Abstract
Objective
In up to 20% of patients, the aetiology of acute pancreatitis (AP) remains elusive and is thus called idiopathic. On more detailed review these cases can often be explained through biliary disease and are amenable to treatment. Findings range from biliary sludge to microlithiasis but their definitions remain fluid and controversial.
Design
A systematic literature review (1682 reports, following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines) analysed definitions of biliary sludge and microlithiasis, followed by an online international expert survey (30 endoscopic ultrasound/hepatobiliary and pancreatic experts; 36 items) which led to definitions of both. These were consented by Delphi voting and clinically evaluated in a retrospective cohort of patients with presumed biliary pancreatitis.
Results
In 13% of original articles and 19.2% of reviews, microlithiasis and biliary sludge were used synonymously. In the survey, 41.7% of experts described the term ‘sludge’ and ‘microlithiasis’ as identical findings. As a consequence, three definitions were proposed, agreed on and confirmed by voting to distinctly discriminate between biliary sludge (hyperechoic material without acoustic shadowing) and microlithiasis (echorich calculi of ≤5 mm with acoustic shadowing) as opposed to larger biliary stones, both for location in gallbladder and bile ducts. In an initial attempt to investigate the clinical relevance in a retrospective analysis in 177 confirmed cases in our hospital, there was no difference in severity of AP if caused by sludge, microlithiasis or stones.
Conclusion
We propose a consensus definition for the localisation, ultrasound morphology and diameter of biliary sludge and microlithiasis as distinct entities. Interestingly, severity of biliary AP was not dependent on the size of concrements warranting prospective randomised studies which treatment options are adequate to prevent recurrence.
Keywords: acute pancreatitis, gallstones
WHAT IS ALREADY KNOWN ON THIS TOPIC.
In up to 20% of patients, the aetiology of acute pancreatitis (AP) remains elusive and is thus termed idiopathic.
A biliary origin explains a sizeable proportion of idiopathic AP cases that have not been identified on routine workup but are detectable on endoscopic ultrasound. The reported spectrum ranges from biliary sludge to microlithiasis, but their definitions remain imprecise and controversial.
These incongruities in the literature preclude an accurate assessment of the risk of recurrent biliary pancreatitis.
WHAT THIS STUDY ADDS
In a systematic review of 1682 articles on the use and definition of the term biliary sludge and microlithiasis, in up to 20% of the publications the terms biliary sludge and microlithiasis were used synonymously.
By consensus. discrete, hyperechoic material without acoustic shadowing, which sediments in the most dependent part of the gallbladder represents biliary sludge.
Similarly, the term ‘biliary microlithiasis’ should be used exclusively for cases in which examination of the biliary tree or gallbladder reveals the presence of calculi ≤5 mm (in diameter) with acoustic shadowing.
In a first retrospective analysis, severity of established AP was independent of biliary concrement definition/size.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Using the proposed definition of biliary sludge and microlithiasis, prospective studies will be able to determine the risk of biliary sludge and/or microlithiasis for the development and recurrence of AP.
Introduction
Gallstones small enough to migrate from the gallbladder into the duodenum can trigger pancreatitis. Pancreatic outflow obstruction as proposed by Opie is the critical event for the disease onset.1 Already the presence of gallbladder stones on imaging (most frequently on ultrasound) in the presence of pancreatitis suggests the diagnosis of biliary pancreatitis according to international guidelines.2 Visualisation of the common bile duct (CBD) by transabdominal ultrasound to diagnose sludge or microlithiasis is highly insensitive (roughly 55%) and unspecific.3 It is thus unsurprising that only in the last decade of the 20th century with the introduction of endoscopic ultrasound (EUS) to investigate the CBD reports by Ros et al and Lee et al made biliary microlithiasis and biliary sludge widely recognised as causes of acute pancreatitis.4 5 The remarkable progress in imaging techniques, especially the development of EUS allowed changing the diagnosis of previously presumed ‘idiopathic’ pancreatitis towards a biliary aetiology caused by microliths or biliary sludge.6–8 EUS, being even more sensitive than microscopic examination of duodenal bile let alone MRCP to diagnose bile duct stones not detected by transabdominal ultrasonography, is widely recognised as a reference diagnostic technique for biliary microlithiasis.9–11 On the other hand, reports on the incidence of microlithiasis or biliary sludge in acute pancreatitis vary substantially.12–14 A recent meta-analysis has shown that biliary aetiology is the the most common cause of ‘idiopathic’ pancreatitis, with a prevalence of 30%.8 However, the authors did not discriminate between biliary sludge or microlithiasis in this analysis.
Interestingly, despite a high number of reports, no meta-analysis directly relates to or distinguishes between biliary sludge and microlithiasis in pancreatitis. This situation is probably due to a need for an agreement on the basic definitions regarding (endo)sonographic features, size of microliths and location of the described material in the biliary system, precluding a methodologically sound meta-analysis. The diversity of definitions poses a risk of misunderstanding between clinicians and results in a lack of high-quality clinical trials. This translates directly to the decision-making of gastroenterologists and surgeons regarding therapeutic strategies, which are nowadays based only on a single, rather controversial prospective observation.15–17 Furthermore, the pathophysiological relevance of biliary sludge and or microlithiasis causing pancreatitis has not been determined for lack of definition and disease models. As many definitions of biliary sludge and microlithiasis are applied, our goal was to establish universally acceptable definitions for these frequent findings by conducting an international expert survey with subsequent participant voting during a consensus conference.
