Abstract
Introduction
Generalized anxiety disorder (GAD) is a common psychiatric disorder that can cause significant functional impairment to a patient’s life. Mind body therapies (MBT) have increasingly been used as an intervention to manage symptoms of anxiety. Heart rate variability (HRV) biofeedback is a specific MBT that utilizes real-time feedback on autonomic functioning to train the physiological stress response through diaphragmatic breathing.
Case Presentation
A 39-year-old female was referred for a seven-week HRV biofeedback training protocol at Bastyr University Clinic for adjunctive treatment of GAD and depression. She had been taking citalopram for approximately four months prior to the first visit.
Discussion/Conclusion
After completing the seven-week protocol, the patient’s anxiety improved from severe to mild, and her depression improved from mild to minimal. This improvement was maintained at a four-week follow-up, and eight weeks after the final visit she reported that her anxiety was no longer a concern to her. HRV biofeedback demonstrated to be an effective adjunctive treatment for GAD in this patient’s case; however further research is needed to elucidate the effects of HRV biofeedback in patients with GAD.
Introduction
Generalized anxiety disorder (GAD) is a common and often chronic psychiatric disorder that can cause a negative impact on an individual’s quality of life. The diagnostic criteria defines GAD as intrusive and excessive worry that causes functional impairment to one’s ability to perform activities of daily living. The anxiety must have been present for more days than not for at least six months and must not be attributable to the physiological effects of a substance or another medical condition.1,2 The anxiety must also be accompanied by at least three of the following six symptoms in adults: (1) restlessness, (2) being easily fatigued, (3) difficulty concentrating, (4) irritability, (5) muscle tension, and (6) sleep disturbance.2
Anxiety disorders are also frequently comorbid with other psychiatric disorders.3 It has been suggested that 90% of patients with GAD also experience symptoms of depression, and that 85% of patients with major depressive disorder (MDD) also experience symptoms of anxiety.4 Both GAD and MDD are typically treated with pharmaceutical interventions and/or psychotherapy.1 Selective serotonin reuptake inhibitors (SSRI) are currently considered the first-line therapy; however, rebound symptoms have been known to occur with discontinuation of treatment.1 Psychotherapy has been shown to be as effective as medication for GAD and may be associated with less frequent recurrence of rebound symptoms.1,5 A combination of both antidepressants and psychotherapy are associated with a reduced risk of rebound symptoms.6 Studies show that mind body therapies (MBT) demonstrate similar effectiveness to traditional psychotherapy models.7-10
MBTs, which include yoga, meditation, progressive relaxation, guided imagery, hypnosis, biofeedback, and others, are non-invasive techniques designed to use the body to influence the mind. Cognitive behavioral therapy (CBT), although recognized as a traditional model of psychotherapy, is also considered to be under the umbrella of MBTs. Heart rate variability (HRV) biofeedback is a specific MBT that utilizes real-time feedback on autonomic functioning to train the physiological stress response through diaphragmatic breathing. HRV is the amount of time fluctuation in between each heartbeat, which are only detectable by specialized devices. It is understood that HRV is a neurobiological marker of the autonomic nervous system, and patients with decreased HRV are thought to have worse physical and psychological health outcomes.11 Long-standing stress, anxiety, depression, and other states of hyperarousal can cause overactivation of the sympathetic nervous system (SNS), leading to disruptions in the body’s ability to regulate responses to stressors. HRV can be trained to induce a physiological state of autonomic balance through guided breathing at the patient’s individual resonance frequency (generally somewhere between 4 to 7 beats per minute).11 This can be determined and practiced through HRV biofeedback training. This case report highlights resolution of anxiety in a 39 year old female patient with a prior diagnosis of GAD after a seven-week HRV-biofeedback protocol.
