Abstract
Background
Chronic primary pelvic pain syndrome in men (CPPPSm) can be associated with urogenital pain, urinary symptoms, sexual dysfunction, and emotional disturbance. Its clinical heterogeneity and incompletely understood pathogenesis make it more difficult to treat. This article is intended to familiarize the reader with basic aspects of the manifestations, pathophysiology, diagnostic evaluation, differential diagnosis, and treatment of this condition.
Method
This article is based on relevant publications retrieved by a selective search of the literature, including the current guidelines of the European Association of Urology. The features of this disease pertaining to urology, psychosomatic medicine, and pain medicine are illuminated from an interdisciplinary perspective.
Results
Chronic pelvic pain appears to arise through a complex interaction of inflammatory, infectious, neurological, musculoskeletal, and psychosomatic factors. A comprehensive diagnostic work-up should be carried out to evaluate and exclude the numerous differential diagnoses. Treatment strategies are based on the clinical phenotype. Randomized controlled trials have shown that significant relief can be achieved with a variety of drugs and non-pharmacological treatments, selected according to the manifestations of the condition in the individual case. Attention must be paid to treatment-specific adverse effects.
Conclusion
The management of patients with CPPPSm should consist of a comprehensive differential diagnostic evaluation and an individually oriented treatment strategy.
Clinical features.
Chronic primary pelvic pain syndrome in men (CPPPSm) can be associated with urogenital pain, urinary symptoms, sexual dysfunction, and emotional disturbance.
Diagnostic evaluation.
The clinical heterogeneity and incompletely understood pathogenesis of this syndrome make it more difficult to treat. The initial presumptive diagnosis is often of prostatitis.
Chronic pelvic pain (i.e., pelvic pain that persists or recurs over a period of at least 3 months) takes many different forms and is treated by physicians from multiple specialties. If there is no specific pathological process, such as an infection, underlying the constellation of clinical manifestations, it is called a primary pain syndrome. In such cases, pain is not only the main symptom, it also plays a central role in the pathophysiology of the condition. In accordance with clinical diversity of chronic pelvic pain, the European Association of Urology (EAU) has divided the chronic primary pelvic pain syndrome (CPPPS) into subtypes depending on the system that is primarily affected—urologic, gastrointestinal, or musculoskeletal (1). Pelvic pain in men is often attributed to a problem in the prostate gland, in which case it is typically associated with urinary and sexual dysfunction and emotional disturbances such as anxiety, depressive manifestations, or catastrophizing. The initial presumptive diagnosis is often of prostatitis; if no infection is detected, or the symptoms persist longer than three months, the preferred term is “primary prostate pain syndrome” once the remaining elements of the differential diagnosis have been ruled out, or else, if the pain cannot be precisely localized, “chronic primary pelvic pain syndrome of the male” (CPPPSm) (1). These terms, however, have not been employed consistently in the literature to date, and thus no reliable data on the prevalence of CPPPSm are yet available. At any rate, it is known that a 2–10% of men suffer from symptoms of prostatitis (2, 3), while only 5–10% of these cases are due to a bacterial pathogen (4– 6), so it appears that many of these patients may, in fact, have CPPPSm. The condition leads not only to high costs for the health care system, but also to wider effects on society arising from these patients’ psychological and social impairment (emotional burden, stress, lessened social participation, impaired ability to work, etc.).
Both the recognition and the management of CPPPSm are a challenge because of inconsistencies in terminology, the clinical heterogeneity and incomplete pathophysiological understanding of the condition, and the lack, to date, of any clear treatment strategy. This CME article, based on a selective literature review and the current EAU guidelines, is intended to broaden the understanding of CPPPSm through a presentation of the diagnostic work-up and differential diagnostic of chronic pelvic pain in men and an outline of the main therapeutic strategies. Perspectives on CPPPSm from the points of view of psychosomatic medicine and pain medicine will be included as well. We focus on prostate-related complaints here, yet we prefer to use the term CPPPSm, as pelvic pain in men is generally imprecisely localized and associated with further manifestations at a variety of anatomic sites.
Prevalence.
No reliable data on the prevalence of CPPPSm are yet available. 2–10% of men suffer from symptoms of prostatitis (2, 3), while only 5–10% of these cases are due to a bacterial pathogen (4– 6); it appears that many of these patients may, in fact, have CPPPSm.
Learning objectives
This CME article is intended to provide readers with a knowledge of:
the main features of chronic primary pelvic pain syndrome in men
its differential diagnosis
its psychosomatic aspects
basic elements of the treatment strategy.
Clinical features and pathophysiology
The clinical features are of four main types:
urogenital pain
irritative and/or obstructive micturition symptoms (“lower urinary tract symptoms,” LUTS)
sexual dysfunction
emotional disturbance
The clinical manifestations of CPPPSm are of four main types: urogenital pain, irritative and/or obstructive micturition symptoms (“lower urinary tract symptoms,” LUTS), sexual dysfunction, and emotional disturbance (7). Pain often impairs these patients’ quality of life (8). The pathophysiology of CPPPSm is incompletely understood, but seems to involve multiple factors (9):
Inflammation: in a prospective study, leukocytes were found in prostate biopsies of only one-third of CPPPSm patients (10), while they were also found in prostatic secretions and urine samples from asymptomatic men (11). However, quantitative changes in pro- and anti-inflammatory cytokines were indeed found in patients with CPPPSm (12– 18). Moreover, the clinical manifestations are correlated with a variety of inflammatory proteins (IgM, C3, IL8, macrophage inflammatory protein 1α) (16, 19, 20).
Infection: Bacterial components have been inconsistently found in the prostatic secretions of men with CPPPSm (6, 21– 23), but men with CPPPSm are significantly more likely than control subjects to have had nonspecific urethritis (12% vs. 4%, p = 0.008). This implies a possible role for chronic post-infectious processes (24).
neural changes: Neuroimaging in men with CPPPSm has revealed microstructural changes in CNS regions associated with sensory perception and integration and with the modulation of pain (25, 26). A combination of neuropathic pain and neuroplasticity might amplify the perception of afferent stimuli and cause abnormal sensations as well as pain (27).
Pelvic floor dysfunction: like CPPPSm, pelvic floor dysfunction is associated with pain, sexual dysfunction, and anxiety; it could be a cause and/or an effect of CPPPSm (28, 29). A cohort study revealed pelvic floor muscle tenderness in patients with CPPPSm, but not in controls (30). Increased smooth muscle tone in the prostate and bladder might be a mechanism that promotes LUTS (31, 32).
mental/emotional aspects: A case-control study revealed that patients with CPPPSm were more than 2.5 times as likely as controls to suffer from mental illness, with an especially high frequency of anxiety/panic disorders (14.5% vs. 2.5%, p = 0.004) (24). Men who have experienced physical, emotional, or sexual abuse were found to be 1.7 to 3.3 times as likely to have CPPPSm (33). Non-traumatic stress has been found to cause mast cell degranulation and pelvic floor spasticity (34, 35), while inflammatory cytokines in seminal plasma are inversely correlated with support from a partner (15). Moreover, a supportive social environment seems to have improve the emotional state (36).
These complex pathophysiological factors must also be considered in the diagnostic and differential diagnostic evaluation. It is especially important to distinguish the changes described above that are related to CPPPSm from organ-specific pathology (such as acute infection, inflammation, or neuropathy). Pain due to an identifiable organic disease does not fall within the definition of CPPPSm.
Diagnostic evaluation
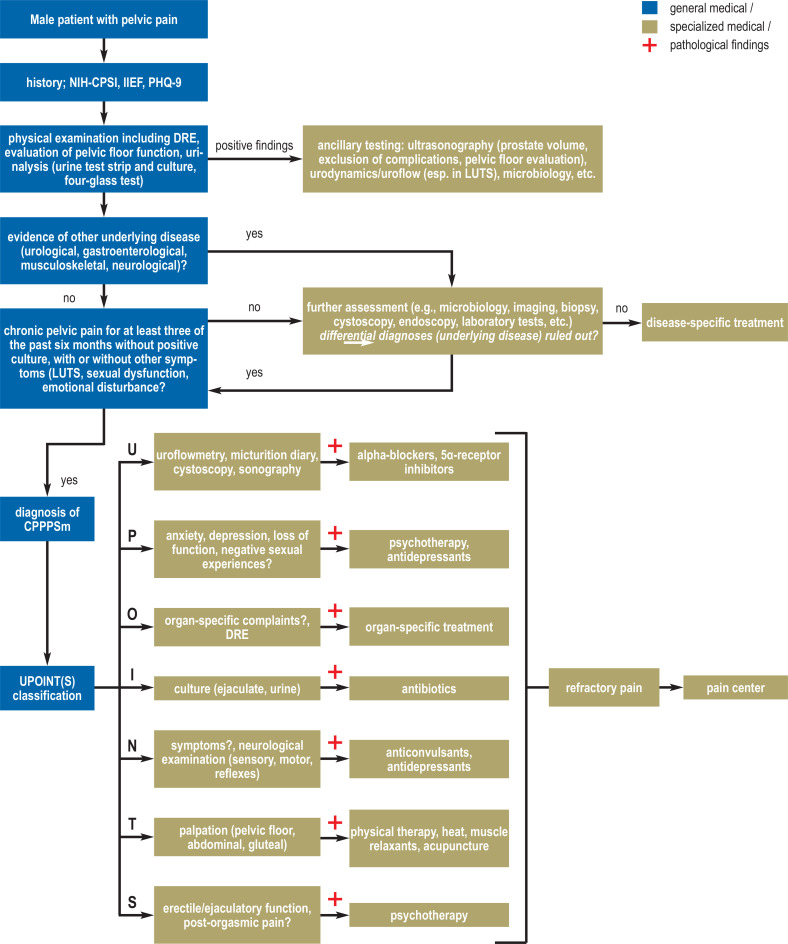
Every patient with CPPPSm should have an individually tailored diagnostic work-up, but certain basic steps should always be included (Figure). All persons involved in the management of patients with chronic pelvic pain should have adequate knowledge of peripheral and central pain mechanisms (1).
Figure.
Algorithms for chronic primary pelvic pain syndrome in men (CPPPSm)
DRE, digital rectal examination; IIEF, International Index of Erectile Function; LUTS, lower urinary tract symptoms; NIH-CPSI, National Institutes of Health Chronic Prostatitis Symptom Index; PHQ-9, Patient Health Questionnaire 9; UPOINT(S) classification, classification according to the following criteria: U = urinary, P = psychosocial, O = organ-specific, I = infectious, N = neurologic/systemic, T = pelvic muscle tenderness, S = sexual.
General practitioners are often the first physicians to be consulted by men with chronic pelvic pain; they face the task of taking a detailed history as to the nature and time course of the patient’s symptoms. Various questionnaires have been found useful for this purpose in the last few years: The National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI) assesses the symptoms of CPPPSm with nine questions about pain, LUTS, and the quality of life (8, 37). The International Prostate Symptom Score (IPSS) likewise assesses LUTS-related symptoms (38). The International Index of Erectile Function (IIEF) yields information about sexual function (39). A psychosocial assessment, e.g., with the Patient Health Questionnaire 9, documents negative cognitive, emotional, social, and behavioral effects (40). After history-taking, the physical examination should cover the abdomen, genitalia, and perineum, including a digital rectal examination (DRE). The latter can reveal prostatic abnormalities that are evident on palpation, as well as rectal and pelvic floor tenderness, sometimes with reproduction of the patient’s pelvic pain; it also enables the examiner to assess the contractility of the pelvic floor muscles.
