Abstract
Background and Aim:
Epidemiological studies conducted mostly in low- and middle-income countries have found a positive association between household combustion of wood and lung cancer. However, most studies have been retrospective, and few have been conducted in the United States where indoor wood-burning usage patterns differ. We examined the association of exposure to indoor wood smoke from fireplaces and stoves with incident lung cancer in a U.S.-wide cohort of women.
Methods:
We included 50,226 women without prior lung cancer participating in the U.S.-based prospective Sister Study. At enrollment (2003-2009), women reported frequency of use of wood-burning stoves and/or fireplaces in their longest-lived adult residence. Cox regression was used to estimate adjusted hazard ratios (HRadj) and 95% confidence intervals (CI) for the association between indoor wood-burning fireplace/stove use and incident lung cancer. Lung cancer was self-reported and confirmed with medical records.
Results:
During an average 11.3 years of follow-up, 347 medically confirmed lung cancer cases accrued. Overall, 62.3% of the study population reported the presence of an indoor wood-burning fireplace/stove at their longest-lived adult residence and 20.6% reported annual usage of ≥30 days/year. Compared to those without a wood-burning fireplace/stove, women who used their wood-burning fireplace/stove ≥30 days/year had an elevated rate of lung cancer (HRadj = 1.68; 95% CI = 1.27, 2.20). In never smokers, positive associations were seen for use 1-29 days/year (HRadj = 1.64; 95% CI = 0.87, 3.10) and ≥;30 days/year (HRadj = 1.99; 95% CI = 1.02, 3.89). Associations were also elevated across all income groups, in Northeastern, Western or Midwestern U.S. regions, and among those who lived in urban or rural/small town settings.
Conclusions:
Our prospective analysis of a cohort of U.S. women found that increasing frequency of wood-burning indoor fireplace/stove usage was associated with incident lung cancer, even among never smokers.
Keywords: Wood smoke, heating, cooking, lung cancer, women
Introduction
Wood smoke is a complex mixture consisting of particulate matter, gases, and hundreds of different chemicals, some of which have been classified as hazardous air pollutants and carcinogens (e.g., benzene) (Pope et al. 2011, NTP 2014, IARC 2016). The World Health Organization (2018) estimates that 3.8 million people globally will die from an illness resulting from household air pollution by burning of solid fuels and kerosene; of these deaths, 8% are estimated to be from lung cancer. Lung cancer is the second most diagnosed cancer and the leading cause of cancer-related death among U.S. women (U.S. Cancer Statistics Working Group 2022).
In the United States, wood smoke is emitted primarily from wood stoves, fireplaces, and boilers. Almost two million U. S. households use wood as their primary heating fuel (U.S. Energy Information Administration 2022); some restaurants use wood for cooking. Studies in the United States have found higher levels of fine particulate matter (PM2.5) in homes with wood stoves compared to those without a stove; the highest levels were those using older stoves (Fleisch et al. 2010). Wood smoke is also a major contributor to outdoor air pollution, contributing nearly 80% of wintertime PM in some geographical areas (Ward et al. 2012).
The International Agency for Research on Cancer (IARC 2010) has characterized indoor emissions from household combustion of biomass fuel (primary wood) as probably carcinogenic to humans (Group 2A) based on more than a dozen case-control studies of indoor wood burning and lung cancer, and studies in experimental animals. A pooled analysis from studies in higher income countries in North America and Europe, where wood burning is primarily used for heating rather than both cooking and heating, suggest that wood users have a 20% higher risk of lung cancer compared to nonsolid-fuel users (Lissowska et al. 2005, Hosgood et al. 2010). Longterm exposure to indoor wood combustion was associated with a 2.5-fold excess risk among nonsmokers in Brazil and seven European countries. However, these studies relied on retrospective exposure assessments for wood smoke exposure and may be subject to recall bias. Using the same prospective study population as presented here, the Sister Study cohort, White and Sandler (2017) found that exposure to wood-burning stoves/fireplaces was associated with an increased incidence of breast cancer.
Wood smoke exposure may differ by sociodemographic and geographic characteristics, with poorer and rural populations being disproportionately exposed (Noonan et al. 2015, Rogalsky et al. 2014). Therefore, this study aims to address whether exposure to indoor wood smoke from fireplaces and stoves is associated with incident lung cancer in a large prospective cohort of U.S. women with consideration of how the association varies by sociodemographic and geographic characteristics.
Methods
Study population and exclusion criteria
The Sister Study is an ongoing prospective cohort of over 50,000 women living in the United States, including Puerto Rico, who have had a sister diagnosed with breast cancer. Participants were enrolled from 2003-2009 (Sandler et al. 2017). Sociodemographic, behavioral, and physical characteristics were collected via questionnaires given at baseline. Sister Study participants provided written informed consent and the study is overseen by the National Institutes of Health Institutional Review Board. Sister Study follow-up data collection is on-going (Sandler et al. 2017). This present analysis includes incident lung cancer diagnosed and reported through September 30, 2019 (Sister Study Data Release 9.1).
Sister Study participants were excluded from the current study if they withdrew from the study (N=3), had missing data on presence of a fireplace or stove at the longest-lived adult residence (N=119), had pre-baseline lung cancer (N=63), had missing or insufficient data on lung cancer status or timing (uncertain lung cancer diagnosis or unknown timing of lung cancer diagnosis, N=19), or had missing or zero person-years of follow-up (N=281). After exclusion criteria, 50,399 (99.0%) women remained in the study sample.
Indoor wood burning stove and/or fireplace exposure
Indoor wood smoke exposure was collected at enrollment. For the longest-lived adult residence, participants were asked whether there was a fireplace or wood-burning stove (yes/no), whether wood was used as a fuel source for fireplaces or stoves in the longest-lived adult residence (yes/no), and annual usage of wood-burning stove or fireplace (0-365 days). Annual use of wood-burning stove or fireplace was categorized as either not having a stove or fireplace or using it zero days/year, 1-29 days/year of use, or 30-365 days/year of use. Participants were also asked the same questions regarding the presence and usage of wood-burning stoves and fireplaces at their baseline residence, if that was different from the long-lived residence.