Methods
Search strategy and selection criteria
Following the (Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and the PRISMA guideline update, we performed a systematic literature review from 1981 to 2021, searching the electronic database PubMed for English-language articles containing the terms ‘biliary sludge OR microlithiasis’.18 As recommended by the PRISMA guideline, the systematic review was registered in the PROSPERO database (registration number: CRD42021274442). The last online database query took place on 19 November 2021. Two independent investigators (SS and MZ) analysed the studies according to the criteria for inclusion in the literature database. In the case of incongruities regarding study inclusion, a discussion took place between the investigators until a consensus could be reached. The respective exclusion criteria for studies not included in the final database can be found in online supplemental file. Peer-reviewed articles in English had to meet at least two out of five predefined inclusion criteria (a detailed indication of how many studies each fulfilled how many predefined inclusion criteria can be found in online supplemental file; subsection 2.1.1).
gutjnl-2022-327955supp001.pdf (11.8MB, pdf)
Inclusion criteria
Definition of microlithiasis and/or biliary sludge is given in the publication.
Endoscopic, imaging and/or biochemical procedures used for microlithiasis and/or biliary sludge diagnosis is defined.
Specific ultrasonographic features of microlithiasis and/or biliary sludge were defined.
A cut-off size value for the diagnosis of microlithiasis was used.
Paper dealt explicitly with treatment methods of microlithiasis and/or biliary sludge.
An exclusion was made for articles that commented on the biliary sludge/microlithiasis only in short comments/editorials or case reports or for articles that dealt with non-biliary microlithiasis (eg, pulmonary or testicular microlithiasis). Paediatric or neonatal studies were also excluded. Since biliary sludge and microlithiasis are of pathophysiological relevance mainly in the context of (idiopathic) acute pancreatitis but have also been influential in other clinical contexts for decades, non-pancreatitis-specific studies were also examined regarding the definitions of the two terms used. These studies dealt with intensive care patients, parenteral nutrition or sludge formation in pregnancy. A distinction was made between included studies and included review articles (see figure 1). A quality assessment was only carried out for included studies (for details on data collection and quality assessment, see online supplemental files 3 and 4).
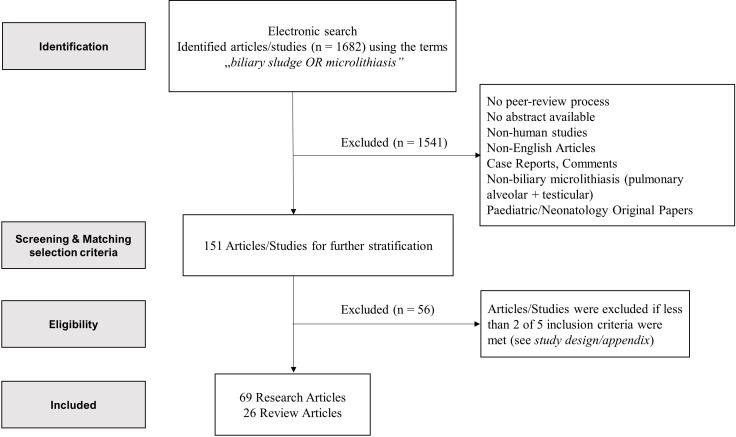
Figure 1.
Study selection. A total of 1682 articles were identified after PubMed-based literature search using the terms ‘biliary sludge or microlithiasis’ in the published period between 1981 and 2021 and PRISMA guideline-based systemic evaluation. In order to further stratify the 151 articles on screening and matching level, 2 of the 5 predefined inclusion criteria had to be fulfilled for the final inclusion of the articles (inclusion criteria: (1) Definition of microlithiasis and/or biliary sludge is given in the publication; (2) Endoscopic, imaging and/or biochemical procedures used for microlithiasis and/or biliary sludge diagnosis is defined; (3) Specific ultrasonographic features of microlithiasis and/or biliary sludge were defined; (4) A cut-off size value for the diagnosis of microlithiasis was used and (5) Paper dealt explicitly with treatment methods of microlithiasis and/or biliary sludge). In order to take into account the scientific visibility of review papers, these were also included in the literature search. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Data analyses
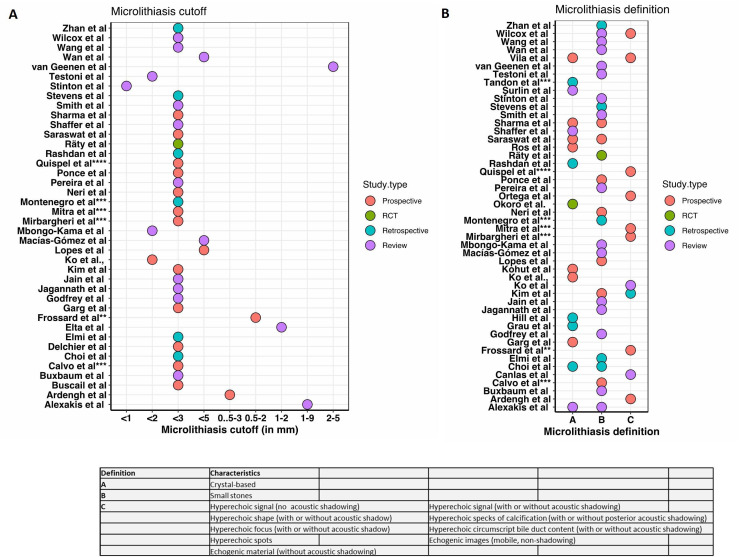
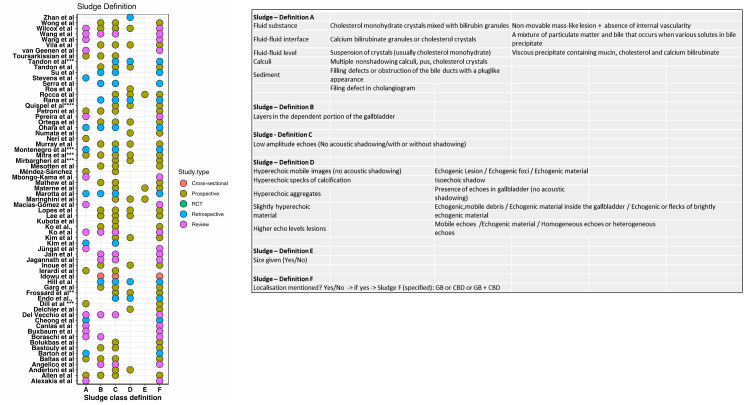
Patient characteristics of all studies were evaluated descriptively. Due to the lack of a reference clinical endpoint in the systematic literature review, we provide in the absence of the option of comparative statistics, a graphical representation of the heterogeneity of definitions found in the studies. Effect sizes or between-study variability measures (eg, I2) were not statistically quantifiable without a gold standard. To better reflect the heterogeneity of the definitions used, the included studies were clustered according to the categories (1) microlithiasis size cut-off value, (2) microlithiasis definition and (3) biliary sludge definition based on predefined characteristics (see figures 2 and 3).
