Abstract
Introduction
The specific aim of this retrospective study was to determine whether bone quality has any effect on the complication rates or overall survivorship between helical blades and lag screws in cephalomedullary nails used for intertrochanteric hip fractures.
Methods
The authors reviewed clinical charts and radiographic studies of patients between January 2012 and August 2019. We reviewed radiographic images (pre-, intra-, and post-operative) to evaluate fracture fixation type, fracture reduction grade, and post-operative complications. We collected dual energy x-ray absorptiometry scan results (T-score) and serum alkaline phosphatase (ALP) isoenzyme activity values to evaluate patient bone quality.
Results
We included 303 cases (helical: 197, screw: 106) in the study. Complications were found in 31 (16%) helical blade cases and 23 (22%) lag screw cases. No statistically significant difference was detected when comparing complication rates with patient bone quality between the two groups. These two groups had similar one-year implant survivorship with respect to T-score, the low ALP level group, and normal ALP level group. The helical blade had higher implant survivorship compared to lag screw in five-year survival rate with respect to osteoporotic group, high ALP level group, and normal ALP level group (osteoporotic: 77% vs 69%, high ALP: 73% vs 67%, normal ALP: 70% vs 64%).
Conclusions
Similar complication rates were observed between helical blade and lag screw constructs in cephalomedullary femoral nails when accounting for patient bone quality. However, the helical blade design had a higher five-year survival rate.
Keywords: hip fractures, intertrochanteric fractures, intramedullary nailing, helical blade screw, lag screw
INTRODUCTION
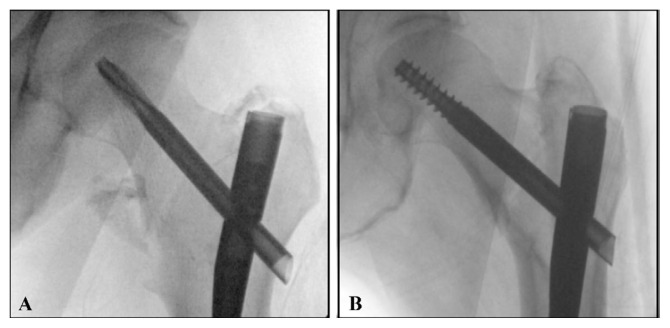
Intertrochanteric hip fractures are one of the most common injuries among the older adult population. They carry significant morbidity and mortality and have a large impact on quality of life.1–4 The number of hip fractures treated each year is expected to continue to increase significantly,5,6 and also is expected to substantially increase health care expenses.4,6 Cephalomedullary nails have become the device of choice for fixation of unstable intertrochanteric hip fractures,7–10 as these implants allow a fixed-angle construct, controlled fracture compression, and adequate stability for immediate post-operative weight bearing.8,11 The cephalic screws are designed to be able to slide within the nail for compression while maintaining load-sharing characteristics at the fracture site. Currently, there are two main designs of cephalic screw implants available: helical blade (Figure 1A) and lag screw (Figure 1B). There are conflicting data in the literature when comparing these two cephalic screw designs.12–17 Several studies have found no difference in the failure rate of trochanteric fractures treated with blade versus screw for femoral fixation.12,16 Other studies have found that when the helical blade was used, implant cutout or implant migration occurred at a significantly higher rate compared with lag screw fixation.13–15,17 Because of these conflicting data in the literature, many orthopedic surgeons select one screw design over the other for their patients based on their comfort level or personal experience. This illustrates the need for a better understanding of the advantages or disadvantages in the use of these two screw designs for intertrochanteric hip fractures as orthopedists aim to optimize patient outcomes.
Figure 1.
Cephalomedullary nails for unstable intertrochanteric hip fractures: (A) helical blade design, (B) sliding lag screw design.
As many intertrochanteric fractures are related to poor bone quality, it is important to consider the effect that bone quality may have on implant stability.18,19 It is well known that accurate positioning of the cephalic screw in the femoral head affects the outcome following fixation of intertrochanteric hip fractures;12,14,20,21 however, the role of bone mineral density (BMD) or alkaline phosphatase (ALP) levels has not been thoroughly evaluated. There are limited clinical studies in the literature that specifically examine the effect of BMD or ALP levels on the lag screw versus helical blade design for intertrochanteric hip fracture fixation. Most of the clinical studies to date have investigated the direct comparison between the blade and screw designs without considering the effect of bone quality.10,13,14,16,21–23 To date, the majority of the literature pertaining to the effect of bone quality has been biomechanical or finite element modeling in nature.15, 17, 24–27 Thus, the specific aim of this retrospective study was to determine whether bone quality has any effect on the complication rates or overall survivorship between helical blades and lag screws in cephalomedullary nails used for intertrochanteric hip fractures.
