Table 2.
ARM: Barriers for Its Use and Proposed Solutions and Graphic Representations
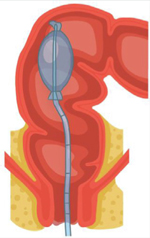
| Barriers | Solution | Graphic Figure |
|---|---|---|
| Education and Training: • Lack of understanding of the indications and clinical utility of ARM • Uncertainty regarding how to perform the procedure |
• Collective efforts from societies, foundations, industry, and practicing physicians to develop workshops and training modules (including hands-on training). • Incorporate ARM education in gastroenterology fellowship training; especially on how to perform and interpret ARM (both anatomical and technical aspects). • ARM should be discussed as a screening tool for other pelvic floor disorders (rectal intussusception, descending perineum syndrome, anorectal pain, and dysfunctional urinary symptoms with overlapping defecatory disorders), in addition to fecal incontinence and constipation. • Utilize the ANMS Clinical Training Program for gastroenterology fellows to obtain first-hand knowledge of these techniques and develop careers in neurogastroenterology/motility. • Support research in improving ARM diagnostic techniques and expanded indications, and development of newer tools. |

|
| Methods: evidence-based protocols/deviations are neededa | The IAPWG protocol could be improved upon by considering the following: • Provide guidance on addition of provocative testing to complement the findings depending on symptom profiles of constipation vs fecal incontinence. • Provide technique-specific and equipment-specific normal values where available, minor variations in the SOP are acceptable. The specific SOP is dictated by the equipment. • Implement seated HR-ARM if feasible for the assessment of defecation disorders. • Improve measurements for puborectalis pressure and coordination during simulated defecation. • Improve which cutoffs to use, as there are many sources with varying degrees of age-matched, sex-matched, etc. normative data. • Use of “push” with a standard rectal balloon volume as a better way to detect dyssynergia. For evacuation disorder, consider defecography to confirm or refute ARM findings suggesting dyssynergia. • Provide further protocol iterations that include normative parameters for quantifying disorders of rectoanal coordination, squeeze, rectal compliance, and sensory thresholds, including defecation index, rectoanal gradient, and integrated pressurized volume. |
|
| Interpretation: guidelines are lackinga | • Need additional normal values: • For subpopulations defined by age, sex, parity, BMI, and ethnicity • For all ARM systems (technique-specific values; HR- ARM vs HD-ARM) • Day-to-day reproducibility • Standardize description of findings and provide more conclusive interpretations. • Improve the definition for poor propulsion. • Determine which elements of the protocol predict interventional success (ie, likelihood of BT response based on abnormalities as defined by the London Classification). • Determine treatment recommendations based on 4 categorizations of dyssynergic defecation. • Provide evidence-based rationale for major and minor disorder classifications. • Define abnormalities identified via ARM that may warrant additional assessment. • Consensus guidelines are needed on how to define sensory abnormalities (rectal hyposensitivity, rectal hypersensitivity), and sensory biofeedback therapy. • Interpretation of ARM using the IAPWG protocol and its flow is cumbersome and less user-friendly and could be improved, including terminology. |
|
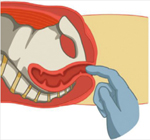
| Miscellaneous | • Teach proper rectal exam skills using video modules, demonstrations, instruction, and guidance on how to find prolapse and rectoceles, including positioning of patient. • Emphasize the utility of balloon expulsion testing. •Equipment manufacturers should provide standard protocols with flexible options to address specific patient needs. • Improve hands on practical training using small group workshops, seminars, and live demonstrations. • Impact of ARM on diagnosis and treatment outcomes are needed. |

|
ANMS, American Neurogastroenterology and Motility Society; ARM, anorectal manometry; BMI, body mass index; BT, biofeedback therapy; EMG, electromyography; HCP, healthcare provider; HD-ARM, high-definition anorectal manometry; HR-ARM, high-resolution anorectal manometry; IAPWG, International Anorectal Physiology Working Group; SOP, standard operating procedure.
Prior to the roundtable meeting, key opinion leaders in the gastroenterology field completed a brief survey. The survey question asked, “In the ideal London Classification, what would you improve? Please prioritize.”