Figure 2.
Heterogeneity of the biliary microlithiasis definitions used. Graphical representation of the definition heterogeneities used in the included studies for the term biliary microlithiasis as well as the stated cut-off values (if mentioned). Original studies (red, green and blue dots) as well as review studies (purple dots) are listed. Each dot symbolises a threshold value (A) or a definition point mentioned in the paper (B); see definition legend. **Gallstones not discriminated from microlithiasis. ***No difference between sludge and microlithiasis patients made. ****Video fragements used. RCT, randomised controlled trial.
Figure 3.
Heterogeneity of the biliary sludge definitions used. Graphical representation of the definition heterogeneities for the term biliary sludge used in the included studies. Original papers (red, green and blue dots) as well as review papers (purple dots) are listed. Each dot symbolises a definition point mentioned in the paper (see definition legend; for specification of the anatomical classification (sludge definition F), see online supplemental file).**Gallstones not discriminated from microlithiasis. ***No difference between sludge and microlithiasis patients made. ****Video fragments used. CBD, common bile duct; GB, gallbladder, RCT, randomised controlled trial.
Expert survey
Based on the incongruent definitions from the systematic review, we developed and validated with the help of an expert epidemiologist (TK) an online questionnaire to be completed by a selected group of 30 gastroenterologists from 11 different countries and 4 continents with high expertise in the field of endosonography-assisted diagnosis and treatment of pancreaticobiliary diseases (see online supplemental table S1). Using definition, treatment and combined questions in the form of case vignettes, the terms concerning diagnostic, clinical and treatment aspects of biliary sludge and biliary microlithiasis were to be defined and assessed. For this purpose, 36 questions within the survey were phrased, which were divided into the subsections:
Responder data (7 questions).
Definition (8 questions).
Treatment (7 questions).
Clinical case vignettes (14 questions).
The complete survey can be found in online supplemental material.
Pancreatitis patient population stratified by underlying biliary entity
A total of 601 patients with the diagnostic code acute biliary pancreatitis were retrospectively identified from the LMU database (period 2005–2021) and stratified according to the new consensus definition into the biliary entity groups sludge-induced pancreatitis (n=50), microlithiasis-induced pancreatitis (n=43) and gallstone-induced pancreatitis (n=84). In case of possible secondary aetiologies besides biliary concrements as pancreatitis triggers, patients had been excluded (n=171). The baseline characteristics of the three entity groups are presented in online supplemental table S2. The group allocation was done by retrospective chart review as well as by assessment of ultrasound (sludge-induced pancreatitis n=42/50 (84%), microlithiasis-induced pancreatitis n=33/43 (76.7%), gallstones-induced pancreatitis n=71/84 (84.5%)) and EUS (sludge-induced pancreatitis n=31/50 (62%), microlithiasis-induced pancreatitis n=16/43 (37%), gallstones-induced pancreatitis 30/84, n=(35.7%)) images and reports.
Results
Search results
Of the initial 1682 articles, 95 articles remained after screening and full-text eligibility assessment and were finally included (69 original articles, 26 review articles; see figure 1). Of the 69 original articles/studies included, 47 followed a prospective study design, 19 followed a retrospective study design, 2 were randomised-controlled studies and 1 followed a cross-sectional study design. In 13.0% (9/69) of the original studies reviewed and in 19.2% (5/26) of the review papers, the terms ‘biliary sludge’ and ‘microlithiasis’ were used as synonyms. In figures 2 and 3, the heterogeneity of the definitions used for the terms biliary microlithiasis and biliary sludge are shown schematically. The same is done for the size cut-off values for biliary microlithiasis derived from the studies. Regardless of the type of study (original paper or review), a lack of homogeneity regarding the definitions given in the studies was evident across all three categories.
