Figure 4. Alterations to pancreas size and organization during type 1 diabetes progression.
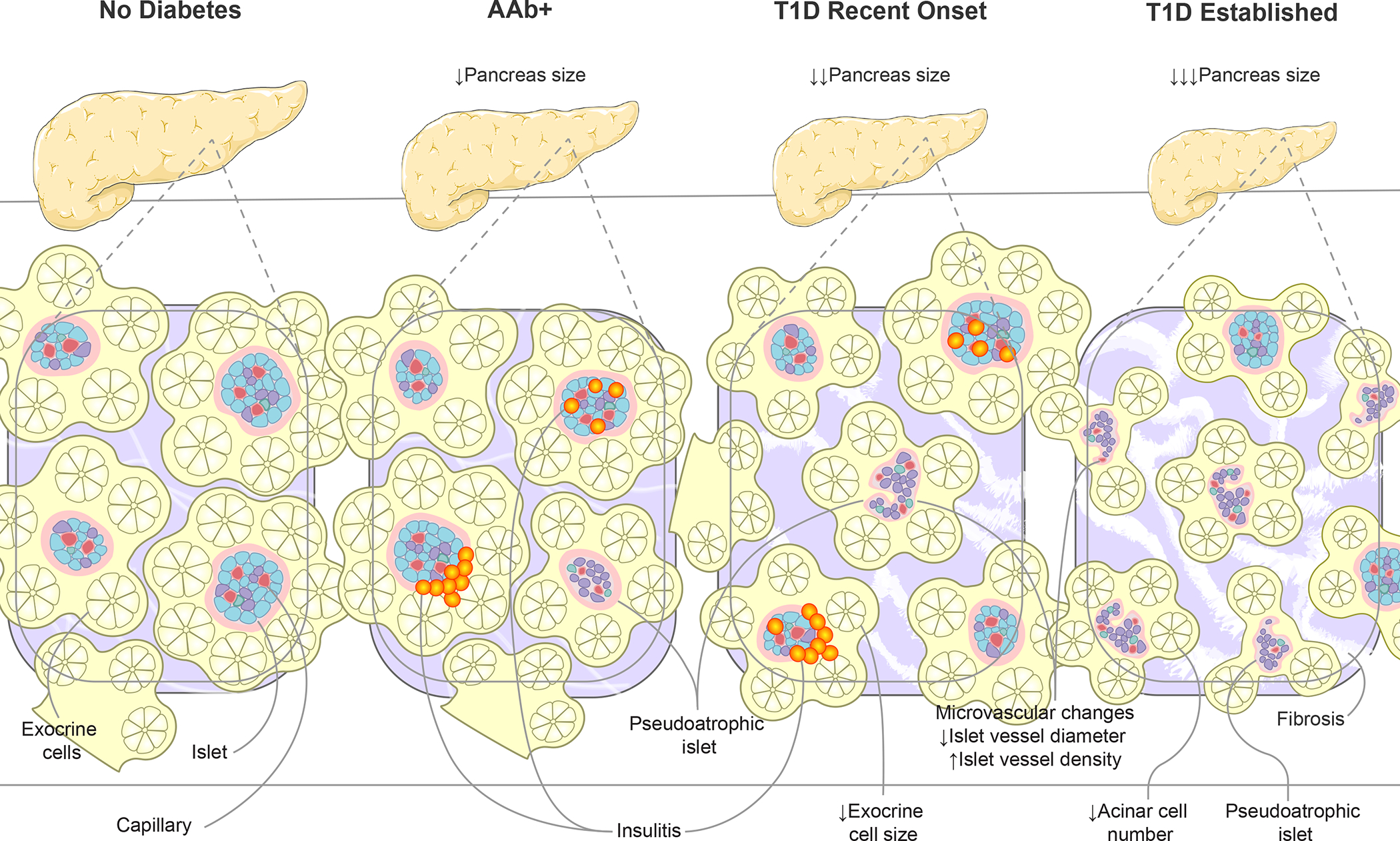
Disease progression, from AAb seroconversion (stage 1–2) to recent-onset and established type 1 diabetes (stage 3), is associated with increasingly smaller pancreas organ size. Insets show highly vascularized islets surrounded by exocrine cell bundles arranged in acini. Asynchronous islet infiltration and β-cell destruction result in a heterogeneous mixture of normal, insulitic, and pseudoatrophic islets in AAb+ and recent onset type 1 diabetes pancreas while the majority of islets are pseudoatrophic in longstanding type 1 diabetes. Insulin negative pseudoatrophic islets have distinct microvascular alterations including reduced vessel diameter and increase vessel density. Within the exocrine compartment, recent onset type 1 diabetes is associated with smaller exocrine cells, eventually leading to reduced acinar cell number in established disease. The exocrine pancreas is commonly characterized by periductal and interlobular fibrosis after type 1 diabetes onset. Arrows depict direction of change. AAb+, islet autoantibody positive; T1D, type 1 diabetes.