Urinalysis with a 4-vial specimen according to Meares and Stamey (alternatively, a 2-vial specimen) is recommended to rule out bacterial prostatitis: in this test, a fractionated urine specimen (initial, midstream urine, expressed prostatic secretions (EPS), and urine after EPS expression) is analyzed both microbiologically and cytologically (e1, e2). 13.3% of patients with CPPPSm symptoms had positive cultures in a case-control study (e3). A neurological and musculoskeletal examination should be performed. Depending on symptoms, further studies such as urodynamics, imaging, or extended microbiological testing may be necessary.
By definition, the diagnosis of CPPPSm is confirmed when pelvic pain with or without accompanying complaints in other domains (LUTS, sexual dysfunction, emotional disturbance) has been present for at least three of the past six months and neither a urinary pathogen nor any other causal pathology can be demonstrated. If the symptoms are found to be due to a specific organ pathology, the diagnosis must be modified accordingly. For phenotypic classification, the so-called UPOINT(S) scheme has proven useful, which classically includes six domains:
U – urinary symptoms (i.e., symptoms relating to micturition)
P – psychosocial dysfunction
O – organ-specific findings
I – infection
N – neurological or systemic pathology
T – muscle tenderness (e4).
The UPOINT scheme has been extended to include the category of sexual dysfunction (S: e.g., erectile or ejaculatory dysfunction, post-orgasmic pain), but the added value of this has yet to be confirmed in studies (e5, e6). There is a specific evaluation for each domain (Figure). For domains with positive findings, there are corresponding recommendations for targeted treatment (e7, e8).
Initial steps in the diagnostic evaluation.
General practitioners are often the first physicians to be consulted by men with chronic pelvic pain; they face the task of taking a detailed history as to the nature and time course of the patient’s symptoms.
Available questionnaires for history-taking:
National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI)
International Prostate Symptom Score (IPSS)
International Index of Erectile Function (IIEF)
Patient Health Questionnaire 9
Differential diagnosis
CPPPSm is to be regarded as a diagnosis of exclusion. The differential diagnosis of chronic pelvic pain includes disorders that are dealt with by a wide range of medical specialties, and consideration must be given to these numerous disorders at an early stage of the diagnostic evaluation. An overview of important elements of the differential diagnosis is provided in the eTable.
eTable. The differential diagnosis of chronic primary pelvic pain syndrome in men (CPPPSm). This list of selected competing diagnoses is not intended to be complete.
| Differential diagnosis | Clinical differentiation from CPPPSm | Diagnostic assessment and confirmation of diagnosis | Treatment options |
| Urological | |||
| Bacterial prostatitis | acute: sudden onset; mainly irritative urinary symptoms; acute/recurrent urinary tract infections, frequent fever | pathological urine test strip findings, documentation of urinary pathogen (acute: urine culture, chronic: two- or four-glass test, urethral swab) |
acute: antibiotics chronic: antibiotics tailored to resistance pattern, supportive symptomatic treatment |
| Interstitial cystitis | chronic pollakisuria, suprapubic pain | cytoscopy with hydrodistention test: glomerulation and fissures of the bladder mucosa | multidisciplinary pain therapy |
| Benign prostatic syndrome | LUTS, more common in old age | ultrasonographic volumetry, IPSS, uroflowmetry, urodynamic testing when indicated | drugs (alpha-blockers, 5α-receptor inhibitors, PDE5 inhibitors), surgery (TURP, SP), interventional procedures |
| Urethritis | LUTS, urethral pain | IPSS, cystoscopy | pain therapy, conservative (often self-limiting) |
| Neurological | |||
| Pudendal neuralgia | intermittent severe intestinal and genital pain, esp. while sitting, sometimes with paresthesiae; can be secondary (fractures, surgery, tumor) | history, physical examination, imaging (MRI) | analgesics, co-analgesics, injection of local anesthetics or cortisone, transcutaneous electrical nerve stimulation, physiotherapy |
| Fibromyalgia | diffuse pain, esp. at muscle and tendon insertions; oversensitive tender points, sleep disturbance, exhaustion, accompanying functional and vegetative symptoms | clinical diagnosis | patient education; when indicated, psychosomatic consultation; pharmacotherapy when indicated for depressive symptoms |
| Gastroenterological | |||
| Chronic inflammatory bowel disease | stool changes (esp. diarrhea), non-gastrointestinal manifestations (arthritis, skin changes, oral changes, uveitis/episcleritis/iritis) | ileocoloscopy with stepwise biopsies, esophagogastroduodenoscopy when indicated | specific regimens of induction and maintenance therapy (mesalazine, steroids, azathioprine, biologic agents, other) |
| Irritable bowel syndrome | functional symptoms: stool changes, bloating, diffuse abdominal pain; often worse under emotional stress | clinical and laboratory exclusion of somatic causes, stool investigation for pathogenic organisms; when indicated, ultrasonography, DRE, colonoscopy | patient education; when indicated, autogenic training, probiotics, spasmolytic agents |
CPPPSm, chronic primary pelvic pain syndrome in men; DRE, digital rectal examination; IPSS, Internationaler Prostata-Symptomen-Score; LUTS, lower urinary tract symptoms; MRI, magnetic resonance imaging; SP, simple prostatectomy; TURP, transurethral resection of the prostate.
Psychosomatic aspects
A basic psychosomatic assessment should be performed early on, in parallel with the somatic diagnostic evaluation, if there is any clinical suspicion of a psychosomatic problem. This can be done, for example, with a seemingly tangential discussion during the physical examination, so that the examiner can note the presence of any core manifestations of depression (depressed mood, reduced drive, joylessness) or of anxiety, including avoiding certain situations (e.g., prolonged sitting, sexual activity) in order not to induce symptoms. The clinician may choose this opportunity to cautiously prepare the patient for the possibility of normal physical findings. It is also helpful to ask how the patient’s symptoms restrict his participation in everyday life, if at all, and to inquire about the patient’s own model of the disease: “In your own subjective view, what do you think is causing your symptoms?”
The symptoms should be proactively acknowledged as legitimate complaints, and the patient should be allowed as much time as possible to describe them; this will strengthen the working relationship between the physician and the patient. It is helpful, too, not just to tell the patient about the negative physical findings, but also to communicate plausible explanatory models for CPPPSm in his case. This will help the patient feel that his suffering is being taken seriously. Many patients will rapidly feel they have been classed as “hypochondriacs” if the doctor only tells them that the physical findings are all negative. The goal is a “both, and” attitude with equal emphasis on the somatic and mental/psychosomatic perspectives.
For patients who consult doctors frequently, the giving of appointments “when needed,” i.e., on demand, may reinforce the symptoms rather than diminish them. It is therefore recommended in the relevant guidelines that visits to the doctor should be regularly scheduled, e.g.., once every two to four weeks, with a clearly defined time for each appointment, even though the extent to which this might alleviate the patient’s symptoms cannot be reliably quantified (e9). If the patient shows signs of an anxiety disorder or a depressive disorder, targeted psychoactive drug treatment can be considered. Pain-modulating antidepressants such as amitriptyline and duloxetine are especially suitable. For duloxetine, an initial and maintenance dose of 60 mg per day is recommended. A starting amitriptyline dose of 25 mg per day may already alleviate the symptoms; if not, it can be slowly and incrementally raised to 100 mg per day until efficacy is achieved without dose-limiting side effects. Doses of up to 150 mg have also been given in clinical trials (e10, e11).
If this strategy does not alleviate or at least stabilize the symptoms, the next step is to seek accompanying psychosomatic, psychiatric, or psychotherapeutic treatment, ideally in collaboration with a specialist in psychosomatic medicine, psychiatry, or psychotherapy.
Phenotypic classification by the UPOINT(S) scheme.
U – urinary symptoms (i.e., symptoms relating to micturition),
P – psychosocial dysfunction, O – organ-specific findings,
I – infection, N – neurological or systemic pathology,
T – muscle tenderness, (S –sexual dysfunction).
Psychosomatic aspects must be considered.
A basic psychosomatic assessment should be performed. If the patient shows signs of an anxiety disorder or a depressive disorder, targeted psychoactive drug treatment can be given.
Treatment options
According to the findings of the Multidisciplinary Approach to the Study of Chronic Pelvic Pain (MAPP) Research Network, the symptoms of CPPPSm tend to remain stable (e12). As the manifestations vary from patient to patient, no single treatment is best for all; treatment strategies should be multidisciplinary and individually tailored. The EAU recommends close collaboration with colleagues from multiple medical specialties (1). In this section, we will mainly discuss the treatment of prostate-associated symptoms.
In two comprehensive systematic reviews (SR), Franco and colleagues from a Cochrane research network studied the efficacy of drugs and non-drug treatments (compared to placebo or other modalities) in alleviating the symptoms of CPPPSm, as measured with the NIH-CPSI. The endpoints studied included micturition-related symptoms, sexual dysfunction, anxiety/depression, and the quality of life, as well as adverse events (e13, e14). Only randomized and controlled trials (RCTs) were evaluated. The main findings of these Cochrane analyses will be outlined here (next paragraph) and supplemented wherever possible with further, more recently published data. Outcomes are presented in detail in the Table. There are more treatment options than can be presented in this brief review; further ones are discussed in the EAU guidelines (1) and elsewhere.
Table. Relevant findings of Cochrane analyses concerning drug and non-drug treatments for CPPPSm. Effects on symptoms as measured with the NIH-CPSI and relevant side effects are listed (e13, e14), without any implication of completeness. Further treatments and their effects are discussed in systematic reviews and in the current EAU guideline (1, e13, e14).
|
CPPPSm symptoms
(NIH-CPSI): follow-up: MD and RR [95% CI]; evidence level |
Side effects:
RR [95% CI]; evidence level |
Sexual dysfunction
(IIEF score) MD [95% CI]; evidence level |
Quality of life (SF-12 HSQ)
MD [95% CI]; evidence level |
Anxiety and depression
(Hospital Anxiety and Depression Scale) MD [95% CI]; evidence level |
| Treatments compared: alpha-blockers vs. placebo/no intervention | ||||
| 6 wk–6 mo MD −5.01 [−7.41; −2.61] very low |
6 wk–6 mo RR 1.6 [1.09; 2.34] low |
6–12 wk MD 0.26 [−1,.3; 1.65] moderate |
6–12 wk MD 0.15 [−2.63; 2.92] moderate |
12 wk MD −1.1 [−2.54; 0.4] low |
| Treatments compared: antibiotics vs. placebo | ||||
| 6 wk–3 mo MD −2.43 [−4.72;−0.15] low |
3 wk–6 mo RR 1.01 [0.66; 1.55] moderate |
6 wk MD 0.4 [−1.59; 2.39] moderate |
6 wk MD −3.9 [−7.94; 0.14] moderate |
– |
| Treatments compared: 5α-reductase inhibitors vs. placebo | ||||
| 6 mo MD −4.6 [−5.43; −3.77] moderate |
6–12 mo RR 0.87 [0.33; 2.3] low |
– | – | – |
| Treatments compared: anti-inflammatory drugs vs. placebo | ||||
| 6 wk–6 mo MD −2.5 [−3.74; –1.26]; low |
4 wk–6 mo RR 1.27 [0.81; 2.0]; low |
– | – | – |
| Treatments compared: phytotherapeutic drugs vs. placebo | ||||
| 1–3 mo MD −5.02 [−6.81; −3,23]; low |
1–3 mo RR 1.13 [0.54; 2.36]; low |
3 mo MD 3.5 [2.67; 4.33]; low |
– | – |
| Treatments compared: intraprostatic botulinum toxin A vs. sham;age > 50, NIH-CPSI baseline > 30 | ||||
| intraprostatic, 6 mo: MD −25.8 [−30.15; −21.45]; low |
1–6 mo: R.R 5.0 [0.25; 99.95]; low |
– | – | – |
| Treatments compared: TCM vs. placebo | ||||
| 2 wk−2 mo MD −3.13 [−4.99;–1.28]; low |
4–8 wk RR 1.34 [0.22; 8.02]; low |
2 wk MD + 0.27 [−1.17; 1.71]; moderate |
– | 2 wk MD –9.5 [−11.7; –7.3]; low |
| Treatments compared: acupuncture vs. sham | ||||
| 6–8 wk MD −5.79 [−7.32; −4.26]; moderate |
6–8 wk RR 1.33 [0.51; 3.46]; low |
6 wk MD −0.5 [−3.46; 2.46]; low |
– | – |
| Treatments compared: ESWT vs. sham/no ESWT | ||||
| 12 wk MD −6.18 [−7.46; −4.9]; high |
24 wk RR 1.22 [0.59; 2.51]; low |
12 wk MD 3.34 [2.68; 4.0]; moderate |
– | – |
| Treatments compared: lifestyle modification vs. no modification | ||||
| 3 mo reponse to treatment (drop in the NIH-CPSI score by at least 6 points) RR 3.9 [2.2; 6.92]; very low |
– | – | – | – |
| Treatments compared: exercise program vs. control (stretching, low activity) | ||||
| 6 wk MD −2.5 [−4.69; −0.31]; low |
– | – | – | 6W SAI-Y score MD −2.8 [−6.78; 1.18]; very low BDIS MD 0.5 [−1.33; 2.33] very low |
BDIS, Beck Depression Inventory Scale; CI, confidence interval; CPPPSm, chronic primary pelvic pain syndrome in men; EAU, European Association of Urology; ESWT, extracorporeal shock-wave therapy; IIEF, International Index of Erectile Function; mo, months; MD, mean difference; NIH-CPSI, National Institutes of Health Chronic Prostatitis Symptom Index; RR, relative risk; SF-12 HSQ, Short Form-12 Health Status Questionnaire; TCM, traditional Chinese medicine; wk, weeks; SAI-Y, State Anxiety Inventory-Y; –, no data available
The studies vary in design and in the inclusion criteria for patients with CPPPSm. This complicates the acquisition of reliable, representative data sets in systematic reviews and makes their findings harder to interpret. Careful patient selection is highly important in the evaluation of individual treatment options in clinical practice. Adherence to the UPOINT(S) system seems to promote the success of treatment (e7, e15-e17).
