Abstract
Clinical trials targeting the gut microbiome to mitigate ocular disease are now on the horizon. A review of clinical data thus far is essential to determine future directions in this novel promising field. This review examines recent clinical trials that support the plausibility of a gut-eye axis, and may form the basis of novel clinical interventions. PubMed was queried for English language clinical studies examining the relationships between gut microbiota and ocular pathology. 25 studies were extracted from 828 candidate publications, which suggest that gut imbalance is associated with ocular pathology. Of these, only four interventional studies exist which suggest probiotic supplementation or fecal microbiota transplant can reduce symptoms of chalazion or uveitis. The gut-eye axis appears to hold clinical relevance, but current data is limited in sample size and design. Further investigation via longitudinal clinical trials may be warranted.
Subject terms: Predictive markers, Epidemiology
Abstract
靶向调节肠道微生物从而减轻眼部疾病的临床试验目前即将拉开帷幕。对迄今为止的临床数据进行回顾, 在确定这一具有前途的新领域的未来发展方向上至关重要。本文综述了最新的支持肠-眼轴的合理性临床试验, 这些临床实验的结果可能成为新的临床干预策略的基础。本文使用PubMed查询了关于肠道菌群与眼部疾病相关性的英文临床研究。从828篇候选文献中筛选了25篇研究, 这些研究表明肠道失衡与眼部疾病的病理相关。其中, 只有4项介入性研究表明, 补充益生菌或移植粪便微生物群可以减轻霰粒肿或葡萄膜炎的症状。肠-眼轴体现了临床相关性, 但目前的数据在样本量和设计方面均具有局限性。需要通过纵向临床试验进行进一步的验证。
Introduction
The human microbiome is a diverse ecosystem that has been attributed to play a major role in the health of cardiovascular and neurologic organ systems over the past decade [1–3]. Emerging evidence also supports the presence of a gut-eye axis, suggesting alterations of the gut microbiome as a potential contributing factor to ocular pathology [4, 5]. Gut dysregulation can be defined by various metrics; the ratio of the taxonomic phyla Firmicutes to Bacteroides (F/B), total species richness, total species diversity, or alterations in bacterial marker profiling on the genus or species level [6, 7]. These metrics have been studied in various pre-clinical models examining the gut-eye-axis with supporting results.
Nakamura et al. and Horai et al. examined mouse models of uveitis in antibiotic treated and germ-free specimens, respectively. Both studies found decreases in experimental autoimmune uveitis scores in the antibiotic and germ-free models, suggesting gut microbiota contribute to the pathogenesis of uveitis models [8, 9]. Rowan et al. in 2017 examined mouse models of Age-related Macular Degeneration (AMD), finding AMD phenotypes were associated with increased Clostridiales and decreased Bacteroidetes [10]. With respect to glaucoma, mouse models have shown an absence of retinal degeneration when raised under germ-free conditions compared to mice with intact gut microbiota [11]. Murine models of diabetic retinopathy have also shown alterations in gut microbial composition relative to control mice [12]. These preclinical studies linked ocular health to gut microbial diversity and health, however, the therapeutic potential remains to be established.
Therapeutic protocols have been implemented in murine models targeting the gut microbiome to improve ocular pathologies. Restructuring the microbiome by intermittent fasting in diabetic mouse models, reduces activation of retinal microglia and development of acellular capillaries, which is theorized to protect the retina against diabetic damage [13]. Additionally, engineered probiotics have been shown to act as effective vectors for the delivery of therapeutic proteins to protect against retinal and systemic damage [14].
Based on murine experimentation, clinical studies examining the human microbiome and its relationship with ocular pathology have begun. Pathologies such as uveitis, age-related macular degeneration, glaucoma, dry eye syndrome, and chalazions are being explored, with hopes of expanding the therapeutic frontier. This systematic review aims to summarize known clinical studies examining the gut-eye-axis, with a focus on potential therapeutics aimed at modifying the microbiome to mitigate ocular pathology.
Materials/subjects and methods
PubMed and Cochrane databases were searched with the following query: ((microbiome) AND (“eye” OR “ocular” OR “ophthalmology”)). Inclusion criteria were as follows: English language, study of human subjects, and focused on the impact of gut-microbiota on ocular health. Exclusion criteria were as follows: studies not addressing the impact of gut microbiota on ocular health. Literature reviews, editorials, conference abstracts, correspondence, and notes were also excluded. The full text of each article was reviewed independently by BLK and MWR. Additional articles were identified from a manual search of reference lists within included articles. Disagreements were resolved by AKW.
Clincialtrials.gov was searched using “eye disease” as a disease and other terms (“microbiome” OR “probiotics” OR “FMT”). Only ongoing trials utilizing oral probiotics for management of ophthalmic diseases were reviewed.
Results
After screening 828 candidate publications, a total of 25 studies were included. A PRISMA diagram can be found in Fig. 1. Microbes associated with disease states can be found in Table 1. In the 21 studies that performed sequencing for microbiome assessment, 20 studies noted gut-microbial change compared to healthy control patients (Table 2). Twelve studies examined retinal pathology, nine studies examined autoimmune conditions or uveitis, and four studies examined either corneal or anterior ocular pathology. Four studies assessed interventions targeting the gut-microbiome in attempt to mitigate ocular pathology. Quality of evidence of studies is outlined in Table 3 according to modified Oxford Centre for Evidence Based Medicine Levels of Evidence guidelines (Table 3) [15]. Infographic depicting studies examining microbiome and ocular pathology can be seen in Supplementary Fig. 1. Two ongoing clinical trials were found in the clinical trial database, examining probiotics in management of blepharitis and Allergic Rhinoconjunctivitis (NCT04742855, NCT04898686) [16, 17].
Fig. 1. PRISMA diagram of study review and selection process.
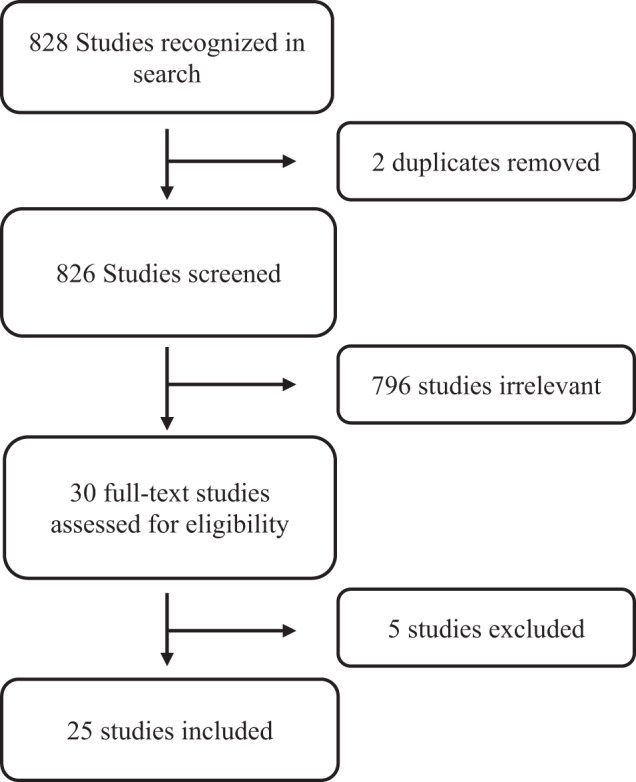
From a total of 828 studies identified from the initial query, 25 were ultimately included in the final analysis.