Also, participants were asked to list the main source of heat (electricity, gas, fuel oil, wood, other fuel sources), main energy source for stove top cooking (electricity, gas, other fuel sources), and other fuel sources used in fireplaces and/or stoves (no fireplace, natural gas/propane, artificial logs, and other fuel sources).
Incident lung cancer
Post-baseline incident lung and bronchus cancer (ICD-10:C34) was identified through September 30, 2019. Lung cancers identified as in situ (D02.2; N=2) or borderline (N=1) were categorized as non-events and censored at the time of their diagnosis. Incident lung cancer was self- (or next of kin) reported and confirmed using medical records or the National Death Index (NDI) and death certificates (DC). Due to the low positive predictive value of self-reported lung cancer among Sister Study participants (76.9%), we further excluded self- or next-of-kin reported lung cancer without any medical or death record confirmation (N=170), though we note that this level of reporting accuracy was similar to other prospective cohort studies (Bergmann et al. 1998, Colditz et al. 1986). Supplemental Table 1 provides participant characteristics of excluded and included lung cancer cases. After exclusion, 50,226 (98.7%) women remained in the final study population.
For lung cancer cases with histopathology data (N=199), we grouped tumor subtypes into adenocarcinomas (ICD-O-3: 8046, 8140-8255, 8480-8481, 8550-8551), other non-small cell lung cancer (large cell carcinoma: ICD-O-3: 8012-8031, 8310; squamous cell carcinoma: ICD-O-3: 8050-8076), small cell carcinomas (ICD-O-3: 8040-8045), and other or unknown histologies (ICD-O-3: 8000-8010, 8560, 8720-8980).
Statistical analysis
Hazard ratios (HRs) and 95% confidence intervals (95% CI) were estimated using Cox proportional hazards regression models to assess the association between indoor wood smoke from fireplaces and stoves and incident lung cancer. Follow-up began at enrollment, age at entry into cohort was used at the beginning of follow-up, and age was used as the time scale. We assessed Cox proportional hazards assumptions using diagnostic tests including plot analyses and time interaction models. To calculate p-for-trend across tertiles of annual wood burning usage, a median value for each tertile was used as a linear term in models.
To identify potential confounders, we used a directed acyclic graph (DAG) (Supplemental Figure 1) and existing literature. Covariates include: highest educational attainment (high school graduate or below, some college or an Associates’ degree, Bachelor’s degree or above), marital status (never married, married or living as married, or previously married including divorced, widowed, or separated), race/ethnicity (non-Hispanic White, Non-Hispanic Black, Hispanic or other race/ethnicity), total household income (≤$49,999, $50,000-$99,999, ≥$100,000), smoking status (never smoker, ever smoker (i.e., past or current smoker)), total smoking intensity (packs/year), years exposed to environmental tobacco smoke (ETS) (years), and urban status at longest-lived residence (urban, suburban, rural or small town). To account for high missingness for total household income (N=1,950), values were imputed using the fully conditional specification multiple imputation method. Participants with missing data for other covariates (<3%) were excluded from complete case analyses.
To further explore the data, we stratified by smoking status, duration of longest-lived residence (< 15 years, ≥ 15 years), race/ethnicity, urban status at longest-lived residence, family history of lung cancer, Census region excluding Puerto Rico for longest-lived residence (Northeast, Midwest, South, West) and household income at baseline. Interaction terms for each wood smoke exposure and potential modifying factor were included in models to test for heterogeneity with a p-value <0.05. All our analysis was performed using data from the entire final study population, producing stratified effect estimates using separate terms for strata specific effects. We also evaluated whether the association varied by histological subtype (adenocarcinoma, other non-small cell lung cancer; excluding small cell, other, unknown, and noncoded histologies due to a limited number of cases).
Though few participants reported coal as a primary or concurrent fuel source, we conducted a sensitivity analysis excluding all participants who reported coal as a fuel for their fireplace or stove (N=325) or as their main heating fuel (N=32). We included a sensitivity analysis limiting to participants whose current residence was also their longest-lived adult residence. We also examined additional fuel sources reported at the participant’s longest-lived residence, including main source of heat at residence, energy sources for stove top cooking, and alternative fuel sources used in fireplaces and/or stoves.
STATA v.14.2 was used for all statistical analyses, DAGitty (http://www.daggity.net) was used to create the DAG, and R v.4.2.1 was used to create the main figures.
Results
The study population’s baseline characteristics by lung cancer status are summarized in Table 1. Overall, the mean follow-up time for all participants was 11.3 years (range: 0.10 – 15.9 years), and 347 women were diagnosed with lung cancer. Compared to those without a wood-burning fireplace or stove, women with a wood-burning fireplace or stove were more likely to be Non-Hispanic white, had higher educational attainment, had higher household income, more often married or living as married, more likely to have lived in the Western U.S., less often lived in an urban setting at their longest-lived residence, had higher mean pack-years, and had lower mean exposure to ETS.
Table 1.