Drugs
Alpha-blockers are thought to alleviate LUTS mainly by relaxing smooth muscle in the prostate and bladder neck. Many studies of their use (with much variation in study design) have yielded only low- or very low-level evidence that alpha-blockers improve symptoms, while mildly increasing side effects (e13, e18-e40).
Further studies of uniform design will be needed to yield firmer conclusions about the efficacy and tolerability of alpha-blockers in patients with CPPPSm. In particular, studies should also include elderly men, who are at increased risk for adverse events (e78).
Even though the causation of CPPPSm is not primarily infectious, it is sometimes treated with antibiotics. These drugs may alleviate the symptoms of CPPPSm (mainly pain) to a small extent (e13, e41-e46). Fluoroquinolones are commonly used, but the risk of major adverse effects (hepatotoxicity, neurotoxicity, phototoxicity; cardiac, vascular, and metabolic side effects; tendinitis, cartilage damage. etc.) should always be kept in mind. In view of the increasing resistance to antibiotics and the lack of evidence to support their use in CPPPSm, they should not be given as initial treatment unless there is a well-founded indication (e47).
Other drugs that may mildly alleviate the symptoms of CPPPSm, without any relevant increase in side effects, are 5α-reductase inhibitors (e13, e48, e49), anti-inflammatory agents (e13, e24, e34, e44, e50-e55), and phytotherapeutic drugs (e13, e32, e56-e77).
Phytotherapeutic drugs may be advantageous for use in the elderly because of their more favorable side effect profile (e78).
Botulinum toxin A (BTA) injections lessen muscle tone by decreasing the presynaptic release of acetylcholine. BTA injected into the prostate is likely to relieve the symptoms of CPPPSm comprehensively, but episodes of hematuria may occur afterward (e13, e79-e82). A prospective, controlled trial in men with medically intractable, chronic pelvic pain revealed that BTA injections alleviate the symptoms effectively (NIH-CPSI at three months, –68.2%, –20.1 points; p < 0.0001) (e83).
Traditional Chinese medicine (TCM) also seems to alleviate CPPPSm symptoms in the short term (up to two months), presumably without a relevant increase in side effects, without improving sexual dysfunction. TCM also seems to alleviate symptoms of anxiety and depression (e13, e84-e93).
There is also evidence that CPPPSm symptoms can be alleviated by phosphodiesterase-5-inhibitors (PDE5-I; e13, e94-e100) and mepartricin (e13, e101, e102) without any increase in side effects. PDE 5-I improve sexual dysfunction; this is, indeed, their primary indication (e13).
It bears emphasizing that the evidence supporting all of the treatments just mentioned is inadequate. To assess the effect of drugs on CPPPSm-related symptoms, further RCTs are needed that have clearly defined inclusion and exclusion criteria and well-documented methodology, and in which the outcomes are measured with objectified criteria (for example, NIH-CPSI, IIEF, PHQ-9).
Pain-modulating antidepressants.
Pain-modulating antidepressants such as amitriptyline and duloxetine are especially suitable for use in patients with CPPPSm.
Drugs that can be used to treat this syndrome.
alpha-blockers
antibiotics (fluoroquinolones: beware of side effects)
5α-reductase inhibitors
botulinum toxin A
traditional Chinese medicine
Treatments other than drugs
Compared to placebo, acupuncture probably alleviates CPPPSm symptoms over the short term, with only mild side effects or none (e14, e103-e109). Tibial nerve stimulation may also yield a clinically relevant reduction in symptoms (e14, e110-e112). Perineal extracorporeal shock wave therapy (ESWT) can also help relieve symptoms, especially pain, and may improve sexual dysfunction (e14, e113-e118). A recent systematic review indicates, however, that symptom relief is probably not sustained over the long term (NIH-CPSI six months after ESWT and sham acupuncture: weighted mean difference 2.18; 95% confidence interval [–3.5; 7.86]) (e119). The efficacy of increased physical activity and certain lifestyle modifications (diet modification, sexual and physical activity, perineal protection) remains uncertain, but these treatments should be used because they are easily implemented in everyday life and tend to have beneficial effects in general (e14, e120, e121).
The treatments just mentioned vary widely in their invasiveness, practicality, and availability, and their risk-benefit profiles must be considered individually (e14). Except for acupuncture and ESWT, the supporting evidence is also generally weak. There is thus a need for further high-quality trials, just as there is regarding drugs for CPPPSm.
Non-drug treatment options.
acupuncture
tibial nerve stimulation
extracorporeal shock-wave therapy (ESWT)
lifestyle changes
Somatic and mental factors in CPPPSm
Interdisciplinary diagnostic evaluation and multimodal pain management
The understanding of chronic pelvic pain syndromes in men within the medical specialty of pain medicine has markedly improved over the past decade (e122). CPPPSm is a chronic visceral pain syndrome characterized by complex neural dysfunction at both peripheral and central levels. There is a mutual hypersensitization of organs served by the visceral pain conduction system (viscero-visceral cross-sensitization), and there is also an amplification of somatic pain that is mediated by systems enabling bidirectional communication between the viscera and the brain (viscerosomatic convergence mediated, e.g., by the autonomic nervous system and the hormonal and immunological axes). Further pathophysiological factors promote pain chronification, including persistent inflammatory changes, vascular mechanisms, and mechanical factors (e123-e125). The combined influence of all these phenomena may lead to the simultaneous presence of visceral pain disorders, myofascial imbalances, and visceral dysfunction, such as urinary urgency and constipation (e124– 127). Moreover, central sensitization with lessened pain inhibition may lead to the further spread of pain (e.g., concomitant fibromyalgia syndrome). Numerous studies have documented the psychological, psychiatric, and social components of CPPPSm in addition to its somatic component (e126, e128, e129).
In a German cross-sectional study, urogenital pain in men had a 1-week prevalence of ca. 10% and was associated with depressiveness and reduced quality of life (e130). This clearly implies that treating physicians should give due attention to psychological factors in their patients with CPPPSm.
These findings imply the need for a biopsychosocial model of CPPPSm. If CPPPSm fulfills the criteria for a “chronic pain disorder with somatic and psychological factors” (ICD-10 F45.41) (e131), then it is considered an independent nosological entity requiring interdisciplinary algesiological (i.e., pain-medical) evaluation, in other words, a standardized interdisciplinary diagnostic assessment for patients with chronic pain, code 1–910 according to the German Operations and Procedures Catalog (OPS) (e132, e133). This comprises pain-medical, psychological, and physiotherapeutic assessments aided by standardized questionnaires (German Pain Questionnaire with the module entitled “Visceral and Urogenital Pain for Men” (e134). In a concluding discussion, the team establishes the indication for interdisciplinary multimodal pain therapy (IMPT), which is the most suitable treatment for chronic pain syndromes.
IMST is characterized by an interdisciplinary collaboration in which the content and timing of the various interventions are coordinated. In a team-integrated approach, multimodal physical and psychotherapeutic exercises and training methods are implemented in small groups (e135, e136). Effective interdisciplinary pain management in CPPPSm requires an approach that is both mechanism-based and individually tailored (e17, e137-e139).
Overview.
Patients with CPPPSm should be managed with a comprehensive differential-diagnostic evaluation and an induvidually tailored treatment strategy.
Further Information on CME.
Participation in the CME certification program is possible only via the Internet: cme.aerzteblatt.de. The submission deadline is 23 July 2024. Submissions by letter, email, or fax cannot be considered.
The completion time for all newly started CME units is 12 months. The results can be accessed 4 weeks following the start of the CME unit. Please note the respective submission deadline at: cme.aerzteblatt.de
This article has been certified by the North Rhine Academy for Continuing Medical Education. CME points can be managed using the “uniform CME number” (einheitliche Fortbildungsnummer, EFN). The EFN must be stated during registration on www.aerzteblatt.de (“Mein DÄ”) or entered in “Meine Daten,” and consent must be given for results to be communicated. The 15-digit EFN can be found on the CME card (8027XXXXXXXXXXX).
Participation is possible at cme.aerzteblatt.de. The submission deadline is 23 July 2024.
Only one answer is possible per question. Please select the answer that is most appropriate.
Question 1
What constellation of symptoms characterizes the chronic primary pelvic pain syndrome in men?
perineal pain, restricted range of motion, dysuria, dizziness
urogenital pain, micturition symptoms (“lower urinary tract symptoms”), sexual dysfunction, emotional disturbance
abdominal pain, erectile dysfunction, restricted mobility, urinary retention
anal pruritus, dysuria, emotional disturbance, nocturia
lumbar pain, sciatica, restricted mobility, sexual dysfunction
Question 2
The pathophysiology of chronic primary pelvic pain syndrome in men (CPPPSm) has not been fully elucidated. According to currently available evidence, which of the following seem to play a role?
hormonal dysregulation, dietary habits, cardiovascular disease
mental illness, cancer, bacterial infection
inflammatory mediators, psychological aspects, spinal degeneration
sexually transmitted diseases, hormonal dysregulation, dietary habits
inflammatory mediators, psychological aspects, neural/neurological changes
Question 3
Mr. M., 48 years old, has been suffering from lower abdominal pain for 6 months, urinary frequency and urge sensation, and erection difficulties. No bacterial infection has been found to date. How should you continue with the diagnostic assessment?
meticulous history-taking and physical examination, including digital rectal examination
urodynamic study and uroflow
ultrasonography of kidneys and urinary bladder, with measurement of the prostate gland
urine PCA for streptococci
blood draw for PSA measurement
Question 4
Which questionnaire is most appropriate for assessing sexual function in patients with CPPPSm?
