Abstract
Introduction and importance
Spinal epidural hematoma (SEH) is an uncommon condition that can result in severe neurological problems and needs to be treated as soon as possible. The incidence of traumatic SEH is 0.5 %–1.7 %, but increases to 9 % in patients with rheumatic diseases. Surgical treatment options include open surgery and minimally invasive surgery. We reported a post-traumatic SEH at T12/L1 level combined with L5 nerve injury and treated by UBE technique. To our knowledge, there was no reported cases like this.
Case presentation
A 38-year-old man with left leg weakness and severe back pain after fell down while cycling. Physical examination suggested left hip abduction was 2/5 strength, left dorsiflexion of hallux dorsal extension was 0/5 strength and the left ankle dorsiflexion was 2/5 strength. Magnetic resonance images (MRI) of lumbar spine showed a two-leveled hematoma extending from T12 to L1. After 1 year of surgery, the patient's symptoms had largely disappeared and he was able to perform daily activities independently.
Clinical discussion
An epidural hematoma at the L1 level is can cause symptoms of the L5 nerve root alone, which may be due to anatomical reasons. Complete removal of the epidural hematoma is necessary to restore the function of the nerve. We report a case of successful removal of an epidural hematoma using the UBE technique with good postoperative results.
Conclusions
The single nerve injury can occur with a thoracolumbar segmental hematoma, and UBE technology could be used to remove epidural hematoma.
Keywords: Case report, Unilateral bi-portal endoscopy, Traumatic spinal epidural hematoma, Minimally invasive surgery
Highlights
-
•
This paper reported a rare case of post-traumatic epidural hematoma combined with L5 unilateral nerve injury;
-
•
The patient was treated by unilateral bi-portal endoscopy;
-
•
After 1 year of postoperative follow-up, the patient's symptoms had largely disappeared.
1. Introduction
Spinal epidural hematoma (SEH) is an uncommon condition that causes spinal cord compression, and it is estimated to occur in 0.1 patients per 100,000 patients per year [1]. It's related to minor trauma, chiropractic manipulation, rheumatoid arthritis, and cervical spondylitis [[2], [3], [4]]. SEH can compress the spinal cord and produce a range of symptoms, such as disturbances of sensory, motor, bladder and bowel.
Traumatic SEH (TSEH) may appear with traumatic spine injuries, the incidence of TSEH is approximately 20–30 % of all SEHs [6]. The symptoms of SHE is acute back pain, accompanied by paralysis or loss of sensory function in one or both legs, and the disease progresses rapidly. CT and MRI are helpful in the diagnosis of SHE, which can provide the extend of the hematoma and the severity of the nerve compression. Surgical treatment is often required for patients with symptomatic SEH. If the patient is treated promptly, the prognosis is often satisfactory; if not, it can result in irreversible nerve damage.
Unilateral biportal endoscopic discectomy (UBE) is an emerging minimally invasive spinal procedure. Of note, the technique has two separate channels for the endoscope, which provides a clear and expanded surgical field, improving surgical flexibility and helping surgeons perform precise and extensive decompression.
This case report is in line with the SCARE criteria. In the present study, we discussed a case who was admitted to our hospital with progressive neurological deficits after traffic accident. We treated him with the UBE technique and used percutaneous pedicle screw fixation to fix his spinal fracture. To the best of our knowledge, this is the first reported case of post-traumatic SEH at the T12/L1 level combined with L5 nerve root injury, which was treated using the UBE technique.
2. Case presentation
This case report is in line with the SCARE criteria [5]. A 38-year-old man presented to hospital with left leg weakness and severe back pain. He fell down while cycling and came to the hospital after 3 days of conservative treatment at home.
2.1. Examination
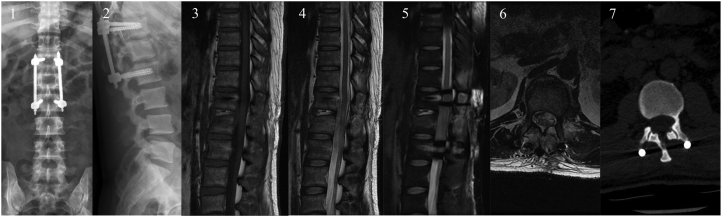
The physical examination suggested that the left lumbar 5 nerve may have been injured. The main manifestation was that the strength of left hip abduction muscle was only 2/5, the strength of left dorsiflexion of hallus dorsal extension was 0/5, and the strength of left ankle dorsiflexion was only 2/5, decreased sensation in the anterolateral aspect of the left calf and dorsum of the foot. The strength of right lower limb was 5/5 and the sensation of the right lower extremity was normal. Bowel/bladder function was normal. Bilateral tendon reflexes were elicited symmetrically. Laboratory studies, including platelet count, prothrombin time, and partial thromboplastin time, were all within normal limits. L1 vertebral compression can be seen on X-ray. Magnetic resonance images (MRI) of lumbar spine showed a two-level hematoma extending from T12 to L1 doral epidural space, causing the L1 spinal cord compression and edema. All pre-operative imaging pictures are shown in Fig. 1.