Participant characteristics of Sister Study participants by presence of wood-burning stove/fireplace at longest-lived residence (N=50,226)
| No stove/fireplace (N=18,949) | Has stove/fireplace (N=31,277) | |||
|---|---|---|---|---|
| Participant characteristic | N | Mean (range) | N | Mean (range) |
|
| ||||
| Age at baseline, years (mean, range) | 18,949 | 55.0 (35.0 – 76.5) | 31,277 | 56.0 (35.1 - 76.5) |
| Follow-up time, years (mean, range) | 18,949 | 11.1 (0.1 – 15.7) | 31,277 | 11.5 (0.1 - 15.9) |
| Total pack-years (mean, range) | 18,818 | 7.2 (0.0 - 130.0) | 31,135 | 5.8 (0.0 - 120.3) |
| Total years exposed to ETS (mean, range) | 18,382 | 23.5 (0.0 - 75.0) | 30,588 | 21.1 (0.0 - 75.0) |
| N | % | N | % | |
|
|
||||
| Race/ethnicity | ||||
| Non-Hispanic white | 14,258 | 75.3 | 27,828 | 89.0 |
| Non-Hispanic black | 2,397 | 12.7 | 1,980 | 6.3 |
| Hispanic/other | 2,288 | 12.1 | 1,465 | 4.7 |
| Highest educational attainment | ||||
| High school degree or less | 3,878 | 20.0 | 3,878 | 12.4 |
| Some college/Associates’ degree | 7,103 | 37.5 | 9,812 | 31.4 |
| Bachelor’s degree or above | 8,061 | 42.6 | 17,583 | 56.2 |
| Household income | ||||
| Less than $50,000 | 7,151 | 37.7 | 5,682 | 18.2 |
| $50,000 - $99,999 | 7,929 | 41.8 | 12,612 | 40.3 |
| At least $100,000 | 3,869 | 20.4 | 12,983 | 41.5 |
| Marital status | ||||
| Never married | 1,677 | 8.9 | 1,042 | 3.3 |
| Married/living as married | 12,400 | 65.5 | 25,185 | 80.5 |
| Previously married | 4,869 | 25.7 | 5,044 | 16.1 |
| Longest-lived Census region | ||||
| Northeast | 3,770 | 20.2 | 5,508 | 17.7 |
| Midwest | 5,730 | 30.7 | 8,363 | 26.9 |
| South | 5,572 | 29.9 | 9,464 | 30.3 |
| West | 2,718 | 14.6 | 7,824 | 25.1 |
| Puerto Rico | 870 | 4.7 | 6 | 0.02 |
| Urban status at longest-lived residence | ||||
| Urban | 5,388 | 28.6 | 4,922 | 15.8 |
| Suburban | 5,995 | 31.8 | 13,751 | 44.1 |
| Rural or small town | 7,474 | 39.6 | 12,515 | 40.1 |
| Smoking status | ||||
| Never | 10,335 | 54.6 | 17,955 | 57.4 |
| Ever (former or current) | 8,611 | 45.4 | 13,319 | 42.6 |
ETS = environmental tobacco smoke
Missing: total pack years (N=273), total years exposed to ETS (N=1,256), race/ethnicity (N=10), highest educational attainment (N=7), marital status (N=9), longest-lived Census region (N=371), urban status at longest-lived residence (N=181), smoking status (N=6)
Overall, 62.3% of the study population reported the presence of an indoor wood-burning stove and/or fireplace at their longest-lived residence, and only 20.6% reported annual usage of at least 30 days/year.
In fully adjusted models (Table 2, Model 2), we found positive associations for incident lung cancer and both presence of a wood-burning fireplace or stove (HRadj = 1.42; 95% CI = 1.11, 1.81) and wood used as a fuel source in wood-burning fireplaces or stoves (HRadj = 1.43; 95% CI = 1.14, 1.79). Compared to those without a wood-burning fireplace or stove or zero days/year usage, the highest incidence of lung cancer was seen in women reporting wood-burning fireplace/stove usage of at least 30 days/year (HRadj = 1.68; 95% CI = 1.27, 2.20; p-for-trend < 0.001).
Table 2.
The association between the presence and usage of a wood-burning fireplace and/or stove presence and incident lung cancer
| Model 11 |
Model 22 |
|||||||
|---|---|---|---|---|---|---|---|---|
| N (cases/noncases) | HR | 95% CI | p-trend | N (cases/noncases) | HRadj | 95% CI | p-trend | |
|
|
|
|||||||
| Presence of wood-burning fireplace/stove | ||||||||
| No wood-burning fireplace/stove (ref) | 119/18,830 | 1.00 | --- | 110/18,075 | 1.00 | --- | ||
| Yes | 228/31,049 | 1.05 | 0.84 – 1.31 | 219/30,160 | 1.42 | 1.11 - 1.81 | ||
|
| ||||||||
| Used wood as a source of fuel | ||||||||
| No wood-burning fireplace/stove or no wood use (ref) | 191/30,949 | 1.00 | --- | 179/29,825 | 1.00 | --- | ||
| Yes | 156/18,915 | 1.25 | 1.01 - 1.54 | 150/18,396 | 1.43 | 1.14 - 1.79 | ||
|
| ||||||||
| Annual wood-burning fireplace/stove use | ||||||||
| No wood-burning fireplace/stove or no wood use (ref) | 163/25,083 | 1.00 | --- | 0.002 | 152/24,110 | 1.00 | --- | <0.001 |
| 1-29 days/year | 86/14,458 | 0.88 | 0.68 - 1.15 | 84/14,088 | 1.12 | 0.85 – 1.48 | ||
| At least 1 month/year | 98/10,257 | 1.40 | 1.09 - 1.80 | 93/9,968 | 1.68 | 1.27 – 2.20 | ||
Age accounted for as underlying time scale
Aditionally adjusted for race/ethnicity (NH black, NH white, Hispanic/other), education (HS or less, some college, Bachelors or above), urban status at longest-lived residence (urban, suburban, rural/small town), smoking status (never, ever), pack years, total years exposed to environmental tobacco smoke, marital status (single, married, previously married), income status (<$50,000, $50,000-$99,999, $100,000+)
We did not see evidence of effect modification by smoking status; elevated estimates were seen for both ever- and never-smoking women (Table 3). Compared to those without a wood-burning fireplace or stove, the incidence of lung cancer among never smokers was higher among women using wood-burning fireplaces/stoves 1-29 days/year (HRadj = 1.64; 95% CI = 0.87, 3.10) and at least 30 days/year (HRadj = 1.99; 95% CI = 1.02, 3.89), with a suggestive linear exposure-response trend (p-for-trend=0.08). A 54% increased incidence of lung cancer was observed among smokers using wood-burning fireplaces/stoves at least 30 days/year (HRadj = 1.54; 95% CI = 1.15, 2.07; p-for-trend = 0.003).
Table 3.