METHODS
Participants
Approval for this study was obtained from our institute research committee and the institutional review board. The authors reviewed the clinical charts and radiographic studies of a consecutive series of patients (18 years and older) who had intertrochanteric fractures treated with a cephalomedulary nail. The inclusion criteria consisted of intertrochanteric hip fracture fixation procedures performed from January 2012 through August 2019 from designated Level-1 trauma centers within a single institution in the Midwestern Region of the United States. Patients with prior hip surgery, hip fractures other than intertrochanteric, hip fracture fixation not utilizing cephalomedulary nail, inadequate length of follow-up, or inadequate radiographs, including unavailable pre- or post-operative films, were excluded from the study. Patients with post-operative clinical and radiographic follow-up of less than three months were excluded from the study; however, patients with complication or failure within three months were included in the study. A minimum follow-up period of three months was similar to those described in the literature.13,21,22,28,29 The surgical cases examined in this study included two commonly used cephalomedullary nails: the Stryker gamma nail (Gamma; Mahwah, NJ) and the Synthes trochanteric fixation nail (TFN; Paoli, PA). The cephalic screw fixation of these implants was performed with either a lag screw or a helical blade. The type of nail, as well as the decision to use a lag screw or helical blade, was made according to surgeon preference.
Variables
The retrospective chart review included information regarding patient age, gender, body mass index (BMI), surgical date, laterality of procedure, initial follow-up date, and latest follow-up date. The intra-operative or initial post-operative plain radiographic images of the hip, pelvis, or femur were utilized to determine the fixation type (lag screw or helical blade), hardware placement, and initial fracture reduction quality. A fracture reduction grade was scored for each case based on a modification of the criteria proposed by Baumgaertner, et al.21 with Tip Apex Distance (TAD) measurement. The TAD measurements on the plain radiographic images were calibrated with the magnification error of the actual stem width. Fractures were graded as “good”, “acceptable”, or “poor” based on three radiographic criteria as judged on the radiographic images. These were (1) alignment on the anteroposterior (AP) film for anatomic or valgus alignment, (2) neutral alignment on the lateral film, and (3) absence of displacement > 4 mm on either view apart from a displaced lesser trochanter fragment. For a reduction to be considered “good”, all three criteria were met. For an “acceptable” reduction, either alignment or displacement criteria were met, but not both. For a “poor” reduction, none of the three criteria were met.21
Bone quality or markers of bone mass assessment was performed using the dual energy x-ray absorptiometry (DEXA) scan results, and serum alkaline phosphatase (ALP) isoenzyme activity. The result of the DEXA scan is presented as a T-score, which represented the difference of the bone density from the average bone density of healthy young adults. The World Health Organization (WHO) operationally defines a T-score greater than -1.0 as normal, a T-score between -1.0 and -2.5 indicated low bone mass (osteopenia), and a T-score of -2.5 or less indicated osteoporotic.30 The result of the ALP isoenzyme activity is presented as low, normal, and high levels. The normal range for the ALP blood test was defined as 44–147 international units per liter (IU/L),31,32 low ALP level was defined as < 44 IU/L, and high ALP level as > 147 IU/L. High bone ALP levels may indicated have a type of bone disorder.33,34
Post-operative data collected included complication variables such as implant cut-out, implant migration without cut-out, femoral neck collapse, periprosthetic fracture, hardware failure or breakage, infection, and persistent hip pain. Survivorship in this study is defined as lack of complications or reoperation.
Statistical Analysis
Descriptive statistics were used to create demographic profile of the patients whose data were used in the study. Independent-samples student-t test with not assumed equal variances was used to evaluate for differences between groups by comparing population means and standard deviation of variables. For categorical variables, a one-sided Fisher’s exact test analysis was used to determine statistical significance. The Pearson chi-square statistic was utilized to determine significant observed differences among bone quality (T-score and ALP) and post-operative comparisons related to bone quality. Frequencies and percentages for other variables were obtained. Kaplan-Meier survival analysis was performed to determine all-cause implant survivorship at final follow-up for every patient. This study assumed that (1) at any time the patients who were censored should have the same survival prospects as those who were still being followed in the study, (2) the survival probabilities were the same for patients recruited early and late in the study, and (3) the event happened at the time specified. Participants who have died are considered censored. All statistical testing methods used were performed using IBM SPSS Statistics software (Version 24.0; IBM Corporation, Armonk, New York), and statistically significant relationships were defined as those with p value of less than 0.05.
RESULTS
There were 303 intertrochanteric hip fracture cases (247 female, 56 male) identified, with 197 cases (159 female, 38 male) treated with helical blade and 106 cases (88 female, 18 male) treated with lag screw. The mean age was 77 years (SD = 9 years, range: 43 – 90 years) and the mean BMI was 26.1 kg/m2 (SD = 6.5 kg/m2, range: 15.0 – 54.6 kg/ m2). The mean follow-up period was 692 days (SD = 631 days, range: 19 – 2,993 days), and 52% (n = 157) were left hip injuries. There were no statistically significant differences in demographics between these two study groups (gender: p = 0.371; age: p = 0.858; BMI: p = 0.159; followup period: p = 0.480; site of procedure: p = 0.205).