Expert profile
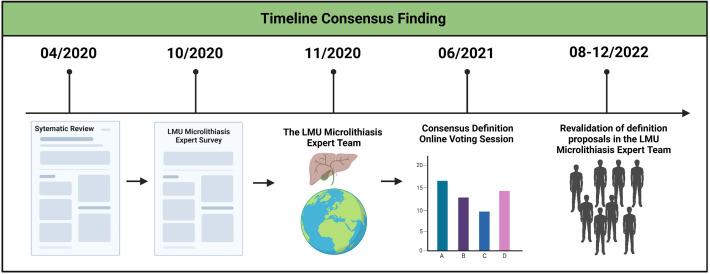
A total of 30 world-renowned experts in the field of endosonography-assisted diagnosis and therapy were contacted, of whom 28 (93.3%) started the survey, and 25 (83.3%) completed the survey questionnaire. All the experts contacted are subspecialised in gastroenterology, 65.5% of them with more than 20 years of professional experience. With 89.7% of survey participants active in endoscopy, 62.1% perform more than 100 endosonographies per year. 89.7% of participants are employed at tertiary care hospitals. The majority were distributed across European centres (72.4%), although experts from the USA, India and Egypt also participated. Details are provided in online supplemental table S1. In the second round of expert consultation, a total of 26 of the initial 30 EUS experts participated and voted on the three definition proposals resulting from the literature review, EUS expert survey round 1 and congress voting results. An overview of the timeline of the consensus process is shown in figure 4.
Figure 4.
LMU, Ludwig-Maximilians-University (Munich).
Diagnostic criteria for biliary sludge
Regarding the location of sludge or microlithiasis, 84% of the experts answered that both can be found in the gallbladder and in the bile tract. As the diagnostic imaging tool employed for detecting biliary sludge and microlithiasis, 93% of experts considered endosonography the most accurate based on their personal experience. Four per cent of respondents preferred transabdominal ultrasound, and 4% did not specify their gold standard. The statement that the term biliary sludge and microlithiasis should be used to define sonographic findings in both, the bile duct and the gallbladder was presented for online voting and received an 89.7% agreement (3.5% abstained from voting and 6.7% of online voters disagreed). In the expert survey, 76% agreed that biliary sludge should be diagnosed sonomorphologically as discrete, hyperechoic material inside the gallbladder or the bile duct, without acoustic shadowing, which sediments in the most dependent part of the gallbladder. This definition was accepted by online voting with 70.6% agreement (23.5% abstention and 5.9% rejection). In the final expert consultation round 2 with presentation of the literature results and congress voting results for review by the EUS expert panel, there was 100% agreement with the definition statement (see table 1, online supplemental table S3). Based on the controversial results of the literature search, an expert survey was made on the question of localisation, sonomorphology and the diagnostic tool of choice. The audience agreement was obtained through an online vote. The participants of the session ‘biliary pancreatitis’ had the opportunity to vote on the definition proposals consented.
Table 1.
Definition of biliary sludge
| Biliary sludge | Literature-based findings | Expert agreement | Audience agreement |
| Localisation | Gallbladder only | 0% | – |
| Bile duct only | 0% | – | |
| Gallbladder and bile duct | 100% | 89.7% | |
| Sonomorphology | Discrete, hyperechoic material (GB+CBD), without acoustic shadowing, sediment in the most dependent part of the GB | 96.15% | 70.6% |
| Imaging method of choice* | EUS | 93% | – |
| Transabdominal ultrasound | 4% | – |
*There is an obvious bias in this voting as first, mainly EUS experts were involved in the questionaire and second we did not discriminate between findings in the CBD and the gallbladder. Transabdominal ultrasound might be the method of choice for gallbladder findings.
CBD, common bile duct; EUS, endoscopic ultrasound; GB, Gallbladder.
Diagnostic criteria for biliary microlithiasis
In the experts’ survey, 93% of respondents selected EUS as the diagnostic tool of choice for diagnosing biliary microlithiasis as well as biliary sludge. Moreover, 76% of the experts voted against the obligatory use of phase-contrast and polarising light microscopy for making the diagnosis of microlithiasis. An explicit voting was recorded regarding the sonographic features of biliary microlithiasis. Regarding concrements’ size, 92% of the experts voted in favour of defining biliary microlithiasis as for cases in which examination of the biliary tree or gallbladder reveals the presence of stones ≤5 mm. Moreover, 76% voted for a size definition of size of less than 3 mm, 16% of the experts voted for a cut-off size of 5 mm. As most consistent definition derived from the survey a size definition of microlithiasis with stones ≥3 mm and ≤5 mm received 65.3% agreement (abstention: 13%, rejection: 21.7%) in the online voting process. In the expert survey round 2 with corresponding prior presentation of the systematic literature review and the audience online voting results, there was no majority for the microlithiasis size range ≥3 mm ≤5 mm (46.2% agreement). On the other hand, there was a majority for an upper microlithiasis limit of ≤5 mm with 57.7% agreement. As such the definition of microlithiasis which aimed highest consensus is as follows: The term ‘biliary microlithiasis’ should be used exclusively for calculi in the biliary tract and gallbladder of ≤5 mm in diameter with acoustic shadowing (see table 2, online supplemental table S3). Accordingly, biliary stones would be defined as calculi in the biliary tract and gallbladder of >5 mm in diameter with acoustic shadowing.
Table 2.
