Abstract
Background
Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF) has revolutionized identification of bacteria and is becoming available in an increasing number of laboratories in malaria-endemic countries. The purpose of this proof-of-concept study was to explore the potential of MALDI-TOF as a diagnostic tool for direct detection and quantification of Plasmodium falciparum in human blood.
Methods
Three different P. falciparum strains (3D7, HB3 and IT4) were cultured and synchronized following standard protocols. Ring-stages were diluted in fresh blood group 0 blood drawn in EDTA from healthy subjects to mimic clinical samples. Samples were treated with saponin and washed in PBS to concentrate protein material. Samples were analysed using a Microflex LT MALDI-TOF and resulting mass spectra were compared using FlexAnalysis software.
Results
More than 10 peaks specific for P. falciparum were identified. The identified peaks were consistent among the three genetically unrelated strains. Identification was possible in clinically relevant concentrations of 0.1% infected red blood cells, and a close relationship between peak intensity and the percentage of infected red blood cells was seen.
Conclusion
The findings indicate that the method has the potential to detect and quantify P. falciparum at clinically relevant infection intensities and provides proof-of-concept for MALDI-TOF-based diagnosis of human malaria. Further research is needed to include other Plasmodium spp., wildtype parasite isolates and to increase sensitivity. MALDI-TOF may be a useful tool for mass-screening purposes and for diagnosis of malaria in settings where it is readily available.
Background
Malaria, caused by infections with Plasmodium parasites, are a leading course of sickness and death especially in endemic low- and middle-income countries [1]. In severe cases malaria can progress from mild symptoms to fatal outcome in a matter of hours and suspicion of malaria is thus an emergency where a proper diagnose is required without delay. To guide treatment, an ideal diagnostic test for malaria should both be able to discriminate between Plasmodium spp., and to quantify the level of infection, as indicated by the percentage of infected red blood cells (IRBC).
Over the years several diagnostic methods have been developed to increase diagnostic precision and shorten time-to-result. Especially the development of rapid antigen tests (RDTs), such as lateral flow immunoassays, have had great impact on anti-malaria programmes due to its simplicity in use and quick results. Unfortunately, all current diagnostic methods also have limitations. Widespread technologies, such as loop-mediated isothermal amplification (LAMP) and RDTs cannot quantify the level of IRBC and can only provide tentative species discrimination. Furthermore, both LAMP and RDTs are limited by false positive results after treatment due to circulating Plasmodium antigens and DNA fragments [2–5]. Microscopy of blood as described by Giemsa in 1904, therefore, still remains the Gold standard for detection of malaria [6, 7]. In trained hands, microscopy can provide excellent sensitivity and species discrimination. However, even in trained hands microscopy is time-consuming, and the diagnostic precision is highly operator dependent with risk of misidentification and wrong diagnosis with less experienced operators.
The purpose of this study was to explore if matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF) may be a candidate for a novel diagnostic approach. MALDI-TOF generates a unique mass spectrum reflecting the size and charge of proteins in an organism. This spectrum is then compared to known reference spectra in large databases. MALDI-TOF technology has revolutionized routine identification of bacteria and is broadly recognized as an inexpensive, fast and robust analysis with minimal risk of operator bias [8]. Apart from the MALDI-TOF platform, only limited laboratory equipment is needed to run MALDI-TOF. Pure material can be analysed directly after application of a thin layer of matrix, while blood-borne organisms require a few purification steps typically involving lysis of erythrocytes, centrifugation, and pipetting. Several commercial companies offer MALDI-TOF platforms, matrix components and purification kits. Despite this, MALDI-TOF analysis has not yet been used as a diagnostic tool for Plasmodium infections in humans. The aim of this study was to provide proof-of-concept for both detection and quantification of P. falciparum in human blood and thus create a framework for development of a novel diagnostic tool.
Methods
Overall study design
This proof-of-concept study was based on bio-bank strains of P. falciparum and negative controls of uninfected blood. Both sample types were prepared and analysed using the same MALDI-TOF protocols and resulting spectra were compared to identify differences.