Based on the DEXA scan results, most of the patients had either osteopenia (helical blade: 79 out of 197 patients [40%]; lag screw: 57 out of 106 patients [54%]) or osteoporosis (helical blade: 100 out of 197 patients [51%]; lag screw: 44 out of 106 patients [42%]) for both groups. However, there were higher numbers of osteoporosis patients (51%) in the helical blade fixation group, with higher numbers of osteopenia patients (54%) in the lag screw fixation group. There was no statistically significant difference detected between these two groups (p = 0.053). Both groups had higher proportions of patients with normal ALP levels (helical blade: 71%; lag screw: 71%), and there was no statistically significant difference detected between these two groups (p = 0.252).
There were 31 out of 197 helical blade fixation cases (16%) and 23 out of 106 lag screw fixation cases (22%) that developed complications (Table 1). A lower rate of implant cut-out and persistent hip pain was observed in the helical blade group when compared to the lag screw group (cut-out: 4% vs 8%; pain: 3% vs 6%). Overall, there was no statistically significant difference detected between these two groups (p = 0.128). When comparing post-operative complication rates with respect to patient bone quality (T-score and ALP levels), there were no statistically significant differences detected between these two groups (Table 2).
Table 1.
Complications for each group.
| Complications | Helical blade (n = 31) | Lag screw (n = 23) |
|---|---|---|
| Implant cut-out | 8(4%) | 8(8%) |
| Device migration without cutout | 2(1%) | 1(1%) |
| Femoral neck collapse | 3(2%) | 1(1%) |
| Periprosthetic fracture | 7(4%) | 5(5%) |
| Hardware failure (bent) | 3(2%) | 2(2%) |
| Infection | 2(1%) | - |
| Persistent hip pain | 6(3%) | 6(6%) |
Table 2.
Post-operative complications evaluation results.
| Variable | Helical blade (n = 31) | Lag screw (n = 23) | p value | |
|---|---|---|---|---|
| Complication with T-Score | Osteopenia (−1 to −2.5) | 14 (18%) | 13 (23%) | 0.301 |
| Normal (>−1) | 4 (18%) | 2 (40%) | 0.392 | |
| Osteoporosis (<−2.5) | 13 (13%) | 8 (18%) | 0.284 | |
| Complication with ALP levels | Low (< 44 IU/L) | - | 1 (33%) | 0.600 |
| Normal (44 – 147 IU/L) | 24 (17%) | 19 (25%) | 0.106 | |
| High (> 147 IU/L) | 6 (18%) | 1 (8%) | 0.402 | |
| No data | 1 (5%) | 2 (13%) | 0.396 | |
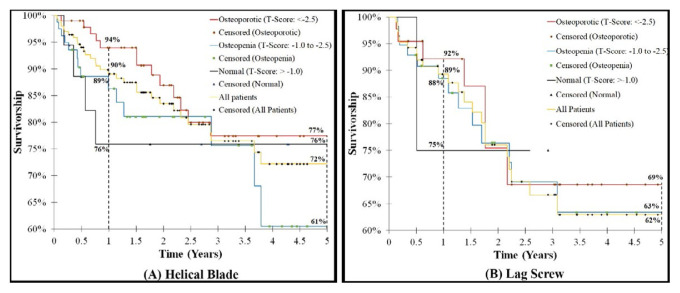
When comparing implant survivorship with respect to T-score, the one-year survival rate for all four groups (osteoporotic, osteopenia, normal bone density, and all patients) between the helical blade design and lag screw design were similar (osteoporotic: 94% vs 92%, osteopenia: 89% vs 88%, normal: 76% vs 75%, and all patients: 90% vs 89%; Figure 2A vs Figure 2B). The five-year survival rate calculated by the Kaplan-Meier survival analysis for the osteoporosis group and all patients group in the helical blade design had higher survival rates compared to the lag screw design (osteoporotic: 77% vs 69%, all patients: 72% vs 62%); the survival rates were similar for the osteopenia group and normal bone density group between the two cephalic screw designs (osteopenia: 61% vs 63%, normal: 72% vs 75%; Figure 2A vs Figure 2B).
Figure 2.
Survival analysis of unstable intertrochanteric hip fractures utilizing cephalomedullary nails related to T-score: (A) helical blade, (B) sliding lag screw design.