Case Presentation
Patient Information
A 39-year-old female was referred to the biofeedback/mind-body medicine shift at Bastyr University Clinic for adjunctive management of GAD. She had been initially diagnosed by a psychiatrist two years prior. Approximately four months prior to the visit, she was prescribed a once daily 10 mg dose of citalopram, an SSRI, by her primary care provider, which she reported helped reduce her anxiety and depressive symptoms a little. She also reported a side effect of low libido from citalopram. She reported previously that she had tried CBT, lorazepam (as needed for flying), and anxiolytic herbs Withania somnifera (Ashwaganda) and Passiflora incarnata (Passionflower), with only minimal resolution of anxiety.
The patient had a history of drug-naive Hashimoto’s thyroiditis and non-thyroid goiter, which is monitored by an endocrinologist. She reported she was radiation exposed in 1986 while living in Minsk north of Chernobyl, USSR. Family history was negative for psychiatric disorders but positive for Hashimoto’s thyroiditis, diabetes and stroke (mother); high cholesterol (mother, father); hypertension (father, maternal grandmother); cardiovascular disease (maternal grandfather, paternal grandfather); kidney disease (paternal grandmother).
Presenting Concerns
The patient reported her main triggers for anxiety as loud noises and repetitive noises such as dogs barking, people talking too loudly, traffic, and thinking about the future or situations out of her control. She characterized her symptoms as anticipatory anxiety, ruminating thoughts, and associated psychosomatic symptoms, such as fatigue, tension headaches, shortness of breath, chest tightness, heart palpitations, dizziness, numbness and tingling in her hands, occasional constipation, nausea, and feeling her stomach in knots or a dropping sensation in her stomach. She reports these psychosomatic symptoms generally lasted up to an hour. Several of these symptoms, such as fatigue and constipation can be attributed to hypothyroidism. She reported that she often had trouble getting out of bed in the morning due to the dread of experiencing anxiety throughout the day. She denied a history of panic attacks or suicidality.
Diagnostic Assessment
We administered two pre-treatment, post-treatment, and follow-up assessments at the initial visit, final visit, and four weeks after the final visit, respectively—the Generalized Anxiety Disorder-7 (GAD-7) and the Patient Health Questionnaire-9 (PHQ-9). Both the GAD-7 and PHQ-9 are validated patient-reported questionnaires that ask patients to rate how often over the last two weeks they were bothered by symptoms of anxiety and depression, respectively. Based on the patient’s responses, her pre-treatment GAD-7 score was determined to be 18 out of 21, categorizing her anxiety as severe (Table 1), and her pre-treatment PHQ-9 score was 6 out of 27, categorizing her depression as mild (Table 2).
Table 1.
A comparison of GAD-7 scores across three checkpoints
| Over the last 2 weeks, how often have you been bothered by the following problems? | Pre-Treatment (April 2022) |
Post-Treatment (June 2022) |
Follow-Up (July 2022) |
|---|---|---|---|
| Feeling nervous, anxious, or on edge | 3 | 1 | 1 |
| Not being able to stop or control worrying | 2 | 1 | 1 |
| Worrying too much about different things | 3 | 1 | 1 |
| Trouble relaxing | 2 | 1 | 1 |
| Being so restless that it’s hard to sit still | 2 | 1 | 1 |
| Becoming easily annoyed or irritable | 3 | 2 | 1 |
| Feeling afraid as if something awful might happen | 3 | 0 | 1 |
| Total Score | 18 | 7 | 7 |
| If you checked off any problems, how difficult have these made it for you to do your work, take care of things at home, or get along with other people? | Somewhat difficult | Not difficult at all | Somewhat difficult |
Abbreviations: GAD-7, Generalized Anxiety Disorder-7.
Point Scale: 0, Not at all; 1, Several days; 2, More than half the days; 3, Nearly every day.
Table 2.