Agreement on definition of biliary microlithiasis
| Biliary microlithiasis | Literature-based findings | Expert agreement | Audience agreement |
| Concrement size | ≤5 mm | 11.54% | |
| ≤3 mm | 46.15% | – | |
| ≥3 mm ≤5 mm | 46.15% | 65.3% | |
| Imaging method of choice | EUS* | 93% | – |
| Bile sample centrifugation and examination by phase-contrast and polarising light microscopy | 16% | – | |
| Sonomorphology | With acoustic shadowing | 96.15% |
*There is an obvious bias in this voting as first, mainly EUS experts were involved in the questionaire and second we did not discriminate between findings in the CBD and the gallbladder. Transabdominal ultrasound might be the method of choice for gallbladder findings.
CBD, common bile duct; EUS, endoscopic ultrasound; GB, Gallbladder.
Clinical relevance and management of biliary sludge and microlithiasis
Expert discussion
The expert group was asked what clinical relevance they assign to the presence of biliary sludge/microlithiasis. Opinion was divided with 36% of expert attributing 10%–50% of idiopathic pancreatitis cases to the presence of biliary sludge or microlithiasis. On the other hand, 32% of experts attribute less than 10% of idiopathic acute pancreatitis to biliary sludge or microlithiasis. Whether the terms ‘biliary sludge’ and ‘biliary microlithiasis’ describe a similar finding (survey question no. 28) was rejected by 48%, while 40% agreed with it (with 12% experts abstaining). Regarding therapeutic options, 64% of the experts chose cholecystectomy as the method of choice. In comparison, 24% recommended endoscopic retrograde cholangiopancreatography (ERCP) with sphincterotomy for treating pancreatitis-related biliary sludge or microlithiasis. This was not the case in patients in whom it was stated that endosonography was not available as a gold standard to diagnose microlithiasis, but elevated liver function tests were detected (eg, alanine aminotransferase (ALAT) levels >150 U/L within 48 hours after onset of symptoms). In this setting, 32% of the experts recommended surgery, while 40% advised against it. ERCP (+SE) with 24% and ursodeoxycholic acid (UDCA) therapy with 20% received even less approval in the described scenario. On using ursodeoxycholic acid in patients with biliary sludge/microlithiasis to prevent complications and concrement dissolution, 64% of the experts responded that they only use UDCA in patients not qualifying for surgical or endoscopic intervention. Moreover, 28% of experts reported never using oral bile acid treatment in clinical practice as part of idiopathic pancreatitis treatment or prevention of sludge/microlithiasis.
Retrospective case analysis at University Hospital Munich-Großhadern
A retrospective evaluation of 177 biliary pancreatitis cases at LMU University Hospital (50 sludge-induced pancreatitis cases, 43 microlithiasis-induced pancreatitis cases and 84 gallstone-induced pancreatitis cases) showed that while sludge and microlithiasis according to the new consensus definition can obviously cause pancreatitis, severity and course does not differ from regular gallstone-induced pancreatitis (table 3). However, these data did not include follow-up results with respect of preventing recurrence of biliary pancreatitis and in light of the responses from the expert survey the question remains which treatment modality is adequate in balancing clinical risk and benefit.
Table 3.
Pancreatitis outcome stratified by underlying biliary entity
| Sludge-AP (n=50) | Microlithiasis-AP (n=43) | Gallstone-AP (n=84) | P value | |
| Severity (RAC), N (%) | 0.40 | |||
| Mild | 27 (54.0) | 29 (67.44) | 42 (50.0) | |
| Moderate | 18 (36.0) | 10 (23.25) | 34 (40.47) | |
| Severe | 5 (10.0) | 4 (9.3) | 8 (9.52) | |
| SIRS at admission, N (%) | 4 (8.0) | 2 (4.65) | 11 (13.09) | 0.28 |
| SIRS at hospital stay, N (%) | 8 (16) | 5 (11.62) | 16 (19.04) | 0.56 |
| Length of hospital stay (mean±SD in days) | 14.7±17.15 | 13.14±10.68 | 12.31±11.45 | 0.59 |
| IMC stay, N (%) | 5 (10.0) | 9 (20.1) | 17 (20.23) | 0.25 |
| ICU stay, N (%) | 5 (10.0) | 3 (6.9) | 8 (10.0) | 0.79 |
| ERCP, N (%) | 18 (36) | 20 (46.51) | 46 (54.76) | 0.18 |
| Concrement extraction rate, N (%) | 15 (75.0) | 12 (54.5) | 35 (72.9) | 0.24 |
| Post-ERCP pancreatitis rate | 0/18 (0) | 2/20 (10) | 0/84 (0) | 0.64 |
| Mortality, N (%) | 0 (0.0) | 0 (0.0) | 1 (1.19) | 0.57 |
| Cholecystectomy | ||||
| Yes | 21 (42.0) | 25 (58.13) | 46 (54.76) | 0.10 |
| No | 24 (48.0) | 11 (25.58) | 23 (27.38) | |
| Unknown | 5 (10.0) | 7 (16.27) | 15 (17.85) |
AP, acute pancreatitis; ERCP, endoscopic retrograde cholangiopancreatography; ICU, intensive care unit; IMC, intermediate care unit ; RAC, revised Atlanta classification; SIRS, systemic inflammatory response syndrome.
