Abstract
Objective:
Impairment in physical function and physical performance leads to decreased independence and health-related quality of life in people living with chronic kidney disease and end-stage kidney disease. Physical activity and exercise in kidney care are not priorities in policy development. We aimed to identify global policy-related enablers, barriers, and strategies to increase exercise participation and physical activity behavior for people living with kidney disease.
Design and Methods:
Guided by the Behavior Change Wheel theoretical framework, 50 global renal exercise experts developed policy barriers and enablers to exercise program implementation and physical activity promotion in kidney care. The consensus process consisted of developing themes from renal experts from North America, South America, Continental Europe, United Kingdom, Asia, and Oceania. Strategies to address enablers and barriers were identified by the group, and consensus was achieved.
Results:
We found that policies addressing funding, service provision, legislation, regulations, guidelines, the environment, communication, and marketing are required to support people with kidney disease to be physically active, participate in exercise, and improve health-related quality of life. We provide a global perspective and highlight Japanese, Canadian, and other regional examples where policies have been developed to increase renal physical activity and rehabilitation. We present recommendations targeting multiple stakeholders including nephrologists, nurses, allied health clinicians, organizations providing renal care and education, and renal program funders.
Conclusions:
We strongly recommend the nephrology community and people living with kidney disease take action to change policy now, rather than idly waiting for indisputable clinical trial evidence that increasing physical activity, strength, fitness, and function improves the lives of people living with kidney disease.
Introduction
CHRONIC KIDNEY DISEASE (CKD) is associated with an increasing human, economic, and health resource burden, and the sustainability of worldwide kidney care growth is uncertain.1 Increased focus on globally cost-effective, preventative lifestyle interventions, such as increased physical activity behavior, is required.2 Physical dysfunction, with low muscle mass and low muscle strength, is an enormous threat to the quality of life and independence of people with CKD3 and end-stage kidney disease (ESKD).4 Impaired physical function and sedentary lifestyles are associated with comorbid disease progression and increased mortality risk.5,6 Unfortunately, people with CKD and ESKD have been largely unsupported about engaging in physical activity and exercise interventions in part because of the limited focus on policy barriers and enablers.7
Health and social policy reform can result in improved health outcomes both at population and individual levels.8 Policy barriers can relate to funding, service provision, legislative, regulatory, clinical practice guideline recommendations, environmental, social, communication, and marketing elements.9 Although lack of physical activity is consistently perceived to be a local issue, a broader global policy review has been recommended to understand policy barriers worldwide.10 We aimed to develop a consensus to identify global policy-related enablers, barriers, and strategies to increase exercise participation and physical activity behavior for people living with kidney disease.
Methods
In November 2019, the Global Renal Exercise Network (GREX) held an inaugural meeting in Alberta, Canada, that was attended by an international mix of 50 leading clinicians, researchers, and people living with kidney disease.10 The overarching objective of this meeting was to increase the inclusion of physical activity and exercise in kidney care on a global scale. The group defined physical activity as bodily movements produced by skeletal muscles that result in energy expenditure11 and exercise as planned, structured, and repetitive bodily physical activity designed to improve physical function and quality of life.12
Guided by the Behavior Change Wheel framework,9 the attendees explored policy barriers and enablers to exercise program implementation and physical activity promotion in kidney care and developed a consensus document over the succeeding 8 months.
The consensus process consisted of developing themes from 50 global regional exercise experts attending the GREX workshop (North America, South America, Continental Europe, United Kingdom, Asia, and Oceania). These themes were submitted to the coordinating GREX group who developed these themes into a 11000-word summary document. This document was then disseminated to the larger consensus group members who refined the consensus document into concise 3000 word “Policy Barriers and Enablers to Exercise and Physical Activity in Kidney Care” that was approved and endorsed by the GREX Network (Figure 1).
Figure 1.
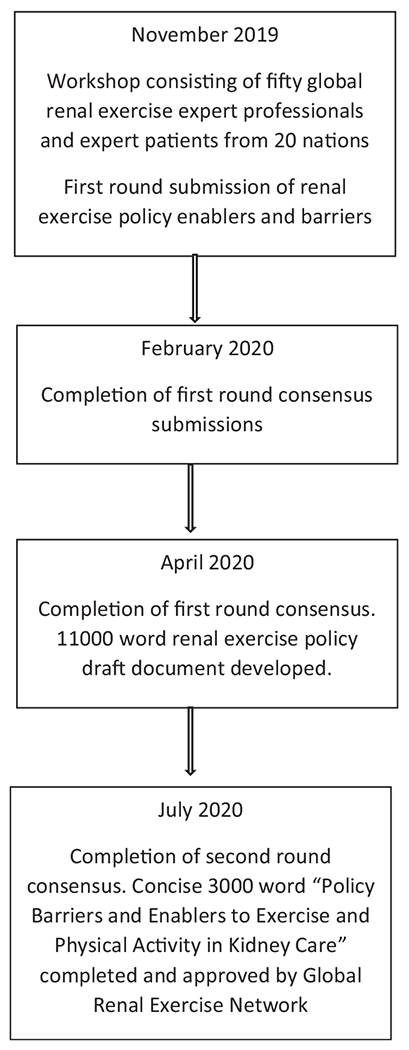
Global renal exercise network policy consensus process.