The association between wood-burning fireplace and/or stove presence and usage and incident lung cancer, stratified by smoking status1
| Never smoker |
Ever (current or former) smoker |
|||||||
|---|---|---|---|---|---|---|---|---|
| N cases | HRadj | 95% CI | p-trend | N cases | HRadj | 95% CI | p-trend | |
|
|
|
|||||||
| Presence of wood-burning stove/fireplace | ||||||||
| No (ref) | 6 | -- | --- | 107 | 1.00 | --- | ||
| Yes | 52 | -- | -- | 167 | 1.14 | 0.89 - 1.48 | ||
|
| ||||||||
| Used wood as a source of fuel | ||||||||
| No (ref) | 28 | 1.00 | --- | 154 | 1.00 | --- | ||
| Yes | 30 | 1.62 | 0.95 - 2.75 | 120 | 1.38 | 1.08 - 1.77 | ||
|
| ||||||||
| Annual wood-burning fireplace/stove use | ||||||||
| No fireplace/stove or zero use (ref) | 20 | 1.00 | --- | 0.08 | 135 | 1.00 | --- | 0.003 |
| 1-29 days used/year | 21 | 1.64 | 0.87 - 3.10 | 63 | 0.99 | 0.73 – 1.35 | ||
| At least 1 month used/year | 17 | 1.99 | 1.02 – 3.89 | 76 | 1.54 | 1.15 – 2.07 | ||
Adjusted for race/ethnicity (NH black, NH white, Hispanic/other), education (HS or less, some college, Bachelors or above), urban status at longest-lived residence (urban, suburban, rural/small town), marital status (single, married, previously married), income status (<$50,000, $50,000-$99,999, $100,000+), total years exposed to environmental tobacco smoke P-for-heterogeneity (used wood as fuel source) = 0.64; p-for-heterogeneity (annual wood-burning fireplace/stove usage) = 0.40
Length of time living at the longest adult residence did not substantially modify the associations between wood burning and lung cancer incidence (Figure 1.A). The increased estimate associated with a wood-burning fireplaces and/or stoves at least 30 days/year was more pronounced, albeit less precise, for those living in an urban area (HRadj = 2.64; 95% CI = 1.43, 4.87; p-for trend = 0.003) (Figure 1.B). Statistically significant associations were observed for those in rural/small settings (HRadj = 1.74; 95% CI = 1.17, 2.57; p-for trend = 0.003) and no increased incidence was found for those in suburban settings, although tests for interaction were not statistically significant (p-for-heterogeneity = 0.26). We also stratified by U.S. Census region (Figure 1.C); the highest incidence of lung cancer in the highest use frequency category was seen for participants in the Midwestern (HRadj = 2.58; 95% CI = 1.52, 4.38), Northeastern (HRadj = 2.30; 95% CI = 1.25, 4.26), and Western (HRadj = 1.37; 95% CI = 0.81, 2.33) U.S. Census regions.
Figure 1.
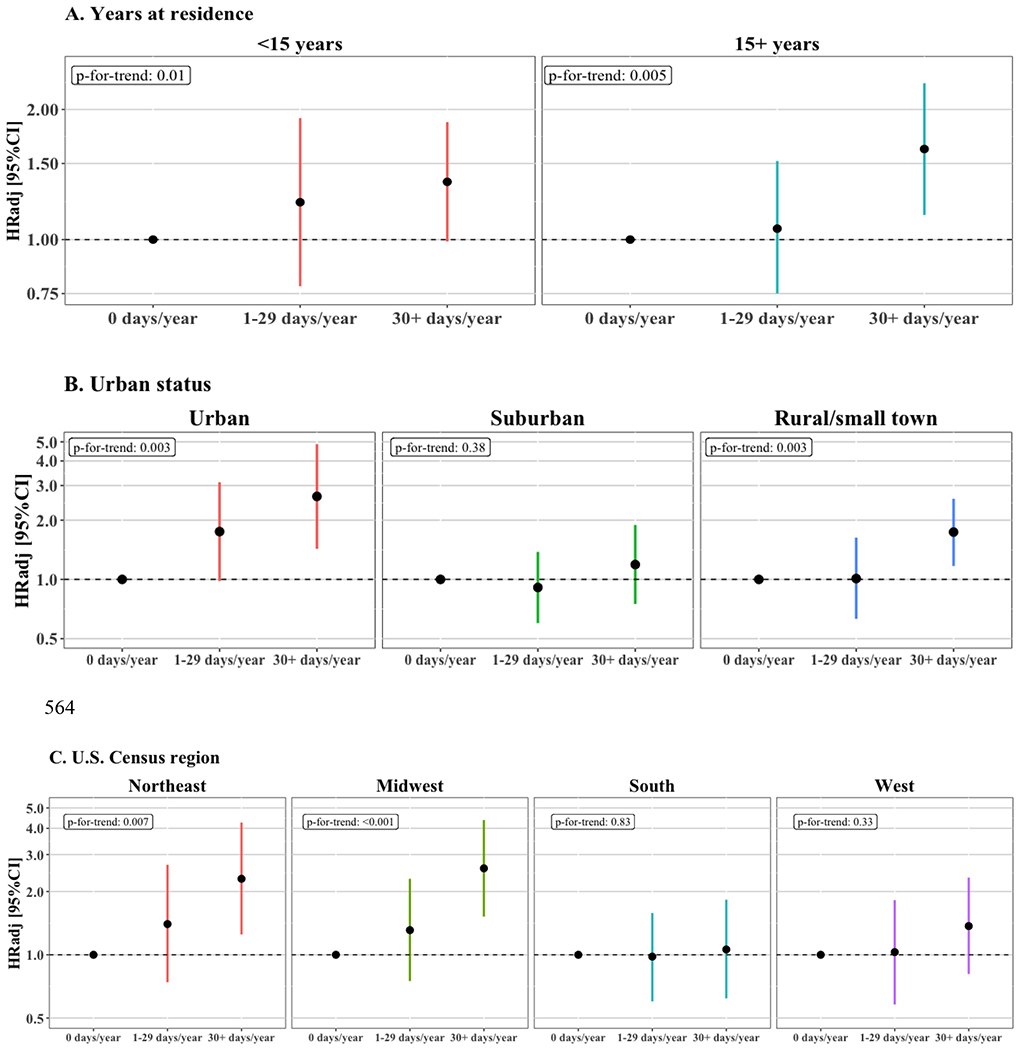
Adjusted HRs (95% CI) of wood-burning fireplace and/or stove usage and incident lung cancer, stratified by residential factors at longest-lived residence, including (A) years lived at residence (<15 years, 15+ years), (B) urban status (urban, suburban, rural/small town), and (C) U.S. Census region (Northeast, Midwest, South, West). All models adjusted for race/ethnicity, education, smoking status, pack years, total years exposed to environmental tobacco smoke, marital status, income status. Models A and C were additionally adjusted for urban status. Test for trend values across tertiles of annual wood burning usage are reported as p-for-trend values in top left of each plot. P-for-heterogeneity for A: 0.87; p-for-heterogeneity for B: 0.26; p-for-heterogeneity for C: 0.34. All plotted values are on a log scale.