Discussion
Acute pancreatitis accounts for the most prevalent benign GI-disease leading to hospital admission. Up to 50% of cases are of biliary origin according to a combination of transabdomial ultrasound, clinical chemistry and EUS. At least up to 20% of the remaining idiopathic cases are caused by microlithiasis or biliary sludge often only diagnosed after recurrency.
It is, therefore, surprising that no uniform definition to accurately describe this frequent finding presently exists.19 20 Questions of clinical relevance regarding the terms biliary sludge and microlithiasis remain unsolved and have not been investigated in prospective studies for the lack of a universally valid definition of biliary sludge and microlithiasis. A recent study from the Netherlands with 41 participating experienced endosonographers showed that even in this preselected group of endoscopy experts, no diagnostic consensus could be reached regarding the findings of biliary sludge and microlithiasis (biliary sludge with slight agreement and microlithiasis with moderate agreement, measured according to Fleiss’ kappa). Regarding the therapeutic recommendations (based on video fragments), 51% of the experts voted in favour of ERCP and 49% of the experts voted against ERCP in patients with biliary sludge.21 22
In our retrospective evaluation stratified using the new consensus definition, no difference in pancreatitis severity was found between the initiating biliary entities gallstone versus microlithiasis versus sludge-induced pancreatitis. This indicates that the pathophysiological risk of sludge and microlithiasis in the pancreatitis context may be no less significant than that of gallstones and that a prospective evaluation for a more precise risk assessment is urgently needed to provide data for appropriate initial treatment as well as prevention of recurrence.
In this paper, we propose for the first time a unified and consented definition of biliary sludge and the size and echogenicity of biliary microlithiasis. The term biliary sludge should be reserved for sonomorphologically discrete, hyperechoic material, without acoustic shadowing and sedimenting in the most dependent part of the gallbladder and in the CBD. For biliary microlithiasis, a majority vote for a threshold ≤5 mm with acoustic shadowing in the EUS expert panel and the congress online vote was obtained. The cut-off of 5 mm is a reasonable threshold as lithiasis of this diameter, and lower will not provoke dilatation of the biliary tree as an immediate sign of CBD stones.23–25 Indeed, widely accepted guidelines emphasise the role of biliary duct dilatation as a key symptom in therapeutic decision-making, with a diameter ≤5 mm being accepted as a referenced cut-off for a regular diameter of the CBD on ultrasound imaging.26 27
The literature analysis exposed an evident lack of unified definition concerning biliary microlithiasis, especially with respect to lower and upper diameter limits. Most original publications and reviews used a cut-off value of more than 3 mm as lower limit. A majority of our experts voted for a cut-off value ≤5 mm. Microlithiasis in this case corresponds to small gallstones with a corresponding acoustic shadow. Since transabdominal ultrasound and endosonography are widely used as pancreaticobiliary diagnostic tool, the polarised light microscopy of bile obtained by cannulation of the bile duct is no longer used in clinical routine.11 28 29 The first pioneering studies described biliary sludge sonomorphologically as hyperechoic, non-shadowing material which is located in the most dependent part of the gallbladder.4 5 This definition is also consistent with the one used frequently in more recent reports.21 30
An inevitable variability can be observed in the literature concerning the pattern of the sludge-triggered echo signal. However, since the term (slightly) hyperechoic has predominantly been used to describe the echo behaviour over the last 20 years, this description was put forward for voting. A strong agreement rate of 96.15% in the expert survey and 70.6% in the participant voting confirmed the definition derived from the literature. In the literature, a sonomorphological description of sludge detected in the gallbladder is given in most publications, however, only one publication directly refers to sludge in the CBD.30–32 Therefore, participant voting with as very strong agreement of 100% confirmed the consensus definition that biliary sludge can also be detected in the CBD. We found an obvious controversy whether the terms ‘biliary sludge’ and ‘biliary microlithiasis’ describe an identical finding (please see survey question no. 28).
In line with this conflicting view both entities could cause clinically significant pain, cholangitis and pancreatitis and should be treated equally. This inconsistent expert consensus reflects the need of a unified definition of those entities. A distinction is made between acute (then no longer idiopathic but biliary driven) pancreatitis or biliary colic as clinical manifestations, which can be associated with biliary sludge or microlithiasis, and the microscopic morphology-based definition of sludge and microlithiasis. In the second case, biliary sludge and biliary microlithiasis are described primarily as conglomerates of primarily cholesterol monohydrate crystals. Biliary microlithiasis is often categorised as ‘small gallstones’ in clinical evaluation. Biliary sludge is described in the literature both as a precursor to microlithiasis and gallstones themselves. The coexistence of sludge alongside gallstones can also occur in clinical practice.12 29 33 34 Ros et al showed that 81.8% of patients with idiopathic acute pancreatitis and evidence of biliary crystals developed gallstones within the next 6 months. However, whether biliary sludge or microlithiasis should be classified as disease inflicting continues to depend primarily on the clinical context of the detection. Regarding treatment, most experts recommended cholecystectomy when sludge/microlithiasis is detected in idiopathic acute pancreatitis, but no agreement was reached on how to proceed when liver function tests suggest sludge/microlithiasis but EUS is not available. Interestingly, in the absence of an episode of idiopathic acute pancreatitis, ERCP with sphincterotomy was selected as the first choice of treatment once symptoms such as abdominal pain were reported in clinical case vignettes. This clearly indicates that only a widely used consensus definition will permit prospective trials addressing not only the clinical relevance of sludge and microlithiasis in the onset of pancreatitis but also in which way they should best be managed.