Result of Consensus Process
The results of the consensus process identified the enablers and barriers to exercise and physical activity. This was aligned with the Behavior Change Wheel approach of funding, service provision, legislative, regulatory, clinical practice guideline recommendations, environmental, social, communication, and marketing as elements required for broad policy change.9 In addition, the consensus group developed potential strategies that nephrology programs could embrace to increase exercise and physical activity for people in their care.
Enablers, Barriers, and Strategies
Funding
The funding of renal services is frequently linked to quality metrics that drive models of clinical care.13 Although patients with kidney disease have identified components of lifestyle management as priorities in renal care,14,15 quality metrics in place commonly fail to incentivize preventive lifestyle activities, such as physical activity.16 In the United States (US), the Center for Medicare and Medicaid Services administers the Quality Incentive Program that links financial reimbursements for dialysis facilities to a core set of quality measures.17 Unfortunately, these quality measures are largely based on biochemical parameters, are not associated with patient-reported outcome measures,18 and do not incentivize action upon measures of quality of life and dialysis experience.19 As a result, these metrics lead to misaligned priorities between the dialysis providers and people requiring dialysis. In countries with one-payer, government-funded universal health-care systems, there is limited funding for lifestyle activity programs. Japan is the outstanding exception, offering exercise training for people with CKD stage 3B–5, funded by the national health insurance system.20,21
Two strategies that can address funding limitations are to (1) mandate funding-linked physical activity metrics and (2) increase physical disability and sarcopenia diagnostic coding (Table 1). Given the high prevalence of physical disability among people with CKD and ESKD,22 increased awareness and use of such diagnostic codes can provide accurate estimates of the prevalence of these conditions to help mobilize reimbursable rehabilitation services. This requires greater coding vigilance similar to what is currently performed in cardiac rehabilitation.23 Implementing the aforementioned strategies could drive health services toward increasing physical function and activity levels in people with CKD and ESKD.
Table 1.
Exercise and Physical Activity Policy Barrier Domains and Strategies in Kidney Care
| Domain | Policy Strategies in Kidney Care |
|---|---|
| Funding | • Mandate funding-linked exercise and physical activity metrics • Increase and improve physical disability diagnostic coding • Fund renal exercise professionals |
| Service provision | • Integrate appropriate clinical algorithms for nonexercise renal professionals that include clinical algorithms, tailored exercise prescriptions, and brief clinical safety reviews • Develop and introduce nationwide policies that mandate the opportunistic delivery of consistent and concise healthy lifestyle information • Integrate cost-effective renal exercise professional models of care • Include exercise and physical activity education in undergraduate and graduate renal professional training programs |
| Regulations and legislation | • Support policy that endures liability cover for health professionals supporting increased physical activity • Decrease risk by introducing stratified activity risk assessment • Develop an education and accreditation process for renal exercise professionals |
| Guidelines and research | • Improved evidence through international, well-designed pragmatic clinical trials • Advance the idea of a global clinical renal exercise and physical activity research consortium into reality |
| Environmental and social | • Design fitness areas into outpatient and dialysis centers • Design and store exercise equipment to maximize staff and patient safety • Develop and coordinate policy-supported, funded group physical activity and exercise programs |
| Communication and marketing | • Encourage national and global nephrology associations to collaborate with rehabilitation and exercise professional organizations • Recommend that organizations supporting people with kidney disease lobby government, policy-makers, and health-care providers to include their voice in policy initiatives • Engage with minority diverse communities to ensure information and education available to all |
Service Provision
Globally, the provision of healthy lifestyle interventions is limited by health service fragmentation. Preventative exercise and rehabilitation programs rely on the coordination and alignment of primary, secondary, and tertiary care.24 Most exercise training programs for people with chronic diseases are managed by community organizations that are commonly not aligned with tertiary renal care.21 The result is that people with CKD and ESKD, who are physically deteriorating, fall into a gap without access to funded exercise programs that individuals living with other chronic diseases have access to25 (i.e., cardiac rehabilitation23,26 and pulmonary rehabilitation).27–29 The inclusion of physical activity assessment, prescription, and management as part of routine clinical care in CKD and ESKD clinical pathways and policies would address this gap. Unfortunately, the capacity of nephrology clinicians to provide exercise expertise is currently limited.30
Most people living with kidney disease believe that an increase in physical activity is beneficial and agree that they would exercise if advised to do so by their physician.31,32 Although nephrologists in some countries (Canada, Australia, and New Zealand) believe that exercise counseling is within their scope of practice,25 few nephrologists consistently discuss exercise as a relevant component of a treatment or prevention strategy during clinical interactions.30,33 Nephrology nurses do not always believe it is their responsibility to conduct exercise programs,34 and they are restricted by high workloads,35 limitations in scope of practice,36 and lack of education relating to physical activity.37
Limited evidence and experience, absence of guidelines, and safety concerns also impact the nephrology clinician’s confidence and capacity to motivate people to increase physical activity. Although people with CKD and ESKD have extremely low functional status compared with the general population, and are at a greater risk for cardiovascular events, evidence to support restricting exercise does not exist.38 A systematic review of 45 CKD and ESKD exercise studies reported no increase in the risk of cardiac events, serious adverse events, hospitalization, or mortality as a consequence of exercise, but rather significant positive effects on physical fitness, walking capacity, blood pressure, heart rate, and health-related quality of life.39 Taking into account contraindications such as cardiac instability and active illnesses, encouraging people to move more is likely to almost always be safe. As clinicians become more comfortable with encouraging physical activity in individuals with various comorbidities and levels of disabilities, the number of people that are approached to participate in exercise programs will increase.40
Strategies to address service provision policy barriers include
Developing better evidence for exercise programming and physical activity programming in individuals with varying levels of function and comorbidities. Promoting exercise research in CKD to achieve decreased disease burden and decreased costs is relevant to policy-makers.41,42 Recent developments to address the lack of evidence have highlighted the need for large studies that focus on the effect of exercise programs on the risk of cardiovascular disease, symptom burden, morbidity, and mortality.25,43–45 Given most renal interventional studies are underpowered and subject to selection bias,45 international, well-funded, pragmatic multicenter clinical trials are required.