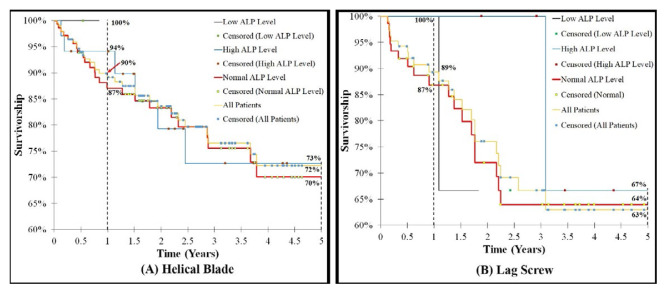
When comparing implant survivorship with respect to ALP levels, this study showed that the implant survivorship rate at mean follow-up of one year for the low ALP level group, normal ALP level group, and all patients group were similar between the helical blade design and lag screw design (low ALP level: 100% vs 100%, normal: 87% vs 87%, and all patients: 90% vs 89%). The high ALP level group had different survivorship rates between these two designs at mean follow-up of one year (94% [helical blade, Figure 3A] vs 100% [lag screw, Figure 3B]). The five-year survival rate for high ALP level group, normal ALP level group, and all patients group in the helical blade design had higher survival rates compared to the lag screw design (high ALP level: 73% [helical blade, Figure 3A] vs 67% [lag screw, Figure 3B], normal ALP level: 70% [helical blade, Figure 3A] vs 64% [lag screw, Figure 3B], and all patients: 72% [helical blade, Figure 3A] vs 63% [lag screw, Figure 3B]).
Figure 3.
Survival analysis of unstable intertrochanteric hip fractures utilizing cephalomedullary nails related to ALP levels: (A) helical blade, (B) sliding lag screw.
When examining fracture reduction quality, most cases (n = 126) for the helical blade fixation group had good reduction quality, and 17 of those cases (13%) developed complications. Fifty-five out of 197 cases had acceptable reduction quality, and 11 of those cases (20%) developed complications. Sixteen out of 197 cases had poor reduction quality, and 3 (19%) of those cases developed complications (Table 3). In the lag screw fixation group, most cases (n = 68) had good reduction quality, and 10 (15%) of those cases developed complications. Ten out of 106 cases had poor reduction quality, and 4 (40%) of those cases developed complications (Table 4). Twenty-eight out of the 106 cases had acceptable fracture reduction, and 9 (32%) of those cases developed complications.
Table 3.
Bone quality, fracture reduction quality, and complications data in the helical blade design group.
| T-score | ALP | All patients | Fracture reduction | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Poor | Acceptable | Good | |||||||
| Cases (n=197) | Cx (n=31) | Cases (n=16) | Cx (n=3) | Cases (n=55) | Cx (n=11) | Cases (n=126) | Cx (n=17) | ||
| Normal (>−1.0) | Low* | - | - | - | - | - | - | 3 | - |
| Normalβ | 13 | 4 | - | - | 8 | 3 | 5 | 1 | |
| Highδ | 2 | - | - | - | 1 | - | 1 | - | |
| No data | 3 | - | - | - | - | - | 3 | - | |
| Osteopenia (−1.0 to −2.5) | Low* | - | - | - | - | - | - | - | - |
| Normalβ | 60 | 11 | 7 | 1 | 13 | 3 | 40 | 7 | |
| Highδ | 9 | 2 | 2 | 1 | 2 | 1 | 5 | - | |
| No data | 10 | 1 | 1 | - | 3 | 1 | 6 | - | |
| Osteoporosis (<−2.5) | Low* | 2 | - | - | - | 2 | - | - | - |
| Normalβ | 67 | 9 | 4 | - | 18 | 2 | 45 | 7 | |
| Highδ | 23 | 4 | 1 | 1 | 7 | 1 | 15 | 2 | |
| No data | 8 | - | 1 | - | 1 | - | 6 | - | |
Note: Cx, Complications; *, ALP Level < 44 IU/L; β, ALP Level 44 – 147 IU/L; δ, ALP Level > 147 IU/L.
Table 4.
Bone quality, fracture reduction quality, and complications data in the lag screw design group.
| T-score | ALP | All patients | Fracture reduction | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Poor | Acceptable | Good | |||||||
| Cases (n=106) | Cx (n=23) | Cases (n=10) | Cx (n=4) | Cases (n=28) | Cx (n=9) | Cases (n=68) | Cx (n=10) | ||
| Normal (>−1.0) | Low* | - | - | - | - | - | - | - | - |
| Normalβ | 3 | 1 | 1 | - | 1 | 1 | 1 | - | |
| Highδ | 1 | - | 1 | - | - | - | - | - | |
| No data | 1 | 1 | 1 | 1 | - | - | - | - | |
| Osteopenia (−1.0 to −2.5) | Low* | 2 | 1 | 1 | 1 | - | - | 1 | - |
| Normalβ | 42 | 10 | 1 | - | 11 | 4 | 30 | 6 | |
| Highδ | 5 | 1 | 1 | - | - | - | 4 | 1 | |
| No data | 8 | 1 | 2 | 1 | 1 | - | 5 | - | |
| Osteoporosis | Low* | 1 | - | - | - | - | - | 1 | - |
| Normalβ | 30 | 8 | 1 | 1 | 12 | 4 | 17 | 3 | |
| Highδ | 6 | - | 1 | - | 3 | - | 2 | - | |
| No data | 7 | - | - | - | - | - | 7 | - | |
Note: Cx, Complications; *, ALP Level < 44 IU/L; β, ALP Level 44 – 147 IU/L; δ, ALP Level > 147 IU/L.