Table 1.
Microorganisms highlighted in dysbiosis of disease states.
| Disease category | Implicated microorganisms |
| Diabetes and Diabetic Retinopathy | ↑ Bacteriodes:Firmicutes: ratio. ↓ Bacteroidetes, Actinobacteria, Faecalibacterium, Clostridium, Escherichia-Shigella, Coriobacteriaceae, Veillonellaceae, Streptococcaceae. ↑ Bifidobacterium, Burkholderiaceae |
| Age related Macular Degeneration | ↑ Ruminococcus, Oscillibacter, Anaerotruncus, Eubacterium |
| Retinal Artery Occlusion | ↑ Actinobacter,Bifidobacterium, Bacteroides, Faecalibacterium |
| Retinopathy of Prematurity | ↑ Enterobacteriaceae |
| Glaucoma | ↑ Prevotellaceae, Enterobacteriaceae, Escherichia coli ↓ Megamonas, Bacterioides |
| Idiopathic intracranial hypertension | ↓ Lactobacillus, Atopobium, Megamonas, Ruminococcus, Streptococcus |
| Uveitis | ↑ Malassezia, Candida,Candida, ↑ Aspergillus gracilis ↓Faecalibacterium, Lachnospira, Ruminococcus, Bacteroides |
| Behcet Syndrome | ↑ Veillonellaceae, Succinivibrionaceae, ↓ Bacteroidaceae |
| Sjogren Syndrome |
↑ Bacteriodetes: Firmicutes: Bacteroidetes ratio ↓ Faecalibacterium, Prevotella, and Ruminococcus, Actinobacteria, Bifidobacterium, Dorea, Agathobacter ↑ Alistipes, Streptococcus, Prevotella, Odoribacter, Actinomycetaceae, Eggerthellaceae, Lactobacillaceae, Akkermanciaceae, Coriobacteriaceae, and Eubacteriaceae |
| Keratitis | ↓ Bifidobacterium, Lactospira, Faecalibacterium, Lachnospira, Ruminococcus, Mitsuokella Megasphera Lachnospiraceae, Dialister, Faecalibacterium, Firmicutes, Veillonellaceae, |
Table 2.
Ocular clinical studies examining gut dysbiosis.
| General | Measurement of microbiome | Intervention if applicable | Outcomes | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author, Date | Title | Study type | Participants (# pts with which disease) | Age of cohorts | Gender (% female) | Racial information | Disease category | Primary Ocular Outcome | GI outcomes? | Microbiome Notes | Bacteria specific notes | ||
| Watane et al. [44] | Fecal Microbial Transplant in Individuals With Immune-Mediated Dry Eye. | Nonrandomized clinical trial | 10 patients diagnoses with Dry Eye due to Sjogren Syndrome | 60.4 years old | 70% | 50% white, 50% hispanic | Sjogren Syndrome | Fecal DNA sequencing | Fecal microbiota transplant | Reduction in self reported Dry Eye symptoms 5/10 patients 3 month FU | No side effects noted of FMT | SS: decreased abundance of genera Faecalibacterium, Prevotella, and Ruminococcus and an increased abundance of genera Alistipes, Streptococcus, and Blautia relative to healthy donor biome. | Faecalibacterium noted to be decreased in prior Dry Eye study |
| McPherson et al. [25] | Irritable bowel syndrome and risk of glaucoma: An analysis of two independent population-based cohort studies. | Analysis of two prospective cohort studies | 71362 IBS patients, 625410 age matched controls | n/a | 51.50% | 97.9 % white | Glaucoma | none | none | Increased odds of developing glaucoma if IBS present (OR = 5.84) | none | none | none |
| Das et al. [18] | Alterations in the gut bacterial microbiome in people with type 2 diabetes mellitus and diabetic retinopathy. | Cross sectional study | 25 patients with diabetes 28 patiens with DR 30 healthy controls | 57.3 55.07 52.2 | 44% 25% 43% | n/a | Diabetes and Diabetic Retinopathy | 16s RNA sequencing | none | none | Dysbiosis most pronounced in patients with retinopathy compared to diabetics or controls. | DR: ↓ Bacteroidetes and Actinobacteria versus HC | ↑ Shannon diversity in DM and DR versus HC |
| Filippelli et al. [46] | Intestinal microbiome: a new target for chalaziosis treatment in children? | Prospective pilot study | 26 children with chalazions | 8.3 | 65% | n/a | Chalazion | none | Probiotic supplementation | Decreased time to resolution of Chalazion in probiotic group (P < 0.0001) | no adverse effects | Probiotic contained Streptococcus thermophilus, Lactococcus lactis, & Lactobacillus delbrueckii | |
| Berkowitz et al. [27] | “More Guts Than Brains?”-The Role of Gut Microbiota in Idiopathic Intracranial Hypertension. | Prospective pilot study | 25 patients with IIH 20 healthy control patients | 35.12 48.5 | n/a | n/a | Idiopathic intracranial hypertension | Fecal DNA sequencing | acetazolamide examined in IIH patients | none | IIH patients had lower microbiota diversity compared to control, Acetazolamide treated patietns showed increased lactobacillus | IIH: ↓ Lactobacillus ruminis, ↓ Atopobium parvulum, ↓ Megamonas hypermegale, ↓ Ruminococcus gnavus, ↓ Streptococcus sp. (beneficial microbiota) | Acetazolamide treated patients: ↑ Lactobacillus brevis (beneficial microbiota |
| Filippelli et al. [45] | Effectiveness of oral probiotics supplementation in the treatment of adult small chalazion. | Prospective pilot study | 20 adults with chalazion | 48.25 | 65% | n/a | Chalazion | none | Probiotic supplementation | Decreased time to resolution of small size Chalazion in probiotic group (P < 0.039) Failure to resolve medium or large chalaion ≥ 2 mm | no adverse effects | Probiotic contained Streptococcus thermophilus, Lactococcus lactis, & Lactobacillus delbrueckii | |
| Moubayed et al. [59] | Screening and identification of gut anaerobes (Bacteroidetes) from human diabetic stool samples with and without retinopathy in comparison to control subjects. | Cross sectional study | 9 patients with diabetes 8 Patients with DR 18 healthy controls | n/a | 44% 25% 43% | n/a | Diabetes and Diabetic Retinopathy | Fecal DNA sequencing | none | Higher ratio of bacteroides in diabetic groups than controls, No difference between those with and without retinopathy | DM & DR: ↑ Bacteriodetes, ↓ Firmicutes: ratio, | ||