Specific education to address concerns or perceived risks of exercise participation in undergraduate and postgraduate renal professional training programs is likely to contribute to increasing emphasis on exercise, physical activity, and patient referral to appropriately qualified exercise professionals.37,46
A policy of integrating clinical tools to facilitate addressing exercise and physical activity in clinical encounters such as the provision of exercise guides,47–49 simple tailored exercise prescriptions, and brief clinical safety reviews (such as checking vitals, ruling out acute cardiovascular symptoms). These clinical algorithms in the form of checklists can assist renal clinicians without exercise professional knowledge and skills.
Actionable national health system policy initiatives to increase the opportunistic delivery of consistent and concise healthy lifestyle information will enable all individuals to engage in conversations about health across all organizations and populations.50
Increasing the number of exercise professionals associated with renal programs. The most successful strategy to date has been the policy to include exercise professionals (exercise physiologists, kinesiologists, physical therapists, rehabilitation specialists, occupational therapists, athletic trainers, personal trainers, student clinical placements) in renal programs to ensure the delivery of safe, individualized, and effective services and to support the sustainability of exercise participation and physical activity behavior change across a range of in-center, community, and home-based settings.51–56
Regulations and Legislation
The regulations and policies governing renal clinicians’ scope of practice may constrain clinically sustainable renal exercise programs. However, nephrologists, renal dietitians, renal social workers, and renal nurses can provide exercise and lifestyle advice while still acting in accordance with their scope of practice.57 In the UK, clinicians can prescribe exercise as if prescribing a medication “off-license” if they are covered to do so by their hospital’s trust and approved to make such prescriptions as part of their professional registration.58 In the regions where exercise professionals provide renal exercise programs, coverage can be assured through their professional registration organizations.
Potential policy strategies to mitigate liability concerns could include stratifying those with the highest risk of complications by assessing baseline physical function status. Policies can include guidelines for reassessment by an exercise professional, such as after a hospitalization episode, hemodynamic instability, or a new or chronic condition.59 Higher risk groups could be triaged for referral to exercise professionals in physical rehabilitation services before engaging in structured exercise and physical activity programs60.
Considered from another perspective, the ethical requirements of nonmaleficence and beneficence implore the clinician to do all that is within their scope of practice to benefit and mitigate harm to people in their care. Therefore, addressing the needs of people with kidney disease who require support to prevent physical deterioration and disability is an ethical responsibility.37
The lack of a career pathway for renal exercise professionals is a further regulatory barrier to the development of expert renal exercise practice. Accreditation is unavailable in most countries except for Japan where the Japanese Society of Renal Rehabilitation, established in 2011, initiated a certification program for the Registered Instructor of Renal Rehabilitation (RIRR).61 The RIRR has embraced interdisciplinary members (nephrologists, registered nurses, physical therapists, occupational therapists, clinical laboratory technicians, medical engineers, dietitians, and exercise trainers) as certified renal rehabilitation instructors who have qualified by passing the RIRR examination. Once qualified, clinicians’ services are then covered by the Japanese National Health Insurance System.
Guidelines
Guidelines addressing renal physical activity implementation strategies are restricted by limited robust evidence. Furthermore, the limited number of rigorous randomized controlled trials addressing physical function have been performed under optimal conditions and often fail to be translated into real-world clinical settings. Therefore, pragmatic clinical trials exploring physical activity in kidney disease should study samples representative of the general CKD population and assess outcomes such as quality-adjusted life years, disability-adjusted life years, and patient-reported outcome measures. Qualitative methodologies that address the importance of exercise and physical activity participation and important factors to consider in the implementation of such programs from the perspective of people living with kidney disease can enhance the findings of quantitative studies.55
Policy-makers require large robust studies to move from non–evidence-based suggestions to definitive recommendations, and although the challenges in designing and conducting randomized controlled trials are not unique to exercise interventions, the absence of influential studies supporting exercise in the nephrology literature is particularly striking. To accelerate knowledge generation and education, the formation of a global clinical research consortium focused on renal exercise and physical activity can contribute to the production and application of these evidence goals.