DISCUSSION
The primary aim of the present retrospective study was to examine the influence of bone quality on the complication rates and overall survivorship of intertrochanteric hip fractures treated with cephalomedullary nails using helical blades or lag screws for cephalic fixation. This study found a slightly lower complication rate in the helical blade group when compared to the lag screw group (16% vs 22%). Our data showed that lag screws and helical blades had equivalent performance with respect to T-score or ALP levels at one-year survivorship. However, five-year survival rates calculated with respect to T-score or ALP levels showed the helical blade design had a higher survival rate compared to the lag screw design.
Helical blades have been advertised as having theoretic advantages over lag screw fixation in the femoral neck component of cephalomedullary nails. They are designed to minimize bone loss during insertion and have greater rotational stability compared to lag screw fixation.23 They also are theorized to have higher cutout resistance. However, the literature has been mixed regarding the veracity of these theories. A retrospective review by Chapman et al.22 found a higher rate of failure when helical blades were compared to screws. They noted that helical blade failures tended to include more medial migration of the blade as opposed to the traditional superior implant cut out. However, a prospective randomized controlled study by Stern et al.16 did not observe a significant difference in complication or cutout rates between helical blades and screws. We suspect that the discrepancy between these studies is caused by the different lengths of follow up. Chapman et al.22 study had an average of 112 follow-up days (range: 94 – 125 days), whereas Stern et al.16 study had a one-year follow-up. Prior studies have reported the follow-up period between 0.7 months and 74 months.12–16,22 We did not observe an overall difference in complication rates between the two groups, and both helical blade and lag screw performed equally well at one-year follow-up; however, this study did note a greater five-year survivorship with helical blade design, especially for patients with osteoporosis. This suggests that helical blade implants may have a long-term advantage for patients with poor bone density. The results of this study suggest that most patients with normal T-score (> -1.0) can successfully be managed with either screw design, but those patients with true osteoporosis as diagnosed by DEXA scan may benefit from use of a helical blade design due to better implant survival in longer-term follow-up periods.
The use of the helical blades not only showed improved five-year survivorship compared to lag screws, but it also should be noted that when examining the subgroup of fractures with a “poor” reduction quality rating, helical blades demonstrated a lower complication rate than lag screws. When looking only at fractures with poor fracture reduction, we noted a 19% (3 out of 16 patients) complication rate in the helical blade group (Table 3) compared to a 40% (4 out of 10 patients) complication rate in the lag screw group (Table 4). Poorly reduced fractures were the minority in both groups; therefore, these numbers are not sufficient to reach statistical significance. However, this trend may suggest that the integrity of the lag screw fixation is more dependent on fracture reduction quality than the helical blade.
Femoral head bone quality is critically important for the integrity of the head screw component of cephalomedullary nails. The lag screw benefits from high-density bone in the femoral head to provide a sufficient gripping force.35–37 On the contrary, the helical blade is designed to have increased purchase in the femoral head of patients with poor bone density. Unfortunately, there is no perfect method for assessment of bone quality of the femoral head. BMD of the hip is not constant and declines in the elderly population by approximately 0.5% per year.38 In patients with a hip fracture, the hip BMD declines one year after the fracture ranges from 2% to 7%.39,40 Karlsson et al.39 investigated changes of BMD in 47 femoral neck fractures, and they concluded that osteoporotic hip fracture cases lose bone mass at an increased rate in the fractured hip relative to the uninjured hip. There was a BMD difference of 20–29% after 4 months and 1–6% after 12 months. Furthermore, BMD values vary among diabetic patients and can be increased, decreased, or remain normal.41
In patients with osteoporosis, the bone metabolism system is disordered, and the levels of bone metabolism markers such as ALP are abnormal. Biochemical markers of bone metabolism are affected by fractures, and total alkaline phosphatase (ALP) is considered one of the bone formation markers and has generally been considered a reliable indicator for evaluating bone structure and performance.42 ALP exists on the cell membrane surface of osteoblasts,43,44 which can inactivate the mineralization inhibitors pyrophosphate and osteopontin,45 thus playing an important role in osteoid formation and mineralization.