| Napolitano et al. [47] | Probiotic Supplementation Improved Acute Anterior Uveitis of 3-Year Duration: A Case Report. | Case Report | 1 patient with autoimmune uveitis | 21 | 100% | n/a | Uveitis | none | probiotic supplementation | BCVA from 3/10 to 4/10 and decreased proteins and mutton-fat deposits after 2 months | none | Probiotic contained Bifidobacterium lacti, Bifidobacterium bifidum, & Bifidobacterium breve | |
| Huang et al. [20] | Dysbiosis and Implication of the Gut Microbiota in Diabetic Retinopathy. | Cross sectional study |
25 DM without DR 25 DM with DR 25 healthy controls |
62.5 60.3 57.8 |
56% 40% 64% |
100% Chinese | Diabetes and Diabetic Retinopathy | 16 S RNA sequencing | none | none | Reduced diversity in both DM and DR groups compared to control group. | DM & DR: ↑ Bifidobacterium, ↑ Lactobacillus, ↓ Bacteriodetes, ↓ Escherichia-Shigella, ↓ Faecalibacterium, ↓ Eubacterium_hallii_group, ↓ Clostridium versus HC | ↓ α and β diversities in the DM and DR groups compared with HC group |
| Jayasudha et al. [33] | Implicating Dysbiosis of the Gut Fungal Microbiome in Uveitis, an Inflammatory Disease of the Eye. | Cross sectional study |
24 healthy controls 14 uveitis patients |
45.9 43.6 |
85% | 100% Indian | Uveitis | Fungal RNA sequencing | none | none | gut fungal richness and diversity were significantly decreased in uveitis patients compared to healthy controls | UVT: ↑ Malassezia restricta, ↑ Candida albicans, ↑ Candida glabrata, ↑ Aspergillus gracilis (pathogenic) | |
| Chakravarthy et al. [34] | Alterations in the gut bacterial microbiome in fungal Keratitis patients. | Cross sectional study |
31 healthy controls 32 fungal keratitis |
42.2 47.1 |
51.6% 40.6% |
100% Indian | Keratitis | 16 s RNA sequencing | none | none | no significant difference in fungal dysbiosis, but bacterial richness and diversity in FK patients was significantly decreased | Keratitis: ↓Bifidobacterium, ↓Lactospira, ↓Faecalibacterium, ↓Lachnospira, ↓Ruminococcus, ↓ Mitsuokella, ↓ Megasphera and ↓ Lachnospiraceae (antiinflammatory mircobiota) | Keratitis: ↑ Aspergillus, ↑ Candida (pathogenic mycobiota) |
| Zysset-Burri et al. [42] | Retinal artery occlusion is associated with compositional and functional shifts in the gut microbiome and altered trimethylamine-N-oxide levels. | Cross sectional study |
29 non arteritic RAO 30 healthy controls |
69.4 69.0 |
51.7% 46.7% |
n/a | Retinal Artery Occlusion | Fecal DNA sequencing | none | none | alterations in gut microbiome and elevated TMAO (risk factor for CV dz) levels in patients with RAO | RAO: ↑ Actinobacter,↑ Bifidobacterium,↑ Bacteroides stercoris, ↑Faecalibacterium prausnitzii | TMAO significantly higher in patients with RAO, p = 0.023 |
| Skondra et al. [60] | The early gut microbiome could protect against severe retinopathy of prematurity. | Cross sectional study |
6 type 1 ROP neonates 4 preterm neonates with similar baseline comorbidities |
24.1 weeks 25.6 weeks |
n/a | n/a | Retinopathy of Prematurity | 16 s RNA sequencing | none | none | significant enrichment of enterobacteriaceae in type 1 ROP patients, with decreased amino acid metabolism pathways | Enterobacteriaceae enrichment in ROP patients at 28 weeks (P < 0.05) | |
| Jayasudha et al. [35] | Alterations in gut bacterial and fungal microbiomes are associated with bacterial Keratitis, an inflammatory disease of the human eye. | Cross sectional study |
21 health controls 19 bacterial keratitis |
48.8 | n/a | 100% Indian | Keratitis | Fecal DNA sequencing | none | none | increase in number of anti-inflammatory organisms in HC compared to BK | Keratitis: ↓Dialister, ↓Megasphera, ↓Faecalibacterium, ↓Lachnospira, ↓Ruminococcus, ↓ Mitsuokella, ↓ Firmicutes, ↓ Veillonellaceae, and ↓ Lachnospiraceae (antiinflammatory mircobiota) | Keratitis: ↑ Aspergillus, ↑ Malassezia (pathogenic mycobiota) |
| Chakravarthy et al. [34] | Dysbiosis in the Gut Bacterial Microbiome of Patients with Uveitis, an Inflammatory Disease of the Eye. | Cross sectional study |
13 uveitis 13 healthy controls |
44.5 43.1 |
84.6% 84.6% |
100% indian | Uveitis | 16 s RNA sequencing | none | none | reduced diversity of several anti-inflammatory organisms in uveitis patients microbiomes and decreased probiotic and antibacterial organisms | UVT: ↓ Faecalibacterium, ↓Lachnospira, ↓Ruminococcus, ↓ Ruminococcaceae and ↓ Bacteroides (antiinflammatory mircobiota) | |
| Khan et al. [61] | Association Between Gut Microbial Abundance and Sight-Threatening Diabetic Retinopathy. | Case control study |
37 sight threatening DR 21 DM no DR |
57.5 57.5 |
33.4% 38.1% |
n/a | Diabetes and Diabetic Retinopathy | bacteroidetes to firmicutes ratio (B/F) | none | none | No difference in gut microbioal abundance between the 2 populations | DR: Increased Bacteroides:Furmicutes ratio compared to controls, p = 0.049 | |
| Yasar Bilge et al. [38] | Intestinal microbiota composition of patients with Behçet’s disease: differences between eye, mucocutaneous and vascular involvement. The Rheuma-BIOTA study. | prospective observational study |
27 Behcet’s 10 control |
40.8 38.9 |
63.0% 60% |
n/a | Behcet Syndrome | 16s RNA sequencing | none | none | significant differences in the relative abundance of some bacterial taxa between patients with BD and healthy controls | UVT: Differences in Lachnospiraceae | |
| Moon et al. [62] | Gut dysbiosis is prevailing in Sjögren’s syndrome and is related to dry eye severity. | Prospective case-control study |
12 healthy controls 10 with Sjogren’s 14 with envrionmental dry eye syndrome (DES) |
47.5 58.5 46.3 |
100% 85.7% 75% |
100% Korean | Sjogren Syndrome | 16s RNA sequencing | none | Bacteriodetes, Actinobacteria, and Bifidobacterium significantly related to dry eye signs (NEI score, tear breakup time) (p < 0.05) Multivariate linear regression showed that tear secretion was strongly affected by Prevotella | gut microbiome showed significant differences in patients with Sjogrens than compared to controls & DES; no significant difference in alpha-diversity across all 3 groups |