A comparison of PHQ-9 scores across three checkpoints
| Over the last 2 weeks, how often have you been bothered by the following problems? | Pre-Treatment (April 2022) |
Post-Treatment (June 2022) |
Follow-Up (July 2022) |
|---|---|---|---|
| Little interest or pleasure in doing things | 0 | 0 | 0 |
| Feeling down, depressed, or hopeless | 1 | 1 | 1 |
| Trouble falling or staying asleep, or sleeping too much | 0 | 0 | 0 |
| Feeling tired or having little energy | 2 | 1 | 1 |
| Poor appetite or overeating | 0 | 0 | 0 |
| Feeling bad about yourself—or that you are a failure or have let yourself or your family down | 1 | 1 | 1 |
| Trouble concentrating on things, such as reading the newspaper or watching television | 2 | 1 | 0 |
| Moving or speaking so slowly that other people could have noticed? Or the opposite—being so fidgety or restless that you have been moving around a lot more than usual | 0 | 0 | 0 |
| Thoughts that you would be better off dead or of hurting yourself in some way | 0 | 0 | 0 |
| Total Score | 6 | 4 | 3 |
| If you checked off any problems, how difficult have these made it for you to do your work, take care of things at home, or get along with other people? | Somewhat difficult | Not difficult at all | Not difficult at all |
Abbreviations: PHQ-9, Patient Health Questionnaire-9.
Point Scale: 0, Not at all; 1, Several days; 2, More than half the days; 3, Nearly every day.
Therapeutic Intervention
The seven-week HRV-biofeedback protocol at Bastyr University Clinic is designed to build upon the previous week at every visit and allow patients time to integrate the findings into their daily lives. A copy of this protocol has been provided in Supplementary Materials. Over the course of seven weeks, the patient was introduced to concepts such as heart rate variability, resonant frequency, and emotional coherence. She was guided on how to practice diaphragmatic breathing and given realtime visual feedback on her physiological functioning through various states for comparison (e.g. baseline, paced diaphragmatic breathing, guided meditation, stressor storylines, vision statement, etc.). Her resonant frequency was determined to be 4.5 BPM, and she was instructed to apply what she learned each week into her regular home practice of breathing exercises at her resonant frequency for 20 minutes twice daily.
Follow-up and Outcomes
At the end of the seven-week biofeedback protocol, the patient reported more overall awareness of her physiological stress responses and felt empowered in her ability to taper her sympathetic tone through diaphragmatic breathing. The patient also reported a reduction in psychosomatic symptoms of dizziness, chest tightness, heart palpitations, and tension headaches. Her post-treatment GAD-7 score was 7 out of 21, indicating mild anxiety (Table 1). Her post-treatment PHQ-9 score was 4 out of 27, indicating minimal depression (Table 2). The patient also reported that she had discontinued her citalopram during the sixth week, with no significant symptoms of antidepressant withdrawal.
Four weeks after the final biofeedback visit, we asked the patient to complete a follow-up assessment of her anxiety and depression via REDCap. Her follow-up GAD-7 score remained at 7 out of 21, still indicating mild anxiety (Table 1). Her follow-up PHQ-9 score went down to 3 out of 27, still indicating minimal depression (Table 2). She did not report symptoms of antidepressant withdrawal or relapse of anxiety or depression. Eight weeks after the final biofeedback visit, the patient reported during a follow-up visit that her anxiety was not a concern at this time. She reported that although she was not practicing her resonant frequency breathing as often as during the seven-week protocol (20 minutes twice daily), she still continued with her home practice and utilized the tool as needed during times of anxiety.
Discussion
Studies have shown significant improvements in conditions such as anxiety,12-14 post-traumatic stress disorder,15,16 MDD,17-18 and depression,14,19-24 from the use of HRV biofeedback, especially when used in combination with the standard treatment.11 Though there are a limited number of studies on HRV biofeedback and GAD, the effects of meditation25-28 and physical activity29-31 for GAD have been well-established. Interestingly, in a study comparing the effects of HRV biofeedback, physical activity, and mindfulness meditation,32 there was a significant improvement in stress, anxiety, and depression, with no significant differences between the interventions, suggesting that all interventions were equally effective. A possible explanation for this is that HRV biofeedback is very similar to meditation and other MBTs. Blase et al33 characterized HRV biofeedback as making the neurophysiological effects of meditation visible through real time feedback. Despite evidence in the literature supporting the use of HRV biofeedback for adjunctive management of stress and mental disorders, this modality has yet to be integrated into widespread psychiatric practices. Further research on the neurophysiological mechanisms of HRV biofeedback is warranted.