The recent UK Renal Association Clinical Practice Guidelines on Haemodialysis provides the most recent and practical guidelines using the best evidence available promoting intradialytic exercise.62 The US Kidney Disease Outcomes Quality Initiative clinical practice guidelines recommend exercise and questionnaire-based assessments; however, there are limited actionable recommendations for those with poor physical function.63,64 Guidelines could include recommendations that physical activity initiatives be mandatory within renal programs.
The Kidney Disease Improving Global Outcomes Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease65 recommends that individuals with CKD engage in physical activity for at least 30 minutes per day, 5 times per week. Importantly, a blanket guideline such as this fails to reflect the complexities that exist for people with kidney disease who are burdened with fatigue and weakness.66 Anything beyond maintenance of activities of daily living may be overwhelming for many.
Although guideline development does not always result in practice change, guidelines can be useful for policy-makers to guide the best policies for clinical care. Thus, exercise and physical activity guidelines such as the upcoming European Renal Best Practice benefits and harms of exercise training in people with CKD (https://www.era-edta.org/en/exercise-as-erbp-guideline-topic/) and the International Society of Peritoneal Dialysis/GREX Peritoneal Dialysis Clinical Recommendations Project (http://grexercise.kch.illinois.edu/) will be beneficial for policy-makers.
Environment and Social Elements
Local neighborhoods and climates matter when developing policy to increase physical activity in CKD and ESKD. People with ESKD have ranked their home as their preferred exercise location, followed by their neighborhood and gym.31 Possession of home exercise equipment and perceived access to physical activity opportunities in the community have been positively associated with the maintenance of postcardiac rehabilitation exercise.67 These findings are likely transferrable to the kidney disease population. Grants for the acquisition of home exercise equipment for motivated financially disadvantaged people with kidney disease could be made available through local kidney foundations or charitable groups that often have favorable taxation arrangements. People with kidney disease can also be directed via social media to walking groups and gyms in their area that can provide a physically active environment for people with multiple comorbid illnesses.
When exercise at home cannot be undertaken, exercise in, or close to, a health clinic may be preferred. Unfortunately, inflexible or unavailable transport can be a barrier to physical activity.68 To overcome this barrier, gymnasiums or fitness areas could be incorporated into newly designed renal clinics and dialysis units to facilitate the implementation of routine exercise and physical activity, ensuring strict precautions to maintain high standards of infection control. This would address transportation barriers and potential fatigue associated with attending multiple appointments and traveling to places of exercise.69,70 Alternatively, funded group exercise programs, where people can be placed into groups according to their location of residence (using postal codes) with sponsored community transportation, can facilitate group exercise, foster mutual encouragement, and create an exercise community for people with kidney disease.
Limited guidelines or policies have been developed to address exercise safety at home or in supervised, clinical environments. Policies are recommended to ensure functional limitations, fear of falling, recent hospitalizations, cardiovascular stability, or the presence of comorbid conditions are recognized and addressed in recommended programming, while still encouraging physical activity.59 Both home- and clinic-based exercise programs require financially feasible equipment that is easily maneuverable with appropriately designed handles and requires minimal storage space.55 Elastic fitness bands are ideal as they are inexpensive and easy to store, and people can keep their bands separate from others to minimize cross-infection if participating in group exercise programs.71 Designing future clinics to enhance space for exercise equipment storage and support staff, such as patient care assistants or service workers, is also an important strategy to help support such exercise initiatives.7 Policies that support and outline staff roles, storage, cleaning, infection control, and moving of exercise equipment such as standard operating procedures can support exercise engagement in renal programs.72
Communication and Marketing
Effective communication and marketing are required to influence health and social policy at various levels of administration and government. This has been a great challenge for the nephrology community. Historically, encouraging and mandating physical assessment and exercise prescription in clinical practice has been largely unsuccessful. National and international nephrology associations can collaborate with rehabilitation and exercise professional organizations to increase the awareness of the impact of physical dysfunction and inactivity in individuals with kidney disease and help develop professional career paths to address the deficit of expertise in this area.61 The JSRR has led the way in this realm, managing to successfully combine nephrology with exercise professionals.61 This has led to the concept of renal rehabilitation which has become accepted among multiple stakeholders in Japan including nephrologists, exercise professionals, nutrition specialists, nurses, and people living with kidney disease.73
On the global stage, GREX is working with professional nephrology societies (International Society of Nutrition and Metabolism) and renal exercise groups (European Association of Rehabilitation in CKD and the JSRR) to improve the evidence base for physical activity and exercise, highlight the known benefits, and provide support for the implementation of physical activity programs.74 GREX is actively pursuing certification processes, international collaborative research, and implementation projects to continue to promote exercise and physical activity in CKD across the globe. Through each of these activities, GREX is hoping to raise awareness among nephrologists, people living with kidney disease, and major decision-makers about the benefits of exercise in CKD and to promote strategies for increased implementation of physical activity programs.