SS: ↑ Bacteriodetes, ↓ Firmicutes: Bacteroidetes ratio, ↓Actinobacteria, ↓ Bifidobacterium (compared to control and DES). ↓ Blautia, Dorea, Agathobacter (vs. controls). ↑ Prevotella, Odoribacter, Alistipes (vs. DES) DES: ↑ Veillonella and ↓ Subdoligranulum (vs. controls) |
-↓ Firmicutes: Bacterioidetes ratio is known to be an early sign of gut dybsiosis -Chronic inflammatory dx (SLE, systemic sclerosis) show ↑ Bacteroidetes and reduced ratio, with ↓ Bifidobacterium and Lactobacillus -Actinobacteria (Bifidobacterium & Collinsella) thought to help with intestinal health due to regulating pathogens -Prevotella associated with rheum. arthritis |
| Gong et al. [26] | Gut microbiota compositional profile and serum metabolic phenotype in patients with primary open-angle glaucoma. | Prospective study |
30 POAG patients 30 non-POAG patients/ controls |
54.8 53.8 |
53.3% 53.3% |
100% Chinese | Glaucoma | 16 s RNA sequencing | none | Mean VA in POAG patients negatively correlated with Blautia (p = 0.034) Mean VF-MD in POAG patients negatively correlated with Megamonas (p = 0.035) average RNFL thickness positively correlated with Streptococcus (p = 0.037) | Bacterial profiles in the gut microbiome had significant differences between the POAG and control patients | POAG: ↑ Prevotellaceae, unidentified_Enterobacteriaceae, Escherichia coli, ↓ Megamonas, Bacterioides_plebeius (vs. controls) | Prevotella shown in mouse models to worsen epithelial inflammation in colitis and thrived in pro-inflammatory environments |
| Ye et al. [19] | Alterations of the Gut Microbiome and Metabolome in Patients With Proliferative Diabetic Retinopathy. | Prospective study |
45 PDR patients 90 T2M without DR (controls) |
59.9 60.9 |
44.4% 44.4% |
100% Chinese (Han) | Diabetes and Diabetic Retinopathy | 16 s RNA sequencing | none | none | PDR associated with reduced microbiome diversity than controls, with significant depletion of 22 familes and enrichment of 2 familes in the PDR group | PDR: ↓ Coriobacteriaceae, Veillonellaceae, Streptococcaceae and ↑ Burkholderiaceae and Burkholderiales_unclassified (vs. controls) | |
| Zinkernagel et al. [23] | Association of the Intestinal Microbiome with the Development of Neovascular Age-Related Macular Degeneration. | Cross-sectional |
12 nAMD 11 controls |
78.4 72.5 |
33.3% 36.4% |
N/A | Age related Macular Degeneration | Fecal DNA sequencing | none | none | Different bacterial compositions noted in the AMD cohort compared to controls |
nAMD: ↑ Ruminococcus torque, Oscillibacter, Anaerotruncus, Eubacterium ventriosum Controls: ↑ Bacteroides eggerthii |
Prior studies have associated Anaerotruncus and Eubacterium with increased inflammatory states/ elevated cytokine levels |
| Huang et al. [32] | Gut Microbiota Composition and Fecal Metabolic Phenotype in Patients With Acute Anterior Uveitis. | Cross-sectional |
38 AAU 40 controls |
33.9 36.0 |
36.8% 35% |
N/A | Uveitis | 16 s RNA sequencing | none | none | No significant difference in gut microbiota composition between AAU and controls; but fecal metabolite phenotype in AAU patients was significantly different from healthy controls | UVT: ↓ Roseburia, Lachnospiracea, Dorea, Blautia, Clostridum, Odoribacter, ↑ Veillonella (vs. controls) -- however significance for all were LOST after false discovery rate (FDR) correction | Roseburia and Veillonella positively correlates to linoleic acid (stimulates proinflammatory mediators in IBD) |
| Tecer et al. [37] | Succinivibrionaceae is dominant family in fecal microbiota of Behçet’s Syndrome patients with uveitis. | Case-control |
7 Behcet syndrome(BS) + uveitis 12 Familial Mediterranean Fever (FMF) 9 Crohns Disease (CD) 16 healthy controls (HC) |
35.6 32.2 35.0 39.4 |
28.6% 50% 66.6% 62.5% |
N/A | Behcet Syndrome | 16 s RNA sequencing | none | none | Significant differences in alpha diversity between the four groups. Prevotella copri was dominant in BS group (a known inflammatory bacteria) |
BS: ↑ Veillonellaceae, Succinivibrionaceae, ↓ Bacteroidaceae (vs. controls) Prevotella copri was a predominant species in the BS, HC, and FMF groups but not the controls |
Prevotella copri is a known inflammatory bacteria |
| Jayasudha et al. [21] | Gut mycobiomes are altered in people with type 2 Diabetes Mellitus and Diabetic Retinopathy. | Cross-sectional |
24 T2DM with DR 21 T2DM 30 Healthy controls |
54.5 57.5 52.2 |
25% 38.1% 43.3% |
100% Indian | Diabetes and Diabetic Retinopathy | Fungal RNA s‘ | none | none | More mycobiome dysbiosis in people with T2DM and DR than compared to healthy controls; mycobiome profiles and beta diversity differed between all three groups to some extent |
21 genera ↓ and 5 genera ↑ in T2DM (Table 3), 18 genera reduced in DR (Table 4) [vs. controls] 6 genera ↓ in DR [vs. T2DM] (Table 5) |
|
| Mendez et al. [63] | Gut microbial dysbiosis in individuals with Sjögren’s syndrome. | Prospective case control |
13 Sjogrens + dry eye 8 Sjogrens without dry eye 21 healthy controls |
58.8 58.4 26.0 |
69% 62% 0% |
N/A | Sjogren Syndrome | 16 s RNA sequencing | none | Various classes of bacteria associated with signs/ symptoms of dry eye (Table 2 in table lists all of them) | Shannon’s diversity index showed no difference between groups. Faith’s phylogenetic diversity showed increased diversity in patients with Sjogrens vs. controls, especially for Sjogrens+dry eye vs. control (p = 0.02) | No differences in Bateroides:Firmicutes ratio between Sjogrens/ controls No significant difference between SDE and NDE groups in Sjogrens or difference in alpha-diversity Sjogrens overall: ↑ Actinomycetaceae, Eggerthellaceae, Lactobacillaceae, Akkermanciaceae, Coriobacteriaceae, and Eubacteriaceae (vs. controls) | |
Table 3.
