HIGHLIGHTS
-
•
Local boards of health may provide key benefits to a local health department's performance.
-
•
Local board of health authority regarding budgets appears to have a positive influence.
-
•
Local health department governance structures appear not directly related to performance scores.
-
•
Involving boards of health in budget-related decision making could improve agency performance.
Keywords: Local health departments, local board of health, governing authority, budgets, governance structures, performance management
Abstract
Introduction
This study examined the relationship between local board of health authority and local health departments’ budget-related activities and performance scores in the Public Health Accreditation Board standards while considering the governance structure under which the local health agencies operate.
Methods
Data from 250 local health departments were obtained from the Public Health Accreditation Board and were combined with data from the 2016 National Association of County and City Officials Profile Survey. Multilevel regression analysis was used to examine the relationship between local board of health authority on local health departments’ budget-related activities, using the governance structure as the group-level variable.
Results
Analyses identified positive associations between local board of health authority on local health departments’ budget-related activities and local health departments’ aggregate average performance scores in Public Health Accreditation Board accreditation. No apparent association was found between the type of governance structure under which a local health department operates and performance scores in Public Health Accreditation Board accreditation standards, perhaps attributable to variation in the characteristics and roles of their governing bodies.
Conclusions
The analyses suggest that local boards of health with authority related to local health departments’ budgets appear to have an influential role in budget-related activities and may improve local health departments’ performance scores in Public Health Accreditation Board accreditation standards. However, vast variations in more specific local boards of health roles and characteristics exist across local health departments and for which there are no national data. More research is thus needed to control for or examine the influences of specific local boards of health characteristics before the benefits of expanded local boards of health authority over local health departments’ budgetary decision making on local health departments’ performance can be fully understood.
INTRODUCTION
Local health departments (LHDs) are key to the effectiveness of public health (PH) systems in the U.S. through programs and activities dedicated to protecting and promoting population health.1,2 There is great interest in LHDs’ continuous quality improvement and the need for strategies to measure their performance because their performance is crucial to communities’ well-being.3, 4, 5
Various factors have been shown to facilitate or hinder LHDs’ performance. Among these factors are the presence and functions,5,6 experience,7 and statutory power8,9 of a local board of health (LBoH) serving an LHD.5, 6, 7, 8, 9, 10 An LHD's LBoH is defined as a “legally designated body whose members are appointed or elected to provide advisory functions and/or governing oversight for the primary governmental PH agency.”7,11
In addition, other factors influencing LHDs’ performance include the type of LHD governance structures—such as centralized (state governed), decentralized (standalone), or shared—in terms of their relationship with their state health department.3, 4, 5,12 Evidence from existing studies on the influence of governance structure on LHDs’ performance in PH services is mixed. Some studies show that state-governed LHDs perform better on PH services than standalone or shared structures4,13; other studies suggest otherwise.4,6
Relatedly, some existing studies show that both LHDs’ governance structure and their LBoH can influence an LHD leader's decision to participate in Public Health Accreditation Board (PHAB) accreditation14, 15, 16—a national accreditation program developed to promote health department performance through a set of standards and measures that determine proficiency in the 10 essential PH services.17,18
Furthermore, studies also show that LHDs’ involvement in performance improvement activities such as interest in accreditation is related to having an LBoH19, 20, 21 and that LBoHs that engage in continuous quality improvement functions are more likely to engage in directing, encouraging, and supporting LHDs’ participation in accreditation. How LHDs distribute their budgets across their programs also appears to influence their performance score in accreditation.22 However, budget decisions for an LHD could be influenced by the agency's governing authority, by their LBoH, or by policies regarding the agency's ability to use its own discretion in distributing available resources to PH programs.23 For example, a state-governed LHD may not have the discretion to allocate available resources for their foundational capabilities in a way that appears to optimize PHAB accreditation performance owing to state policy on allowable program expenditures.15 Therefore, understanding the association between these influencing factors and specific performance scores in the PHAB standards could provide insight to guide PH practitioners’ and policymakers’ decisions regarding LHD governance and LBoH oversight to support improvement in specific areas of PH performance.
This study aimed to examine the relationship between LHDs’ LBoH authority on LHDs’ budget-related activities and their performance scores in the PHAB standards while considering the governance structure under which the agencies operate.