Limitations
This study has certain limitations to recognize. First, a small sample size made it difficult to reach statistical significance on many variables. The low number of procedures included was unfortunately unavoidable due to a high rate of loss of follow-up secondary to patient mortality. Second, this study was a retrospective chart review study which introduces the possibility of selection and/or observation bias, as it was neither randomized nor blinded. Third, the patients who received cephalomedullary nails used for intertrochanteric hip fractures may have undergone revision surgery outside our institution post-operatively, which would not have been registered in this study, and subsequently falsely decrease the number of post-operative failures and other complications recorded. Furthermore, the changes of BMD, ALP, and other indices before and after surgery in the two groups were not recorded. Further evaluation in a larger randomized controlled study would be required to support the findings of this study.
CONCLUSIONS
In conclusion, the overall findings of this study showed bone quality had no influence on the complication rates between the helical blades and lag screws in cephalomedullary nails used for intertrochanteric hip fractures. Similar complication rates were observed between these two constructs; however, the helical blade design had a higher five-year survival rate.
ACKNOWLEDGEMENTS
The authors want to acknowledge the Enterprise Data and Analytics team from Sanford Health for their support on data pulling. The authors wish to thank Robert Van Demark III, M.D., Kelly McKnight, M.D., and Mikayla Forness, M.D. for their assistance on this study.
REFERENCES
- 1.Magaziner J, Hawkes W, Hebel JR, et al. Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci. 2000;55(9):M498–507. doi: 10.1093/gerona/55.9.m498. [DOI] [PubMed] [Google Scholar]
- 2.Chrischilles EA, Butler CD, Davis CS, Wallace RB. A model of lifetime osteoporosis impact. Arch Intern Med. 1991;151(10):2026–2032. [PubMed] [Google Scholar]
- 3.Cummings SR, Black DM, Rubin SM. Lifetime risks of hip, Colles', or vertebral fracture and coronary heart disease among white postmenopausal women. Arch Intern Med. 1989;149(11):2445–2448. [PubMed] [Google Scholar]
- 4.Cummings SR, Kelsey JL, Nevitt MC, O'Dowd KJ. Epidemiology of osteoporosis and osteoporotic fractures. Epidemiol Rev. 1985;7:178–208. doi: 10.1093/oxfordjournals.epirev.a036281. [DOI] [PubMed] [Google Scholar]
- 5.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7(5):407–413. doi: 10.1007/pl00004148. [DOI] [PubMed] [Google Scholar]
- 6.Cummings SR, Rubin SM, Black D. The future of hip fractures in the United States. Numbers, costs, and potential effects of postmenopausal estrogen. Clin Orthop Relat Res. 1990;(252):163–166. [PubMed] [Google Scholar]
- 7.Eberle S, Gerber C, von Oldenburg G, Hungerer S, Augat P. Type of hip fracture determines load share in intramedullary osteosynthesis. Clin Orthop Relat Res. 2009;467(8):1972–1980. doi: 10.1007/s11999-009-0800-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anglen JO, Weinstein JN American Board of Orthopaedic Surgery Research Committee. Nail or plate fixation of intertrochanteric hip fractures: Changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg Am. 2008;90(4):700–707. doi: 10.2106/JBJS.G.00517. [DOI] [PubMed] [Google Scholar]
- 9.Pajarinen J, Lindahl J, Michelsson O, Savolainen V, Hirvensalo E. Pertrochanteric femoral fractures treated with a dynamic hip screw or a proximal femoral nail. A randomised study comparing post-operative rehabilitation. J Bone Joint Surg Br. 2005;87(1):76–81. [PubMed] [Google Scholar]
- 10.Ahrengart L, Tornkvist H, Fornander P, et al. A randomized study of the compression hip screw and Gamma nail in 426 fractures. Clin Orthop Relat Res. 2002;(401):209–222. doi: 10.1097/00003086-200208000-00024. [DOI] [PubMed] [Google Scholar]
- 11.Madsen JE, Naess L, Aune AK, Alho A, Ekeland A, Stromsoe K. Dynamic hip screw with trochanteric stabilizing plate in the treatment of unstable proximal femoral fractures: A comparative study with the Gamma nail and compression hip screw. J Orthop Trauma. 1998;12(4):241–248. doi: 10.1097/00005131-199805000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Li S, Chang SM, Niu WX, Ma H. Comparison of tip apex distance and cut-out complications between helical blades and lag screws in intertrochanteric fractures among the elderly: A meta-analysis. J Orthop Sci. 2015;20(6):1062–1069. doi: 10.1007/s00776-015-0770-0. [DOI] [PubMed] [Google Scholar]