Quality of evidence in studies examined.
| Author, Date | Study type | Quality of Evidence |
|---|---|---|
| Watane et al. [44] | Nonrandomized clinical trial | 2 |
| McPherson et al. [25] | Prospective cohort | 2 |
| Das et al. [18] | Cross-sectional | 4 |
| Filippelli et al. [47] | Prospective pilot | 2 |
| Berkowitz et al. [27] | Case-Control | 3 |
| Filippelli et al. [45] | Prospective pilot | 2 |
| Moubayed et al. [59] | Cross-sectional | 4 |
| Napolitano et al. [47] | Case Report | 5 |
| Huang et al. [20] | Cross-sectional | 4 |
| Jayasudha et al. [33] | Cross-sectional | 4 |
| Chakravarthy et al. [34] | Cross-sectional | 4 |
| Zysset-Burri et al. [42] | Cross-sectional | 4 |
| Skondra et al. [60] | Cross-sectional | 4 |
| Jayasudha et al. [35] | Cross-sectional | 4 |
| Chakravarthy et al. [34] | Cross-sectional | 4 |
| Khan et al. [61] | Case-Control | 3 |
| Yasar Bilge et al. [38] | Case-Control | 3 |
| Moon et al. [62] | Case-Control | 3 |
| Gong et al. [26] | Case-Control | 3 |
| Ye et al. [19] | Case-Control | 3 |
| Zinkernagel et al. [23] | Cross-sectional | 4 |
| Huang et al. [32] | Cross-sectional | 4 |
| Tecer et al. [37] | Case-Control | 3 |
| Jayasudha et al. [21] | Cross-sectional | 4 |
| Mendez et al. [63] | Case-Control | 3 |
Results
Microbial community changes in ocular pathologies
In general, the studies reviewed herein display a broad degree of change across multiple pathologies and bacterial classifications (Table 1). In diabetic retinopathy, major taxonomic phyla including Bacteroidetes, Actinobacteria, Faecalibacterium, and Clostridium were depleted compared to healthy controls [18–21]. In two studies that assessed microbiome diversity in cohorts with diabetic retinopathy, decreases in diversity were noted, consistent with preclinical murine models [19, 20, 22]. One trial examining 12 patients with neovascular AMD (nAMD) noted “dysbiosis” present in nAMD patients relative to controls [23]. Of note, increases in Anaerotruncus were found, which have also been associated with increased inflammatory signaling in murine models, suggesting a possible mechanism of action for gut microbial changes and nAMD progression [24].
In glaucomatous patients, McPherson et al. found irritable bowel syndrome a disease with broad microbiota dysregulation significantly increases the odds of developing glaucoma (OR = 5.84) [25]. In addition to finding differences in bacteria profiles in glaucomatous patients versus controls, Gong et al. also noted visual outcomes to be negatively correlated with Megamonas and Blautia genus abundance [26]. A final retinal study examined a cohort of patients with idiopathic intracranial hypertension, again finding microbiota differences compared to control groups. Interestingly, patients treated with acetazolamide were found to have increases in Lactobacillus, thought to be beneficial for gut microbial health [27].
As shown in Table 1, a variety of bacteria may be altered or disrupted in ocular pathologies. The reviewed studies support a direct gut microbiome-eye axis, however the underlying, unproven assumption is a negative causal association: the missing microbes cause the dysregulation.
Interfering axes
The gut microbiome is known to regulate changes in inflammatory signaling. Therefore, if gut tissue is impacted resulting in a systemic pro-inflammatory state, it is possible that ocular consequences are secondary to or parallel the gut-inflammatory axis, or perhaps differ in primary processes [28–30]. Chakravarthy et al. examined gut dysregulation in the setting of uveitis, finding reductions in various anti-inflammatory microorganisms [31]. Huang et al. also examined gut dysregulation in uveitis, but did not note significant compositional differences between cases and controls, suggesting bacteria may not be contributing to this pathological state [32]. This possibility was further explored by Jayasudha et al. who found increases in pathogenic Candida and Aspergillus genera compared to control patients [33]. Chakravarthy et al. and Jayasudha et al. also examined gut dysregulation in patients with keratitis compared to control patients, both studies finding marked bacterial community alteraions [34, 35]. These studies examined changes in fungi as well, noting trends toward increased pathogenic Aspergillus, Candida, and Malassezia which have been shown to exhibit antifungal resistance and involvement in other disease processes [36]. Two trials examined differences in microbiota of patients with Behcet’s disease with uveitis, finding significant compositional differences between cases and controls [36, 37]. Tercer et al. found significant decreases in microbiota diversity in Behcet’s disease patients compared to control patients as well [38]. The above data suggest a possible link between gut health and ocular pathology. However, it is not clear if fungi and bacteria directly mediate ocular pathology, if the immune system is additionally implicated, or if other, undiscovered pathways are at play.
Zysset-Burri et al. examined Retinal Artery Occlusion (RAO), finding an increase in various taxonomic genus of bacteria compared to healthy control patients. This study also examined Trimethylamine-N-oxide (TMAO), a microbiota derived metabolite which has been found to be an independent risk factor for adverse cardiovascular events, mortality, and thrombosis [39–41]. TMAO was found to be significantly increased in RAO patients compared to control patients. In this study, a positive correlation was found between TMAO and Akkermansia abundance, suggesting a potential mechanistic link between microbiota and RAO. However, it must be noted in other studies Akkermansia was found to be negatively associated with TMAO concentrations suggesting the findings by Zysset-Burri et al. may not be causative [42, 43]. Alternatively, TMAO could function as an intermediary or principle player itself in ocular pathology. This study, as the above, are not powered or designed to prove a link and simply postulate the existence of one.
Clinical trials
Four clinical studies (≤23 patients) to date have examined the effect of targeting the gut-microbiota through Faecal Microbiota Transplant (FMT) or probiotic supplementation for management of ocular pathology. Watane et al. [44] in 2021 examined FMT in 10 patients with Sjogren syndrome complicated by dry eye. Three months after FMT, no side effects were reported and the patient self-reported dry eye symptoms were reduced in half of the cohort [44].
Filippelli et al. in 2021 and 2022 examined probiotic supplementation and its efficacy in treating chalazion in 10 adult and 13 pediatric patients. In both studies, a probiotic containing Streptococcus thermophilus, Lactococcus lactis, and Lactobacillus delbrueckii was used. All adult patients receiving the probiotic formulation experienced significant reductions in time to resolution of the chalazion, while this effect held true for children with only small Chalazion of less than 2.0 mm [45, 46]. Napolitano et al. [47] in 2021 reported a case of probiotic supplementation in a patient with a three-year history of anterior Uveitis. The patient was given a probiotic supplement containing Bifidobacterium lacti, Bifidobacterium bifidum, and Bifidobacterium breve. After two months, this patient was noted to experience increases in visual function and decreased clinical signs of uveitis [47]. Notably, probiotic formulations did not consist of the species that were noted to be absent from microbiomes of patients studies in observational trials.
Discussion
Multiple studies postulated a link between gut imbalance and common ocular pathologies. No single species was frequently implicated, and directionality of association remains to be clarified. Furthermore, the complexity of the microbiome presents unique challenges on reporting microbial alterations as dysbiosis may be attributed to simultaneous overgrowth or loss of a multitude of species. A well-studied approach is to assessing changes in large microbial communities reporting on the variety and abundance of organisms in a community over time (alpha diversity) [48].