In race-stratified analyses, lung cancer incidence was elevated among non-Hispanic White participants using wood-burning fireplaces and/or stoves at least 30 days/year (HRadj=1.71; 95% CI = 1.29, 2.26; p-for-trend < 0.001), but sample sizes were too small to evaluate associations in other groups. Associations did not vary by household income (Supplemental Table 2) or by family history of lung cancer (Supplemental Table 3).
Wood burning was positively associated with lung adenocarcinoma rates, but not the rates of other non-small cell lung cancers (Supplemental Table 4).
We did not see a change in the results when we restricted to only those whose longest-lived residence was also their residence at baseline, or when coal users were excluded from final models (not shown). Rate of lung cancer was similarly elevated for non-wood fuel sources used in fireplaces/stoves, including natural gas/propane (HRadj = 1.29; 95% CI = 0.91, 1.82) and artificial logs (HRadj = 1.33; 95% CI = 0.97, 1.83) (Supplemental Table 5.1). As shown in Supplemental Table 5.2, compared to using electricity as the main heating source, use of other fuel sources was associated with higher rates (HRadj=1.32; 95% CI=0.83, 2.09); as was use of wood as the main fuel source (HRadj=1.40; 95% CI=0.73, 2.66), but based on only on a small number of exposed cases (N=11). Lastly, we did not find an association between lung cancer and types of energy sources for stovetop cooking (Supplemental Table 5.3).
Discussion
In this large cohort of U.S. women, we observed higher rates of lung cancer with higher frequency of use of indoor wood-burning fireplaces and/or stoves in participants’ longest-lived residence, including among non-smoking women. To our knowledge, this is the first prospective analysis of indoor stoves and fireplaces in relation to lung cancer risk. This study contributes to the existing evidence base suggesting that indoor air pollution from stoves/fireplaces may contribute to lung cancer risk and suggests that this holds true even in populations where wood-burning is predominately not used for cooking or heating inside the home.
Our prospective study results largely align with previous case-control studies of indoor wood burning and lung cancer in women (Sobue 1990, Ko et al. 1997, Le et al. 2001, Garcia-Sancho et al. 2012, Hernandez-Garduno et al. 2004, Hosgood et al. 2010, Tang et al. 2010, Vermeulen et al. 2019, Phukan et al. 2014). Our findings are also consistent with IARC’s classification of biomass burning (primarily wood) as a probable lung carcinogen (IARC 2010). Smoke from wood burning contains known and suspected lung carcinogens, including benzene, 1,3-butadiene, polycyclic aromatic hydrocarbons, and other hazardous air pollutants. The mechanistic pathways by which wood smoke exposure causes cancer are not fully elucidated; however, wood smoke has been found to be genotoxic, inducing DNA damage and mutations (Mumford et al. 1993, Ozturk et al. 2002, Musthapa et al. 2004). Wood smoke can cause immunosuppression and chronic inflammation via inflammatory cytokines (IARC 2010), and induces oxidative stress (IARC 2010), which may lead to tumorigenesis.
Similarly, both natural gas/propane and artificial logs used as a fuel source in fireplaces or stoves were also associated with an increased incidence of lung cancer. Lung carcinogens have been identified in household gas emissions (Lebel et al. 2022, Dutton et al. 2001) and manufactured synthetic logs (Gullet et al. 2003). When examining just fuel sources of stovetop cooking, we did not find an increased incidence in lung cancer for women using natural gas, compared to electricity.
The pronounced associations of lung cancer in relation to wood-burning exposure metrics when restricting to never-smoking women in this study provides further evidence of wood smoke as an independent risk factor of lung cancer. In a pooled analysis of four case-control studies of nonsmoking women from Europe and North America (Hosgood et al. 2010), the association of wood use and lung cancer was slightly elevated but not significant (OR = 1.15; 95% CI = 0.81, 1.64). Particularly among low- and middle-income countries, nonsmoking women may be at increased exposure to wood burning due to greater cooking and traditional household roles (Delgado et al. 2005, Torres-Duque et al. 2008).
Overall, our results are consistent with studies of women from other Western countries; the risk estimate of the pooled analyses for all women from Europe and North America (Hosgood et al. 2010) found a similar higher rates of lung cancer using wood as their predominant indoor fuel source (OR=1.19, 95% CI = 0.94, 1.51). Globally, indoor wood use patterns significantly differ by country, region, and sociodemographic characteristics. Compared to low- and middle-income countries, the U.S. is much less reliant on wood as a primary fuel source for cooking (Bonjour et al. 2013) and heating (1.7% of U.S. population, U.S. Census Bureau 2020); however, use varies by region and socioeconomic status, with those in rural poverty at greatest exposure to residential wood smoke (Rogalsky et al. 2014).
Of histopathology data reported, adenocarcinomas represented the largest proportion of lung cancer subtypes and associations were seen between wood burning and adenocarcinoma in our study. Other studies have also found elevated risk for adenocarcinoma associated with wood use (Baez-Saldana et al. 2021, Figueroa et al. 2012, Hernandez-Garduno et al. 2004).