International Prostate Symptom Score (IPSS)
International Index of Erectile Function (IIEF)
Patient Health Questionnaire 9
Clinical Frailty Scale
Mini-Mental-Status-Test (MMST)
Question 5
The symptoms of CPPPSm can be assigned to the different domains of the so-called UPOINT(S) system. Which of the following assignments of letters and domains is correct?
U – abdominal pain
P – pathology
I – infection
N – nocturnal urination
T – trauma
Question 6
What percentage of men suffer from symptoms of prostatitis?
2–10%
4–20%
6–30%
8–40%
10–50%
Question 7
Early in the diagnostic work-up of chronic primary pelvic pain syndrome, the examiner should be alert for potential evidence of a depressive state. What are the core symptoms that should be particularly sought?
joylessness, reduced drive, depressed mood
apathy, headaches, sleep disturbances
aching limbs, sadness, anxiety
lethargy, fatigue, pain
delusions, daytime sleepiness, hyperactivity
Question 8
What substance class is appropriate for men with lower urinary tract symptoms (LUTS) who mainly suffer from voiding dysfunction?
selective serotonin reuptake inhibitors
macrolide antibiotics
anticonvulsants
alpha-blockers
vasopressin analogues
Question 9
Mr. F, 54, is under treatment for chronic primary pelvic pain syndrome. To date, he has received only alpha-blockers and physical therapy, but he now complains of new-onset erectile dysfunction. Which of the following therapeutic options should you consider first?
aripiprazole
acupuncture
psychotherapy
glucocorticoids
prostate massage
Question 10
Which approach is most appropriate for treating chronic pain syndromes such as the chronic primary pelvic pain syndrome?
interdisciplinary multimodal pain therapy (IMST)
use of low-potency opioids
various methods of acupuncture
extensive physiotherapy and psychotherapy
combination of deep brain stimulation and nonsteroidal anti-inflammatory drugs
► Participation is only possible online: cme.aerzteblatt.de
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement
KK has received research funding from the State of Baden-Württemberg Ministry of Social Affairs, Health, and Integration; further funding from the “Kirstin’s Way” Foundation to Support Cancer Medicine (Verein zur Förderung der Krebsmedizin e.V. „Kirstins Weg,“ Neuwied, Germany); author’s and editor’s fees from Kohlhammer publishers, Stuttgart; and a lecture honorarium from Riemser Pharma GmbH, Berlin.
CL has been a paid consultant for Falk Foundation, Lilly Pharma, Novartis, Novocure, and Roche and has received lecture honoraria from MedUpdate.
CG has been a paid consultant for for Astellas, Ipsen, Janssen, Steba, Bayer, Olympus, Medi-Tate, MSD, Astra-Zeneca, and Roche; has received reimbursement of meeting participation fees from Astellas, Olympus, and Recordati and of travel expenses Procept, Olympus, Medi-Tate, MSD, Astra-Zeneca, Roche, GSK, and Recordati; and has been paid for preparing continuing medical education events relating to the theme of this article by Astellas, Amgen, Ipsen, Janssen, Bayer, Takeda and Medac. He has also received financial support for conducting clinical trials on behalf of Astellas Pharma, Neotract, Medi-Tate, and Recordati, as well as funding for a research project that he initiated from Recordati and Medi-Tate.
AM has received research funding from the German Federal Ministry of Education and Research (BMBF); travel sponsorship from the German Society of Urology, Düsseldorf, and the European Society of Urology, Arnhem, NL; author’s fees from Walter de Gruyter publishers, Berlin, and Springer Science+Business Media, Germany; lecture honoraria from RichardWolf GmbH, Germany, and Boston Scientific, USA; and consultant’s fees from KLS Martin, Tuttlingen, Germany, Dornier medtech GmbH, Germany, Medi-Tate, Or Akiva, Israel, and b. Braun New Ventures GmbH, Germany.
JF states that she has no conflict of interest.
References
- 1.Fall M, Baranowski AP, Berghmans B, et al. EAU guidelines on chronic pelvic pain Edn Present EAU Annu Congr Amsterdam 2022. https://d56bochluxqnz.cloudfront.net/documents/full-guideline/EAU-Guidelines-on-Chronic-Pelvic-Pain-2022_2022-03-29-084111_kpbq.pdf (last accessed on 5 June 2023) 2022 ISBN 978-9. [Google Scholar]
- 2.Clemens JQ, Meenan RT, O’Keeffe Rosetti MC, et al. Prevalence of and risk factors for prostatitis: population based assessment using physician assigned diagnoses. J Urol. 2007;178:1333–1337. doi: 10.1016/j.juro.2007.05.140. [DOI] [PubMed] [Google Scholar]
- 3.Krieger JN, Lee SWH, Jeon J, Cheah PY, Liong ML, Riley DE. Epidemiology of prostatitis. Int J Antimicrob Agents. 2008;31(1):S85–S90. doi: 10.1016/j.ijantimicag.2007.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de la Rosette JJ, Hubregtse MR, Meuleman EJ, Stolk-Engelaar MV, Debruyne FM. Diagnosis and treatment of 409 patients with prostatitis syndromes. Urology. 1993;41:301–307. doi: 10.1016/0090-4295(93)90584-w. [DOI] [PubMed] [Google Scholar]
- 5.Krieger JN, Nyberg LJ, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999;282:236–237. doi: 10.1001/jama.282.3.236. [DOI] [PubMed] [Google Scholar]
- 6.Weidner W, Schiefer HG, Krauss H, Jantos C, Friedrich HJ, Altmannsberger M. Chronic prostatitis: a thorough search for etiologically involved microorganisms in 1,461 patients. Infection. 1991;19(3):S119–S125. doi: 10.1007/BF01643680. [DOI] [PubMed] [Google Scholar]
- 7.Rees J, Abrahams M, Doble A, Cooper A. Diagnosis and treatment of chronic bacterial prostatitis and chronic prostatitis/chronic pelvic pain syndrome: a consensus guideline. BJU Int. 2015;116:509–525. doi: 10.1111/bju.13101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wagenlehner FME, van Till JWO, Magri V, et al. National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI) symptom evaluation in multinational cohorts of patients with chronic prostatitis/chronic pelvic pain syndrome. Eur Urol. 2013;63:953–959. doi: 10.1016/j.eururo.2012.10.042. [DOI] [PubMed] [Google Scholar]
- 9.Pontari MA, Ruggieri MR. Mechanisms in prostatitis/chronic pelvic pain syndrome. J Urol. 2004;172:839–845. doi: 10.1097/01.ju.0000136002.76898.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.True LD, Berger RE, Rothman I, Ross SO, Krieger JN. Prostate histopathology and the chronic prostatitis/chronic pelvic pain syndrome: a prospective biopsy study. J Urol. 1999;162:2014–2018. doi: 10.1016/S0022-5347(05)68090-1. [DOI] [PubMed] [Google Scholar]
- 11.Nickel JC, Alexander RB, Schaeffer AJ, Landis JR, Knauss JS, Propert KJ. Leukocytes and bacteria in men with chronic prostatitis/chronic pelvic pain syndrome compared to asymptomatic controls. J Urol. 2003;170:818–822. doi: 10.1097/01.ju.0000082252.49374.e9. [DOI] [PubMed] [Google Scholar]
- 12.Alexander RB, Ponniah S, Hasday J, Hebel JR. Elevated levels of proinflammatory cytokines in the semen of patients with chronic prostatitis/chronic pelvic pain syndrome. Urology. 1998;52:744–749. doi: 10.1016/s0090-4295(98)00390-2. [DOI] [PubMed] [Google Scholar]
- 13.Orhan I, Onur R, Ilhan N, Ardiçoglu A. Seminal plasma cytokine levels in the diagnosis of chronic pelvic pain syndrome. Int J Urol Off J Japanese Urol Assoc. 2001;8:495–499. doi: 10.1046/j.1442-2042.2001.00358.x. [DOI] [PubMed] [Google Scholar]
- 14.Hochreiter WW, Nadler RB, Koch AE, et al. Evaluation of the cytokines interleukin 8 and epithelial neutrophil activating peptide 78 as indicators of inflammation in prostatic secretions. Urology. 2000;56:1025–1029. doi: 10.1016/s0090-4295(00)00844-x. [DOI] [PubMed] [Google Scholar]
- 15.Miller LJ, Fischer KA, Goralnick SJ, et al. Interleukin-10 levels in seminal plasma: implications for chronic prostatitis-chronic pelvic pain syndrome. J Urol. 2002;167:753–756. doi: 10.1016/S0022-5347(01)69139-0. [DOI] [PubMed] [Google Scholar]
- 16.Desireddi NV, Campbell PL, Stern JA, et al. Monocyte chemoattractant protein-1 and macrophage inflammatory protein-1alpha as possible biomarkers for the chronic pelvic pain syndrome. J Urol. 2008;179:1857–1861. doi: 10.1016/j.juro.2008.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nadler RB, Koch AE, Calhoun EA, et al. IL-1beta and TNF-alpha in prostatic secretions are indicators in the evaluation of men with chronic prostatitis. J Urol. 2000;164:214–218. [PubMed] [Google Scholar]
- 18.Shoskes DA, Albakri Q, Thomas K, Cook D. Cytokine polymorphisms in men with chronic prostatitis/chronic pelvic pain syndrome: association with diagnosis and treatment response. J Urol. 2002;168:331–335. [PubMed] [Google Scholar]
- 19.Doble A, Walker MM, Harris JR, Taylor-Robinson D, Witherow RO. Intraprostatic antibody deposition in chronic abacterial prostatitis. Br J Urol. 1990;65:598–605. doi: 10.1111/j.1464-410x.1990.tb14827.x. [DOI] [PubMed] [Google Scholar]
- 20.Penna G, Mondaini N, Amuchastegui S, et al. Seminal plasma cytokines and chemokines in prostate inflammation: interleukin 8 as a predictive biomarker in chronic prostatitis/chronic pelvic pain syndrome and benign prostatic hyperplasia. Eur Urol. 2007;51:524–533. doi: 10.1016/j.eururo.2006.07.016. discussion 533. [DOI] [PubMed] [Google Scholar]
- 21.Hou D-S, Long W-M, Shen J, Zhao LP, Pang XY, Xu C. Characterisation of the bacterial community in expressed prostatic secretions from patients with chronic prostatitis/chronic pelvic pain syndrome and infertile men: a preliminary investigation. Asian J Androl. 2012;14:566–573. doi: 10.1038/aja.2012.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nickel JC, Stephens A, Landis JR, et al. Search for microorganisms in men with urologic chronic pelvic pain syndrome: a culture-independent analysis in the MAPP research network. J Urol. 2015;194:127–135. doi: 10.1016/j.juro.2015.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leskinen MJ, Rantakokko-Jalava K, Manninen R, et al. Negative bacterial polymerase chain reaction (PCR) findings in prostate tissue from patients with symptoms of chronic pelvic pain syndrome (CPPS) and localized prostate cancer. Prostate. 2003;55:105–110. doi: 10.1002/pros.10218. [DOI] [PubMed] [Google Scholar]