Culture of Plasmodium falciparum and negative controls
Frozen samples of P. falciparum previously identified as HB3, IT-4 and 3D7 strains were thawed, cultured, and synchronized using magnet activated cell sorting (MACS, Miltenyi biotec, Bergish Gladbach, Germany) following standard protocols [9, 10]. Negative controls were prepared using the same protocol but leaving out P. falciparum. Lifecycle-stage and % IRBC were followed with daily microscopy of Giemsa-stained blood smears. When cultures reached > 2% IRBC with a predominance of ring stages, cultures were centrifuged at 779 g for 8 min (1800 RPM, CryoFuge 5500i, LH-4000 75,006,478, Thermo Scientific, Waltham, MA, USA). After centrifugation, cultures were adjusted to a final haematocrit of 50%. Final exact % IRBC was determined by microscopy of Giemsa-stained blood smears. A total of 2000 red blood cells (RBC) were reviewed pr. blood-smear. Final samples were stored at 5℃ for a maximum of 2 days before sample preparation. All cultures were controlled for Mycoplasma contamination with MycoAlert Mycoplasma Detection kit (Lonza, Basel, Switzerland). Strain identity was controlled with an in-house polymerase chain reaction (PCR) using MSP2-IC1-, MSP2-FC27- and GLURP-specific primer pairs. To control for cross-contamination, negative controls were controlled by microscopy of Giemsa-stained blood smears. A total of 100 microscopy fields containing RBC monolayers were reviewed for each negative control.
Sample preparation
To extract parasites from RBC, 250 µl blood was vortex mixed for 15 s with 250 µl 0.7% saponin in 140 mM phosphate-buffered saline pH 7.4 (PBS) and incubated 5 min at room temperature. After incubation 1500 µl PBS was added and samples were vortex mixed for 15 s and centrifuged for 2 min at 2579 g (6200 RPM, Minispin F-45-12-11, Eppendorf AG, Hamborg, Germany). After centrifugation, the supernatant was removed, and the lid and edges of the sample tube were carefully cleaned with a sterile cotton swap without touching the pellet. The pellet was then resuspended in 2000 µl PBS and samples were centrifuged for 1 min at 12,045 g (13.400 RPM, Minispin F-45-12-11, Eppendorf AG). The resulting pellet was spotted in a thin layer on clean steel target plates using a wooden toothpick and 1 µl matrix (alpha-cyano-4-hydroxycinnamic acid, Bruker Daltonics, Billerica, MA, USA) was applied to each sample spot. Samples were dried at room temperature before further processing. The sample preparation protocol was based on a method described by Baumeister et al. to separate intact Plasmodium parasites from erythrocytes [11].
Identification of P. falciparum
Samples were analysed using a Microflex LT MALDI-TOF (Bruker Daltonics) and FlexContol v.3.4 (Bruker Daltonics). The following settings were applied: Sampling range 1000–20,000 Da, laser power 30–50% of maximum, accumulation of 800 shots pr. spectra, movement pattern random walk, maximum 20 shots allowed pr. raster position, automated peak quality evaluation from 4000 to 10,000 Da, standard exclusion of the one largest peak in the mass range, minimum peak resolution 200 a.u., fuzzy control peptide mode with high signal intensity, and automated termination if 100 consecutive shots failed. Resulting spectra were visually evaluated in FlexAnalysis v.3.4 (Bruker Daltonics). Baseline subtraction and smoothing was applied once before visual inspection. Peaks found in Plasmodium samples but not in the negative controls were noted. As a quality control, spectra were further compared to the existing bacterial database with the standard built-in automated comparison tool. MALDI-TOF calibration and detector check was preformed according to the manufacturer’s instructions before initiating the study.
Quantification of P. falciparum
A culture of P. falciparum 3D7 was diluted in fresh blood group 0 blood drawn in EDTA from healthy subjects. Dilution was done with 50%, 25%, 12.5%, 7.5% and 4% of the original sample. For each dilution step negative controls were prepared with the same concentrations of cultured negative samples and fresh EDTA blood. At each dilution step parasitaemia degree was determined by microscopy of Giemsa-stained blood smears, as previously described. Samples were hereafter processed using the same protocols for extractions and MALDI-TOF analysis as previously described. Further, peaks intensity was determined for six unique P. falciparum peaks for each dilution step.