We found elevated associations for wood-burning among women living in urban and rural/small town settings, but not for suburban settings. Women in rural and small-town settings may more heavily rely on wood burning as a fuel type and have been estimated to have greater exposure to wood smoke in the U.S. (Noonan et al. 2015, Rogalsky et al. 2014). Estimates were highest for urban settings, although these results were more imprecise. Including urbanicity as a confounder in our main analyses to adjust for traffic-related air pollution still resulted in elevated effect estimates. Further, adjustment for urbanicity as a proxy for outdoor air pollution may not account for sources of non-traffic related air pollution, including outdoor wood burning. Evidence suggests ambient outdoor air pollution in total is a known risk factor for lung cancer (Loomis et al. 2013).
In this population, wood-burning was positively associated with lung cancer incidence in all income groups. Though we were limited by spatial granularity and smaller sample sizes, the positive association was consistently present among participants living in the Midwestern, Northeastern, and Western U.S. Further exploration into these broad geographic regions may yield spatial variations, particularly among rural populations as previously estimated (Noonan et al. 2015).
Our study population primarily used electricity and gas as their main fuel sources for cooking and heating in their longest-lived residence. As such, indoor wood burning for many is likely a secondary or tertiary fuel source. Still, an estimated 10.8 million U.S. households used wood as a fuel source in 2020 (U.S. Energy Information Agency 2022), and nondaily use can still contribute a consequential amount of wood smoke exposure. To capture women using wood-burning appliances at least seasonally, we categorized “at least one month per year” of wood-burning appliance usage as our highest use frequency category which is consistent with this not being a predominate source of heating in this population. Seasonal indoor wood-burning has been found to be a significant contributor to outdoor air pollution, particularly during colder months (Croft et al. 2017, Tsiodra et al. 2021). Ward and Lange (2010) identified higher PM concentrations in winter months associated with a higher proportion of wood-burning residences. We were also unable to compare the efficiency of wood-burning appliances, a major factor in the contribution to higher indoor air pollution in the United States. Recognizing efficiency of wood-burning appliances is a public health issue, U.S. EPA promulgated updated performance requirements in 2015 for new residential wood heaters to lower harmful emissions (U.S. EPA 2015), which may ultimately provide substantial reductions in cancer and noncancer hazard from indoor wood burning practices in the United States (Marin et al. 2022).
With a prospective study design, we reduced the potential of recall bias compared to previous retrospective case-control studies. The large Sister Study sample and US-wide enrollment allowed for examination of sex- and geographic-specific lung cancer rates. Given the large sample size of the cohort, we were able to assess effect modification by smoking status and household income. The availability of in-depth baseline survey questions on presence, use, frequency, and fuel types allowed for a greater examination of wood smoke exposure. Lastly, we were able to eliminate confounding concerns by coal co-exposure.
Demographically, our study participants are more affluent, older, and less diverse than the U.S. population of women, which may limit our generalizability. Use of wood-burning fireplaces and stoves may be an imprecise proxy for actual indoor wood smoke exposure. Since wood burning usage variables were self-reported, there is potential for nondifferential misclassification of wood smoke exposure, which would like attenuate affect estimates. To categorize wood smoke exposure, we relied on longest-lived residence, and were not able to assess lifetime exposure. Further interrogation by more granular geographic regions is needed given regional variability in climate and heating practices. Lastly, other co-exposures were unaccounted for, such as radon, poor housing quality, and other sources of wood smoke (e.g., outdoor wood burning, wildfires).
In conclusion, in this large prospective study of U.S. women, we provide evidence consistent with prior case-control studies that even infrequent exposure to indoor wood smoke is associated with a higher incidence of lung cancer, including among never smokers.
Supplementary Material
Highlights:
First prospective study of wood burning and lung cancer incidence among U.S. women
Higher wood stove/fireplace usage associated with 70% higher incidence of lung cancer
Associations were also elevated when analysis was restricted to never smokers
Suggest even occasional indoor wood burning can contribute to lung cancer
Acknowledgements
The authors would like to thank Aimee D’Alosio, Heather Carroll, and Patrick Ringwald for their assistance in dataset preparation, and Kyla Taylor, Katie O’Brien, Andy Rooney, and Scott Masten for their critical manuscript review.