In addition to established professional nephrology organizations, highly effective organizations run by, and representing, people with kidney disease have a pivotal role to play. Government, policy-makers, and health-care providers require a voice and input from the true kidney experts, those who are living with kidney disease. Not-for-profit health charities and nongovernment organizations supporting kidney health can be found in most countries, and many have been successful in partnering with local health service activities. These organizations can offer expertise and support to pilot projects and initiatives to encourage activity and patient-centered research within the renal population. The involvement of people living with kidney disease in evaluating exercise and physical activity initiatives provides a strong basis for the adoption of policies and practices. This strategy can provide the “patient perspective” to challenge or refute perceived barriers that appear insurmountable to those working in the health-care system.
Globally, we are an increasingly diverse world in terms of race, color, ethnicity, nationality, religion, socioeconomic status, education, marital status, language, age, gender, gender expression, gender identity, sexual orientation, mental or physical ability, genetic information, and learning styles. Integrating the voice of the person living with kidney disease from all individuals into policy requires the voice of those from all diverse backgrounds. In particular, the development and dissemination of educational resources using traditional and social media methods for those from all backgrounds is vital for a culture of exercise and physical activity to be maintained. Globally, minorities are particularly at risk of CKD, physical inactivity, and lifestyle diseases, yet insufficient resources are allocated to generate educational materials that meet these groups’ specific requirements.
The barriers to increasing physical activity behavior in people living with kidney disease are numerous. Overcoming these barriers requires all stakeholders associated with kidney care to consider what each can do to enhance policy development and implementation in this area. We have summarized policy initiatives that can enable diverse stakeholders to better encourage physical activity and exercise participation, independence, and improved quality of life in people with kidney disease in Table 2.
Table 2.
Renal Exercise and Physical Activity Policy Recommendations for Nephrology Stakeholders
| Stakeholder | Recommendations |
|---|---|
| Nephrologists and renal clinicians | • Include physical function and physical activity as part of the medical history • Discuss exercise and physical activity as interventions for risk factor modification • Support exercise and physical activity studies by encouraging participation • Determine medical clearance when indicated only before initiating vigorous exercise |
| Renal care provider organizations | • Include physical activity assessment and strategies in clinical pathways • Develop local, regional, and national renal physical activity key performance indicators • Advocate for exercise professionals with the capacity to individualize exercise and physical activity assessment and counseling • Disseminate free online toolkits already available for exercise programs • Seek opportunities and partnerships with universities specializing in exercise professional training for clinical placements • Design gymnasiums, equipment, and activity centers in future clinic design |
| Funders | • Include exercise professionals in future funding models • Include physical activity credits to offset medication or insurance costs • Promote fitness membership in insurance packages • Include physical activity metrics in funding models • Provide incentives for clinics that promote physical activity |
| Education providers | • Develop short course, online, and postgraduate education options in renal rehabilitation • Develop nephrology exercise certification programs • Increase and incentivize exercise and physical activity education in nephrology medicine and nursing programs • Increase the amount of renal education in exercise professional courses • Seek opportunities with renal providers for student placement in renal programs |
Conclusion
The effective delivery of exercise interventions and physical activity promotion via clinical services will require pragmatic policies to ensure the development of sustainable systems that support education, leadership, expertise, facilities, and equipment. People living with kidney disease, who are burdened with low physical function and high prevalence of troublesome symptoms, require global and local policy reform to address funding, service provision, legislation, regulations, guidelines, environmental aspects, and communication and marketing to maintain physical activity and a high quality of life. Given that other chronic disease communities have pre-existing, long-adopted exercise and physical activity policies, we strongly recommend that the nephrology community act now to promote “moving more” to improve the lives of people living with kidney disease.
Practical Application
Even though physical dysfunction decreases the quality of life and independence of people with kidney disease, physical activity and exercise is not a policy priority. Clinicians, administrators, renal care provider organizations, program funders, and education providers are well positioned to incorporate and promote local and regional policies to improve the physical function of individuals with kidney disease.
Acknowledgments
The authors wish to acknowledge the support of the Global Renal Exercise Network (GREX). This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Funding Disclosures:
B.R. acknowledges funding from the National Institutes of Diabetes, Digestive and Kidney Diseases (K23 DK0099442 and R03 DK114502) and Dialysis Clinics Incorporated (C-4112). M.M.-D.’s work is supported by NIDDK R01DK114074. C.B. is supported by the Manitoba Medical Services Fund FW Duval Clinical Research Professorship. T.J.W., C.J.L., and A.C.S. gratefully acknowledge funding from the Stoneygate Trust, and their work is supported by the UK National Institute for Health Research Leicester Biomedical Research Centre (NIHR BRC). The views expressed are those of the author and not necessarily those of the National Health Service, NIHR BRC, or the Department of Health. J.L. V.’s work is supported by the Portuguese Foundation of Science and Technology (UID/04045/2020).