The studies reviewed herein opted to focus on species level change, either reporting changes in species or ratios lie the F/B ratio. In effect, this describes a changed microbiome not a dysbiotic microbiome.
Research reviewed here centers on immune mediated ocular reactions; it is possible that ocular consequences are secondary to or parallel the gut-inflammatory axis, or perhaps differ in primary processes [28–30]. The current literature does not parse out causality. Moreover, current trials involve nonspecific interventions such as FMT, which may not be needed. A 17-week randomized, prospective study of 36 patients demonstrated comparable effects on immune function could be achieved by less drastic measures such as gradual introduction of fermented foods [49]. Recent literature has also challenged the idea that increased microbial diversity is beneficial. Rao et al examined 30 patients with aggressive probiotic use increasing microbial diversity, showing they developed SIBO and D-lactic acidosis from this supplementation. Patients’ symptoms were reduced upon initiation of antibiotic therapy (P = 0.005) [50]. These recent findings suggest that interventions aimed at improving systemic health through microbiome modification ought to be carefully employed.
Furthermore, current ophthalmic clinical interventions remain limited to three small pilot studies and one case report, leaving the effect of microbiome modification on ocular pathology largely unknown (Table 2). While 11 ocular pathological states have been examined to exhibit gut-microbiota change, only three of these pathologies have been studied with respect to microbiome-targeted therapy to mitigate symptoms (Table 2). Larger powered prospective clinical trials examining the effects of probiotic supplementation across a wide variety of ocular pathologies are essential to further elucidate the efficacy of these interventions. Two ongoing prospective clinical trials are designed to investigate the effects of oral probiotics in management of Blepharitis and Allergic Rhinoconjunctivitis [16, 17]. While the trial examining probiotic supplementation in Blepharitis is observational, NCT04898686 examines probiotic supplementation in Allergic Rhinoconjunctivitis is randomized, blinded, and placebo controlled, allowing for higher quality of evidence to be obtained.
Future studies may consider referring to NCT04898686 and other randomized controlled trials (RCTs) which have demonstrated the benefit of probiotic supplementation in reducing clinical symptoms of Irritable Bowel Syndrome, dental health, insulin resistance, and depression [51–54]. RCTs investigating FMT therapy have also shown clinical benefit in patients with metabolic syndrome, hepatic encephalopathy, irritable bowel syndrome, and Clostridium difficile induced diarrhea. [44, 55–57] Small molecule inhibitors targeting the gut microbiota are currently in development, but have not yet reached clinical trials [58]. Many of these studies utilized 12 week treatment protocols, placebo or sham treatments, and recruited over 30 patients per arm to achieve statistical power. To establish a causative therapeutic relationship between gut microbiota and mitigation of ocular pathology, future studies may consider employing FMT, probiotic supplementation in 12 week protocols with sample sizes over 30 patients. Trials may seek to isolate microbiome-immune-ocular mediated effects from purely microbiome -ocular effects. Additionally, these trials may consider employing more targeted intervention as they become available rather than FMT and probiotic supplementation.
Taken together, recent clinical trials examining the connection between gut microbiota and ocular pathology have shown an association between the two systems. Additionally, limited early therapeutic investigations aimed at targeting the microbiome to mitigate ocular pathology appear to show beneficial responses. Large-scale randomized controlled clinical trials may provide further proof of this link and clarify areas for novel therapeutic targets.
Supplementary information
Author contributions
MWR, JCM, and RPS were involved in project conception and designing study. MWR, BLK, and AKW were involved in data collection and table generation. All authors were involved in manuscript writing and editing.
Competing interests
RPS reports personal fees from Genentech/Roche, personal fees from Alcon/Novartis, grants from Apellis and Graybug, personal fees from Zeiss, personal fees from Bausch + Lomb, personal fees from Regeneron Pharmaceuticals, Inc. All other authors report no disclosures.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41433-023-02462-7.
References
- 1.Napolitano P, Filippelli M, Davinelli S, Bartollino S, dell’Omo R, Costagliola C. Influence of gut microbiota on eye diseases: an overview. Ann Med. 2021;53:750–61. doi: 10.1080/07853890.2021.1925150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Durack J, Lynch SV. The gut microbiome: relationships with disease and opportunities for therapy. J Exp Med. 2019;216:20–40. doi: 10.1084/jem.20180448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van der Meulen TA, Harmsen H, Bootsma H, Spijkervet F, Kroese F, Vissink A. The microbiome-systemic diseases connection. Oral Dis. 2016;22:719–34. doi: 10.1111/odi.12472. [DOI] [PubMed] [Google Scholar]
- 4.Gut microbiome in retina health: the crucial role of the gut-retina axis. Front Microbiol. Accessed 7 Mar 2022. https://www.frontiersin.org/articles/10.3389/fmicb.2021.726792/full [DOI] [PMC free article] [PubMed]
- 5.Xue W, Li JJ, Zou Y, Zou B, Wei L. Microbiota and ocular diseases. Front Cell Infect Microbiol. 2021;11. Accessed 7 Mar 2022. https://www.frontiersin.org/article/10.3389/fcimb.2021.759333 [DOI] [PMC free article] [PubMed]
- 6.Radjabzadeh D, Uitterlinden AG, Kraaij R. Microbiome measurement: possibilities and pitfalls. Best Pr Res Clin Gastroenterol. 2017;31:619–23. doi: 10.1016/j.bpg.2017.10.008. [DOI] [PubMed] [Google Scholar]
