath fenestration outcomes by Shaddy El-Masri, Matthew Wilson, Jonathan Goh, Paul Sanfilippo, Anthony Fok, Thomas Hardy, Rahul Chakrabarti and Anneke Van Der Walt in Therapeutic Advances in Neurological Disorders