- 13.Stern LC, Gorczyca JT, Kates S, Ketz J, Soles G, Humphrey CA. Radiographic review of helical blade versus lag screw fixation for cephalomedullary nailing of low-energy peritrochanteric femur fractures: There is a difference in cutout. J Orthop Trauma. 2017;31(6):305–310. doi: 10.1097/BOT.0000000000000853. [DOI] [PubMed] [Google Scholar]
- 14.Flores SA, Woolridge A, Caroom C, Jenkins M. The utility of the tipapex distance in predicting axial migration and cutout with the trochanteric fixation nail system helical blade. J Orthop Trauma. 2016;30(6):e207–211. doi: 10.1097/BOT.0000000000000505. [DOI] [PubMed] [Google Scholar]
- 15.Liu W, Zhou D, Liu F, Weaver MJ, Vrahas MS. Mechanical complications of intertrochanteric hip fractures treated with trochanteric femoral nails. J Trauma Acute Care Surg. 2013;75(2):304–310. doi: 10.1097/TA.0b013e31829a2c43. [DOI] [PubMed] [Google Scholar]
- 16.Stern R, Lubbeke A, Suva D, Miozzari H, Hoffmeyer P. Prospective randomised study comparing screw versus helical blade in the treatment of low-energy trochanteric fractures. Int Orthop. 2011;35(12):1855–1861. doi: 10.1007/s00264-011-1232-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weil YA, Gardner MJ, Mikhail G, Pierson G, Helfet DL, Lorich DG. Medial migration of intramedullary hip fixation devices: A biomechanical analysis. Arch Orthop Trauma Surg. 2008;128(2):227–234. doi: 10.1007/s00402-007-0497-2. [DOI] [PubMed] [Google Scholar]
- 18.Kanis JA, Borgstrom F, De Laet C, et al. Assessment of fracture risk. Osteoporos Int. 2005;16(6):581–589. doi: 10.1007/s00198-004-1780-5. [DOI] [PubMed] [Google Scholar]
- 19.Feola M, Rao C, Tempesta V, Gasbarra E, Tarantino U. Femoral cortical index: An indicator of poor bone quality in patient with hip fracture. Aging Clin Exp Res. 2015;27(Suppl 1):S45–50. doi: 10.1007/s40520-015-0423-3. [DOI] [PubMed] [Google Scholar]
- 20.Geller JA, Saifi C, Morrison TA, Macaulay W. Tip-apex distance of intramedullary devices as a predictor of cut-out failure in the treatment of peritrochanteric elderly hip fractures. Int Orthop. 2010;34(5):719–722. doi: 10.1007/s00264-009-0837-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77(7):1058–1064. doi: 10.2106/00004623-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 22.Chapman T, Zmistowski B, Krieg J, Stake S, Jones CM, Levicoff E. Helical blade versus screw fixation in the treatment of hip fractures with cephalomedullary devices: Incidence of failure and atypical “medial cutout”. J Orthop Trauma. 2018;32(8):397–402. doi: 10.1097/BOT.0000000000001193. [DOI] [PubMed] [Google Scholar]
- 23.Lenich A, Vester H, Nerlich M, Mayr E, Stockle U, Fuchtmeier B. Clinical comparison of the second and third generation of intramedullary devices for trochanteric fractures of the hip--Blade vs screw. Injury. 2010;41(12):1292–1296. doi: 10.1016/j.injury.2010.07.499. [DOI] [PubMed] [Google Scholar]
- 24.Goffin JM, Pankaj P, Simpson AH, Seil R, Gerich TG. Does bone compaction around the helical blade of a proximal femoral nail anti-rotation (PFNA) decrease the risk of cut-out?: A subject-specific computational study. Bone Joint Res. 2013;2(5):79–83. doi: 10.1302/2046-3758.25.2000150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schwarzkopf R, Takemoto RC, Kummer FJ, Egol KA. Helical blade vs telescoping lag screw for intertrochanteric fracture fixation. Am J Orthop (Belle Mead NJ) 2011;40(9):452–456. [PubMed] [Google Scholar]
- 26.Strauss E, Frank J, Lee J, Kummer FJ, Tejwani N. Helical blade versus sliding hip screw for treatment of unstable intertrochanteric hip fractures: A biomechanical evaluation. Injury. 2006;37(10):984–989. doi: 10.1016/j.injury.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 27.Sommers MB, Roth C, Hall H, et al. A laboratory model to evaluate cutout resistance of implants for pertrochanteric fracture fixation. J Orthop Trauma. 2004;18(6):361–368. doi: 10.1097/00005131-200407000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Ibrahim I, Appleton PT, Wixted JJ, DeAngelis JP, Rodriguez EK. Implant cut-out following cephalomedullary nailing of intertrochanteric femur fractures: Are helical blades to blame? Injury. 2019;50(4):926–930. doi: 10.1016/j.injury.2019.02.015. [DOI] [PubMed] [Google Scholar]
- 29.Ciufo DJ, Zaruta DA, Lipof JS, Judd KT, Gorczyca JT, Ketz JP. Risk factors associated with cephalomedullary nail cutout in the treatment of trochanteric hip fractures. J Orthop Trauma. 2017;31(11):583–588. doi: 10.1097/BOT.0000000000000961. [DOI] [PubMed] [Google Scholar]
- 30.BoneDensityTest. [Accessed: July 17, 2023]. UpdatedSept2022 https://www.mayoclinic.org/tests-procedures/bone-density-test/about/pac-20385273#:~:text=and%20Z%2Dscore.-,T%2Dscore,What%20your%20score%20means.