Results
Identification of P. falciparum
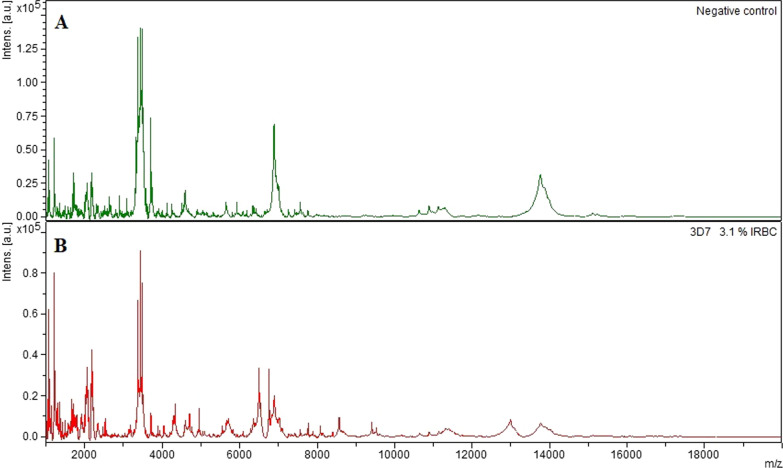
Visual inspection revealed 20 peaks that were specific for P. falciparum. The peaks were found in undiluted samples of all three strains. (Fig. 1; Table 1). Six additional P.falciparum-specific peaks were identified in the 3D7 strain, 1 peak in the HB3 strain, 1 peak in the IT4 strain, and 3 peaks in both the 3D7 and IT4 strain but not the HB3 strain (Table 1). After dilution of the 3D7 strain correct identification of P. falciparum samples was possible at concentrations down to 0.1% IRBC. In total All 18 extractions from uninfected RBC were correctly identified as negative. Of 23 P. falciparum extractions, 22 were correctly identified while 1 run was invalid (flatline - no peaks found). Subsequent re-run of this extraction was correctly identified.
Fig. 1.
MALDI-TOF spectra of Plasmodium falciparum and negative controls. An example of mass spectra in the sample range 1000–20.000 m/z. A = Negative control of uninfected erythrocytes. B = Positive sample with 3,1% 3D7 Plasmodium falciparum-infected erythrocytes. Each peak in the spectra represents proteins of a specific charge and size. A full description of peak differences can be found in Table 1. Plasmodium cultures and negative controls were prepared using the same protocols. See Methods section for details
Table 1.
Plasmodium falciparum-specific peaks found by MALDI-TOF analysis
| Sample type | |||||||||||||||
| Culture type | 3D7 | HB3 | IT4 | NC | 3D7 | NC | 3D7 | NC | 3D7 | NC | 3D7 | NC | 3D7 | NC | |
| % Culture | 100 | 100 | 100 | 100 | 50 | 50 | 25 | 25 | 12,5 | 12,5 | 7,5 | 7,5 | 4 | 4 | |
| % EDTA dilution | 0 | 0 | 0 | 0 | 50 | 50 | 75 | 75 | 87,5 | 87,5 | 92,5 | 92,5 | 96 | 96 | |
| Microscopy results | |||||||||||||||
| Ring stages | 54 | 49 | 30 | 0 | 32 | 0 | 13 | 0 | 7 | 0 | 4 | 0 | 2 | 0 | |
| Late stages | 8 | 9 | 9 | 0 | 6 | 0 | 3 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | |
| Total IRBC | 3,1% | 2.9% | 2.5% | None | 1,9% | None | 0,80% | None | 0,40% | None | 0,20% | None | 0,10% | None | |
| MALDI-TOF results | |||||||||||||||
| Successful runs | 3 of 3 | 3 of 3 | 3 of 3 | 3 of 3 | 3 of 3 | 3 of 3 | 3 of 3 | 3 of 3 | 3 of 3 | 3 of 3 | 2 of 3 | 3 of 3 | 3 of 3 | 3 of 3 | |
| MALDI-TOF diagnose | Pos | Pos | Pos | Neg | Pos | Neg | Pos | Neg | Pos | Neg | Pos | Neg | Pos | Neg | |
| Peaks found (m/z) | |||||||||||||||
| 1014 | + | + | + | – | + | – | + | – | – | – | – | – | – | – | |
| 1130 | + | + | + | – | + | – | + | – | + | – | + | – | + | – | |
| 1366 | + | + | + | – | + | – | + | – | + | – | + | – | + | – | |
| 1470 | + | + | + | – | + | – | – | – | – | – | – | – | – | – | |
| 1657 | + | + | + | – | + | – | + | – | + | – | + | – | + | – | |
| 1984 | + | + | + | – | + | – | + | – | – | – | – | – | – | – | |
| 2006 | + | + | + | – | + | – | + | – | + | – | + | – | + | – | |
| 2473 | + | + | + | – | + | – | + | – | + | – | + | – | + | – | |
| 2527 | + | + | + | – | + | – | + | – | – | – | – | – | – | – | |
| 3176 | + | – | – | – | + | – | + | – | – | – | – | – | – | – | |