HRV biofeedback is a non-invasive, relatively inexpensive modality that teaches patients tools to self-regulate their emotional responses, which can lead to sustained improvement even after cessation of the treatment. Piaserico et al34 suggested that biofeedback “improves self-efficacy in patients by enabling them to gain voluntary control of their covert physiological responses by making them explicit through real-time visual or auditory feedback.” The patient perspective detailed in this case report supports this suggestion, as she stated that knowing this tool was in her anxiety tool kit alone reduced her anxiety levels.
One limitation of this case report is that the patient was on citalopram, so it is difficult to determine whether the improvements observed were due to the SSRI, biofeedback, or both. SSRIs typically have a delayed therapeutic response, taking anywhere from four to 12 weeks to provide symptomatic relief.1 However, the patient had been prescribed citalopram approximately four months prior to her initial biofeedback appointment, which makes the possibility that her improvement in anxiety due to the SSRI unlikely. It is plausible that her depressive symptoms may have been improved prior to beginning biofeedback, but without PHQ-9 scores prior to treatment with citalopram, it is difficult to tell how much of an impact the SSRI or biofeedback had on her depression.
Additionally, SSRIs are typically effective while in use, but in the absence of psychological interventions such as CBT or biofeedback, patients commonly experience a relapse in symptoms after discontinuation of the medication.1 The patient’s follow-up scores reflected that she was maintaining her low levels of anxiety. At another follow-up visit four weeks after the initial follow-up, she reported that her anxiety was no longer an issue for her at this time.
Conclusion
HRV biofeedback demonstrated effectiveness as an adjunctive treatment of GAD in this patient’s case; however further research is needed to elucidate the effects of HRV biofeedback in patients with GAD.
Patient Perspective
I started the seven-week biofeedback study while dealing with anxiety, and taking 10 mg of citalopram (prescribed by my primary care physician three months prior). I wasn’t sure what to expect and I was a little surprised that the process started off slow with just learning how to do diaphragm breathing, then finding my ideal breathe-in/breathe-out count. It was great to work with Autumn and create such a personalized protocol! Not only did we find my ideal breath timing, we also worked through several anxiety-inducing scenarios, from a low-anxiety one to increasingly higher ones. With each of these, I would use the breath exercises given to me by Autumn to help guide me out of my anxious state that was initially induced through one of these scenarios. Doing the exercises at home, I noticed that I would get less anxious about certain triggers around me, whether it was traffic or my neighbor’s dog barking incessantly. I also noticed that while the breathing exercises were helpful during a triggering situation, doing them prior to experiencing a negative event would “precondition” me to remain in a calmer state. After the seven-week treatment, I was able to cycle off the citalopram and I am happy to report that my mood and anxiety levels have remained much lower. It’s not been a month, and while I probably won’t do the breathing exercises as often as I should (I try!), I know I can always turn to them when I need to. Even knowing that I have this in my “anxiety tool kit” already helps reduce anxiety.
Figure 1.