- 24.Pontari MA, McNaughton-Collins M, O’leary MP, et al. A case-control study of risk factors in men with chronic pelvic pain syndrome. BJU Int. 2005;96:559–565. doi: 10.1111/j.1464-410X.2005.05684.x. [DOI] [PubMed] [Google Scholar]
- 25.Woodworth D, Mayer E, Leu K, et al. Unique microstructural changes in the brain associated with urological chronic pelvic pain syndrome (UCPPS) revealed by diffusion tensor MRI, super-resolution track density imaging, and statistical parameter mapping: a MAPP network neuroimaging study. PLoS One. 2015;10 doi: 10.1371/journal.pone.0140250. e0140250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huang L, Kutch JJ, Ellingson BM, et al. Brain white matter changes associated with urological chronic pelvic pain syndrome: multisite neuroimaging from a MAPP case-control study. Pain. 2016;157:2782–2791. doi: 10.1097/j.pain.0000000000000703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Curtis Nickel J, Baranowski AP, Pontari M, Berger RE, Tripp DA. Management of men diagnosed with chronic prostatitis/chronic pelvic pain syndrome who have failed traditional management. Rev Urol. 2007;9:63–72. [PMC free article] [PubMed] [Google Scholar]
- 28.Khorasani B, Arab AM, Sedighi Gilani MA, Samadi V, Assadi H. Transabdominal ultrasound measurement of pelvic floor muscle mobility in men with and without chronic prostatitis/chronic pelvic pain syndrome. Urology. 2012;80:673–677. doi: 10.1016/j.urology.2012.05.026. [DOI] [PubMed] [Google Scholar]
- 29.Davis SN, Morin M, Binik YM, Khalife S, Carrier S. Use of pelvic floor ultrasound to assess pelvic floor muscle function in Urological Chronic Pelvic Pain Syndrome in men. J Sex Med. 2011;8:3173–3180. doi: 10.1111/j.1743-6109.2011.02452.x. [DOI] [PubMed] [Google Scholar]
- 30.Shoskes DA, Berger R, Elmi A, Landis JR, Propert KJ, Zeitlin S. Muscle tenderness in men with chronic prostatitis/chronic pelvic pain syndrome: the chronic prostatitis cohort study. J Urol. 2008;179:556–560. doi: 10.1016/j.juro.2007.09.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Giannitsas K, Mitropoulos D, Konstantinopoulos A, Athanasopoulos A, Perimenis P. Phosphodiesterase-5 inhibitors in the treatment of lower urinary tract symptoms and benign prostatic hyperplasia. Expert Opin Pharmacother. 2008;9:1687–1693. doi: 10.1517/14656566.9.10.1687. [DOI] [PubMed] [Google Scholar]
- 32.Gacci M, Andersson KE, Chapple C, et al. Latest evidence on the use of phosphodiesterase type 5 inhibitors for the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia. Eur Urol. 2016;70:124–133. doi: 10.1016/j.eururo.2015.12.048. [DOI] [PubMed] [Google Scholar]
- 33.Hu JC, Link CL, McNaughton-Collins M, Barry MJ, McKinlay JB. The association of abuse and symptoms suggestive of chronic prostatitis/chronic pelvic pain syndrome: results from the Boston Area Community Health survey. J Gen Intern Med. 2007;22:1532–1537. doi: 10.1007/s11606-007-0341-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spanos C, Pang X, Ligris K, et al. Stress-induced bladder mast cell activation: implications for interstitial cystitis. J Urol. 1997;157:669–672. [PubMed] [Google Scholar]
- 35.Makovey I, Dolinga R, Shoskes DA. ’Spousal Revenge Syndrome’—description of a new chronic pelvic pain syndrome patient cohort. Can J Urol. 2016;23:8176–8178. [PubMed] [Google Scholar]
- 36.Nickel JC, Tripp DA, Chuai S, et al. Psychosocial variables affect the quality of life of men diagnosed with chronic prostatitis/chronic pelvic pain syndrome. BJU Int. 2008;101:59–64. doi: 10.1111/j.1464-410X.2007.07196.x. [DOI] [PubMed] [Google Scholar]
- 37.Litwin MS, McNaughton-Collins M, Fowler FJJ, et al. The National Institutes of Health chronic prostatitis symptom index: development and validation of a new outcome measure. Chronic Prostatitis Collaborative Research Network. J Urol. 1999;162:369–375. doi: 10.1016/s0022-5347(05)68562-x. [DOI] [PubMed] [Google Scholar]
- 38.Barry MJ, Fowler FJJ, O’Leary MP, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol. 1992;148:1549–1557. doi: 10.1016/s0022-5347(17)36966-5. discussion 1564. [DOI] [PubMed] [Google Scholar]
- 39.Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–830. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 40.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E1.Meares EM, Stamey TA. Bacteriologic localization patterns in bacterial prostatitis and urethritis. Invest Urol. 1968;5:492–518. [PubMed] [Google Scholar]
- E2.Nickel JC, Shoskes D, Wang Y, et al. How does the pre-massage and post-massage 2-glass test compare to the Meares-Stamey 4-glass test in men with chronic prostatitis/chronic pelvic pain syndrome? J Urol. 2006;176:119–124. doi: 10.1016/S0022-5347(06)00498-8. [DOI] [PubMed] [Google Scholar]
- E3.Bartoletti R, Cai T, Mondaini N, et al. Prevalence, incidence estimation, risk factors and characterization of chronic prostatitis/chronic pelvic pain syndrome in urological hospital outpatients in Italy: results of a multicenter case-control observational study. J Urol. 2007;178:2411–2415. doi: 10.1016/j.juro.2007.08.046. discussion 2415. [DOI] [PubMed] [Google Scholar]
- E4.Shoskes DA, Nickel JC, Dolinga R, Prots D. Clinical phenotyping of patients with chronic prostatitis/chronic pelvic pain syndrome and correlation with symptom severity. Urology. 2009;73:533–538. doi: 10.1016/j.urology.2008.09.074. [DOI] [PubMed] [Google Scholar]
- E5.Magri V, Wagenlehner F, Perletti G, et al. Use of the UPOINT chronic prostatitis/chronic pelvic pain syndrome classification in European patient cohorts: sexual function domain improves correlations. J Urol. 2010;184:2339–2345. doi: 10.1016/j.juro.2010.08.025. [DOI] [PubMed] [Google Scholar]
- E6.Samplaski MK, Li J, Shoskes DA. Inclusion of erectile domain to UPOINT phenotype does not improve correlation with symptom severity in men with chronic prostatitis/chronic pelvic pain syndrome. Urology. 2011;78:653–658. doi: 10.1016/j.urology.2011.04.016. [DOI] [PubMed] [Google Scholar]
- E7.Shoskes DA, Nickel JC, Kattan MW. Phenotypically directed multimodal therapy for chronic prostatitis/chronic pelvic pain syndrome: a prospective study using UPOINT. Urology. 2010;75:1249–1253. doi: 10.1016/j.urology.2010.01.021. [DOI] [PubMed] [Google Scholar]
- E8.Bryk DJ, Shoskes DA. Using the UPOINT system to manage men with chronic pelvic pain syndrome. Arab J Urol. 2021;19:387–393. doi: 10.1080/2090598X.2021.1955546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E9.Roenneberg C, Hausteiner-Wiehle C, Schäfert R, Sattel H, Henningsen P. Langfassung S3 Leitlinie „Funktionelle Körperbeschwerden.“. https://register.awmf.org/assets/guidelines/051-001l_S3_Funktionelle_Koerperbeschwerden_2018-11.pdf (last accessed on 27 June 2023) 2018 [Google Scholar]
- E10.Saarto T, Wiffen PJ. Antidepressants for neuropathic pain. Cochrane database Syst Rev. 2007 doi: 10.1002/14651858.CD005454.pub2. CD005454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E11.Lunn MPT, Hughes RAC, Wiffen PJ. Duloxetine for treating painful neuropathy, chronic pain or fibromyalgia. Cochrane database Syst Rev. 2014 doi: 10.1002/14651858.CD007115.pub3. CD007115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E12.Bradley CS, Gallop R, Sutcliffe S, et al. Long-term symptom trajectories in Urologic Chronic Pelvic Pain Syndrome: a MAPP research network study. Urology. 2022;169:58–64. doi: 10.1016/j.urology.2022.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E13.Franco JVA, Turk T, Jung JH, et al. Pharmacological interventions for treating chronic prostatitis/chronic pelvic pain syndrome. Cochrane Database Syst Rev. 2019;10 doi: 10.1002/14651858.CD012552.pub2. CD012552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E14.Franco JV, Turk T, Jung JH, et al. Non-pharmacological interventions for treating chronic prostatitis/chronic pelvic pain syndrome. Cochrane Database Syst Rev. 2018;5 doi: 10.1002/14651858.CD012551.pub3. CD012551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E15.Guan X, Zhao C, Ou Z-Y, et al. Use of the UPOINT phenotype system in treating Chinese patients with chronic prostatitis/chronic pelvic pain syndrome: a prospective study. Asian J Androl. 2015;17:120–123. doi: 10.4103/1008-682X.138189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E16.Krakhotkin DV, Chernylovskyi VA, Bakurov EE, Sperl J. Evaluation of influence of the UPOINT-guided multimodal therapy in men with chronic prostatitis/chronic pelvic pain syndrome on dynamic values NIH-CPSI: a prospective, controlled, comparative study. Ther Adv Urol. 2019;11 doi: 10.1177/1756287219857271. 1756287219857271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E17.Magri V, Marras E, Restelli A, Wagenlehner FM, Perletti G. Multimodal therapy for category III chronic prostatitis/chronic pelvic pain syndrome in UPOINTS phenotyped patients. Exp Ther Med. 2015;9:658–666. doi: 10.3892/etm.2014.2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E18.Minggen Y, Zhouda Z, Zhiming Z, et al. Tamsulosin therapy for chronic nonbacterial prostatitis: a randomized double-blind placebo controlled clinical trial. Chinese J Androl. 2010;24:32–35. [Google Scholar]
- E19.Youn CW, Son K-C, Choi H-S, et al. Comparison of the efficacy of antibiotic monotherapy and antibiotic plus alpha-blocker combination therapy for patients with inflammatory chronic prostatitis/chronic pelvic pain syndrome. Korean J Urol. 2008;49:72–76. [Google Scholar]
- E20.Mehik A, Alas P, Nickel JC, Sarpola A, Helström PJ. Alfuzosin treatment for chronic prostatitis/chronic pelvic pain syndrome: a prospective, randomized, double-blind, placebo-controlled, pilot study. Urology. 2003;62:425–429. doi: 10.1016/s0090-4295(03)00466-7. [DOI] [PubMed] [Google Scholar]
- E21.Lü M, Zhao S, Wang S, Shi BK, Fan YD, Wang JZ. [Alpha-blockers and bioflavonoids in men with chronic nonbacterial prostatitis (NIH-IIIa): a prospective, placebo-controlled trial] Zhonghua Liu Xing Bing Xue Za Zhi (Chinese Journal of Epidemiology) 2004;25:169–172. [PubMed] [Google Scholar]
