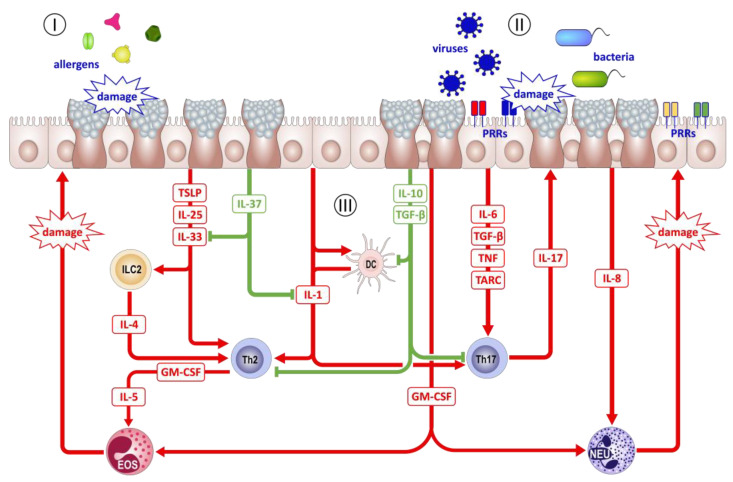
Figure 3.
Immune functions of the airway epithelium in asthma pathogenesis. (I) Airway epithelial cells (AECs) react to damage by allergens with the release of mediators, such as thymic-stromal lymphopoietin (TSLP), interleukin (IL) 25, and IL-33, three factors that on the one hand stimulate innate lymphoid tissue cells (ILC2) to release IL-4, which in turn favors T helper 2 (TH2) cell differentiation, and on the other hand support production of TH2 type cytokines, such as IL-5, by TH2 cells. IL-5, together with GM-CSF, directs the recruitment of eosinophils to the inflammation site, which, in the case of allergic asthma, leads to further damage to the epithelium. (II) Contact with or infection with bacteria or respiratory viruses also leads to damage to AECs. AECs are able to recognize such pathogens through pattern recognition receptors (PRRs) and respond with the release of cytokines, such as IL-1, IL-6, and tumor necrosis factor (TNF) and the thymus and activation chemokine (TARC), which generally promote a local inflammatory reaction as well as the differentiation and recruitment of TH17 cells. TH17 cells, in turn, release proinflammatory IL-17, which drives the release of IL-8 by AECs, leading to chemotaxis of neutrophils and, thus, further damage to the airway mucosa. (III) While such a reaction to inhaled pathogens typically leads to aggravation of airway inflammation and exacerbation of established asthma, AECs are also capable of regulating inflammatory reactions. The release of IL-37 directly inhibits the proinflammatory effect of IL-1 as well as the TH2-favoring effects of IL-33, while the release of IL-10 and transforming growth factor (TGF) β generally downregulates the activity of all types of inflammation in order to foster repair processes. Red arrows indicate proinflammatory effects, whereas green lines indicate anti-inflammatory effects.