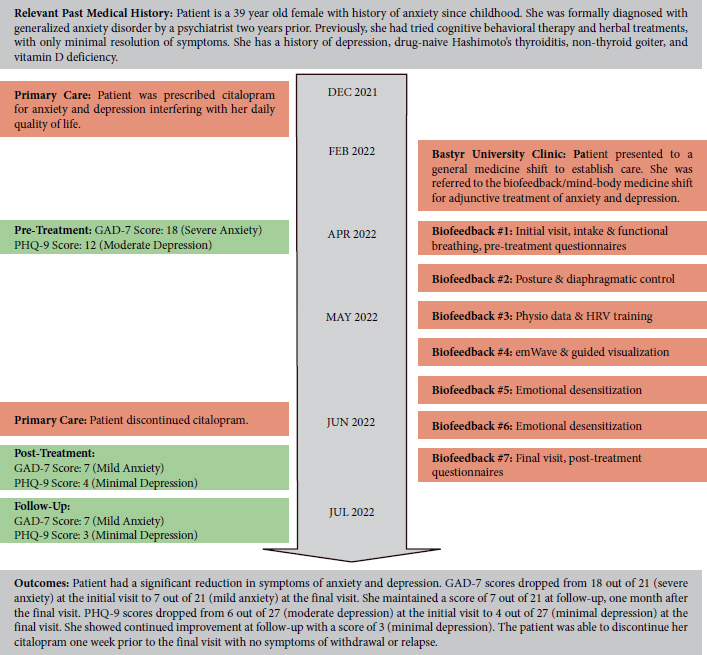
Timeline of the patient’s case history and outcomes
Table 3.
A summary of GAD-7 and PHQ-9 total scores and severity across three checkpoints
| Questionnaires | Pre-Treatment (April 2022) |
Post-Treatment (June 2022) |
Follow-Up (July 2022) |
|---|---|---|---|
| GAD-7 Total Score | 18 | 7 | 7 |
| Anxiety Severity | Severe | Mild | Mild |
| PHQ-9 Total Score | 6 | 4 | 3 |
| Depression Severity | Mild | Minimal | Minimal |
Abbreviations: GAD-7, Generalized Anxiety Disorder-7; PHQ-9, Patient Health Questionnaire-9.
GAD-7 Scoring: 0-4, Minimal; 5-9, Mild; 10-14, Moderate; 15-21, Severe.
PHQ-9 Scoring: 0-4, None-minimal; 5-9, Mild; 10-14, Moderate; 15-19, Moderately severe; 20-27, Severe.
Footnotes
Abbreviations
CBT, Cognitive Behavioral Therapy; GAD, Generalized Anxiety Disorder; GAD-7, Generalized Anxiety Disorder-7; HRV, Heart Rate Variability; MBT, Mind Body Therapy; MDD, Major Depressive Disorder; PHQ-9, Patient Health Questionnaire-9; SSRI, Selective Serotonin Reuptake Inhibitor.
Timeline
A timeline of the patient’s case history and outcomes (Figure 1) can be viewed under the Figures section.
Disclosures
The authors have no conflicts of interest or funding sources to declare. This case report was written according to CaRe Guidelines.35
Informed Consent
Written consent was obtained from the patient for publication of this case report. A copy of the written consent is available for review.
References
- 1.Locke AB, Kirst N, Shultz CG. Diagnosis and management of generalized anxiety disorder and panic disorder in adults. Am Fam Physician. 2015;91(9):617-624. [PubMed] [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013. [Google Scholar]
- 3.Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci. 2015;17(3):327-335. doi:10.31887/DCNS.2015.17.3/bbandelow [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tiller JW. Depression and anxiety. Med J Aust. 2013;199(S6):S28-S31. doi:10.5694/mja12.10628 [DOI] [PubMed] [Google Scholar]
- 5.National Institute for Health and Care Excellence. Generalised anxiety disorder and panic disorder (with or without agoraphobia) in adults: management in primary, secondary and community care. January 2011. http://www.nice.org.uk/Guidance/CG113. Accessed August 14, 2022.
