Figure 2 -. Optic nerve sheath meningioma misdiagnosed as seronegative NMOSD.
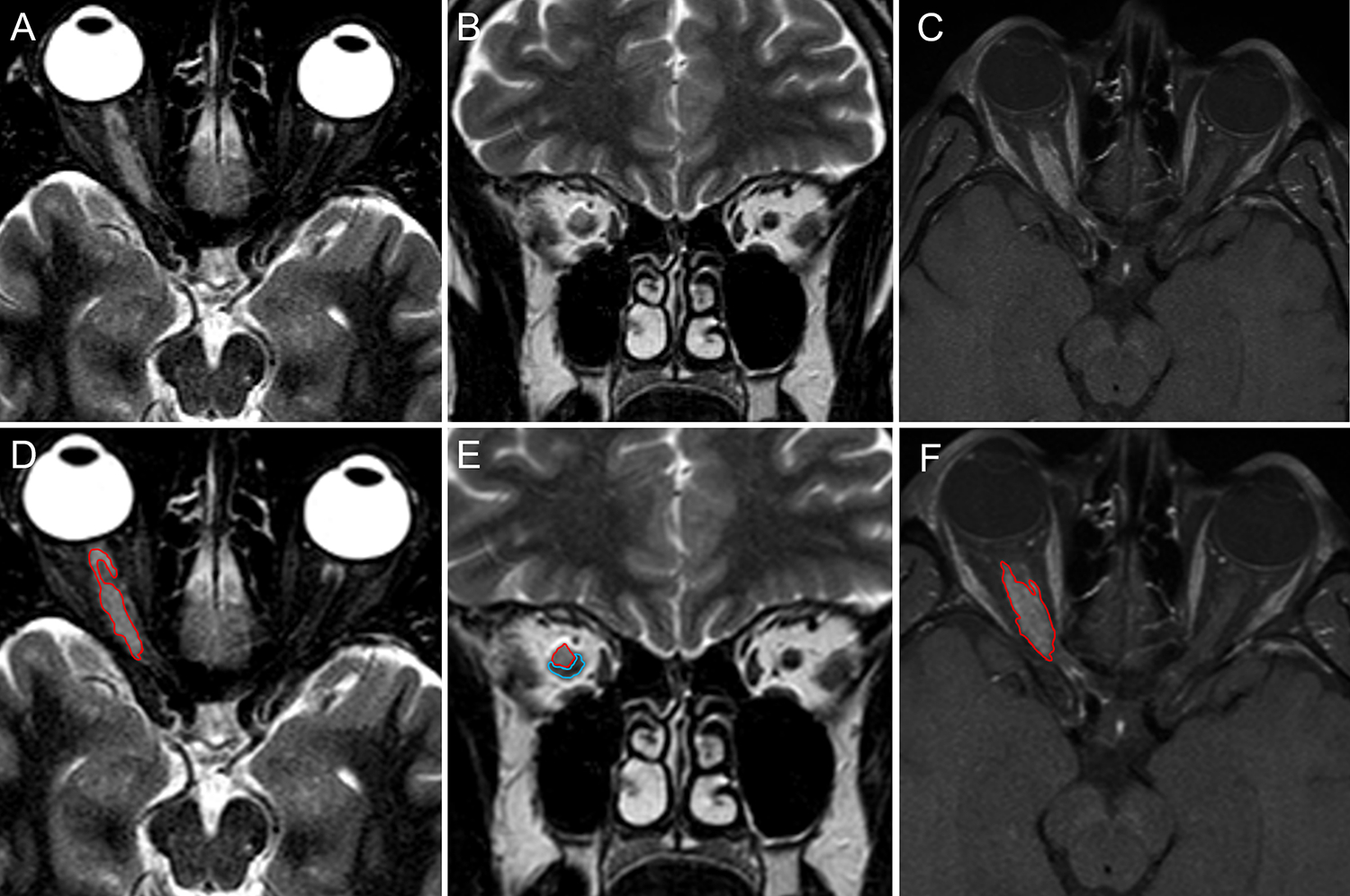
A 52-years old Caucasian woman developed blurred vision in the right eye over one week. She denied headache, diplopia, or other neurologic symptoms. Brain MRI showed marked swelling of the right optic nerve with associated gadolinium enhancement (not shown). A diagnosis of optic neuritis was made and she was treated with intravenous methylprednisolone (1 g daily for 5 days), with resolution of the visual symptoms. In the following two years, she experienced several recurrences of symptoms in the same eye interpreted as recurrent optic neuritis and treated with intravenous methylprednisolone pulses and oral prednisone taper. Repeat MRIs over the two years showed persistent enhancement of the right optic nerve, substantially unmodified compared to the first exam. Despite some temporary improvement with corticosteroid therapy, she experienced progressive vision impairment. NMOSD was eventually suspected and the patient was referred to the Neurology Unit of the University-Hospital of Sassari. Orbital MRI showed a discrete tissue mass surrounding the right optic nerve that was hyperintense on both axial (A) and coronal (B) T2-images and enhanced diffusely after gadolinium administration on fat-suppression sequences (C). The margins of the mass and adjacent optic nerve are highlighted in red and blue, respectively (D-F). A final diagnosis of probable optic nerve sheath meningioma was made based on clinical and MRI findings.
