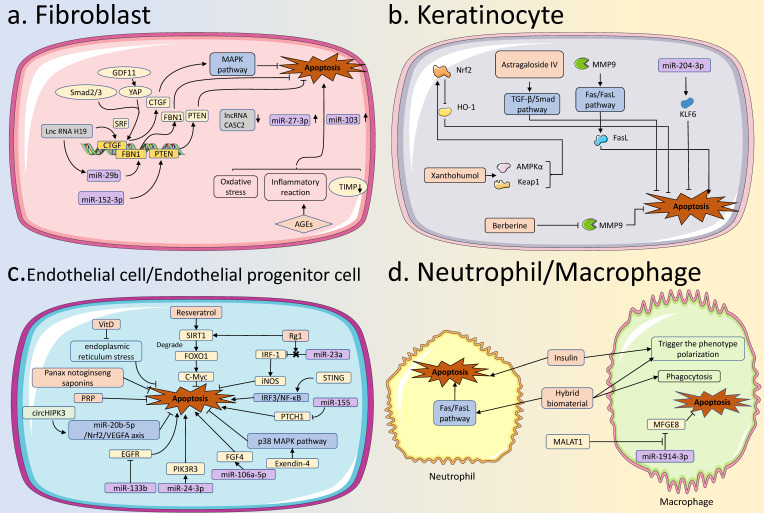
Figure 3.
Apoptosis in various skin cells in diabetic wound healing. (A) Apoptosis in fibroblasts: GDF11, miR-29b, miR-152-3p, and lncRNA H19 are involved in apoptotic regulation of fibroblasts in diabetic wound healing by regulating the expression of targeted genes. MiR-103, miR-27-3p, and lncRNA CASC2 are also aberrantly expressed in fibroblasts. AGEs can regulate apoptosis by increasing intracellular levels of oxidative stress, and inflammatory reaction, and decreasing levels of TIMP. (B) Apoptosis in KCs: Various drugs, such as Astragaloside IV, Xanthohumol, and Berberine, can inhibit the apoptosis of keratinocytes in diabetic wounds. Some specific miRNAs, such as miR-204-3p, can inhibit the apoptosis of KCs to promote the healing of diabetic wounds. (C) Apoptosis in ECs: Some factors, represented by Resveratrol, VitD, STING, miR-133b, miR-106a-5p, miR-155, and circHIPK3, can modify the healing process of diabetic wounds by regulating apoptosis of ECs. (D) Apoptosis in neutrophils and macrophages: Normal apoptosis of immune cells is essential for the normal healing of diabetic wounds. In diabetic wounds, insulin promotes the apoptosis of neutrophils and also affects the phenotypic transformation of macrophages. The hybrid biomaterial can facilitate apoptosis of neutrophils and also influence phagocytosis and phenotypic transformation of macrophages. The exosomal MALAT1 can enhance diabetic wound healing by inhibiting macrophage apoptosis. AGEs, Advanced Glycation End products; TIMP, Tissue Inhibitor of Metalloproteinase; KCs, keratinocytes; Ecs, Endothelial Cells.