- 31.Alkaline Phosphatase (ALP) - What is the normal range for alkaline phosphatase (ALP)? [Accessed: July 17, 2023]. Updated Nov 2021 https://my.clevelandclinic.org/health/diagnostics/22029-alkaline-phosphatase-alp.
- 32.ALP isoenzyme test - Normal Results. [Accessed: July 17, 2023]. Updated May 2021 https://ssl.adam.com/content.aspx?productid=117&pid=1&gid=003497&site=makatimed.adam.com&login=MAKA1603.
- 33.Alkaline Phosphatase (ALP) - What does it mean if my alkaline phosphatase (ALP) is high? [Accessed: July 17, 2023]. Updated Nov 2021 https://my.clevelandclinic.org/health/diagnostics/22029-alkaline-phosphatase-alp.
- 34.ALP isoenzyme test - What Abnormal Results Mean. [Accessed: July 17, 2023]. Updated May 2021 https://ssl.adam.com/content.aspx?productid=117&pid=1&gid=003497&site=makatimed.adam.com&login=MAKA1603.
- 35.McCormack R, Panagiotopolous K, Buckley R, et al. A multicentre, prospective, randomised comparison of the sliding hip screw with the Medoff sliding screw and side plate for unstable intertrochanteric hip fractures. Injury. 2013;44(12):1904–1909. doi: 10.1016/j.injury.2013.06.017. [DOI] [PubMed] [Google Scholar]
- 36.Verettas DA, Ifantidis P, Chatzipapas CN, et al. Systematic effects of surgical treatment of hip fractures: Gliding screw-plating vs intramedullary nailing. Injury. 2010;41(3):279–284. doi: 10.1016/j.injury.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 37.Laohapoonrungsee A, Arpornchayanon O, Phornputkul C. Two-hole side-plate DHS in the treatment of intertrochanteric fracture: Results and complications. Injury. 2005;36(11):1355–1360. doi: 10.1016/j.injury.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 38.Cauley JA, Lui LY, Stone KL, et al. Longitudinal study of changes in hip bone mineral density in Caucasian and African-American women. J Am Geriatr Soc. 2005;53(2):183–189. doi: 10.1111/j.1532-5415.2005.53101.x. [DOI] [PubMed] [Google Scholar]
- 39.Karlsson M, Nilsson JA, Sernbo I, Redlund-Johnell I, Johnell O, Obrant KJ. Changes of bone mineral mass and soft tissue composition after hip fracture. Bone. 1996;18(1):19–22. doi: 10.1016/8756-3282(95)00422-x. [DOI] [PubMed] [Google Scholar]
- 40.Fox KM, Magaziner J, Hawkes WG, et al. Loss of bone density and lean body mass after hip fracture. Osteoporos Int. 2000;11(1):31–35. doi: 10.1007/s001980050003. [DOI] [PubMed] [Google Scholar]
- 41.Dutta M, Pakhetra R, Garg M. Evaluation of bone mineral density in type 2 diabetes mellitus patients before and after treatment. Med J Armed Forces India. 2012;68(1):48–52. doi: 10.1016/S0377-1237(11)60120-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nakatoh S. The importance of assessing the rate of bone turnover and the balance between bone formation and bone resorption during daily teriparatide administration for osteoporosis: A pilot study. J Bone Miner Metab. 2016;34(2):216–224. doi: 10.1007/s00774-015-0665-3. [DOI] [PubMed] [Google Scholar]
- 43.Gombos GC, Bajsz V, Pek E, et al. Direct effects of physical training on markers of bone metabolism and serum sclerostin concentrations in older adults with low bone mass. BMC Musculoskelet Disord. 2016;17:254. doi: 10.1186/s12891-016-1109-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bergman A, Qureshi AR, Haarhaus M, et al. Total and bone-specific alkaline phosphatase are associated with bone mineral density over time in end-stage renal disease patients starting dialysis. J Nephrol. 2017;30(2):255–262. doi: 10.1007/s40620-016-0292-7. [DOI] [PubMed] [Google Scholar]
- 45.Buchet R, Millan JL, Magne D. Multisystemic functions of alkaline phosphatases. Methods Mol Biol. 2013;1053:27–51. doi: 10.1007/978-1-62703-562-0_3. [DOI] [PubMed] [Google Scholar]