Conclusion
In summary, we conducted a systematic literature review followed by two rounds of an international expert survey and a live consensus meeting to arrive at a consensus definition for biliary sludge and biliary microlithiasis. The obtained definitions will permit to conduct prospective trials to determine the possibly different clinical relevance of these two entities as well as define the optimal treatment in order to prevent or treat pancreatitis of biliary origin.
gutjnl-2022-327955supp002.pdf (543.4KB, pdf)
Footnotes
MŻo and SS contributed equally.
Correction notice: This article has been corrected since it published Published Online. Missing content from the abstract has been added.
Collaborators: The LMU Microlithiasis Expert Survey Team listed in the online supplemental appendix.
Contributors: MZ, SS and JM study design, data acquisition and analysis, manuscript and figure preparation; UMM statistical analysis; GB, CS and JS study design and technical advice; SS, KB and MZ data acquisition; MML study design and manuscript preparation. JM acts as guarantor for this project.
Funding: JM and GB are funded by the Deutsche Forschungsgemeinschaft (DFG MA 4115/1-2/3, SFB1321: Project-ID 329628492, BE 6395/1 -1). MZ is funded by a United European Gastroenterology (UEG) Research Fellowship 2019 (award number N/A). SS is funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation)—413635475—and the Munich Clinician Scientist Program (MCSP) of the LMU Munich.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; internally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Opie EL. The relation OP cholelithiasis to disease of the pancreas and to fat necrosis. The American Journal of the Medical Sciences 1901;121:27–42. 10.1097/00000441-190101000-00002 [DOI] [Google Scholar]
- 2. Working Group IAP/APA Acute Pancreatitis Guidelines . IAP/apa evidence-based guidelines for the management of acute pancreatitis. Pancreatology 2013;13(4 Suppl 2):e1–15.:S1424-3903(13)00525-5. 10.1016/j.pan.2013.07.063 [DOI] [PubMed] [Google Scholar]
- 3. Ko CW, Sekijima JH, Lee SP. Biliary sludge. Ann Intern Med 1999;130:301–11. 10.7326/0003-4819-130-4-199902160-00016 [DOI] [PubMed] [Google Scholar]
- 4. Ros E, Navarro S, Bru C, et al. Occult microlithiasis in “idiopathic” acute pancreatitis: prevention of relapses by cholecystectomy or ursodeoxycholic acid therapy. Gastroenterology 1991;101:1701–9. 10.1016/0016-5085(91)90410-m [DOI] [PubMed] [Google Scholar]
- 5. Lee SP, Nicholls JF, Park HZ. Biliary sludge as a cause of acute pancreatitis. N Engl J Med 1992;326:589–93. 10.1056/NEJM199202273260902 [DOI] [PubMed] [Google Scholar]
- 6. Pereira R, Eslick G, Cox M. Endoscopic ultrasound for routine assessment in idiopathic acute pancreatitis. J Gastrointest Surg 2019;23:1694–700. 10.1007/s11605-019-04272-3 [DOI] [PubMed] [Google Scholar]
- 7. Umans DS, Timmerhuis HC, Hallensleben ND, et al. Role of endoscopic ultrasonography in the diagnostic work-up of idiopathic acute pancreatitis (PICUS): study protocol for a nationwide prospective cohort study. BMJ Open 2020;10:e035504. 10.1136/bmjopen-2019-035504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Umans DS, Rangkuti CK, Sperna Weiland CJ, et al. Endoscopic ultrasonography can detect a cause in the majority of patients with idiopathic acute pancreatitis: a systematic review and meta-analysis. Endoscopy 2020;52:955–64. 10.1055/a-1183-3370 [DOI] [PubMed] [Google Scholar]
- 9. Mariani A, Arcidiacono PG, Curioni S, et al. Diagnostic yield of ERCP and secretin-enhanced MRCP and EUS in patients with acute recurrent pancreatitis of unknown aetiology. Dig Liver Dis 2009;41:753–8. 10.1016/j.dld.2009.01.009 [DOI] [PubMed] [Google Scholar]
- 10. Thevenot A, Bournet B, Otal P, et al. Endoscopic ultrasound and magnetic resonance cholangiopancreatography in patients with idiopathic acute pancreatitis. Dig Dis Sci 2013;58:2361–8. 10.1007/s10620-013-2632-y [DOI] [PubMed] [Google Scholar]
- 11. Dahan P, Andant C, Lévy P, et al. Prospective evaluation of endoscopic ultrasonography and microscopic examination of duodenal bile in the diagnosis of cholecystolithiasis in 45 patients with normal conventional ultrasonography. Gut 1996;38:277–81. 10.1136/gut.38.2.277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Alexakis N, Lombard M, Raraty M, et al. When is pancreatitis considered to be of biliary origin and what are the implications for management? Pancreatology 2007;7:131–41. 10.1159/000104238 [DOI] [PubMed] [Google Scholar]
- 13. Frossard JL, Sosa-Valencia L, Amouyal G, et al. Usefulness of endoscopic ultrasonography in patients with “idiopathic” acute pancreatitis. Am J Med 2000;109:196–200. 10.1016/s0002-9343(00)00478-2 [DOI] [PubMed] [Google Scholar]