Fig. 1.
Pre-operative images; (1) (2) pre-operative X-ray front and side views; (3) (4) (5) (6) preoperative MRI images; the arrow shows the hematoma.
2.2. Operation technique
We recommended an urgent surgical evacuation because of spinal cord compression. The entire procedure consists of unilateral biportal endoscopic decompressive laminectomy, hematoma removal and percutaneous pedicle screw fixation. Intraoperative pictures were shown in Fig. 2.
Fig. 2.
Intraoperative images; (1) preoperative positioning markers; (2) intraoperative positioning; (3) microscopic image before hematoma cleanup; (4) (5) frontal and lateral views under fluoroscopy at the end of nail placement; (6) microscopic image after hematoma cleanup.
The procedure was performed in the prone position. Level confirmation was conducted under C-arm prior to operation. Two portals were used to securing the working space, each portal was approximately 1 cm in size. One was the viewing portal, the other was the working portal. The portals were positioned below the left pedicle of lamina and separated by 1 cm. A continuous irrigation system was connected and controlled to set a pressure of approximately 40 mmHg. Radiofrequency catheter was used to clean the soft tissue on the surface of the left side of the interlaminar space of T12-L1. Abrasive drill and Kerrison punch were used to achieve a laminotomy. Partial laminectomy was performed to expose the ligament flavum sufficiently before flavectomy. Intraoperative visualization: hematoma was visible in the spinal canal. Used nerve probe hook to remove the hematoma, hemostasis of the intradural radiofrequency blade tip to ensure no clear active bleeding or new hematoma formation.
The placement of the T12-L2 pedicle screw was then completed under C-arm fluoroscopy.
2.3. Postoperative course
After the operation, the patient's symptoms of nerve damage were initially relieved, left hip abduction was 4/5 strength, left dorsiflexion of hallus dorsal extension was 3/5 strength and the left ankle dorsiflexion was 3/5 strength. MRI showed that the epidural hematoma was significantly smaller than before the operation (Fig. 3), and the patient was able to walk with a walker after the operation two weeks. At 3 months post-operative follow-up, the patient was able to perform daily activities independently, the MRI showed that the epidural hematoma was mostly gone (Fig. 4). At 1 year post-operative follow-up, the patient had achieved significant relief of lower limb symptoms and was able to perform daily activities independently, left hip abduction was 5/5 strength, left dorsiflexion of hallus dorsal extension was 5/5 strength and the left ankle dorsiflexion was 5/5 strength, the MRI showed that the epidural hematoma had almost disappeared (Fig. 5).
Fig. 3.
Postoperative images; (1) (2) frontal and lateral views of X-ray; (3) (4) (5) (6) the postoperative MRI image shows a significant reduction in the hematoma compared to the preoperative period. (7) CT showing the manifestations after decompression of the spinal canal.
Fig. 4.
MRI images at 3-month postoperative follow-up.
Fig. 5.
MRI images at 1-year postoperative follow-up, the visible hematoma largely disappeared.
3. Discussion
SEH is defined as a blood collection in the outermost layer of the spinal canal. It can cause nerve root and/or spinal cord compression and may result in neurological sequelae. The spinal epidural hematomas are rare in clinical findings, accounting only for 0.3–0.9 % of all lesions, occupying spinal canal space reported [2]. And the incidence of TSEH was reported to be only 0.5 %–1.7 % of all spinal injuries [7].
The clinical presentation of TSEH is similar to that of herniated discs and intravertebral canal tumors. They both cause symptoms of nerve root or spinal cord compression. The symptoms of herniated discs and intravertebral canal tumors tend to be long-term and chronic, while SHE is generally acute and rapidly progressive. The indications for surgery are progressively neurological symptoms. The diagnosis of TSEH relies on computed tomography scan or MRI [8]. MRI can provide information on the segmentation and extent of the hematoma and can also show the extent of spinal cord compression, which can provide guidance for surgical treatment. MRI is instructive in the diagnosis of new spinal fractures. In this case, the patient had progressively weakness of left limb and combined lumbar vertebral fracture. So we arranged for the patient to be treated surgically as soon as possible. We chose the UBE technique because, as a minimally invasive procedure, it is less invasive to the patient and its effectiveness in treating SHE has been previously reported in the literature.