| 4042 | + | + | + | – | + | – | + | – | + | – | – | – | – | – | |
| 4300 | + | – | – | – | + | – | – | – | – | – | – | – | – | – | |
| 4332 | + | + | + | – | + | – | + | – | + | – | + | – | – | – | |
| 4421 | – | + | – | – | – | – | – | – | – | – | – | – | – | – | |
| 4432 | + | – | – | – | + | – | + | – | + | – | + | – | + | – | |
| 4704 | + | – | – | – | + | – | + | – | + | – | + | – | – | – | |
| 4765 | + | – | + | – | – | – | – | – | – | – | – | – | – | – | |
| 4773 | – | + | – | – | – | – | – | – | – | – | – | – | – | – | |
| 4957 | + | + | + | – | + | – | + | – | – | – | – | – | – | – | |
| 5547 | + | + | + | – | + | – | – | – | – | – | – | – | – | – | |
| 5567 | + | + | + | – | + | – | + | – | + | – | + | – | + | – | |
| 5705 | + | – | – | – | + | – | – | – | – | – | – | – | – | – | |
| 6086 | + | – | – | – | + | – | + | – | + | – | + | – | + | – | |
| 6286 | + | – | – | – | + | – | + | – | – | – | – | – | – | – | |
| 6500 | + | + | + | – | + | – | + | – | + | – | + | – | + | – | |
| 6533 | + | – | + | – | + | – | + | – | + | – | + | – | – | – | |
| 6760 | + | + | + | – | + | – | + | – | + | – | + | – | + | – | |
| 7886 | + | + | + | – | + | – | – | – | – | – | – | – | – | – | |
| 8086 | + | + | + | – | + | – | + | – | – | – | – | – | – | – | |
| 8568 | + | + | + | – | + | – | + | – | + | – | + | – | + | – | |
| 8843 | – | + | – | – | – | – | – | – | – | – | – | – | – | – | |
| 9340 | – | – | + | – | – | – | – | – | – | – | – | – | – | – | |
| 9409 | + | – | – | – | + | – | + | – | – | – | – | – | – | – | |
| 9530 | + | – | + | – | + | – | – | – | – | – | – | – | – | – | |
| 9546 | + | + | – | – | – | – | – | – | – | – | – | – | – | – | |
| 12,993 | + | + | + | – | + | – | + | – | + | – | + | – | + | – | |
Plasmodium falciparum-specific peaks found by MALDI-TOF analysis using different parasite strains and dilutions. + indicates the presence of a peak at the given m/z. – indicates the absence of a peak at the given m/z. 3D7, HB3 and IT4 indicate the strains of P. falciparum used in the experiment. NC = Negative control cultures consisting of uninfected erythrocytes. IRBC = Plasmodium-infected red blood cells. EDTA dilution = fresh type 0 blood in EDTA drawn from healthy subjects. Giemsa-Stained blood smears were used for microscopy. A total of 2000 red blood cells were reviewed for microscopy of each P. falciparum culture. A total of 100 microscopic fields were reviewed for negative control cultures. Mass spectra were compared by visual inspection using the FlexAnalysis software (Bruker Daltonics, Bremen, Germany) see method section for details. Plasmodium cultures and negative controls were prepared using identical steps. See method section for details
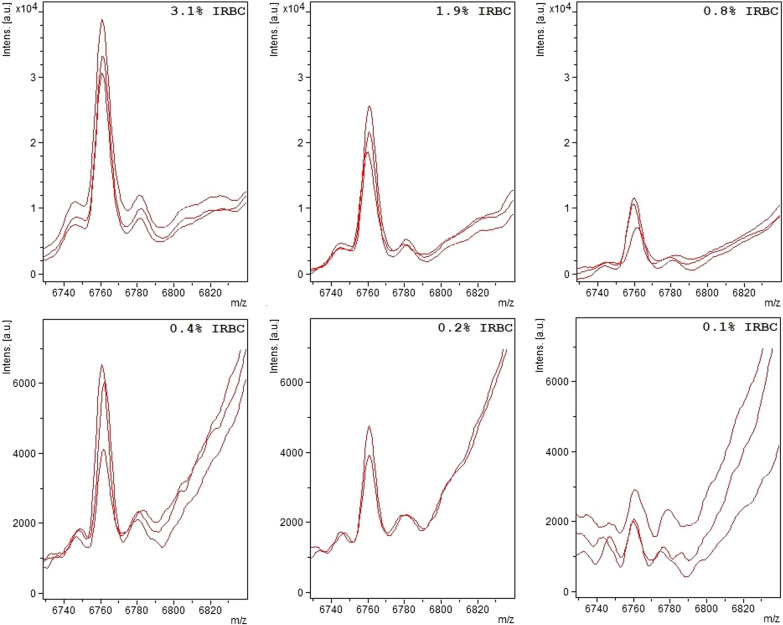
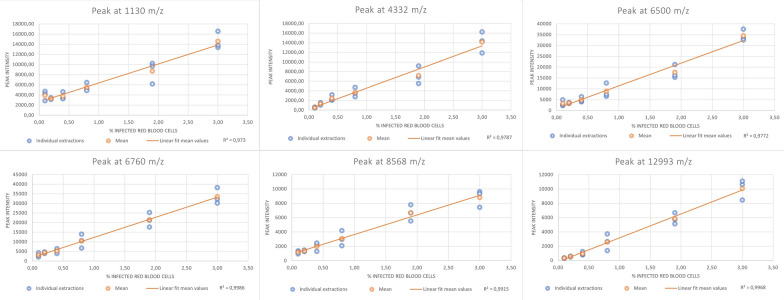
Quantification of parasitaemia
A linear relationship was seen between peak intensity and % IRBC with r2 ranging from 0.98 to 0.99 (Figs. 2 and 3). Furthermore, a higher number of P. falciparum-specific peaks were seen at higher concentrations of IRBC (Table 1).