References
- 1.Luyckx VA, Tonelli M, Stanifer JW. The global burden of kidney disease and the sustainable development goals. Bull World Health Organ. 2018;96:414–422D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luyckx VA, Tuttle KR, Garcia-Garcia G, et al. Reducing major risk factors for chronic kidney disease. Kidney Int Suppl. 2017;72:71–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sheshadri A, Johansen KL. Prehabilitation for the frail patient approaching ESRD. Semin Nephrol. 2017;37:159–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Intiso D. The rehabilitation role in chronic kidney and end stage renal disease. Kidney Blood Press Res. 2014;39:180–188. [DOI] [PubMed] [Google Scholar]
- 5.Robinson-Cohen C, Littman AJ, Duncan GE, et al. Assessment of physical activity in chronic kidney disease. J Ren Nutr. 2013;23:123–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Matsuzawa R, Roshanravan B, Shimoda T, et al. Physical activity dose for hemodialysis patients: where to begin? Results from a prospective cohort study. J Ren Nutr. 2018;28:45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clarke AL, Jhamb M, Bennett PN. Barriers and facilitators for engagement and implementation of exercise in end-stage kidney disease: future theory-based interventions using the behavior change wheel. Semin Dial. 2019;32:308–319. [DOI] [PubMed] [Google Scholar]
- 8.Wenger NK, Froelicher ES, Smith LK, et al. Cardiac rehabilitation as secondary prevention. Agency for health care policy and research and national heart, lung, and blood Institute. Clin Pract Guidel Quick Ref Guide Clin. 1995;17:1–23. [PubMed] [Google Scholar]
- 9.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation Sci. 2011;6:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilund K, Thompson S, Bennett PN. A global approach to increasing physical activity and exercise in kidney care: the international society of renal nutrition and metabolism global renal exercise group. J Ren Nutr. 2019;29:467–470. [DOI] [PubMed] [Google Scholar]
- 11.Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126–131. [PMC free article] [PubMed] [Google Scholar]
- 12.Bayoumi MM, Al Wakeel JS. Impacts of exercise programs on hemodialysis patients’ quality of life and physical fitness. Qual Prim Care. 2015;23. [Google Scholar]
- 13.Toussaint ND, McMahon LP, Dowling G, et al. Introduction of renal key performance indicators associated with increased uptake of peritoneal dialysis in a publicly funded health service. Peritoneal Dial Int. 2017;37:198–204. [DOI] [PubMed] [Google Scholar]
- 14.Ju A, Scholes-Robertson N, Johnson DW, et al. Patient-led identification and prioritization of exercise interventions for fatigue on dialysis: a workshop report. Clin Kidney J. 2020;14:831–839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ju A, Unruh M, Davison S, et al. Establishing a core outcome measure for fatigue in patients on hemodialysis: a standardized outcomes in nephrology-hemodialysis (SONG-HD) consensus workshop report. Am J kidney Dis. 2018;72:104–112. [DOI] [PubMed] [Google Scholar]
- 16.De Vecchi AF, Dratwa M, Wiedemann ME. Healthcare systems and end-stage renal disease (ESRD) therapies—an international review: costs and reimbursement/funding of ESRD therapies. Nephrol Dial Transplant. 1999;14(suppl_6):31–41. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Medicare Medicaid Services. Medicare program; end-stage renal disease prospective payment system, and quality incentive program. Final rule. Fed Regist. 2015;80:68967. [PubMed] [Google Scholar]
- 18.Sturgill DA, Bal N, Nagavally S, Wolfgram DF. The relationship between dialysis metrics and patient-reported cognition, fatigue, and physical function. Kidney Dis. 2020;6:364–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weiner D, Watnick S. The ESRD quality incentive program—can we bridge the chasm? J Am Soc Nephrol. 2017;28:1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Didsbury M, McGee RG, Tong A, et al. Exercise training in solid organ transplant recipients: a systematic review and meta-analysis. Transplantation. 2013;95:679–687. [DOI] [PubMed] [Google Scholar]
- 21.Zelle DM, Klaassen G, van Adrichem E, Bakker SJL, Corpeleijn E, Navis G. Physical inactivity: a risk factor and target for intervention in renal care. Nat Rev Nephrol. 2017;13:152–168. [DOI] [PubMed] [Google Scholar]
- 22.Nixon AC, Bampouras TM, Pendleton N, Woywodt A, Mitra S, Dhaygude A. Frailty and chronic kidney disease: current evidence and continuing uncertainties. Clin Kidney J. 2018;11:236–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Medicaid Services. National Coverage Determination (NCD) for Cardiac Rehabilitation Programs for Chronic Heart Failure (20.10.1). U.S. Centers for Medicare & Medicaid Services. https://www.cms.gov/medicare-coverage-database/details/ncd-details.aspx?NCDId=359&ncdver=1&MCDIndexType=2&mcdtypename=Potential+National+Coverage+Determination+(NCD)+Topics&bc=AAAAIAAAAAAA&. Accessed February 12, 2020. [Google Scholar]