- 7.Allaband C, McDonald D, Vázquez-Baeza Y, et al. Microbiome 101: studying, analyzing, and interpreting gut microbiome data for clinicians. Clin Gastroenterol Hepatol Clin Pr J Am Gastroenterol Assoc. 2019;17:218–30. doi: 10.1016/j.cgh.2018.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nakamura YK, Metea C, Karstens L, et al. Gut microbial alterations associated with protection from autoimmune uveitis. Invest Ophthalmol Vis Sci. 2016;57:3747–58. doi: 10.1167/iovs.16-19733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Horai R, Zárate-Bladés CR, Dillenburg-Pilla P, et al. Microbiota-dependent activation of an autoreactive T cell receptor provokes autoimmunity in an immunologically privileged site. Immunity. 2015;43:343–53. doi: 10.1016/j.immuni.2015.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rowan S, Jiang S, Korem T, et al. Involvement of a gut-retina axis in protection against dietary glycemia-induced age-related macular degeneration. Proc Natl Acad Sci USA. 2017;114:E4472–81. doi: 10.1073/pnas.1702302114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen H, Cho KS, Vu THK, et al. Commensal microflora-induced T cell responses mediate progressive neurodegeneration in glaucoma. Nat Commun. 2018;9:3209. doi: 10.1038/s41467-018-05681-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duan Y, Prasad R, Feng D, et al. Bone marrow-derived cells restore functional integrity of the gut epithelial and vascular barriers in a model of diabetes and ACE2 deficiency. Circ Res. 2019;125:969–88. doi: 10.1161/CIRCRESAHA.119.315743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beli E, Yan Y, Moldovan L, et al. Restructuring of the gut microbiome by intermittent fasting prevents retinopathy and prolongs survival in db/db mice. Diabetes. 2018;67:1867–79. doi: 10.2337/db18-0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Verma A, Xu K, Du T, et al. Expression of human ACE2 in Lactobacillus and beneficial effects in diabetic retinopathy in mice. Mol Ther Methods Clin Dev. 2019;14:161–70. doi: 10.1016/j.omtm.2019.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oxford Centre for Evidence-Based Medicine: Levels of Evidence (March 2009)—Centre for Evidence-Based Medicine (CEBM), University of Oxford. Accessed 16 Jun 2022. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009
- 16.Costagliola C. Effect of probiotics on the occurrence of blepharitis in adults and children. clinicaltrials.gov; 2021. Accessed 16 Mar 2022. https://clinicaltrials.gov/ct2/show/NCT04742855
- 17.Lebeer S. Study of the Probiotic Potential of a Lacticaseibacillus Strain in the Upper Airways in Patients With Allergic Rhinoconjunctivitis After Administration in a Chewable. clinicaltrials.gov; 2021. Accessed 16 Mar 2022. https://clinicaltrials.gov/ct2/show/NCT04898686
- 18.Das T, Jayasudha R, Chakravarthy S, et al. Alterations in the gut bacterial microbiome in people with type 2 diabetes mellitus and diabetic retinopathy. Sci Rep. 2021;11:2738. doi: 10.1038/s41598-021-82538-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ye P, Zhang X, Xu Y, Xu J, Song X, Yao K. Alterations of the gut microbiome and metabolome in patients with proliferative diabetic retinopathy. Front Microbiol. 2021;12:667632. doi: 10.3389/fmicb.2021.667632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang Y, Wang Z, Ma H, et al. Dysbiosis and implication of the gut microbiota in diabetic retinopathy. Front Cell Infect Microbiol. 2021;11:646348. doi: 10.3389/fcimb.2021.646348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jayasudha R, Das T, Kalyana Chakravarthy S, et al. Gut mycobiomes are altered in people with type 2 diabetes mellitus and diabetic retinopathy. PloS One. 2020;15:e0243077. doi: 10.1371/journal.pone.0243077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Singh H, Miyamoto S, Darshi M, et al. Gut microbial changes in diabetic db/db mice and recovery of microbial diversity upon pirfenidone treatment. Microorganisms. 2020;8:1347. doi: 10.3390/microorganisms8091347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zinkernagel MS, Zysset-Burri DC, Keller I, et al. Association of the intestinal microbiome with the development of neovascular age-related macular degeneration. Sci Rep. 2017;7:40826. doi: 10.1038/srep40826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Conley MN, Wong CP, Duyck KM, Hord N, Ho E, Sharpton TJ. Aging and serum MCP-1 are associated with gut microbiome composition in a murine model. PeerJ. 2016;4:e1854. doi: 10.7717/peerj.1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McPherson ZE, Sørensen HT, Horváth-Puhó E, et al. Irritable bowel syndrome and risk of glaucoma: an analysis of two independent population-based cohort studies. U Eur Gastroenterol J. 2021;9:1057–65. doi: 10.1002/ueg2.12136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gong H, Zhang S, Li Q, et al. Gut microbiota compositional profile and serum metabolic phenotype in patients with primary open-angle glaucoma. Exp Eye Res. 2020;191:107921. doi: 10.1016/j.exer.2020.107921. [DOI] [PubMed] [Google Scholar]
- 27.Berkowitz E, Kopelman Y, Kadosh D, et al. “More guts than brains?”—The role of gut microbiota in idiopathic intracranial hypertension. J Neuroophthalmol. 2022;42:e70. doi: 10.1097/WNO.0000000000001330. [DOI] [PubMed] [Google Scholar]
- 28.Bolte LA, Vich Vila A, Imhann F, et al. Long-term dietary patterns are associated with pro-inflammatory and anti-inflammatory features of the gut microbiome. Gut. 2021;70:1287–98. doi: 10.1136/gutjnl-2020-322670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lobionda S, Sittipo P, Kwon HY, Lee YK. The role of gut microbiota in intestinal inflammation with respect to diet and extrinsic stressors. Microorganisms. 2019;7:271. doi: 10.3390/microorganisms7080271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hakansson A, Molin G. Gut microbiota and inflammation. Nutrients. 2011;3:637–82. doi: 10.3390/nu3060637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kalyana Chakravarthy S, Jayasudha R, Sai Prashanthi G, et al. Dysbiosis in the gut bacterial microbiome of patients with uveitis, an inflammatory disease of the eye. Indian J Microbiol. 2018;58:457–69. doi: 10.1007/s12088-018-0746-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang X, Ye Z, Cao Q, et al. Gut microbiota composition and fecal metabolic phenotype in patients with acute anterior uveitis. Investig Ophthalmol Vis Sci. 2018;59:1523–31. doi: 10.1167/iovs.17-22677. [DOI] [PubMed] [Google Scholar]
- 33.Jayasudha R, Kalyana Chakravarthy S, Sai Prashanthi G, Sharma S, Tyagi M, Shivaji S. Implicating dysbiosis of the gut fungal microbiome in uveitis, an inflammatory disease of the eye. Investig Ophthalmol Vis Sci. 2019;60:1384–93. doi: 10.1167/iovs.18-26426. [DOI] [PubMed] [Google Scholar]
- 34.Chakravarthy SK, Jayasudha R, Ranjith K, et al. Alterations in the gut bacterial microbiome in fungal Keratitis patients. PLOS One. 2018;13:e0199640. doi: 10.1371/journal.pone.0199640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jayasudha R, Chakravarthy SK, Prashanthi GS, et al. Alterations in gut bacterial and fungal microbiomes are associated with bacterial Keratitis, an inflammatory disease of the human eye. J Biosci. 2018;43:835–56. doi: 10.1007/s12038-018-9798-6. [DOI] [PubMed] [Google Scholar]
- 36.Kothavade RJ, Kura MM, Valand AG, Panthaki MH. Candida tropicalis: its prevalence, pathogenicity and increasing resistance to fluconazole. J Med Microbiol. 2010;59:873–80. doi: 10.1099/jmm.0.013227-0. [DOI] [PubMed] [Google Scholar]