METHODS
This secondary analysis used cross-sectional data to analyze the relationships described earlier. The study did not involve human subjects nor required review by our university's Human Subjects Division.
Study Sample
The sample included 250 LHDs from 38 states that completed the accreditation assessments with PHAB between the years 2013 and 2020 and participated in the 2016 National Association of County and City Health Officials (NACCHO) Profile survey. For regression analysis, only LHDs that participated in the 2016 NACCHO Profile were included (n=218).
Measures
Data for LHD governance structure, LBoH authority over budget, education level of LHD lead executive, and the number of counties served were obtained from the NACCHO Profile.24 The 2016 version of the NACCHO Profile had a 76% response rate and provided LHD data closest in time to when most of the accreditation assessments in our sample were conducted.24 Composite governance structure was established as an index providing a comprehensive classification of the LHDs’ relationship to their state, whether they operated under a local health and human services (LHHS) agency, and whether they had an LBoH or not (Table 1). LBoH authority level over budget was defined as the number (0–4) of budget-related activities that an LHD's LBoH has control over and that could impact budget decisions. These 4 items were depicted in the NACCHO Profile as hire or fire agency head; approve the LHD budget; advise LHD or elected officials on policies, programs, and budgets; and set policies, goals, and priorities that guide the LHD. Accreditation version (Version 1.0 or 1.5) and accreditation scores were obtained from PHAB. LHDs’ jurisdictional social and economic data came from the U.S. Census Bureau.25
Table 1.
Percentage of LHDs in Each Composite Governance Structure Category and Different LBoH Authority Levels on Budget-Related Activities
| Composite governance structure indexa | Percentage of LHD (n=250), % | LBoH authority level: number of budget-related activities under LBoH control |
|||
|---|---|---|---|---|---|
| 0, % | 1, % | 2, % | 3–4, % | ||
| 100 | 1 | 100 | 0 | 0 | 0 |
| 101 | 2 | 0 | 75 | 25 | 0 |
| 110 | 0 | 0 | 0 | 0 | 0 |
| 111 | 0 | 0 | 0 | 0 | 0 |
| 200 | 11 | 100 | 0 | 0 | 0 |
| 201 | 52 | 2 | 10 | 15 | 73 |
| 210 | 4 | 100 | 0 | 0 | 0 |
| 211 | 8 | 0 | 19 | 14 | 67 |
| 300 | 0 | 100 | 0 | 0 | 0 |
| 301 | 6 | 13 | 13 | 19 | 56 |
| 310 | 0 | 0 | 0 | 0 | 0 |
| 311 | 2 | 0 | 40 | 20 | 40 |
The first digit of the index indicates whether an LHD is 1 of 3 options: 1, state governed; 2, standalone; or 3, shared. The second digit indicates whether an LHD operates under an LHHS agency or not (1, yes; 0, no). The last digit indicates whether the LHD has an LBoH (1, yes; 0, no).
LBoH, local board of health; LHD, local health department.
Statistical Analysis
We used a multilevel regression approach to evaluate the association between LBoH authority and LHD performance scores in PHAB accreditation standards with LHDs grouped by composite governance structure index. The primary independent variable was LBoH authority. The dependent variable was performance scores in PHAB accreditation standards.27 We first used a generalized least square model to determine covariates that best fit the models. The selected model included the following covariates to control for their potential effects on the performance score: accreditation version, number of counties served by the LHD (usually 1), average median household income of the jurisdiction served, and education level of LHD lead executive. We used a mixed-model lognormal regression (assuming varying intercept and fixed slope for the independent variable and all covariates) to model the aggregate average performance score and performance scores in each of the PHAB standards.
The models were also stratified by performance cluster—the cluster number identified the performance group to which an LHD belonged. The cluster number was generated from a k-means cluster analysis of performance scores in PHAB standards, the methods for which are described elsewhere.26 The cluster analysis identified 3 distinct groups: Cluster 1 (n=103) with an average score of 0.95, Cluster 2 (n=135) with an average score of 0.87, and Cluster 3 (n=12) with an average score of 0.71.
The regression estimates were used to predict the aggregate average score in PHAB accreditation for an average LHD with differing LBoH authority levels. The prediction was stratified by accreditation version and performance cluster, and the final output was transformed from a log scale to a linear (percent) scale. All data treatment and statistical analyses were performed in R Software package, Version 4.0.2. Missing values were imputed using Amelia bootstrap expectation maximization algorithm with 5 replicates. The percentage of missing values for each covariate ranged from 0.8% to 13%. Total missing values were approximately 3.5% of the total observations.