Fig. 2.
Plasmodium falciparum specific peak at 6760 m/z at different concentrations. The Plasmodium falciparum-specific peak at 6760 m/z in samples with different concentrations of infected red blood cells (IRBC). Each panel corresponds to a different concentration as indicated by the IRBC %. Traces from three independent sample preparations are shown for each concentration. Please note change in vertical scale between panels
Fig. 3.
Correlation between peak intensity and % IRBC for different Plasmodium falciparum specific peaks. Correlation between signal intensity of the Plasmodium falciparum specific peaks at 1130, 4332, 6500, 6760, 8568 and 129,993 m/z and the concentration of P. falciparum-infected red blood cells. Each panel represents a specific peak as indicated in the panel headline. Blue dots represent individual sample preparations at each concentration. Orange dots represent the mean peak intensity of the given concentration. The orange line represents a linear fit of mean peak intensity and concentration of P. falciparum-infected red blood cells
Quality controls
Genotyping confirmed strain identity as HB3, IT4 and 3D7. The control experiments did not suggest contamination of the samples. Thus, all cultures were Mycoplasma free, and automated comparison of spectra to the bacterial and fungal database showed a very low similarity with any microorganism in the database. Microscopy of negative controls did not identify any parasites.
Discussion
Findings in relations to existing literature
This study provide proof-of-concept for the use of MALDI-TOF for identification and quantification of P. falciparum in human blood. Despite the broad application in clinically microbiology, MALDI-TOF is not routinely used in parasitology [12]. Previous studies have provided early evidence of the capability of MALDI-TOF to identify different Giardia, Cryptosporidium, Blastocystis, Entamoeba, Leishmania, Trichomonas, and Trichinella species [12–14]. Like the current study, most previous studies have been done on cultured parasites and not with the use of clinical samples. For Plasmodium spp., previous attempts have been made to detect haemozoin using technologies similar to the MALDI-TOF used in the current study [15, 16]. These studies showed that haemozoin could be detected, but that the sensitivity was too low for clinical application [15–17]. Apart from the technical differences in these studies, a major difference is that the method used in the current study is based on a broad range of P. falciparum proteins instead of relying on a single residue product. Theoretically this approach can provide greater sensitivity and specificity than a hemozoin-based method. The haemozoin peaks have been reported around 500 m/z which is outside the detection area used in the current study [17, 18]. An interesting perspective of the current study is the possibility to quantify P. falciparum. Quantification is essential to inform patient management but currently microscopy is the only clinically applied method. Microscopy is time-consuming and several studies have shown large interobserver variation [7, 19]. In the current study both peak intensity and number of Plasmodium-specific peaks were found to correlate well with the concentration of P. falciparum. Both correlations could form basis for MALDI-TOF-based quantification of Plasmodium infections. Even if it should turn out to be impossible to improve the sensitivity of MALDI-TOF to a level where it can replace molecular based methods, a combination of MALDI-TOF quantification and nucleic acid detection of human Plasmodium could represent a major improvement for malaria diagnostics with respect to accuracy and time-to-result. Furthermore, MALDI-TOF-based quantification could potentially be used for treatment control, which is presently not possible with molecular methods or rapid diagnostic tests due to persistence of antigens and DNA fragments after treatment [2–5].
