Figure 1 -. Spinal cord infarction misdiagnosed as seronegative NMOSD.
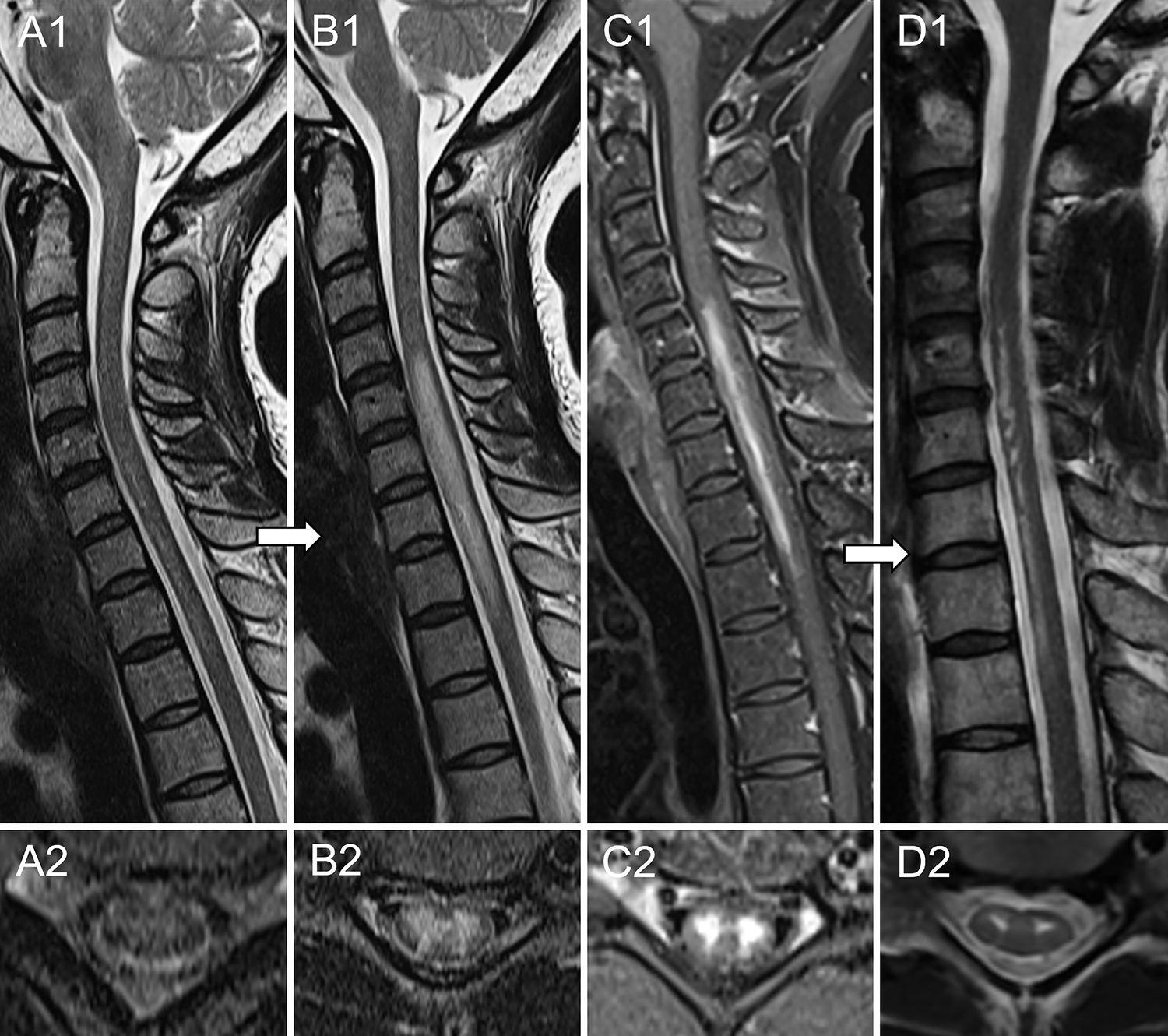
A 41-year-old African American woman with medical history of Sjögren syndrome was admitted to the emergency department for sudden onset of chest tightness. The following day she reported severe back pain and, over the course of 2–3 hours, developed acute paraplegia accompanied by numbness in lower extremities, severe weakness of upper extremities and urinary retention requiring catheterization. Spinal cord MRI obtained five hours later was unremarkable (A). CSF analysis showed 7 white blood cells and absence of oligoclonal bands; infectious and immunological evaluations were negative, except for positive anti-nuclear antibodies. Aquaporin-4-IgG and myelin oligodendrocyte glycoprotein-IgG were negative in both serum and CSF by live cell-based assay. Repeat MRI 6 days later revealed a longitudinal extensive T2-hyperintense lesion in the cervico-thoracic spinal cord (B) with associated enhancement on post-gadolinium T1-weighted sequences (C). A working diagnosis of seronegative NMOSD was made and she was treated with intravenous immune-globulins, slow taper prednisone and rituximab induction with only mild improvement of symptoms. The patient underwent a repeat MRI 2.5 months later, which showed persistence of the T2-hyperintense lesion restricted to the ventral spinal cord, with a “snake eyes” appearance on axial images (D). The patient was later referred to the Mayo Clinic (Rochester, Minnesota) where a final diagnosis of spinal cord infarction was made and rituximab was discontinued. Despite investigations no cause for the spinal cord infarct was found.