Traditional open decompression surgery had some disadvantages such as heavy muscle damage, long operation time, large intraoperative bleeding, and high incidence of postoperative complications [9]. The UBE technique, an emerging minimally invasive spinal technique, have been shown to result in less structural damage, blood loss and operation time [10]. Moreover, the UBE can provide a good visualization of the lesion, which increases the accuracy of intraoperative manipulation.
Compared with traditional open internal fixation surgery, percutaneous pedicle screw fixation has the advantages of rapid postoperative pain relief, less trauma and faster recovery [11]. In this case, the patient had a spinal epidural hematoma combined with a spinal fracture. The surgeon chose to perform a minimally invasive procedure on the patient based on his years of experience. The postoperative MRI showed a significant reduction in the epidural hematoma and relief of the patient's symptoms.
Most of the current literature reports on the treatment of spontaneous epidural hematomas and epidural hematomas after spinal surgery, and rear literature reports on the surgical treatment of TSEH. Wu et al. [12] reported a 26-year-old man was diagnosed as L4-5 SEH and treated with a full endoscopic transforaminal approach, the radicular symptom disappeared soon after surgery. A 63-year-old man with three-leveled hematoma was reported by Kim, the patient was treated by biportal endoscopic spine surgery and could present normal activity of daily living after 3 month after surgery [13]. In present study, we reported a patient with T12-L1 TSEH, however, it showed symptoms of L5 nerve injury. To our knowledge, this case is the first reported of TSEH combined with nerve injury treated by UBE technology.
The inferior distal spinal cone is located between T12-L1 and is surrounded by the cauda equina nerve [14], and compression here often results in a mixed injury. The cone is relatively fixed and poorly cushioned against external forces, while the cauda equina is more strongly cushioned against external forces. Injuries to the cone alone are common, injuries to the cauda equina alone are rare, while injuries to a single nerve are even rarer. This case compresses the L5 nerve in the dural sac at the level of T12-L1, which is part of the cauda equina.
Our patient's recovered motor power at 1 year after surgery, enabling his to walk independently, and his symptoms of nerve damage mostly disappeared. And he was able to carry out his daily work and life independently.
The advantages of biportal endoscopic spine surgery can be presented in three ways. Firstly, UBE does not require novel surgical equipment, the procedure can be performed using conventional spine surgical instruments. Secondly, with two channels, the movement of the operating instruments is not restricted and the endoscopic view is close to that of open surgery [15]. Thirdly, the UBE technique prevents the destruction of the normal spine anatomy [16]. However, UBE technology also has some disadvantages. In addition, the amount of hidden blood loss in patients undergoing UBE surgery may be significant [17].
We reported this case with the aim of sharing this rare case, which single nerve injury can occur with a thoracolumbar segmental hematoma, and UBE technology could be used to remove epidural hematoma. The present study suggests that the biportal endoscopic spine surgery approach provides safe access to TSEH. And the procedure allows for adequate drainage of the hematoma and the patient recovered well after surgery. However, large-scale studies are needed to validate our results. The efficacy of treatment should be demonstrated using comparative studies and long-term follow-up.
4. Conclusions
Epidural hematomas in the thoracolumbar segmental can cause a single nerve root injury as the main symptom. UBE, as As an emerging minimally invasive approach to the spine, could be used to remove epidural hematoma.
Ethical approval
This case report was approved by the Ethics Committee of Beijing Friendship Hospital, Capital Medical University (BHF20220602013).
Funding
Not applicable.
CRediT authorship contribution statement
HM and QF performed the surgical interventions and designed the study. HXZ, JSL and HNT performed the literature search and data collection. HXZ was major contributors in writing the manuscript. HNT, JSL, HM, YY contributed to the surgical technical support. All authors read and approved the final manuscript.
Guarantor
Qi Fei.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Declaration of competing interest
The authors declare that they have no competing interests.
Contributor Information
Qi Fei, Email: spinefei@126.com.
Hai Meng, Email: menghaione@aliyun.com.