Limitations of the study
This study was solely based on cultured biobank samples and only included P. falciparum. Further studies using clinical samples are required to examine the clinical application of the described method. Due to the design, using cultured P. falciparum, the studied samples presumably had a higher fraction of late-stage parasites than expected in clinical samples. To account for this, cultures were synchronized but late-stage parasites were still seen in control microscopy. It is unknown how this will have affected the peaks found by MALDI-TOF, but a recent comprehensive proteomic analysis of P. falciparum has shown a substantial overlap between proteins expressed by ring-stage and late stage parasites [20]. On the other hand, the reduced number of peaks found at low parasite concentrations could be due to disappearance of peaks specific to late-stage parasites after dilution. In this study spectra analysis was based on visual inspection. While this method is very useful in early-stage research, it is a limitation for clinical application of the method. In future studies it will be key to establish a database containing spectra from all Plasmodium species, as well as other blood borne parasites for automated spectra analysis and on-the-go differential diagnostics. Lastly, the reference method has been microscopy and results are, therefore, affected by the limitation previously described associated with this method. The effect is particularly important with regards to quantification, and it could be interesting to supplement future studies with quantitative-PCR or quantitation of parasite antigens for a more precise reference method.
Future perspectives
Concentration limits for MALDI-TOF identification of blood borne bacteria are reported to be 10–1000 bacteria/µl [8]. From whole genome sequencing it has been calculated that two-third of the proteins expressed in P. falciparum are unique for the organism, a proportion that is higher than what is seen in other eukaryotes [21]. With that in mind, as well as the fact that Plasmodium parasites are considerably larger organisms than bacteria and, therefore, presumable have higher concentrations of proteins pr. organism, MALDI-TOF identification of P. falciparum should be possible at lower concentrations than the 0.1% IRBC used in this study. The direct cost of bacterial identification using MALDI-TOF is estimated to be less than 0.5 $ [22, 23]. When including depreciation of the machine, maintenance, and training, costs will vary depending on local factors such as salary levels, maintenance agreements, sample volume and estimated life-span of the MALDI-TOF platform, but overall costs have been estimated between 0.7 $ and 3.14 $ [23–25]. If a lower detection level could be achieved, it is possible that MALDI-TOF could allow cost effective malaria screening programmes. This is especially the case if MALDI-TOF proofs to be able to detect gametocytes, as this parasite stage is easily missed with microscopy and advanced PCR methods are needed for identification. Future studies focusing on enhanced extraction protocols, MALDI-TOF settings and matrix components are required to further explore these perspectives. If future research corroborates the applicability of MALDI-TOF in patient diagnosis and screening programmes, screening programmes could potentially be combined with vector control programmes. A growing number of studies have demonstrated that MALDI-TOF can distinguish between different species of Anopheles mosquitoes, and in 2017 Laroche et al. used MALDI-TOF to differentiate between Anopheles stephensi with and without Plasmodium berghei infection [13, 14, 26]. Another interesting perspective is the detection of resistance against anti-malarial drugs. Discrimination between bacterial strains with different resistance patterns based on characteristic peaks of the MALDI-TOF spectra is possible for a wide range of bacteria [27, 28]. Currently, no clinically relevant method for identification of anti-malarial drug resistance is established and anti-malarial drug resistance is, therefore, typically identified after treatment failure [29, 30]. The perspective of MALDI-TOF-based resistance testing would be targeted use of anti-malarial drugs and better surveillance of resistance development. Future studies are needed to explore this perspective. Finally, the peaks found in the MALDI-TOF spectrum represent proteins expressed by the Plasmodium parasite. Extended use of MALDI-TOF could identify proteins that are abundantly expressed and could guide studies using more advanced proteomics platforms to characterize these proteins further.
Barriers for clinical use
This study should be seen as early-stage research and future research is needed to establish basic parameters such as sensitivity, specificity, and detection limits in a clinical population before clinical application. Secondly the detection limits will need improvement to compete with the sensitivity of the currently used methods, such as RDTs and microscopy. Detection limits for microscopy and RDTs vary depending on the manufacturer of the test and the skills of the microscopist [7, 31]. The World Health Organization estimates that the detection limits of microscopy under typical field conditions are 100 parasites per µL and recommends that RDTs are only used if they have > 75% sensitivity at 200 parasites per µL [7]. The 0,1% IRBC used in this study corresponds to 5000 parasites per µL and improved sensitivity is, therefore, needed. Lastly, the availability of MALDI-TOF platforms will be a barrier in many endemic countries. MALDI-TOF is considered a basic standard equipment for microbiology laboratories in high-income countries, and there is a growing availability of the equipment in low- and middle-income countries. Yet, MALDI-TOF is currently not available in many endemic settings. With the high establishing cost, cost-effective distribution of MALDI-TOF would require a general capacity building also involving its many applications in bacterial identification.
Conclusion
Detection and quantification of P. falciparum in human blood with the use of MALDI-TOF is possible. Studies on clinical samples and novel sample processing protocols are however needed to further develop the method.