Funding:
This work is supported by the Divisions of Translational Toxicology and Intramural Research at National Institute of Environmental Health Sciences (Z01ES044005, Z1AES103332).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CRediT author statement
Suril S. Mehta: Conceptualization, Methodology, Software, Formal analysis, Data Curation, Writing - Original Draft, Writing - Review & Editing, Visualization, Project administration, Supervision. M. Elizabeth Hodgson: Methodology, Data Curation, Writing - Review & Editing. Ruth M. Lunn: Conceptualization, Writing - Review & Editing. Claire E. Ashley: Data Curation, Writing - Review & Editing. Whitney D. Arroyave: Writing - Review & Editing. Dale P. Sandler: Writing - Review & Editing. Alexandra J. White: Conceptualization, Methodology, Formal analysis, Writing - Original Draft, Writing - Review & Editing, Project administration, Supervision.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Báez-Saldaña R, Canseco-Raymundo A, Ixcot-Mejía B, Juárez-Verdugo I, Escobar-Rojas A, Rumbo-Nava U, Castillo-González P, León-Dueñas S, Arrieta O. Case–control study about magnitude of exposure to wood smoke and risk of developing lung cancer. European Journal of Cancer Prevention. 2021. Sep 17;30(6):462–8. [DOI] [PubMed] [Google Scholar]
- Bergmann MM, Calle EE, Mervis CA, Miracle-McMahill HL, Thun MJ, Health CW. Validity of self-reported cancers in a propsective cohort study in comparison with data from state cancer registries. American journal of epidemiology. 1998. Mar 15;147(6):556–62. [DOI] [PubMed] [Google Scholar]
- Bonjour S, Adair-Rohani H, Wolf J, Bruce NG, Mehta S, Prüss-Ustün A, Lahiff M, Rehfuess EA, Mishra V, Smith KR. Solid fuel use for household cooking: country and regional estimates for 1980–2010. Environmental health perspectives. 2013. Jul;121(7):784–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colditz GA, Martin P, Stampfer MJ, Willett WC, Sampson L, Rosner B, Hennekens CH, Speizer FE. Validation of questionnaire information on risk factors and disease outcomes in a prospective cohort study of women. American journal of epidemiology. 1986. May 1;123(5):894–900. [DOI] [PubMed] [Google Scholar]
- Croft DP, Cameron SJ, Morrell CN, Lowenstein CJ, Ling F, Zareba W, Hopke PK, Utell MJ, Thurston SW, Thevenet-Morrison K, Evans KA, Chalupa D, Rich DQ. Associations between ambient wood smoke and other particulate pollutants and biomarkers of systemic inflammation, coagulation and thrombosis in cardiac patients. Environ Res. 2017. Apr;154:352–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delgado J, Martinez LM, Sánchez TT, Ramirez A, Iturria C, González-Avila G. Lung cancer pathogenesis associated with wood smoke exposure. Chest. 2005. Jul;128(1):124–31. doi: 10.1378/chest.128.1.124. [DOI] [PubMed] [Google Scholar]
- Dutton SJ, Hannigan MP and Miller SL, 2001. Indoor pollutant levels from the use of unvented natural gas fireplaces in Boulder, Colorado. Journal of the Air & Waste Management Association, 51(12), pp.1654–1661. [DOI] [PubMed] [Google Scholar]
- Fleisch AF, Rokoff LB, Garshick E, Grady ST, Chipman JW, Baker ER, Koutrakis P, Karagas MR. Residential wood stove use and indoor exposure to PM2.5 and its components in Northern New England. J Expo Sci Environ Epidemiol. 2020. Mar;30(2):350–361. doi: 10.1038/s41370-019-0151-4. Epub 2019 Jun 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Figueroa CG, Fernández-Plata R, Rivera-de la Garza MS, de los Ángeles Mora-Pizano M, Martínez-Briseño D, Franco-Marina F, Pérez-Padilla JR. Wood smoke as a risk factor for lung cancer in nonsmoking hospitalized population. NCT Neumología y Cirugía de Tó;rax. 2012;71(4):325–32. [Google Scholar]
- Hernandez-Garduno E, Brauer M, Perez-Neria J, Vedal S. Wood smoke exposure and lung adenocarcinoma in non-smoking Mexican women. The International Journal of Tuberculosis and Lung Disease. 2004. Mar 1;8(3):377–83. [PubMed] [Google Scholar]
- Hosgood HD III, Boffetta P, Greenland S, Lee YC, McLaughlin J, Seow A, Duell EJ, Andrew AS, Zaridze D, Szeszenia-Dabrowska N, Rudnai P. In-home coal and wood use and lung cancer risk: a pooled analysis of the International Lung Cancer Consortium. Environmental health perspectives. 2010. Dec;118(12):1743–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Agency for Research on Cancer. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Volume 95. Household Use of Solid Fuels and High-Temperature Frying. Lyon, IARC, 2010. [PMC free article] [PubMed] [Google Scholar]
- Ko YC, Lee CH, Chen MJ, Huang CC, Chang WY, Lin HJ, Wang HZ, Chang PY. Risk factors for primary lung cancer among non-smoking women in Taiwan. International journal of epidemiology. 1997. Feb;26(1):24–31. [DOI] [PubMed] [Google Scholar]
- Le CH, Ko YC, Cheng LS, Lin YC, Lin HJ, Huang MS, Huang JJ, Kao EL, Wang HZ. The heterogeneity in risk factors of lung cancer and the difference of histologic distribution between genders in Taiwan. Cancer Causes Control. 2001. May;12(4):289–300. [DOI] [PubMed] [Google Scholar]
- Lebel ED, Michanowicz DR, Bilsback KR, Hill LAL, Goldman JS, Domen JK, Jaeger JM, Ruiz A and Shonkoff SB, 2022. Composition, Emissions, and Air Quality Impacts of Hazardous Air Pollutants in Unburned Natural Gas from Residential Stoves in California. Environmental Science & Technology, 56(22), pp.15828–15838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lissowska J, Bardin-Mikolajczak A, Fletcher T, Zaridze D, Szeszenia-Dabrowska N, Rudnai P, Fabianova E, Cassidy A, Mates D, Holcatova I, Vitova V. Lung cancer and indoor pollution from heating and cooking with solid fuels: the IARC international multicentre case-control study in Eastern/Central Europe and the United Kingdom. American journal of epidemiology. 2005. Aug 15;162(4):326–33. [DOI] [PubMed] [Google Scholar]
- Loomis D, Grosse Y, Lauby-Secretan B, El Ghissassi F, Bouvard V, Benbrahim-Tallaa L, Guha N, Baan R, Mattock H, Straif K. The carcinogenicity of outdoor air pollution. Lancet Oncology. 2013. Dec 1;14(13):1262. [DOI] [PubMed] [Google Scholar]
- Marin A, Rector L, Morin B, Allen G. Residential wood heating: An overview of US impacts and regulations. Journal of the Air & Waste Management Association. 2022. Jul 3;72(7):619–28. [DOI] [PubMed] [Google Scholar]