References
- 1.Holtas S., Heiling M., Lonntoft M. Spontaneous spinal epidural hematoma: findings at MR imaging and clinical correlation. Radiology. 1996;199(2):409–413. doi: 10.1148/radiology.199.2.8668786. May. [DOI] [PubMed] [Google Scholar]
- 2.Sarubbo S., Garofao F., Maida G., Fainardi E., Granieri E., Cavallo M. Spontaneous and idiopathic chronic spinal epidural hematoma: two case reports and review of the literature. Eur. Spine J. 2009;18(11):1555–1561. doi: 10.1007/s00586-009-1175-6. Nov. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gustafsson H., Rutberrg H., Bengtsson M. Spinal haematoma following epidural analgesia. Report of a patient with ankylosing spondylitis and a bleeding diathesis. Anaesthesia. 1988;43(3):220–222. Mar. [PubMed] [Google Scholar]
- 4.Jea A., Moza K., Levi A.D., Vanni S. Spontaneous spinal epidural hematoma during pregnancy: case report and literature review. Neurosurgery. 2005;56(5) May. E1156; discussion E1156. [PubMed] [Google Scholar]
- 5.Agha R.A., Franchi T., Sohrab C., Mathew G., Kirwan A., Thomas A., et al. The SCARE 2020 guideline: updating consensus Surgical Case Report (SCARE) guidelines. Int. J. Surg. 2020;84(1):226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Domenicucci M., Mancarella C., Santoro G., Dugoni D.E., Ramieri A., Arezzo M.F., et al. Spinal epidural hematomas: personal experience and literature review of more than 1000 cases. J. Neurosurg. Spine. 2017;27(2):198–208. doi: 10.3171/2016.12.SPINE15475. Aug. [DOI] [PubMed] [Google Scholar]
- 7.Foo D., Rossier A.B. Post-traumatic spinal epidural hematoma. Neurosurgery. 1982;11(1 pt 1):25–32. doi: 10.1227/00006123-198207010-00006. Jul. [DOI] [PubMed] [Google Scholar]
- 8.Chang F.C., Lirng J.F., Luo C.B., Yen Y.S., Guo W.Y., Teng M.M.H., et al. Evaluation of clinical and MR findings for the prognosis of spinal epidural haematomas. Clin. Radiol. 2005;60(7):762–770. doi: 10.1016/j.crad.2004.12.008. Jul. [DOI] [PubMed] [Google Scholar]
- 9.Weinstein J.N., Tosteson T.D., Lurie J.D., Tosteson A., Blood E., Herkowitz H., et al. Surgical versus nonoperative treatment for lumbar spinal stenosis four-year results of the Spine Patient Outcomes Research Trial. Spine. 2010;35(14):1329–1338. doi: 10.1097/BRS.0b013e3181e0f04d. Jun 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eum J.H., Heo D.H., Son S.K., Park C.K. Percutaneous biportal endoscopic decompression for lumbar spinal stenosis: a technical note and preliminary clinical results. J. Neurosurg. Spine. 2016;24(4):602–607. doi: 10.3171/2015.7.SPINE15304. Apr. [DOI] [PubMed] [Google Scholar]
- 11.Dahdaleh N.S., Smith Z.A., Hitchon P.W. Percutaneous pedicle screw fixation for thoracolumbar fractures. Neurosurg. Clin. N. Am. 2014;25(2):337–346. doi: 10.1016/j.nec.2013.12.011. Apr. [DOI] [PubMed] [Google Scholar]
- 12.Wu Z.Y., Zhu Y.J., Chu L., Cheng C.Y., Chen C.M., Hui-Ting H. Full-endoscopic transforaminal approach for removal of a spontaneous spinal epidural hematoma. World Neurosurgery. 2017;98(883):e13–883.e20. doi: 10.1016/j.wneu.2016.07.086. Feb. [DOI] [PubMed] [Google Scholar]
- 13.Kim N., Jung S.B. Biportal endoscopic spine surgery in the treatment of multi-level spontaneous lumbar epidural hematoma: case report. J. Orthop. Sci. 2022;27(1):288–291. doi: 10.1016/j.jos.2019.03.010. Jan. [DOI] [PubMed] [Google Scholar]
- 14.Wall E.J., Conen M.S., Abitbol J.J., et al. Organization of intrathecal nerve roots at the level of the conus medullaris.[J/OL] The Journal of Bone & Joint Surgery. 1990;72(10):1495–1499. [PubMed] [Google Scholar]
- 15.Kim H.S., Choi S.H., Shim D.M., Lee I.S., Oh Y.K., Woo Y.H. Advantages of new endoscopic unilateral laminectomy for bilateral decompression (ULBD) over conventional microscopic ULBD. Clinics in Orthopedic Surgery. 2020;12(3):330–336. doi: 10.4055/cios19136. Sep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choi D.J., Kim J.E. Efficacy of biportal endoscopic spine surgery for lumbar spinal stenosis. Clinics in Orthopedic Surgery. 2019;11(1):82–88. doi: 10.4055/cios.2019.11.1.82. Mar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guo S., Tan H., Meng H., Li X., Su N., Yu L.J., et al. Risk factors for hidden blood loss in unilateral biportal endoscopic lumbar spine surgery. Frontiers in Surgery. 2022;15(9) doi: 10.3389/fsurg.2022.966197. Aug. 966197. [DOI] [PMC free article] [PubMed] [Google Scholar]