Acknowledgements
The authors would like to thank Kåre Mølbak from Statens Serum Institut, Copenhagen, Denmark, for helpful discussions and constructive feedback during the study.
Abbreviations
- EDTA
Ethylene Diamine Tetra Acetic acid
- IRBC
Infected red blood cells
- LAMP
Loop-mediated isothermal amplification
- MACS
Magnet activated cell sorting
- MALDI-TOF
Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry
- PBS
Phosphate-buffered saline
- PCR
Polymerase chain reaction
- RBC
Red blood cells
- RDTs
Rapid diagnostic tests
- RPM
Revolutions per minute
Author contributions
Conceptualization: MAS. Methodology: MAS, CSJ, TS and JK. Investigation: MAS and TS. Formal analysis: MAS. Writing—Original draft: MAS. Writing—Review & editing: MAS, CSJ, TS and JK.
Funding
Open access funding provided by Royal Library, Copenhagen University Library.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The donation of blood for parasite culturing and negative controls were reviewed by the regional ethics committee that found that this did not require formal ethical approval. Blood collection was performed by licensed doctors after informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO. World malaria report 2022. Geneva, World Health Organization, 2022.
- 2.Iqbal J, Siddique A, Jameel M, Hira PR. Persistent histidine-rich protein 2, parasite lactate dehydrogenase, and panmalarial antigen reactivity after clearance of Plasmodium falciparum monoinfection. J Clin Microbiol. 2004;42:4237–4241. doi: 10.1128/JCM.42.9.4237-4241.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abba K, Deeks JJ, Olliaro PL, Naing C-M, Jackson SM, Takwoingi Y, et al. Rapid diagnostic tests for diagnosing uncomplicated P. falciparum malaria in endemic countries. Cochrane Database Syst Rev. 2011;2011:CD008122. doi: 10.1002/14651858.CD008122.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vafa Homann M, Emami SN, Yman V, Stenström C, Sondén K, Ramström H, et al. Detection of malaria parasites after treatment in travelers: a 12-months longitudinal study and statistical modelling analysis. EBioMedicine. 2017;25:66. doi: 10.1016/j.ebiom.2017.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haanshuus CG, Mørch K. Detection of remaining Plasmodium DNA and gametocytes during follow up after curative malaria treatment among returned travellers in Norway. Malar J. 2020;19:296. doi: 10.1186/s12936-020-03367-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Giemsa G. Eine Vereinfachung und Vervollkommnung meiner methylenblau-Eosin-Färbemethode zur Erzielung der Romanowsky-Nocht’schen Chromatinfärbung. Centralbl Bakteriol. 1904;32:307–313. [Google Scholar]
- 7.WHO. WHO Guidelines for malaria. Geneva, World Health Organization; 2022.
- 8.Cuadros E. Direct identification of pathogens from blood cultures by MALDI-TOF technology. In: Cobo F, editor. The use of mass spectrometry technology (MALDI-TOF) in clinical microbiology. Academic Press; 2018.
- 9.Nielsen MA, Staalsoe T. Establishment of long-term in vitro cultures of Plasmodium falciparum In: Moll K, Kaneko A, Scherf A, Wahlgren M, editors. Methods Malaria Research. 6th edn. 2013, p. 3–5.
- 10.Leitgeb A. Selection of trophozoites by using magnetic cell sorting (MACS). In: Moll K, Kaneko A, Scherf A, Wahlgren M, editors. Methods Malaria Research. 6th edn. 2013, p. 41–3.
- 11.Baumeister S, Winterberg M, Lingelbach K. Subcellular fractionation of IRBC: use of saponin and streptolysin O. In: Moll K, Kaneko A, Scherf A, Wahlgren M, editors. Methods Malaria Research. 6th edn. 2013, p. 97–8.
