Figure 4 -. Suggested diagnostic work-up in patients with suspected NMOSD.
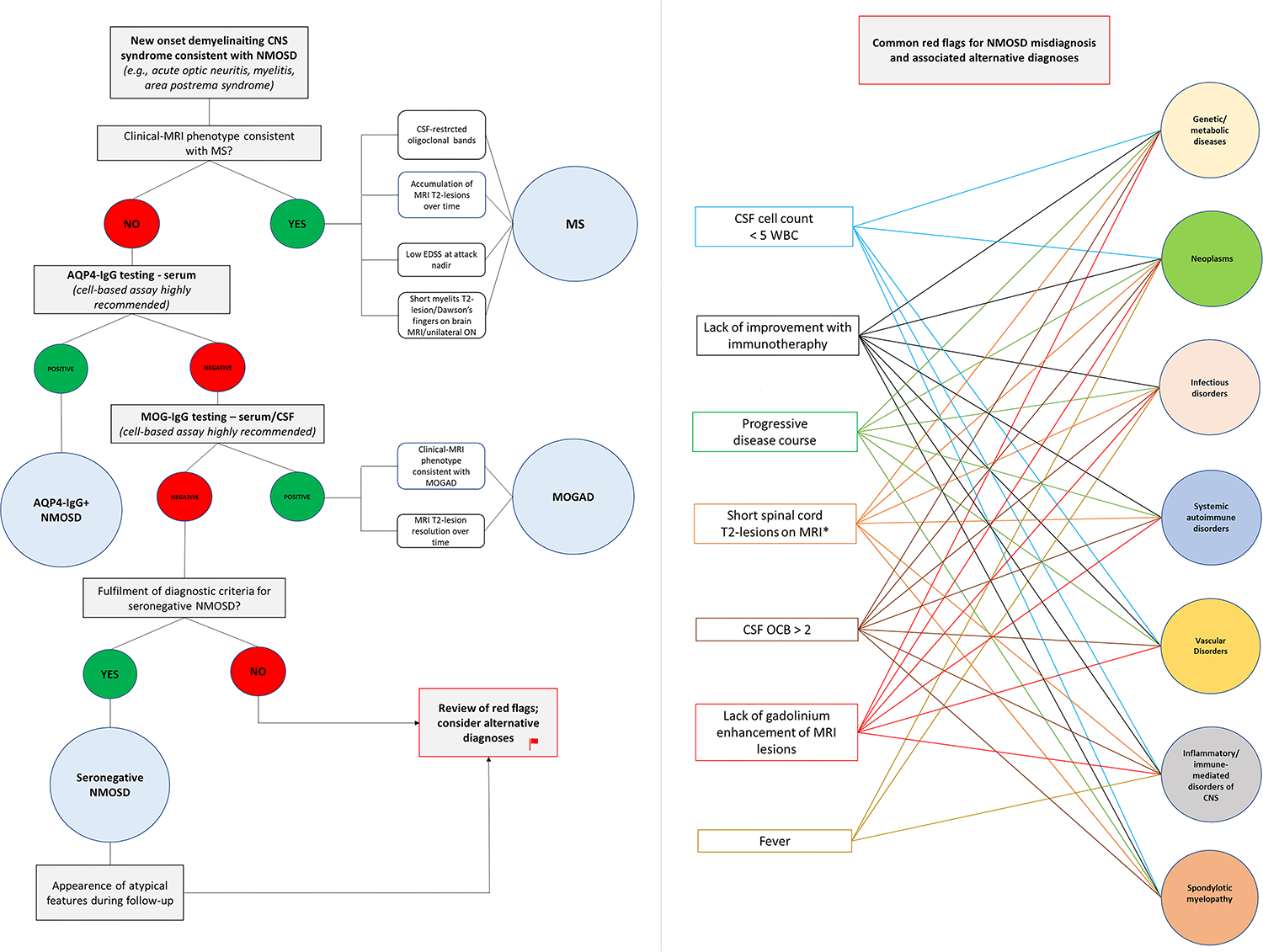
The left half of the figure shows the recommended diagnostic work-up in patients with new-onset demyelinating CNS syndromes compatible with NMOSD (e.g., optic neuritis, myelitis). Multiple sclerosis is the most common demyelinating CNS disorder and should be the first to considered in case of suggestive features (e.g., short myelitis lesions on MRI, CSF-restricted oligoclonal bands). If the clinical-MRI phenotype is not consistent with MS, testing for aquaporin-4-IgG and myelin oligodendrocyte glycoprotein-IgG by cell-based assay is recommended. In case autoantibody testing gives a negative result and a diagnosis of seronegative NMOSD is considered, a careful evaluation for common red-flags is important to avoid misdiagnosis. The right half of the figure shows the most common red-flags encountered in patients with NMOSD misdiagnosis and associated alternative etiologies reported in the literature. Once common red-flags have been excluded, a reasonable diagnosis of seronegative NMOSD can be made. In these patients, however, the lack of response to immunotherapy is another red flag that should prompt reconsideration of alternative diagnoses.