- 6.Cuijpers P, Sijbrandij M, Koole SL, Andersson G, Beekman AT, Reynolds CF, III. Adding psychotherapy to antidepressant medication in depression and anxiety disorders: a meta-analysis. World Psychiatry. 2014;13(1):56-67. doi:10.1002/wps.20089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khoury B, Lecomte T, Fortin G, et al. Mindfulness-based therapy: a comprehensive meta-analysis. Clin Psychol Rev. 2013;33(6):763-771. doi:10.1016/j.cpr.2013.05.005 [DOI] [PubMed] [Google Scholar]
- 8.Marchand WR. Mindfulness-based stress reduction, mindfulness-based cognitive therapy, and Zen meditation for depression, anxiety, pain, and psychological distress. J Psychiatr Pract. 2012;18(4):233-252. doi:10.1097/01. pra.0000416014.53215.86 [DOI] [PubMed] [Google Scholar]
- 9.Chen KW, Berger CC, Manheimer E, et al. Meditative therapies for reducing anxiety: a systematic review and meta-analysis of randomized controlled trials. Depress Anxiety. 2012;29(7):545-562. doi:10.1002/da.21964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krisanaprakornkit T, Krisanaprakornkit W, Piyavhatkul N, Laopaiboon M. Meditation therapy for anxiety disorders. Cochrane Database Syst Rev. 2006;1(1):CD004998. [DOI] [PubMed] [Google Scholar]
- 11.Blase K, Vermetten E, Lehrer P, Gevirtz R. Neurophysiological approach by self-control of your stress-related autonomic nervous system with depression, stress and anxiety patients. Int J Environ Res Public Health. 2021;18(7):3329. Published 2021 Mar 24. doi:10.3390/ijerph18073329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee J, Kim J, Wachholtz A. The benefit of heart rate variability biofeedback and relaxation training in reduction trait anxiety. Hanguk Simni Hakhoe Chi. Kongang. 2015;20:391-408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Henriques G, Keffer S, Abrahamson C, Horst SJ. Exploring the effectiveness of a computer-based HRV biofeedback program in reducing anxiety in college students. Appl Psychophysiol Biofeedback. 2011;36:101-112. doi:10.1007/S10484-011-9151-4 [DOI] [PubMed] [Google Scholar]
- 14.van der Zwan JE, Huizink AC, Lehrer PM, Koot HM, de Vente W. The effect of Heart Rate Variability Biofeedback training on mental health of pregnant and non-pregnant women: A randomized contolled trial. Int J Environ Res Public Health. 2019;16(6):1051. doi:10.3390/ijerph16061051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zucker TL, Samuelson KW, Muench F, Greenberg MA, Gevirtz RN. The effects of respiratory sinus arrhythmia biofeedback on heart rate variability and posttraumatic stress disorder symptoms: a pilot study. Appl Psychophysiol Biofeedback. 2009;34(2):135-143. doi:10.1007/s10484-009-9085-2 [DOI] [PubMed] [Google Scholar]
- 16.Tan G, Dao TK, Farmer L, Sutherland RJ, Gevirtz R. Heart rate variability (HRV) and posttraumatic stress disorder (PTSD): a pilot study. Appl Psychophysiol Biofeedback. 2011;36(1):27-35. doi:10.1007/s10484-010-9141-y [DOI] [PubMed] [Google Scholar]
- 17.Thode L. Heart Rate Variability Biofeedback as a Complementary Treatment for Depression in Latinos. Alliant International University; 2019. [Google Scholar]
- 18.Lin IM, Fan SY, Yen CF, et al. Heart rate variability biofeedback increased autonomic activation and improved symptoms of depression and insomnia among patients with major depression disorder. Clin Psychopharmacol Neurosci. 2019;17(2):222-232. doi:10.9758/cpn.2019.17.2.222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lin IM, Ko JM, Fan SY, Yen CF. Heart Rate Variability and the efficacy of biofeedback in heroin users with depressive symptoms. Clin Psychopharmacol Neurosci. 2016;14(2):168-176. doi:10.9758/cpn.2016.14.2.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rene R. The efficacy of a portable HRV feedback device in conjunction with mental health treatment of clients with major depressive disorder enrolled in a country welfare-to-work program. Diss. Abstr. Int. Sect. B Sci. Eng. 2008, 69, 2000. [Google Scholar]