- Mumford JL, Lee X, Lewtas J, Young TL, Santella RM. DNA adducts as biomarkers for assessing exposure to polycyclic aromatic hydrocarbons in tissues from Xuan Wei women with high exposure to coal combustion emissions and high lung cancer mortality. Environmental health perspectives. 1993. Mar;99:83–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musthapa MS, Lohani M, Tiwari S, Mathur N, Prasad R, Rahman Q. Cytogenetic biomonitoring of Indian women cooking with biofuels: micronucleus and chromosomal aberration tests in peripheral blood lymphocytes. Environmental and molecular mutagenesis. 2004;43(4):243–9. [DOI] [PubMed] [Google Scholar]
- Noonan CW, Ward TJ, Semmens EO. Estimating the number of vulnerable people in the United States exposed to residential wood smoke. Environ Health Perspect. 2015. Feb;123(2):A30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NTP (National Toxicology Program). 2016. Report on Carcinogens, Fourteenth Edition.; Research Triangle Park, NC: U.S. Department of Health and Human Services, Public Health Service. https://ntp.niehs.nih.gov/go/roc14. [Google Scholar]
- Öztürk Ş, Vatansever S, Çefle K, Palanduz Ş, Güler K, Erten N, Erk O, Karan MA, Taşcıoğlu C. Acute wood or coal exposure with carbon monoxide intoxication induces sister chromatid exchange. Journal of Toxicology: Clinical Toxicology. 2002. Jan 1;40(2):115–20. [DOI] [PubMed] [Google Scholar]
- Phukan RK, Saikia BJ, Borah PK, Zomawia E, Sekhon GS, Mahanta J. Role of household exposure, dietary habits and glutathione S-Transferases M1, T1 polymorphisms in susceptibility to lung cancer among women in Mizoram India. Asian Pacific Journal of Cancer Prevention. 2014;15(7):3253–60. [DOI] [PubMed] [Google Scholar]
- Pope CA III, Burnett RT, Turner MC, Cohen A, Krewski D, Jerrett M, Gapstur SM, Thun MJ. Lung cancer and cardiovascular disease mortality associated with ambient air pollution and cigarette smoke: shape of the exposure–response relationships. Environmental health perspectives. 2011. Nov;119(11):1616–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogalsky DK, Mendola P, Metts TA, Martin WJ 2nd. Estimating the number of low-income americans exposed to household air pollution from burning solid fuels. Environ Health Perspect. 2014. Aug;122(8):806–10. doi: 10.1289/ehp.1306709. Epub 2014 May 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandler DP, Hodgson ME, Deming-Halverson SL, Juras PS, D’Aloisio AA, Suarez LM, Kleeberger CA, Shore DL, DeRoo LA, Taylor JA, Weinberg CR; Sister Study Research Team. The Sister Study Cohort: Baseline Methods and Participant Characteristics. Environ Health Perspect. 2017. Dec 20;125(12):127003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobue T Association of indoor air pollution and lifestyle with lung cancer in Osaka, Japan. International journal of epidemiology. 1990;19:S62–6. [DOI] [PubMed] [Google Scholar]
- Tang L, Lim WY, Eng P, Leong SS, Lim TK, Ng AW, Tee A, Seow A. Lung cancer in Chinese women: evidence for an interaction between tobacco smoking and exposure to inhalants in the indoor environment. Environmental health perspectives. 2010. Sep;118(9):1257–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres-Duque C, Maldonado D, Pérez-Padilla R, Ezzati M, Viegi G. Biomass fuels and respiratory diseases: a review of the evidence. Proceedings of the American Thoracic Society. 2008. Jul 15;5(5):577–90. [DOI] [PubMed] [Google Scholar]
- Tsiodra I, Grivas G, Tavernaraki K, Bougiatioti A, Apostolaki M, Paraskevopoulou D, Gogou A, Parinos C, Oikonomou K, Tsagkaraki M, Zarmpas P. Annual exposure to polycyclic aromatic hydrocarbons in urban environments linked to wintertime wood-burning episodes. Atmospheric Chemistry and Physics. 2021. Dec 7;21(23):17865–83. [Google Scholar]
- U.S. Cancer Statistics Working Group. U.S. Cancer Statistics Data Visualizations Tool, based on 2021 submission data (1999-2019): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; https://www.cdc.gov/cancer/dataviz, released in November 2022. [Google Scholar]
- U.S. Census Bureau. American Community Survey (ACS). Available at: https://www.census.gov/programs-surveys/acs. Table DP04.
- U.S. Energy Information Administration. 2022. Residential Energy Consumption Survey. 2020 RECS Survey Data.Available: https://www.eia.gov/consumption/residential/data/2020/#fueluses.
- U.S. Energy Information Administration. 2022. Office of Energy Demand and Integrated Statistics, Form EIA-457A of the 2020 Residential Energy Consumption Survey. Available: https://www.eia.gov/consumption/residential/data/2020/hc/pdf/HC%201.1.pdf.
- U.S. Environmental Protection Agency. Standards of performance for new residential wood heaters, new residential hydronic heaters and forced-air furnaces. 80 FR 13671, March 16, 2015. https://www.govinfo.gov/content/pkg/FR-2015-03-16/pdf/2015-03733.pdf.
- Vermeulen R, Downward GS, Zhang J, Hu W, Portengen L, Bassig BA, Hammond SK, Wong JYY, Li J, Reiss B, He J, Tian L, Yang K, Seow WJ, Xu J, Anderson K, Ji BT, Silverman D, Chanock S, Huang Y, Rothman N, Lan Q. Constituents of Household Air Pollution and Risk of Lung Cancer among Never-Smoking Women in Xuanwei and Fuyuan, China. Environ Health Perspect. 2019. Sep;127(9):97001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward T, Lange T. The impact of wood smoke on ambient PM2. 5 in northern Rocky Mountain valley communities. Environmental Pollution. 2010. Mar 1;158(3):723–9. [DOI] [PubMed] [Google Scholar]
- Ward T, Trost B, Conner J, Flanagan J and Jayanty R (2012). Source Apportionment of PM2.5 in a Subarctic Airshed - Fairbanks, Alaska. Aerosol Air Qual. Res 12: 536–543. [Google Scholar]
- White AJ, Sandler DP. Indoor wood-burning stove and fireplace use and breast cancer in a prospective cohort study. Environmental health perspectives. 2017. Jul 18;125(7):077011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Household air pollution and health World Health Organization. Ambient (outdoor) air quality and health [online], http://www.who.int/mediacentre/factsheets/fs313/en/ (May 8, 2018).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