- 24.Booth FW, Gordon SE, Carlson CJ, Hamilton MT. Waging war on modern chronic diseases: primary prevention through exercise biology. J Appl Physiol. 2000;88:774–787. [DOI] [PubMed] [Google Scholar]
- 25.Taryana AA, Krishnasamy R, Bohm C, et al. Physical activity for people with chronic kidney disease: an international survey of nephrologist practice patterns and research priorities. BMJ Open. 2019;9:e032322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Turk-Adawi K, Sarrafzadegan N, Grace SL. Global availability of cardiac rehabilitation. Nat Rev Cardiol. 2014;11:586–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moscovice IS, Casey MM, Wu Z. Disparities in geographic access to hospital outpatient pulmonary rehabilitation programs in the United States. Chest. 2019;156:308–315. [DOI] [PubMed] [Google Scholar]
- 28.Eichstaedt CA, Benjamin N, Xanthouli P, Marra AM, Grunig E. The role of rehabilitation in patients with pulmonary arterial hypertension. Curr Opin Pulm Med. 2019;25:398–404. [DOI] [PubMed] [Google Scholar]
- 29.Manns B, Hemmelgarn B, Lillie E, et al. Setting research priorities for patients on or nearing dialysis. Clin J Am Soc Nephrol. 2014;9:1813–1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Delgado C, Johansen KL. Deficient counseling on physical activity among nephrologists. Nephron Clin Pract. 2010;116:c330–c336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moorman D, Suri R, Hiremath S, et al. Benefits and barriers to and desired outcomes with exercise in patients with ESKD. Clin J Am Soc Nephrol. 2019;14:268–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Delgado C, Johansen KL. Barriers to exercise participation among dialysis patients. Nephrol Dial Transplant. 2012;27:1152–1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johansen KL, Sakkas GK, Doyle J, Shubert T, Dudley RA. Exercise counseling practices among nephrologists caring for patients on dialysis. Am J Kidney Dis. 2003;41:171–178. [DOI] [PubMed] [Google Scholar]
- 34.Bennett PN, Peter J, Wang W, Street M. Attitudes of nephrology nurses toward patient exercise during hemodialysis. Nephrol Nurs J. 2016;43:331–337. [PubMed] [Google Scholar]
- 35.Bennett PN, Dewald G. Patient care technicians managing hemodialysis central venous catheter care: pro and con. Nephrol Nurs J. 2017;44:449–454. [PubMed] [Google Scholar]
- 36.Bennett PN. Satellite dialysis nursing: technology, caring and power. J Adv Nurs. 2011;67:149–157. [DOI] [PubMed] [Google Scholar]
- 37.Bennett PN, Capdarest-Arest N, Parker K. The physical deterioration of dialysis patients-Ignored, ill-reported, and ill-treated. Semin Dial. 2017;30:409–412. [DOI] [PubMed] [Google Scholar]
- 38.Wilund KR, Jeong JH, Greenwood SA. Addressing myths about exercise in hemodialysis patients. Semin Dial. 2019;32:297–302. [DOI] [PubMed] [Google Scholar]
- 39.Heiwe S, Jacobson SH. Exercise training for adults with chronic kidney disease. Cochrane database Syst Rev. 2011;10:CD003236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kidney Health Canada. Physical Activity. Kidney Health Canada. https://www.kidneyhealth.ca/living-with-kidney-disease/fitness-wellness/. Accessed February 12, 2020. [Google Scholar]
- 41.Parker K, Zhang X, Lewin A, MacRae JM. The association between intradialytic exercise and hospital usage among hemodialysis patients. Appl Physiol Nutr Metab. 2015;40:371–378. [DOI] [PubMed] [Google Scholar]
- 42.Graham-Brown MP, March DS, Churchward DR, et al. Design and methods of CYCLE-HD: improving cardiovascular health in patients with end stage renal disease using a structured programme of exercise: a randomised control trial. BMC Nephrol. 2016;17:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hemmelgarn BR, Pannu N, Ahmed SB, et al. Determining the research priorities for patients with chronic kidney disease not on dialysis. Nephrol Dial Transplant. 2017;32:847–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Levin A, Adams E, Barrett BJ, et al. Canadians seeking solutions and innovations to overcome chronic kidney disease (Can-SOLVE CKD): Form and function. Can J kidney Health Dis. 2018;5. 2054358117749530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Clarkson MJ, Bennett PN, Fraser SF, Warmington SA. Exercise interventions for improving objective physical function in patients with end-stage kidney disease on dialysis: a systematic review and meta-analysis. Am J Physiol Ren Physiol. 2019;316:F856–F872. [DOI] [PubMed] [Google Scholar]
- 46.Greenwood SA, Koufaki P, Rush R, Macdougall IC, Mercer TH. Exercise counselling practices for patients with chronic kidney disease in the UK: a renal multidisciplinary team perspective. Nephron Clin Pract. 2014;128:67–72. [DOI] [PubMed] [Google Scholar]
- 47.Painter PL. Exercise: A Guide for People on Dialysis. Medical Media Associates; 1995. [Google Scholar]
- 48.Bennett P. Resource packs to facilitate exercise on dialysis. Aust Nurs Midwifery J. 2015;23:39. [PubMed] [Google Scholar]