- 14. Yusoff IF, Raymond G, Sahai AV. A prospective comparison of the yield of EUS in primary vs. recurrent idiopathic acute pancreatitis. Gastrointest Endosc 2004;60:673–8. 10.1016/s0016-5107(04)02018-8 [DOI] [PubMed] [Google Scholar]
- 15. Räty S, Pulkkinen J, Nordback I, et al. Can laparoscopic cholecystectomy prevent recurrent idiopathic acute pancreatitis?: a prospective randomized multicenter trial. Ann Surg 2015;262:736–41. 10.1097/SLA.0000000000001469 [DOI] [PubMed] [Google Scholar]
- 16. Mentula P. Effect of laparoscopic cholecystectomy after idiopathic acute pancreatitis may be overestimated. Ann Surg 2017;266:e77–8. 10.1097/SLA.0000000000001612 [DOI] [PubMed] [Google Scholar]
- 17. Said M, Rongen APM. Can laparoscopic cholecystectomy prevent recurrent idiopathic acute pancreatitis? Ann Surg 2017;266:e94–5. 10.1097/SLA.0000000000001748 [DOI] [PubMed] [Google Scholar]
- 18. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Peery AF, Crockett SD, Murphy CC, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the united states: update 2018. Gastroenterology 2019;156:254–72. 10.1053/j.gastro.2018.08.063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. O’Morain N, O’Morain C. The burden of digestive disease across Europe: facts and policies. Digestive and Liver Disease 2019;51:1–3. 10.1016/j.dld.2018.10.001 [DOI] [PubMed] [Google Scholar]
- 21. Quispel R, Schutz HM, Hallensleben ND, et al. Do endosonographers agree on the presence of bile duct sludge and the subsequent need for intervention? Endosc Int Open 2021;9:E911–7. 10.1055/a-1452-8919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Beyer G, Hoffmeister A, Michl P, et al. S3-leitlinie pankreatitis – leitlinie der deutschen gesellschaft für gastroenterologie, verdauungs- und stoffwechselkrankheiten (DGVS) – september 2021 – AWMF registernummer 021-003. Z Gastroenterol 2022;60:419–521. 10.1055/a-1735-3864 [DOI] [PubMed] [Google Scholar]
- 23. Niederau C, Müller J, Sonnenberg A, et al. Extrahepatic bile ducts in healthy subjects, in patients with cholelithiasis, and in postcholecystectomy patients: a prospective ultrasonic study. J Clin Ultrasound 1983;11:23–7. 10.1002/jcu.1870110106 [DOI] [PubMed] [Google Scholar]
- 24. Sienz M, Ignee A, Dietrich CF. Reference values in abdominal ultrasound-biliopancreatic system and spleen. Z Gastroenterol 2011;49:845–70. 10.1055/s-0031-1273362 [DOI] [PubMed] [Google Scholar]
- 25. Benjaminov F, Leichtman G, Naftali T, et al. Effects of age and cholecystectomy on common bile duct diameter as measured by endoscopic ultrasonography. Surg Endosc 2013;27:303–7. 10.1007/s00464-012-2445-7 [DOI] [PubMed] [Google Scholar]
- 26. Manes G, Paspatis G, Aabakken L, et al. Endoscopic management of common bile duct stones: European Society of gastrointestinal endoscopy (ESGE) guideline. Endoscopy 2019;51:472–91. 10.1055/a-0862-0346 [DOI] [PubMed] [Google Scholar]
- 27. Beyer G, Kasprowicz F, Hannemann A, et al. Definition of age-dependent reference values for the diameter of the common bile duct and Pancreatic duct on MRCP: a population-based, cross-sectional cohort study. Gut 2023;72:1738–44. 10.1136/gutjnl-2021-326106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kohut M, Nowak A, Nowakowska-Duiawa E, et al. Presence and density of common bile duct microlithiasis in acute biliary pancreatitis. World J Gastroenterol 2002;8:558–61. 10.3748/wjg.v8.i3.558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jacobson BC, Waxman I, Parmar K, et al. Endoscopic ultrasound-guided gallbladder bile aspiration in idiopathic pancreatitis carries a significant risk of bile peritonitis. Pancreatology 2002;2:26–9. 10.1159/000049444 [DOI] [PubMed] [Google Scholar]
- 30. Hill PA, Harris RD. Clinical importance and natural history of biliary sludge in outpatients. J Ultrasound Med 2016;35:605–10. 10.7863/ultra.15.05026 [DOI] [PubMed] [Google Scholar]
- 31. Venneman NG, van Brummelen SE, van Berge-Henegouwen GP, et al. Microlithiasis: an important cause of “idiopathic” acute pancreatitis? Ann Hepatol 2003;2:30–5. [PubMed] [Google Scholar]
- 32. Anderloni A, Galeazzi M, Ballarè M, et al. Early endoscopic ultrasonography in acute biliary pancreatitis: a prospective pilot study. World J Gastroenterol 2015;21:10427–34. 10.3748/wjg.v21.i36.10427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Levy MJ. The HUNT for microlithiasis in idiopathic acute recurrent pancreatitis: should we abandon the search or intensify our efforts? Gastrointest Endosc 2002;55:286–93. 10.1067/mge.2002.121224 [DOI] [PubMed] [Google Scholar]
- 34. Şurlin V, Săftoiu A, Dumitrescu D. Imaging tests for accurate diagnosis of acute biliary pancreatitis. World J Gastroenterol 2014;20:16544–9. 10.3748/wjg.v20.i44.16544 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
gutjnl-2022-327955supp001.pdf (11.8MB, pdf)
gutjnl-2022-327955supp002.pdf (543.4KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information.