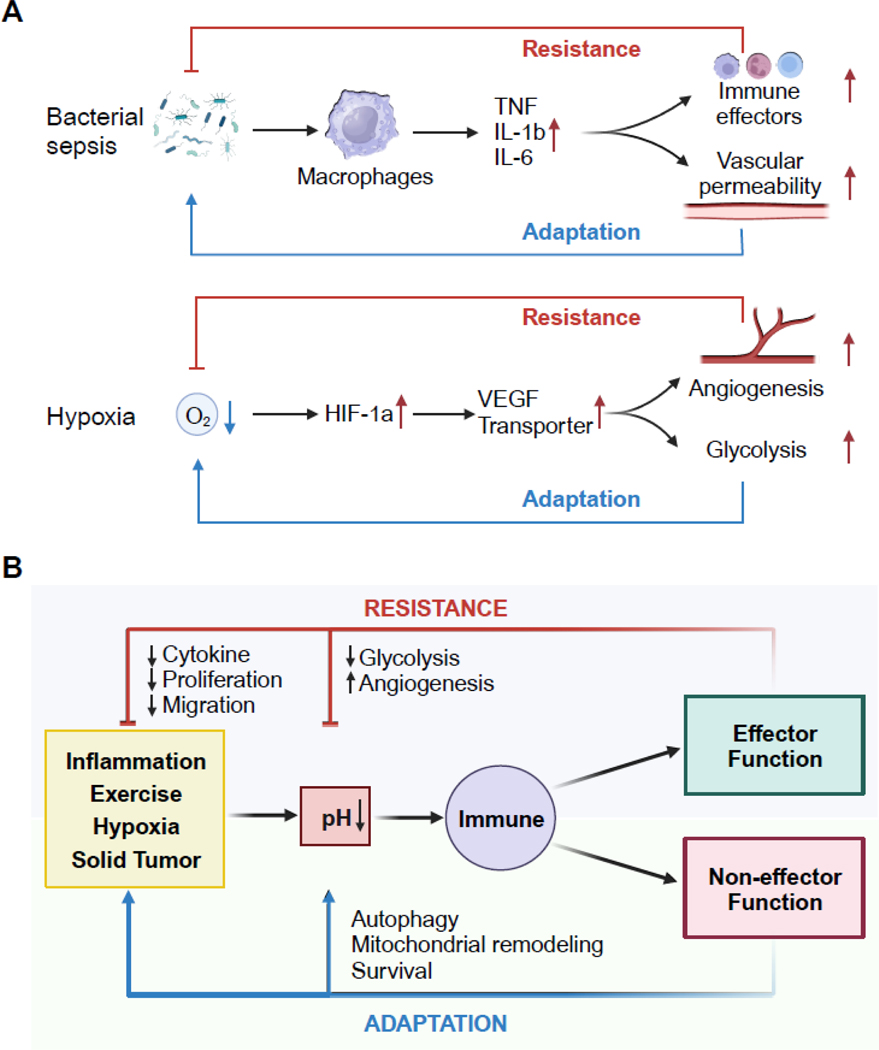
Key Figure, Figure 6. Model of resistance and adaptation responses to pH perturbations.
(A) In response to an infection, sensor cells (e.g., macrophages, dendritic cells) secrete inflammatory mediators (e.g., TNF, IL-1β and IL-6) leading to the recruitment of effector cells (e.g., neutrophils, monocytes) that directly eliminate the pathogen as the resistance arm. The pro-inflammatory cytokines can also modulate other tissue targets (e.g., endothelial cells) to enable the inflammatory state as the adaptation arm of the response. In a second example, low oxygen tension is sensed by transcription factor HIF-1a, which induces angiogenic factors and activates glycolytic metabolism. New blood vessels deliver oxygen to relieve hypoxia (resistance) and anerobic glycolysis supplies energy (adaptation).
(B) pH alterations from physiological and inflammatory perturbation can be sensed to regulate effector and non-effector functions in immune cells. The effector responses resist reduction in pH, by either directly regulating pH or the initial trigger that causes pH deviation. In contrast, pH responses can carry non-effector functions that are permissive for cells to adapt to a new pH environment. (see main text for references).