- 49.Cooney J, Macdonald J, Noyes J. My Health Professional Exercise Prescription Guide. Bangor, UK: University of Bangor; 2019. [Google Scholar]
- 50.Mulroe J, Collins C, Cuddihy J, et al. Making Every Contact Count (MECC)–Chronic disease risk factor and brief advice recording. Int J Integrated Care. 2017;17. [Google Scholar]
- 51.Koufaki P, Greenwood S, Painter P, Mercer T. The BASES expert statement on exercise therapy for people with chronic kidney disease. J Sports Sci. 2015;33:1902–1907. [DOI] [PubMed] [Google Scholar]
- 52.Abdulnassir L, Egas-Kitchener S, Whibley D, Fynmore T, Jones GD. Captivating a captive audience: a quality improvement project increasing participation in intradialytic exercise across five renal dialysis units. Clin Kidney J. 2017;10:516–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Capitanini A, Lange S, D’Alessandro C, et al. Dialysis exercise team: the way to sustain exercise programs in hemodialysis patients. Kidney Blood Press Res. 2014;39:129–133. [DOI] [PubMed] [Google Scholar]
- 54.Johansen KL. The Frail dialysis population: a growing burden for the dialysis community. Blood Purif. 2015;40:288–292. [DOI] [PubMed] [Google Scholar]
- 55.Thompson S, Tonelli M, Klarenbach S, Molzahn A. A qualitative study to explore patient and staff perceptions of intradialytic exercise. Clin J Am Soc Nephrol. 2016;11:1024–1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bennett PN, Daly RM, Fraser SF, et al. The impact of an exercise physiologist coordinated resistance exercise program on the physical function of people receiving hemodialysis: a stepped wedge randomised control study. BMC Nephrol. 2013;14:204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Milam RH. Exercise guidelines for chronic kidney disease patients. J Ren Nutr. 2016;26:e23–e25. [DOI] [PubMed] [Google Scholar]
- 58.Roche WR. Healthcare Management. UK: Oxford University Press; 2018. [Google Scholar]
- 59.Gordon EJ, Prohaska T, Siminoff LA, Minich PJ, Sehgal AR. Needed: tailored exercise regimens for kidney transplant recipients. Am J Kidney Dis. 2005;45:769–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yamagata K, Hoshino J, Sugiyama H, et al. Clinical practice guideline for renal rehabilitation: systematic reviews and recommendations of exercise therapies in patients with kidney diseases. Ren Replace Ther. 2019;5:4. [Google Scholar]
- 61.Japanese Society of Renal Rehabilitation. Guideline for Renal Rehabilitation, Renal Replacement Therapy. Tokyo: Nankodo Inc.; 2018. [Google Scholar]
- 62.Ashby D, Borman N, Burton J, et al. Renal association clinical practice guideline on Haemodialysis. BMC Nephrol. 2019;20:379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.National Kidney Foundation. KDOQI clinical practice guidelines and clinical practice recommendations for Diabetes and chronic kidney disease. Am J kidney Dis. 2007;49(2 Suppl. 2):S1–S180. [DOI] [PubMed] [Google Scholar]
- 64.National Kidney Foundation. KDOQI clinical practice guideline for Diabetes and CKD: 2012 update. Am J kidney Dis. 2012;60:850–886. [DOI] [PubMed] [Google Scholar]
- 65.Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 2013;3:5–14. [DOI] [PubMed] [Google Scholar]
- 66.Jefferson NM. A patient’s view on exercise and ESKD. Clin J Am Soc Nephrol. 2019;14:171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Reid RD, Morrin LI, Pipe AL, et al. Determinants of physical activity after hospitalization for coronary artery disease: the Tracking Exercise after Cardiac Hospitalization (TEACH) Study. Eur J Cardiovasc Prev Rehabil. 2006;13:529–537. [DOI] [PubMed] [Google Scholar]
- 68.Kontos PC, Miller K-L, Brooks D, et al. Factors influencing exercise participation by older adults requiring chronic hemodialysis: a qualitative study. Int Urol Nephrol. 2007;39:1303–1311. [DOI] [PubMed] [Google Scholar]
- 69.Débora Pacheco B, Guimarães Caetano LC, Amorim Samora G, Sant’Ana R, Fuscaldi Teixeira-Salmela L, Scianni AA. Perceived barriers to exercise reported by individuals with stroke, who are able to walk in the community. Disabil Rehabil. 2019;43:331–337. [DOI] [PubMed] [Google Scholar]
- 70.Giuliano C, Cowie K, Saliba J, et al. Barriers to exercise rehabilitation in the older adult with heart failure. Heart Lung Circ. 2015;24:S450. [Google Scholar]
- 71.Bennett P, Hussein W, Matthews K, et al. An exercise program for peritoneal dialysis patients in the United States: a feasibility study. Kidney Med. 2020;2:267–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Parker K. Establishing a successful intradialytic exercise program: part 2 of 2. CANNT J. 2012;22:38–40. [PubMed] [Google Scholar]
- 73.Kohzuki M. Renal rehabilitation: present and future perspectives. In: Suzuki H, ed Tokyo: Intech; 2013:743–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bennett PN, Thompson S, Wilund KR. An introduction to exercise and physical activity in dialysis patients: preventing the unacceptable journey to physical dysfunction. Semin Dial. 2019;32:281–282. [DOI] [PubMed] [Google Scholar]