- 21.Chaudhri P. The effects of cardiorespiratory biofeedback and dialectical behavioral skills training with sertraline on post myocardial infarction major depression and low heart rate variability. Alliant University; 2008. [Google Scholar]
- 22.Patron E, Benvenutti GF, Palomba D. Biofeedback assisted control of RSA as a biobehavioral intervention for depressive symptoms in patients after cardiac surgery: A preliminary study. Appl. Psychophysiol. Biof. 2013;38:1-9. doi:10.1007/s10484-012-9202-5 [DOI] [PubMed] [Google Scholar]
- 23.Karavidas MK, Lehrer PM, Vaschillo E, et al. Preliminary results of an open label study of heart rate variability biofeedback for the treatment of major depression. Appl Psychophysiol Biofeedback. 2007;32(1):19-30. doi:10.1007/s10484-006-9029-z [DOI] [PubMed] [Google Scholar]
- 24.Siepmann M, Aykac V, Unterdörfer J, Petrowski K, Mueck-Weymann M. A pilot study on the effects of heart rate variability biofeedback in patients with depression and in healthy subjects. Appl Psychophysiol Biofeedback. 2008;33(4):195-201. doi:10.1007/s10484-008-9064-z [DOI] [PubMed] [Google Scholar]
- 25.Vahia VN, Shetty HK, Motiwala S, Thakkar G, Fernandes L, Sharma JC. Efficacy of meditation in generalized anxiety disorder. Indian J Psychiatry. 1993;35(2):87-91. [PMC free article] [PubMed] [Google Scholar]
- 26.Hoge EA, Bui E, Marques L, et al. Randomized controlled trial of mindfulness meditation for generalized anxiety disorder: effects on anxiety and stress reactivity. J Clin Psychiatry. 2013;74(8):786-792. doi:10.4088/JCP.12m08083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hoge EA, Bui E, Palitz SA, et al. The effect of mindfulness meditation training on biological acute stress responses in generalized anxiety disorder. Psychiatry Res. 2018;262:328-332. doi:10.1016/j.psychres.2017.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Saeed SA, Cunningham K, Bloch RM. Depression and Anxiety Disorders: Benefits of Exercise, Yoga, and Meditation. Am Fam Physician. 2019;99(10):620-627. [PubMed] [Google Scholar]
- 29.Kandola A, Vancampfort D, Herring M, et al. Moving to Beat Anxiety: Epidemiology and Therapeutic Issues with Physical Activity for Anxiety. Curr Psychiatry Rep. 2018;20(8):63. Published 2018 Jul 24. doi:10.1007/s11920-018-0923-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Herring MP, Monroe DC, Gordon BR, Hallgren M, Campbell MJ. Acute Exercise Effects among Young Adults with Analogue Generalized Anxiety Disorder. Med Sci Sports Exerc. 2019;51(5):962-969. doi:10.1249/MSS.0000000000001860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carek PJ, Laibstain SE, Carek SM. Exercise for the treatment of depression and anxiety. Int J Psychiatry Med. 2011;41(1):15-28. doi:10.2190/PM.41.1.c [DOI] [PubMed] [Google Scholar]
- 32.van der Zwan JE, de Vente W, Huizink AC, Bögels SM, de Bruin EI. Physical activity, mindfulness meditation, or heart rate variability biofeedback for stress reduction: a randomized controlled trial. Appl Psychophysiol Biofeedback. 2015;40(4):257-268. doi:10.1007/s10484-015-9293-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Blase KL, van Waning A. Heart rate variability, cortisol and attention focus during Shamatha quiescence meditation. Appl Psychophysiol Biofeedback. 2019;44(4):331-342. doi:10.1007/s10484-019-09448-w [DOI] [PubMed] [Google Scholar]
- 34.Piaserico S, Marinello E, Dessi A, Linder MD, Coccarielli D, Peserico A. Efficacy of biofeedback and cognitive-behavioural therapy in psoriatic patients: A single-blind, randomized and controlled study with added narrow-band ultraviolet B therapy. Acta Derm Venereol. 2016;96(217):91-95. doi:10.2340/00015555-2428 [DOI] [PubMed] [Google Scholar]
- 35.Riley DS, Barber MS, Kienle GS, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol. 2017;89:218-235. doi:10.1016/j.jclinepi.2017.04.026 [DOI] [PubMed] [Google Scholar]