Results
Descriptive Statistics of Composite Governance Structure Index and Local Board of Health Authority
Table 1 shows the percentage of LHDs in each composite governance structure index and the percentage of LHDs with respect to the number (0–4) of budget-related activities under the LBoH authority. The majority (52%) of LHDs have governance structure Category 201 (standalone governance class, not under an LHHS agency, and having an LBoH). The percentage of LHDs with respect to the number of budget-related activities under the LBoH authority indicates that LBoHs of state-governed LHDs (Categories 101 and 111) had less authority than those that were standalone (Categories 201 and 211) or under shared governance (Categories 301 and 311). Among LHDs that reported having an LBoH (n=176), 86% (n=151) reported having a standalone governance structure (Categories 201 and 211), and a high percentage (>67%) of these LHDs had an LBoH with ≥3 authority levels. This was followed by LHDs with shared-governance structures, with 40% from Category 301 and 56% from Category 311 having 3 or more LBoH authority levels. None of the state-governed LHDs had 3 or more LBoH authority levels, and as expected, LHDs with no LBoH (Categories 100, 110, 200, 210, 300, and 310) reported no LBoH authority.
Modeling Authority and Performance Score in Public Health Accreditation Board Accreditation
The fixed effects estimate for aggregate average performance score suggests a strong association between LBoH authority level (0.72, p<0.01) and the aggregate average score in PHAB accreditation27 (Table 2). The model suggests that the aggregate average score in PHAB accreditation is likely to increase by 0.72% with a unit increase in the number of budget-related activities under the LBoH authority. Positive associations were also observed for performance scores in each of the individual PHAB standards, except for 8 standards, across a variety of different domains (Table 2). The strength of the association with individual standards varied, with a significance of p<0.05 found in 12 of the 32 standards. For a unit increase in the level of LBoH authority, the magnitude of a performance score increase in each of the standards ranged from 0.1% to 5.6%. The random effect estimates (results not shown) suggest that performance scores in PHAB accreditation standards have no apparent association with governance structure.
Table 2.
Change in Average PHAB Standard Performance Score (%) With an Increase in LBoH Budget-Related Authority Level
| Categories of PHAB score domains and standards | Percent change in PHAB score for each unit increase in the LBoH authority level | p-Value |
|---|---|---|
| Aggregate average scorea | 0.72 | 0.006 |
| D1S1 | 2.06 | 0.013 |
| D1S2 | 1.78 | 0.046 |
| D1S3 | 0.74 | 0.343 |
| D1S4 | 0.10 | 0.757 |
| D2S1 | –0.21 | 0.219 |
| D2S2 | 1.17 | 0.080 |
| D2S3 | 0.83 | 0.259 |
| D2S4 | 1.41 | 0.054 |
| D3S1 | –1.30 | 0.035 |
| D3S2 | 0.45 | 0.264 |
| D4S1 | 3.24 | 0.003 |
| D4S2 | –1.29 | 0.113 |
| D5S1 | 2.14 | 0.019 |
| D5S2 | 2.43 | 0.038 |
| D5S3 | 2.44 | 0.012 |
| D5S4 | 0.68 | 0.481 |
| D6S1 | 0.98 | 0.214 |
| D6S2 | –0.07 | 0.607 |
| D6S3 | –0.83 | 0.259 |
| D7S1 | –1.01 | 0.189 |
| D7S2 | –0.79 | 0.244 |
| D8S1 | –1.16 | 0.245 |
| D8S2 | 0.29 | 0.521 |
| D9S1 | 0.97 | 0.251 |
| D9S2 | 1.85 | 0.042 |
| D10S1 | 0.18 | 0.327 |
| D10S2 | 0.23 | 0.569 |
| D11S1 | 0.72 | 0.173 |
| D11S2 | 1.76 | 0.022 |
| D12S1 | 0.64 | 0.122 |
| D12S2 | 5.55 | 0.000 |
| D12S3 | 0.53 | 0.359 |
Note: Domain description: D1, conduct and disseminate assessments focused on population health status and public health issues facing the community; D2, investigate health problems and environmental public health hazards to protect the community; D3, inform and educate about public health issues and functions; D5, develop public health policies and plans; D6, enforce public health laws; and D9, evaluate and continuously improve processes, programs, and interventions. Full descriptions of domains and standards are described elsewhere.27 D denotes domain, and S denotes standard.