- E22.Lacquaniti S, Destito A, Servello C, et al. Terazosine and tamsulosin in non bacterial prostatitis: a randomized placebo-controlled study. Arch Ital di Urol Androl Organo Uff [di] Soc Ital di Ecogr Urol e Nefrol. 1999;71:283–285. [PubMed] [Google Scholar]
- E23.Kulovac B, Aganović D, Prcić A, Hadziosmanović O. Management of chronic nonbacterial prostatitis/chronic pelvic pain syndrome. Bosn J basic Med Sci. 2007;7:245–249. doi: 10.17305/bjbms.2007.3053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E24.Kim SW, Ha JS, Lee SJ, et al. Clinical effect of tamsulosin in noninflammatory chronic pelvic pain syndrome. Korean J Urol. 2003:120–123. [Google Scholar]
- E25.Jung YH, Kim JG, Cho IR. The efficacy of terazosin in the management of chronic pelvic pain syndrome (CPPS): comparison between category IIIa and IIIb. Korean J Urol. 2006;47:1191–1196. [Google Scholar]
- E26.Jeong CW, Lim DJ, Son H, Lee SE, Jeong H. Treatment for chronic prostatitis/chronic pelvic pain syndrome: levofloxacin, doxazosin and their combination. Urol Int. 2008;80:157–161. doi: 10.1159/000112606. [DOI] [PubMed] [Google Scholar]
- E27.Gül O, Eroğlu M, Ozok U. Use of terazosine in patients with chronic pelvic pain syndrome and evaluation by prostatitis symptom score index. Int Urol Nephrol. 2001;32:433–436. doi: 10.1023/a:1017504830834. [DOI] [PubMed] [Google Scholar]
- E28.Erdemir F, Firat F, Atilgan D, et al. The comparison of the efficacy of three different treatment protocols on the type 3 chronic prostatitis (Chronic Pelvic Pain Syndrome) J Clin Anal Med. 2010;1:26–30. [Google Scholar]
- E29.Dunzendorfer U, Kruschwitz K, Letzel H. Effects of phenoxybenzamine on clinical picture, laboratory test results and spermatogram in chronic abacterial prostatitis. Therapiewoche. 1983;33:4694–4705. [Google Scholar]
- E30.Wang J, Yan D, Liang K, Xu Z. A randomized controlled trial of levofloxacin, terazosin, and combination therapy in patients with category III chronic prostatitis/chronic pelvic pain syndrome. Int Urol Nephrol. 2016;48:13–18. doi: 10.1007/s11255-015-1147-1. [DOI] [PubMed] [Google Scholar]
- E31.Alexander RB, Propert KJ, Schaeffer AJ, et al. Ciprofloxacin or tamsulosin in men with chronic prostatitis/chronic pelvic pain syndrome: a randomized, double-blind trial. Ann Intern Med. 2004;141:581–589. doi: 10.7326/0003-4819-141-8-200410190-00005. [DOI] [PubMed] [Google Scholar]
- E32.Cha WH, Kim KH, Seo YJ. Comparison of the efficacy of a terpene mixture and alpha-blocker for treatment of category III chronic prostatitis/chronic pelvic pain syndrome: a prospective study. Korean J Urol. 2009;50:148–153. doi: 10.4111/kju.2009.50.2.148. (last accessed on 6 June 2023) [DOI] [Google Scholar]
- E33.Cheah PY, Liong ML, Yuen KH, et al. Terazosin therapy for chronic prostatitis/chronic pelvic pain syndrome: a randomized, placebo controlled trial. J Urol. 2003;169:592–596. doi: 10.1097/01.ju.0000042927.45683.6c. [DOI] [PubMed] [Google Scholar]
- E34.Wu Z, Xia S, Geng H, et al. Combined therapy for chronic prostatitis/chronic pelvic pain syndrome with doxazosin and diclofenac. Chinese J Androl. 2008;22:20–22. [Google Scholar]
- E35.Sivkov AV, Oshchepkov VN, Egorov AA. Double-blind placebo-controlled trial of terazosine efficacy in patients with chronic abacterial prostatitis. Urol (Moscow, Russ 1999) 2005:47–53. [PubMed] [Google Scholar]
- E36.Ryu YG, Kim HJ, Park HJ. The efficacy of alfuzosin for chronic prostatitis/chronic pelvic pain syndrome in young and middle aged patients. Korean J Urol. 2007;48:858–862. [Google Scholar]
- E37.Nickel JC, O’Leary MP, Lepor H, et al. Silodosin for men with chronic prostatitis/chronic pelvic pain syndrome: results of a phase II multicenter, double-blind, placebo controlled study. J Urol. 2011;186:125–131. doi: 10.1016/j.juro.2011.03.028. [DOI] [PubMed] [Google Scholar]
- E38.Nickel JC, Krieger JN, McNaughton-Collins M, et al. Alfuzosin and symptoms of chronic prostatitis-chronic pelvic pain syndrome. N Engl J Med. 2008;359:2663–2673. doi: 10.1056/NEJMoa0803240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E39.Nickel JC, Narayan P, McKay J, Doyle C. Treatment of chronic prostatitis/chronic pelvic pain syndrome with tamsulosin: a randomized double blind trial. J Urol. 2004;171:1594–1597. doi: 10.1097/01.ju.0000117811.40279.19. [DOI] [PubMed] [Google Scholar]
- E40.Mo KI, Lee KS, Kim DG. Efficacy of combination therapy for patients with chronic prostatitis/chronic pelvic pain syndrome: a prospective study. Korean J Urol. 2006;47:536–540. [Google Scholar]
- E41.Ye ZQ, Lan RZ, Yang WM, Yao LF, Yu X. Tamsulosin treatment of chronic non-bacterial prostatitis. J Int Med Res. 2008;36:244–252. doi: 10.1177/147323000803600205. [DOI] [PubMed] [Google Scholar]
- E42.Zhou Z, Hong L, Shen X, et al. Detection of nanobacteria infection in type III prostatitis. Urology. 2008;71:1091–1095. doi: 10.1016/j.urology.2008.02.041. [DOI] [PubMed] [Google Scholar]
- E43.Nickel JC, Downey J, Clark J, et al. Levofloxacin for chronic prostatitis/chronic pelvic pain syndrome in men: a randomized placebo-controlled multicenter trial. Urology. 2003;62:614–617. doi: 10.1016/s0090-4295(03)00583-1. [DOI] [PubMed] [Google Scholar]
- E44.Kim TH, Lee KS, Kim JH, et al. Tamsulosin monotherapy versus combination therapy with antibiotics or anti-inflammatory agents in the treatment of chronic pelvic pain syndrome. Int Neurourol J. 2011;15:92–96. doi: 10.5213/inj.2011.15.2.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E45.Choe H-S, Lee S-J, Han CH, Shim BS, Cho YH. Clinical efficacy of roxithromycin in men with chronic prostatitis/chronic pelvic pain syndrome in comparison with ciprofloxacin and aceclofenac: a prospective, randomized, multicenter pilot trial. J Infect Chemother Off J Japan Soc Chemother. 2014;20:20–25. doi: 10.1016/j.jiac.2013.07.010. [DOI] [PubMed] [Google Scholar]
- E46.Lai Y, Cheng C, Hsueh T, Chiu Y, Chen S, Chiu A. The efficacy of levofloxacin or ciprofloxacin in management of chronic nonbacterial prostatitis. Urology. 2012;80 [Google Scholar]
- E47.Shoskes DA, Nickel JC. Classification and treatment of men with chronic prostatitis/chronic pelvic pain syndrome using the UPOINT system. World J Urol. 2013;31:755–760. doi: 10.1007/s00345-013-1075-6. [DOI] [PubMed] [Google Scholar]
- E48.Leskinen M, Lukkarinen O, Marttila T. Effects of finasteride in patients with inflammatory chronic pelvic pain syndrome: a double-blind, placebo-controlled, pilot study. Urology. 1999;53:502–505. doi: 10.1016/s0090-4295(98)00540-8. [DOI] [PubMed] [Google Scholar]
- E49.Nickel JC, Downey J, Pontari MA, Shoskes DA, Zeitlin SI. A randomized placebo-controlled multicentre study to evaluate the safety and efficacy of finasteride for male chronic pelvic pain syndrome (category IIIA chronic nonbacterial prostatitis) BJU Int. 2004;93:991–995. doi: 10.1111/j.1464-410X.2003.04766.x. [DOI] [PubMed] [Google Scholar]
- E50.Zhao WP, Zhang ZG, Li XD, et al. Celecoxib reduces symptoms in men with difficult chronic pelvic pain syndrome (Category IIIA) Brazilian J Med Biol Res. 2009;42:963–967. doi: 10.1590/s0100-879x2009005000021. [DOI] [PubMed] [Google Scholar]
- E51.Yang MG, Zhao XK, Wu ZP, Xiao N, Lü C, Hou Y. [Corticoid combined with an antibiotic for chronic nonbacterial prostatitis] Zhonghua Nan Ke Xue (National Journal of Andrology) 2009;15:237–240. Chinese. PMID: 19452696. [PubMed] [Google Scholar]
- E52.Tuğcu V, Taşçi AI, Fazlioğlu A, et al. A placebo-controlled comparison of the efficiency of triple- and monotherapy in category III B chronic pelvic pain syndrome (CPPS) Eur Urol. 2007;51:1113–1117. doi: 10.1016/j.eururo.2006.09.036. discussion 1118. [DOI] [PubMed] [Google Scholar]
- E53.Jiang MH, Wu GC, Liu HL. [Dexketoprofen trometamol in the treatment of chronic prostatitis/chronic pelvic pain syndrome] Zhonghua Nan Ke Xue (National Journal of Andrology) 2009;15:825–828. Chinese. PMID: 19947568. [PubMed] [Google Scholar]
- E54.Goldmeier D, Madden P, McKenna M, Tamm N. Treatment of category III A prostatitis with zafirlukast: a randomized controlled feasibility study. Int J STD AIDS. 2005;16:196–200. doi: 10.1258/0956462053420239. [DOI] [PubMed] [Google Scholar]
- E55.Bates SM, Hill VA, Anderson JB, et al. A prospective, randomized, double blind trial to evaluate the role of a short reducing course of oral corticosteroid therapy in the treatment of chronic prostatitis/chronic pelvic pain syndrome. BJU Int. 2007;99:355–359. doi: 10.1111/j.1464-410X.2007.06667.x. [DOI] [PubMed] [Google Scholar]
- E56.Apolikhin OI, Aliaev IuG, Sivkov AV, et al. A comparative clinical randomized trial of cernilton efficacy and safety in patients with chronic abacterial prostatitis. Urol (Moscow, Russ 1999) 2010:29–34. [PubMed] [Google Scholar]
- E57.Macchione N, Catalani M. Pollen extract in association with vitamins (Deprox 500®) versus serenoa repens in chronic prostatitis/chronic pelvic pain syndrome; a single center experience. J Urol. 2017;197:e120–e120. [Google Scholar]
- E58.Maurizi A, De Luca F, Zanghi A, et al. The role of nutraceutical medications in men with non bacterial chronic prostatitis and chronic pelvic pain syndrome: a prospective non blinded study utilizing flower pollen extracts versus bioflavonoids. Arch Ital di Urol Androl organo Uff [di] Soc Ital di Ecogr Urol e Nefrol. 2019;90:260–264. doi: 10.4081/aiua.2018.4.260. [DOI] [PubMed] [Google Scholar]
- E59.Morgia G, Mucciardi G, Galì A, et al. Treatment of chronic prostatitis/chronic pelvic pain syndrome category IIIA with Serenoa repens plus selenium and lycopene (profluss®) versus S. repens alone: an Italian randomized multicenter-controlled study. Urol Int. 2010;84:400–406. doi: 10.1159/000302716. [DOI] [PubMed] [Google Scholar]
- E60.Morgia G, Russo GI, Urzì D, et al. A phase II, randomized, single-blinded, placebo-controlled clinical trial on the efficacy of Curcumina and Calendula suppositories for the treatment of patients with chronic prostatitis/chronic pelvic pain syndrome type III. Arch Ital di Urol e Androl. 2017;89:110–113. doi: 10.4081/aiua.2017.2.110. [DOI] [PubMed] [Google Scholar]