- 12.De J, Caballero D, Martin O. Application of MALDI-TOF in parasitology. In: Cobo F, editor. The use of mass spectrometry technology (MALDI-TOF) in clinical microbiology. Academic Press; 2018. pp. 235–253. [Google Scholar]
- 13.Murugaiyan J, Roesler U. MALDI-TOF MS profiling-advances in species identification of pests, parasites, and vectors. Front Cell Infect Microbiol. 2017;7:184. doi: 10.3389/fcimb.2017.00184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sánchez-Juanes F, Calvo Sánchez N, Belhassen García M, Vieira Lista C, Román RM, Álamo Sanz R, et al. Applications of MALDI-TOF mass spectrometry to the identification of parasites and arthropod vectors of human diseases. Microorganisms. 2022;10:2300. doi: 10.3390/microorganisms10112300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Demirev PA, Feldman AB, Kongkasuriyachai D, Scholl P, Sullivan D, Kumar N. Detection of malaria parasites in blood by laser desorption mass spectrometry. Anal Chem. 2002;74:3262–3266. doi: 10.1021/ac025621k. [DOI] [PubMed] [Google Scholar]
- 16.Scholl PF, Kongkasuriyachai D, Demirev PA, Feldman AB, Lin JS, Sullivan DJ, et al. Rapid detection of malaria infection in vivo by laser desorption mass spectrometry. Am J Trop Med Hyg. 2004;71:546–551. doi: 10.4269/ajtmh.2004.71.546. [DOI] [PubMed] [Google Scholar]
- 17.Christner M, Frickmann H, Klupp E, Rohde H, Kono M, Tannich E, et al. Insufficient sensitivity of laser desorption-time of flight mass spectrometry-based detection of hemozoin for malaria screening. J Microbiol Methods. 2019;160:104–106. doi: 10.1016/j.mimet.2019.04.002. [DOI] [PubMed] [Google Scholar]
- 18.Demirev PA. Mass spectrometry for malaria diagnosis. Expert Rev Mol Diagn. 2004;4:821–829. doi: 10.1586/14737159.4.6.821. [DOI] [PubMed] [Google Scholar]
- 19.WHO World. Malaria Report 2021. Geneva,World Health Organization; 2021.
- 20.Siddiqui G, De Paoli A, MacRaild CA, Sexton AE, Boulet C, Shah AD, et al. A new mass spectral library for high-coverage and reproducible analysis of the Plasmodium falciparum-infected red blood cell proteome. GigaScience. 2022;11:giac008. doi: 10.1093/gigascience/giac008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gardner MJ, Hall N, Fung E, White O, Berriman M, Hyman RW, et al. Genome sequence of the human malaria parasite Plasmodium falciparum. Nature. 2002;419:498–511. doi: 10.1038/nature01097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dhiman N, Hall L, Wohlfiel SL, Buckwalter SP, Wengenack NL. Performance and cost analysis of matrix-assisted laser desorption ionization-time of flight mass spectrometry for routine identification of yeast. J Clin Microbiol. 2011;49:1614–1616. doi: 10.1128/JCM.02381-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tran A, Alby K, Kerr A, Jones M, Gilligan PH. Cost savings realized by implementation of routine microbiological identification by matrix-assisted laser desorption ionization-time of flight mass spectrometry. J Clin Microbiol. 2015;53:2473–2479. doi: 10.1128/JCM.00833-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seng P, Abat C, Rolain JM, Colson P, Lagier JC, Gouriet F, et al. Identification of rare pathogenic bacteria in a clinical microbiology laboratory: impact of matrix-assisted laser desorption ionization-time of flight mass spectrometry. J Clin Microbiol. 2013;51:2182–2194. doi: 10.1128/JCM.00492-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ge MC, Kuo AJ, Liu KL, Wen YH, Chia JH, Chang PY, et al. Routine identification of microorganisms by matrix-assisted laser desorption ionization time-of-flight mass spectrometry: success rate, economic analysis, and clinical outcome. J Microbiol Immunol Infect. 2017;50:662–668. doi: 10.1016/j.jmii.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 26.Laroche M, Almeras L, Pecchi E, Bechah Y, Raoult D, Viola A, et al. MALDI-TOF MS as an innovative tool for detection of Plasmodium parasites in Anopheles mosquitoes. Malar J. 2017;16:5. doi: 10.1186/s12936-016-1657-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Singhal N, Kumar M, Kanaujia PK, Virdi JS. MALDI-TOF mass spectrometry: an emerging technology for microbial identification and diagnosis. Front Microbiol. 2015;6:791. doi: 10.3389/fmicb.2015.00791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rojo-Martín MD. Detecting bacterial resistance, biomarkers, and virulence factors by MALDI-TOF mass spectrometry. In: Cobo F, editor. The use of mass spectrometry technology (MALDI-TOF) in clinical microbiology. Academic Press; 2018. pp. 113–26.
- 29.Hastings IM, Felger I. WHO antimalarial trial guidelines: good science, bad news? Trends Parasitol. 2022;38:933–941. doi: 10.1016/j.pt.2022.08.005. [DOI] [PubMed] [Google Scholar]
- 30.Bayih AG, Debnath A, Mitre E, Huston CD, Laleu B, Leroy D, et al. Susceptibility testing of medically important parasites. Clin Microbiol Rev. 2017;30:647–669. doi: 10.1128/CMR.00111-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.WHO. Malaria rapid diagnostic test performance: results of WHO product testing of malaria RDTs: round 8 (2016–2018). Geneva, World Health Organization; 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.