- 37.Tecer D, Gogus F, Kalkanci A, et al. Succinivibrionaceae is dominant family in fecal microbiota of Behçet’s Syndrome patients with uveitis. PloS One. 2020;15:e0241691. doi: 10.1371/journal.pone.0241691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yasar Bilge NS, Pérez Brocal V, Kasifoglu T, et al. Intestinal microbiota composition of patients with Behçet’s disease: differences between eye, mucocutaneous and vascular involvement. The Rheuma-BIOTA study. Clin Exp Rheumatol. 2020;38127:60–68. [PubMed] [Google Scholar]
- 39.Roncal C, Martínez-Aguilar E, Orbe J, et al. Trimethylamine-N-Oxide (TMAO) predicts cardiovascular mortality in peripheral artery disease. Sci Rep. 2019;9:15580. doi: 10.1038/s41598-019-52082-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhu W, Gregory JC, Org E, et al. Gut microbial metabolite TMAO enhances platelet hyperreactivity and thrombosis risk. Cell. 2016;165:111–24. doi: 10.1016/j.cell.2016.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roberts AB, Gu X, Buffa JA, et al. Development of a gut microbe-targeted nonlethal therapeutic to inhibit thrombosis potential. Nat Med. 2018;24:1407–17. doi: 10.1038/s41591-018-0128-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zysset-Burri DC, Keller I, Berger LE, et al. Retinal artery occlusion is associated with compositional and functional shifts in the gut microbiome and altered trimethylamine-N-oxide levels. Sci Rep. 2019;9:15303. doi: 10.1038/s41598-019-51698-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Griffin LE, Djuric Z, Angiletta CJ, et al. A Mediterranean diet does not alter plasma trimethylamine N-oxide concentrations in healthy adults at risk for colon cancer. Food Funct. 2019;10:2138–47. doi: 10.1039/c9fo00333a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Watane A, Cavuoto KM, Rojas M, et al. Fecal microbial transplant in individuals with immune-mediated dry eye. Am J Ophthalmol. 2022;233:90–100. doi: 10.1016/j.ajo.2021.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Filippelli M, dell’Omo R, Amoruso A, et al. Effectiveness of oral probiotics supplementation in the treatment of adult small chalazion. Int J Ophthalmol. 2022;15:40–44. doi: 10.18240/ijo.2022.01.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Filippelli M, dell’Omo R, Amoruso A, et al. Intestinal microbiome: a new target for chalaziosis treatment in children? Eur J Pediatr. 2021;180:1293–8. doi: 10.1007/s00431-020-03880-5. [DOI] [PubMed] [Google Scholar]
- 47.Napolitano P, Filippelli M, D’andrea L, Carosielli M, dell’Omo R, Costagliola C. Probiotic supplementation improved acute anterior uveitis of 3-year duration: a case report. Am J Case Rep. 2021;22:e931321. doi: 10.12659/AJCR.931321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wilkins LJ, Monga M, Miller AW. Defining dysbiosis for a cluster of chronic diseases. Sci Rep. 2019;9:12918. doi: 10.1038/s41598-019-49452-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wastyk HC, Fragiadakis GK, Perelman D, et al. Gut-microbiota-targeted diets modulate human immune status. Cell. 2021;184:4137–.e14. doi: 10.1016/j.cell.2021.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rao SSC, Rehman A, Yu S, Andino NMde. Brain fogginess, gas and bloating: a link between SIBO, probiotics and metabolic acidosis. Clin Transl Gastroenterol. 2018;9:162. doi: 10.1038/s41424-018-0030-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rudzki L, Ostrowska L, Pawlak D, et al. Probiotic Lactobacillus Plantarum 299v decreases kynurenine concentration and improves cognitive functions in patients with major depression: a double-blind, randomized, placebo controlled study. Psychoneuroendocrinology. 2019;100:213–22. doi: 10.1016/j.psyneuen.2018.10.010. [DOI] [PubMed] [Google Scholar]
- 52.Burton JP, Drummond BK, Chilcott CN, et al. Influence of the probiotic Streptococcus salivarius strain M18 on indices of dental health in children: a randomized double-blind, placebo-controlled trial. J Med Microbiol. 2013;62:875–84. doi: 10.1099/jmm.0.056663-0. [DOI] [PubMed] [Google Scholar]
- 53.Kijmanawat A, Panburana P, Reutrakul S, Tangshewinsirikul C. Effects of probiotic supplements on insulin resistance in gestational diabetes mellitus: a double-blind randomized controlled trial. J Diabetes Investig. 2019;10:163–70. doi: 10.1111/jdi.12863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.van Nood E, Vrieze A, Nieuwdorp M, et al. Duodenal infusion of donor feces for recurrent clostridium difficile. N Engl J Med. 2013;368:407–15. doi: 10.1056/NEJMoa1205037. [DOI] [PubMed] [Google Scholar]
- 55.Rokkas T, Gisbert JP, Gasbarrini A, et al. A network meta-analysis of randomized controlled trials exploring the role of fecal microbiota transplantation in recurrent Clostridium difficile infection. U Eur Gastroenterol J. 2019;7:1051–63. doi: 10.1177/2050640619854587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Holvoet T, Joossens M, Vázquez-Castellanos JF, et al. Fecal microbiota transplantation reduces symptoms in some patients with irritable bowel syndrome with predominant abdominal bloating: short- and long-term results from a placebo-controlled randomized trial. Gastroenterology. 2021;160:145–.e8. doi: 10.1053/j.gastro.2020.07.013. [DOI] [PubMed] [Google Scholar]
- 57.Allegretti JR, Kassam Z, Hurtado J, et al. Impact of fecal microbiota transplantation with capsules on the prevention of metabolic syndrome among patients with obesity. Hormones. 2021;20:209–11. doi: 10.1007/s42000-020-00265-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cully M. Microbiome therapeutics go small molecule. Nat Rev Drug Discov. 2019;18:569–72. doi: 10.1038/d41573-019-00122-8. [DOI] [PubMed] [Google Scholar]
- 59.Moubayed NM, Bhat RS, Al Farraj D, et al. Screening and identification of gut anaerobes (Bacteroidetes) from human diabetic stool samples with and without retinopathy in comparison to control subjects. Microb Pathog. 2019;129:88–92. 10.1016/j.micpath.2019.01.025 [DOI] [PubMed]
- 60.Skondra D, Rodriguez SH, Sharma A, et al. The early gut microbiome could protect against severe retinopathy of prematurity. J AAPOS. 2020;24:236–8. 10.1016/j.jaapos.2020.03.010 [DOI] [PMC free article] [PubMed]
- 61.Khan R, Sharma A, Ravikumar R, et al. Association Between Gut Microbial Abundance and Sight-Threatening Diabetic Retinopathy. Invest Ophthalmol Vis Sci. 2021;62:19. 10.1167/iovs.62.7.19 [DOI] [PMC free article] [PubMed]
- 62.Moon J, Choi SH, Yoon CH, et al. Gut dysbiosis is prevailing in Sjögren’s syndrome and is related to dry eye severity. PLoS One. 2020;15:e0229029. 10.1371/journal.pone.0229029 [DOI] [PMC free article] [PubMed]
- 63.Mendez R, Watane A, Farhangi M, et al. Gut microbial dysbiosis in individuals with Sjögren’s syndrome. Microbial Cell Factories. 2020;19:90. 10.1186/s12934-020-01348-7 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