- E61.Okada S, Hamada K, Takasaki N, et al. [Clinical application of PPC for nonspecific chronic prostatitis] Hinyokika Kiyo. 1985;31:179–185. [PubMed] [Google Scholar]
- E62.Park SJ, Yoon HN, Shim BS. Prevention of relapse with the cranberry juice in chronic pelvic pain syndrome. Korean J Urol. 2005:63–67. [Google Scholar]
- E63.Reissigl A, Djavan B, Pointner J, et al. Prospective placebo-controlled multicenter trial on safety and efficacy of phytotherapy in the treatment of chronic prostatitis/chronic pelvic pain syndrome. J Urol. 2004;171 [Google Scholar]
- E64.Shoskes DA, Zeitlin SI, Shahed A, Rajfer J. Quercetin in men with category III chronic prostatitis: a preliminary prospective, double-blind, placebo-controlled trial. Urology. 1999;54:960–963. doi: 10.1016/s0090-4295(99)00358-1. [DOI] [PubMed] [Google Scholar]
- E65.Wagenlehner FME, Schneider H, Ludwig M, Schnitker J, Brähler E, Weidner W. A pollen extract (Cernilton) in patients with inflammatory chronic prostatitis-chronic pelvic pain syndrome: a multicentre, randomised, prospective, double-blind, placebo-controlled phase 3 study. Eur Urol. 2009;56:544–551. doi: 10.1016/j.eururo.2009.05.046. [DOI] [PubMed] [Google Scholar]
- E66.Wagenlehner FME, Schneider H, Ludwig M, et al. Long term efficacy of cernilton in patients with chronic prostatitis/chronic pelvic pain syndrome type NIH IIIA. Eur Urol Suppl. 2009;4 doi: 10.1016/j.eururo.2009.05.046. [DOI] [PubMed] [Google Scholar]
- E67.Cai T, Wagenlehner FME, Luciani LG, et al. Pollen extract in association with vitamins provides early pain relief in patients affected by chronic prostatitis/chronic pelvic pain syndrome. Exp Ther Med. 2014;8:1032–1038. doi: 10.3892/etm.2014.1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E68.Xu M, Zhang Y. Effect of antibacterial agents in treatment of chronic nonbacterial prostatitis. JOURNAL-SHANGHAI Med Univ. 2000;27:497–498. [Google Scholar]
- E69.Ye Z, Lan R, Wang S, et al. [A clinical study of prostat combined with an antibiotic for chronic nonbacterial prostatitis] Zhonghua Nan Ke Xue. 2006;12:807–810. [PubMed] [Google Scholar]
- E70.Cai T, Gallelli L, Cione E, et al. The efficacy and tollerability of pollen extract in combination with hyaluronic acid and vitamins in the management of patients affected by chronic prostatitis/chronic pelvic pain syndrome: a 26 weeks, randomized, controlled, single-blinded, phase III study. Minerva Urol Nephrol. 2022;74:780–788. doi: 10.23736/S2724-6051.21.04141-2. [DOI] [PubMed] [Google Scholar]
- E71.Breusov AA, Kul’chavenia EV. Influence of combined phytotherapy on sexual function in patients with chronic abacterial prostatitis. Urologiia (Moscow, Russ 1999) 2014:24–26. [PubMed] [Google Scholar]
- E72.Cai T, Verze P, La Rocca R, et al. The clinical efficacy of pollen extract and vitamins on chronic prostatitis/chronic pelvic pain syndrome is linked to a decrease in the pro-inflammatory cytokine interleukin-8. World J Mens Health. 2017;35:120–128. doi: 10.5534/wjmh.2017.35.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E73.Elist J. Effects of pollen extract preparation Prostat/Poltit on lower urinary tract symptoms in patients with chronic nonbacterial prostatitis/chronic pelvic pain syndrome: a randomized, double-blind, placebo-controlled study. Urology. 2006;67:60–63. doi: 10.1016/j.urology.2005.07.035. [DOI] [PubMed] [Google Scholar]
- E74.Giammusso B, Di Mauro R, Bernardini R. The efficacy of an association of palmitoylethanolamide and alpha-lipoic acid in patients with chronic prostatitis/chronic pelvic pain syndrome: a randomized clinical trial. Arch Ital di Urol Androl organo Uff [di] Soc Ital di Ecogr Urol e Nefrol. 2017;89:17–21. doi: 10.4081/aiua.2017.1.17. [DOI] [PubMed] [Google Scholar]
- E75.Iwamura H, Koie T, Soma O, et al. Eviprostat has an identical effect compared to pollen extract (Cernilton) in patients with chronic prostatitis/chronic pelvic pain syndrome: a randomized, prospective study. BMC Urol. 2015;15 doi: 10.1186/s12894-015-0115-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E76.Kaplan SA, Volpe MA, Te AE. A prospective, 1-year trial using saw palmetto versus finasteride in the treatment of category III prostatitis/chronic pelvic pain syndrome. J Urol. 2004;171:284–288. doi: 10.1097/01.ju.0000101487.83730.80. [DOI] [PubMed] [Google Scholar]
- E77.Lee CB, Ha U-S, Lee SJ, Kim SW, Cho YH. Preliminary experience with a terpene mixture versus ibuprofen for treatment of category III chronic prostatitis/chronic pelvic pain syndrome. World J Urol. 2006;24:55–60. doi: 10.1007/s00345-005-0039-x. [DOI] [PubMed] [Google Scholar]
- E78.Pena VN, Engel N, Gabrielson AT, Rabinowitz MJ, Herati AS. Diagnostic and management strategies for patients with chronic prostatitis and chronic pelvic pain syndrome. Drugs Aging. 2021;38:845–886. doi: 10.1007/s40266-021-00890-2. [DOI] [PubMed] [Google Scholar]
- E79.Elshawaf H. Chemodenervation of the rhabdosphincter (EUS) alone versus combined injection of both EUS & prostate in patients with prostatitis and chronic pelvic pain syndrome type III. Prospective randomized controlled trial. (Abstract number 394) Proc 39th Annu Meet Int Cont Soc (ICS), 2009 Sep 29-Oct 3, San Fr CA. 2009 [Google Scholar]
- E80.Falahatkar S, Shahab E, Gholamjani Moghaddam K, Moghaddam K, Kazemnezhad E. Transurethral intraprostatic injection of botulinum neurotoxin type A for the treatment of chronic prostatitis/chronic pelvic pain syndrome: results of a prospective pilot double-blind and randomized placebo-controlled study. BJU Int. 2015;116:641–649. doi: 10.1111/bju.12951. [DOI] [PubMed] [Google Scholar]
- E81.Gottsch H, Berger R, Miller J, et al. Pelvic floor injection of botulinum toxin A for pelvic pain: a randomized, controlled pilot study. J Urol. 2010;183:e405–e405. [Google Scholar]
- E82.Parsons BA, Goonewardene S, Dabestani S, et al. The benefits and harms of Botulinum Toxin-A in the treatment of chronic pelvic pain syndromes: a systematic review by the European Association of Urology Chronic Pelvic Pain Panel. Eur Urol Focus. 2022;8:320–338. doi: 10.1016/j.euf.2021.01.005. [DOI] [PubMed] [Google Scholar]
- E83.Abdel-Meguid TA, Mosli HA, Farsi H, et al. Treatment of refractory category III nonbacterial chronic prostatitis/chronic pelvic pain syndrome with intraprostatic injection of onabotulinumtoxinA: a prospective controlled study. Can J Urol. 2018;25:9273–9280. [PubMed] [Google Scholar]
- E84.Chen DN, Chen WT, Ma QH, Qin Z, Huang ZW. [Qiantongding Decoction: An efficacious therapeutic for type III B prostatitis] Zhonghua Nan Ke Xue (National Journal of Andrology) 2009;15:89–91. [PubMed] [Google Scholar]
- E85.Hu AD, Hu MZ, Wang B, et al. Chinese and western medicine in treatment of chronic nonbacterial prostatitis. Liaoning J Tradit Chin Med. 2015;42:353–354. [Google Scholar]
- E86.Li N, Zhang K, Xiao H. The efficacy and safety of Prostant™ in the treatment of chronic prostatitis: a multi-center, randomized, double-blind, placebo-controlled clinical trial. Chinese J Urol. 2001 [Google Scholar]
- E87.Li B, Jiang L, Chai J. [Clinical observation on treatment of chronic prostatitis syndrome type III B by Tiaoshen Tonglin Decoction] Zhongguo Zhong xi yi jie he za zhi Zhongguo Zhongxiyi jiehe zazhi (Chinese J Integr Tradit West Med) 2007;27:251–254. [PubMed] [Google Scholar]
- E88.Li J-P, Chong T, Chen H-W, et al. [Qianlieping capsule plus alpha-blocker for chronic non-bacterial prostatitis: analysis of 220 cases] Zhonghua Nan Ke Xue. 2012;18:856–858. [PubMed] [Google Scholar]
- E89.Peng S-F, Yang Z-Z, Lin X-F, et al. [Clinical trials of antiphlogistic agent series in treating chronic nonbacterial prostatitis] Zhonghua Nan Ke Xue. 2003;9:716–719. [PubMed] [Google Scholar]
- E90.Tan Y, Zhu X, Liu Y. Clinical efficiency of Tamsulosin combining with Prostant in the treatment of patients with chronic abacterial prostatitis. Chinese J Androl. 2009;23:44–47. [Google Scholar]
- E91.Wang W, He H, Hu W, Zhang X, Wang Y. [Efficacy and safety of intraprostatic injection of chuanshentong for chronic abacterial prostatitis/chronic pelvic pain syndrome] Zhonghua Nan Ke Xue. 2004;10:182–184. 187. [PubMed] [Google Scholar]
- E92.Xia YG, Zeng WT, Mei XF, et al. [Yuleshu oral mixture combined with conventional therapy for chronic prostatitis] Zhonghua Nan Ke Xue. 2014;20:177–180. [PubMed] [Google Scholar]
- E93.Zhang M, Chu K, Shi Y. [Clinical study on treatment of chronic prostatitis/chronic pelvic pain syndrome by three different TCM principles] Zhongguo Zhong xi yi jie he za zhi Zhongguo Zhongxiyi jiehe zazhi (Chinese J Integr Tradit West Med) 2007;27:989–992. [PubMed] [Google Scholar]
- E94.Singh P, Shukla A, Dogra PN. Role of PDE-5 inhibitor in the treatment of chronic pelvic pain syndrome: a randomized control trial. J Urol. 2017;197 [Google Scholar]
- E95.El Sayed AA, Dosyk H, Marouf A, et al. Daily low dose tadalafil in treatment of chronic prostatitis/ chronic pelvic pain syndrome: randomized controlled study of efficacy and safety. J Urol. 2018;199 [Google Scholar]
- E96.Kong DH, Yun CJ, Park HJ, Park NC. The efficacy of mirodenafil for chronic prostatitis/chronic pelvic pain syndrome in middle-aged males. World J Mens Health. 2014;32:145–150. doi: 10.5534/wjmh.2014.32.3.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E97.Lin Z, Chen B, Zeng K, Lan HM, Wun J. [Effects of Huafenqinutang and vardenafil for treatment of chronic prostatitis/chronic pelvic pain syndrome with concomitant erectile dysfunction] Nan Fang Yi Ke Da Xue Xue Bao. 2007;27:532–534. [PubMed] [Google Scholar]
- E98.Park HJ, Park NC, Moon DG, et al. Efficacy of tadalafil for treating chronic prostatitis/chronic pelvic pain syndrome in patients without erectile dysfunction. Eur Urol Suppl. 2017;3 [Google Scholar]
- E99.Park PHJ, Park PNC. The efficacy of tadalafil for chronic prostatitis/chronic pelvic pain syndrome in young and middle aged patients. Eur Urol Suppl. 2012;1 [Google Scholar]
- E100.Tawfik AM, Radwan MH, Abdulmonem M, Abo-Elenen M, Elgamal SA, Aboufarha MO. Tadalafil monotherapy in management of chronic prostatitis/chronic pelvic pain syndrome: a randomized double-blind placebo controlled clinical trial. World J Urol. 2022;40:2505–2511. doi: 10.1007/s00345-022-04074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E101.Cavallini G. Mepartricin in the treatment of male pelvic pain syndrome secondary to chronic nonbacterial prostatitis/prostatodynia. Minerva Urol e Nefrol Ital J Urol Nephrol. 2001;53:13–17. [PubMed] [Google Scholar]
- E102.De Rose AF, Gallo F, Giglio M, Carmignani G. Role of mepartricin in category III chronic nonbacterial prostatitis/chronic pelvic pain syndrome: a randomized prospective placebo-controlled trial. Urology. 2004;63:13–16. doi: 10.1016/j.urology.2003.08.006. [DOI] [PubMed] [Google Scholar]
- E103.Sun Y, Liu Y, Liu B, et al. Efficacy of acupuncture for chronic prostatitis/chronic pelvic pain syndrome: a randomized trial. Ann Intern Med. 2021;174:1357–1366. doi: 10.7326/M21-1814. [DOI] [PubMed] [Google Scholar]
- E104.Qin Z, Zang Z, Zhou K, et al. Acupuncture for chronic prostatitis/chronic pelvic pain syndrome: a randomized, sham acupuncture controlled trial. J Urol. 2018;200:815–822. doi: 10.1016/j.juro.2018.05.001. [DOI] [PubMed] [Google Scholar]
- E105.Sahin S, Bicer M, Eren GA, et al. Acupuncture relieves symptoms in chronic prostatitis/chronic pelvic pain syndrome: a randomized, sham-controlled trial. Prostate Cancer Prostatic Dis. 2015;18:249–254. doi: 10.1038/pcan.2015.13. [DOI] [PubMed] [Google Scholar]
- E106.Lee S-H, Lee B-C. Electroacupuncture relieves pain in men with chronic prostatitis/chronic pelvic pain syndrome: three-arm randomized trial. Urology. 2009;73:1036–1041. doi: 10.1016/j.urology.2008.10.047. [DOI] [PubMed] [Google Scholar]
- E107.Lee SWH, Liong ML, Yuen KH, et al. Acupuncture versus sham acupuncture for chronic prostatitis/chronic pelvic pain. Am J Med. 2008;121:79–e1. doi: 10.1016/j.amjmed.2007.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E108.Küçük EV, Suçeken FY, Bindayı A, Boylu U, Onol FF, Gümüş E. Effectiveness of acupuncture on chronic prostatitis-chronic pelvic pain syndrome category IIIB patients: a prospective, randomized, nonblinded, clinical trial. Urology. 2015;85:636–640. doi: 10.1016/j.urology.2014.11.004. [DOI] [PubMed] [Google Scholar]
- E109.Chen Z-X. [Observation on therapeutic effect of warm needle moxibustion on chronic non-bacterial prostatitis] Zhongguo Zhen Jiu. 2009;29:275–278. [PubMed] [Google Scholar]
- E110.Kabay S, Kabay SC, Yucel M, Ozden H. Efficiency of posterior tibial nerve stimulation in category IIIB chronic prostatitis/chronic pelvic pain: a sham-controlled comparative study. Urol Int. 2009;83:33–38. doi: 10.1159/000224865. [DOI] [PubMed] [Google Scholar]
- E111.Cottrell AM, Schneider MP, Goonewardene S, et al. Benefits and harms of electrical neuromodulation for chronic pelvic pain: a systematic review. Eur Urol Focus. 2020;6:559–571. doi: 10.1016/j.euf.2019.09.011. [DOI] [PubMed] [Google Scholar]
- E112.Tutolo M, Ammirati E, Heesakkers J, et al. Efficacy and safety of sacral and percutaneous tibial neuromodulation in non-neurogenic lower urinary tract dysfunction and chronic pelvic pain: a systematic review of the literature. Eur Urol. 2018;73:406–418. doi: 10.1016/j.eururo.2017.11.002. [DOI] [PubMed] [Google Scholar]
- E113.Zimmermann RP, Cumpanas A, Miclea F, et al. One year follow up of extracorporeal shock wave therapy (ESWT) for chronic pelvic pain syndrome (CPPS) in a randomised placebo-controlled double-blind study. Eur Urol Suppl. 2010;2 [Google Scholar]
- E114.Zimmermann R, Cumpanas A, Miclea F, Janetschek G. Extracorporeal shock wave therapy for the treatment of chronic pelvic pain syndrome in males: a randomised, double-blind, placebo-controlled study. Eur Urol. 2009;56:418–424. doi: 10.1016/j.eururo.2009.03.043. [DOI] [PubMed] [Google Scholar]
- E115.Zeng X, Liang C, Ye ZQ. Extracorporeal shock wave treatment for non-inflammatory chronic pelvic pain syndrome: a prospective, randomized and sham-controlled study. Chin Med J (Engl) 2012;125:114–118. [PubMed] [Google Scholar]
- E116.Moayednia A, Haghdani S, Khosrawi S, Yousefi E, Vahdatpour B. Long-term effect of extracorporeal shock wave therapy on the treatment of chronic pelvic pain syndrome due to non bacterial prostatitis. J Res Med Sci Off J Isfahan Univ Med Sci. 2014;19:293–296. [PMC free article] [PubMed] [Google Scholar]
- E117.Vahdatpour B, Alizadeh F, Moayednia A, Emadi M, Khorami MH, Haghdani S. Efficacy of extracorporeal shock wave therapy for the treatment of chronic pelvic pain syndrome: a randomized, controlled trial. ISRN Urol 2013. 2013 doi: 10.1155/2013/972601. 972601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E118.Pajovic B, Radojevic N, Dimitrovski A, Vukovic M. Comparison of the efficiency of combined extracorporeal shock-wave therapy and triple therapy versus triple therapy itself in Category III B chronic pelvic pain syndrome (CPPS) Aging Male. 2016;19:202–207. doi: 10.1080/13685538.2016.1197899. [DOI] [PubMed] [Google Scholar]
- E119.Mykoniatis I, Pyrgidis N, Sokolakis I, et al. Low-intensity shockwave therapy for the management of chronic prostatitis/chronic pelvic pain syndrome: a systematic review and meta-analysis. BJU Int. 2021;128:144–152. doi: 10.1111/bju.15335. [DOI] [PubMed] [Google Scholar]
- E120.Giubilei G, Mondaini N, Minervini A, et al. Physical activity of men with chronic prostatitis/chronic pelvic pain syndrome not satisfied with conventional treatments—could it represent a valid option? The physical activity and male pelvic pain trial: a double-blind, randomized study. J Urol. 2007;177:159–165. doi: 10.1016/j.juro.2006.08.107. [DOI] [PubMed] [Google Scholar]
- E121.Gallo L. Effectiveness of diet, sexual habits and lifestyle modifications on treatment of chronic pelvic pain syndrome. Prostate Cancer Prostatic Dis. 2014;17:238–245. doi: 10.1038/pcan.2014.18. [DOI] [PubMed] [Google Scholar]
- E122.Curran NC. Commentary on the influence of gender on the management of chronic pelvic pain. BJOG. 2015;122:766–768. doi: 10.1111/1471-0528.13292. [DOI] [PubMed] [Google Scholar]
- E123.Aulenkamp J, Steinmüller K, Icenhour A, Elsenbruch S. [From gut feeling to visceral pain: effects of negative expectations in the context of the gut-brain axis] Schmerz. 2022;36:182–188. doi: 10.1007/s00482-021-00614-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E124.Lamvu G, Ouyang C, Rapkin A. A review of chronic pelvic pain in women-reply. JAMA. 2021;326:2207–2208. doi: 10.1001/jama.2021.17989. [DOI] [PubMed] [Google Scholar]
- E125.Aziz Q, Giamberardino MA, Barke A, et al. The IASP classification of chronic pain for ICD-11: chronic secondary visceral pain. Pain. 2019;160:69–76. doi: 10.1097/j.pain.0000000000001362. [DOI] [PubMed] [Google Scholar]
- E126.Afari N, Buchwald D, Clauw D, et al. A MAPP network case-control study of urological chronic pelvic pain compared with nonurological pain conditions. Clin J Pain. 2020;36:8–15. doi: 10.1097/AJP.0000000000000769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E127.Rodríguez MAB, Afari N, Buchwald DS. Evidence for overlap between urological and nonurological unexplained clinical conditions. J Urol. 2009;182:2123–2131. doi: 10.1016/j.juro.2009.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E128.Gasperi M, Panizzon M, Goldberg J, Buchwald D, Afari N. Posttraumatic stress disorder and chronic pain conditions in men: a twin study. Psychosom Med. 2021;83:109–117. doi: 10.1097/PSY.0000000000000899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E129.Naliboff BD, Stephens AJ, Afari N, et al. Widespread psychosocial difficulties in men and women with urologic chronic pelvic pain syndromes: case-control findings from the multidisciplinary approach to the study of chronic pelvic pain research network. Urology. 2015;85:1319–1327. doi: 10.1016/j.urology.2015.02.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E130.Häuser W, Schmutzer G, Hinz A, Brähler E. [Prevalence and predictors of urogenital pain in men. Results from a survey of a representative German population sample] Schmerz. 2012;26:192–199. doi: 10.1007/s00482-011-1141-1. [DOI] [PubMed] [Google Scholar]
- E131.Nilges P, Rief W. [F45.41: chronic pain disorder with somatic and psychological factors: a coding aid] Schmerz. 2010;24:209–212. doi: 10.1007/s00482-010-0908-0. [DOI] [PubMed] [Google Scholar]
- E132.Treede R-D, Rief W, Barke A, et al. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the International Classification of Diseases (ICD-11) Pain. 2019;160:19–27. doi: 10.1097/j.pain.0000000000001384. [DOI] [PubMed] [Google Scholar]
- E133.Casser H-R, Arnold B, Brinkschmidt T, et al. [Multidisciplinary assessment for multimodal pain therapy. Indications and range of performance] Schmerz. 2013;27:363–370. doi: 10.1007/s00482-013-1337-7. [DOI] [PubMed] [Google Scholar]
- E134.Elsenbruch S, Koenen LR, Siedentopf F, Häuser W. www.schmerzgesellschaft.de/fileadmin/user_upload/DS_Fragebogen_AK_Visz_Schmerz_Ma__nnlich_24082017_RZ_Screen_final.pdf (last accessed on 6 June 2023) Berlin: 2019. Modul Viszerale und urogenitale Schmerzen für Männer. Dtsch Schmerzgesellschaft e. V. [Google Scholar]
- E135.Arnold B, Brinkschmidt T, Casser H-R, et al. [Multimodal pain therapy: principles and indications] Schmerz. 2009;23:112–120. doi: 10.1007/s00482-008-0741-x. [DOI] [PubMed] [Google Scholar]
- E136.Kieselbach K, Wirz S, Schenk M. Multimodale Schmerztherapie. Ein Praxislehrbuch. W Kohlhammer. 2021:54–61. [Google Scholar]
- E137.Kessler TM. Chronic pelvic pain syndrome: light at the end of the tunnel? Eur Urol. 2016;69:298–299. doi: 10.1016/j.eururo.2015.09.028. [DOI] [PubMed] [Google Scholar]
- E138.Magistro G, Wagenlehner FME, Grabe M, Weidner W, Stief CG, Nickel JC. Contemporary management of chronic prostatitis/chronic pelvic pain syndrome. Eur Urol. 2016;69:286–297. doi: 10.1016/j.eururo.2015.08.061. [DOI] [PubMed] [Google Scholar]
- E139.Magri V, Boltri M, Cai T, et al. Multidisciplinary approach to prostatitis. Arch Ital di Urol Androl organo Uff [di] Soc Ital di Ecogr Urol e Nefrol. 2019;90:227–248. doi: 10.4081/aiua.2018.4.227. [DOI] [PubMed] [Google Scholar]