Average of D1 through D12 and S1 through S2–S4 (depending on domain).LBoH, local board of health; LHD, local health department; PHAB, Public Health Accreditation Board.
Prediction of Performance Score With Different Levels of Authority
Using the fixed effects estimates of the log-linear multilevel regression, a prediction of performance score with respect to LBoH authority level for an average LHD was examined using a counterfactual do-calculus approach. Figure 1 shows the performance score with a 95% prediction interval for an average LHD with LBoH authority from 0 to 4, accredited with PHAB Accreditation Standards and Measures, Version 1.5, and in performance Cluster 2 (moderate-performance group). Other covariates were kept constant at their average. In general, performance scores increased with LBoH authority level, inclusive of authority activities outside of those that were directly budget related.
Figure 1.
Predicted aggregated performance score for an average LHD as a function of LBoH authority level. Shaded region represents a 95% prediction interval.
LboH, local board of health; LHD, local health department.
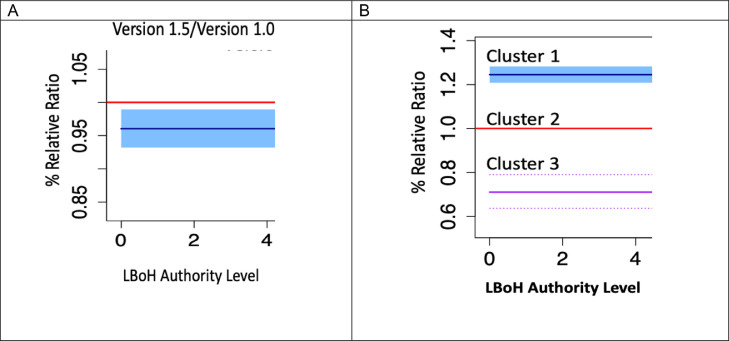
Accreditation version also appeared to influence the performance score for the sample used in this study because the LHDs accredited with PHAB Standards and Measures, Version 1.0, were likely to score approximately 4% higher than those accredited with Version 1.5 (Figure 2A). Similarly, Figure 2B shows the RRR of performance score for an LHD in performance Cluster 1 (high-performance group) and Cluster 3 (low-performance group). The results indicate that the performance scores for LHDs in Cluster 1 were approximately 15% higher than for LHDs in Cluster 2 at any level of authority between 0 and 4. Conversely, the performance score for LHDs in Cluster 3 was approximately 20% less than that of LHDs in Cluster 2 at any level of authority between 0 and 4.
Figure 2.
Relative ratio of performance score for an average LHD accredited in Version 1.5 vs. Version 1.0 as a function of LBoH authority level. (A) Version 1.5 and 1.0 are represented by the blue and red lines, respectively. The shaded region represents a 95% prediction interval. (B) The shaded region (Cluster 1/high performance group) and dashed lines (Cluster 3/low performance group) represent a 95% prediction interval. LbOH, local board of health; LHD, local health department.
Discussion
The descriptive analyses show that LBoHs of LHDs under standalone governance were more likely to have more budget-related authority than those that reported being state governed or shared. This suggests that LBoHs of LHDs that are standalone appear to have more power and responsibility to direct and influence LHDs’ activities. In addition, being under an LHHS agency appears related to lesser LBoH authority levels but to a lesser degree than being under state governance. Despite these apparent relationships between LBoH and governance, no apparent relationship between LHDs’ governance structures and performance scores in PHAB accreditation was observed. Although analysis of the average PH expenditures per capita in a previously reported study suggests that state-governed LHDs tend to spend less per capita than standalone or shared-governed LHDs,28 performance scores in PHAB accreditation in this study seemed to be similar for each of the governance structure categories. This observation seems consistent with those of previous studies where the conclusions on the association between governance structure and PH agencies’ performance were mixed and perhaps underscores a lack of relationship.4,6,13 Lack of a distinct association between governance structure and PHAB performance score may also be because of the influence of accreditation policy in some states. For example, Ohio and Florida have a mandatory policy on accreditation and leverage the PHAB standards. Other states (e.g., North Carolina, Michigan) have developed statewide accreditation policies that leverage state-based accreditation-like programs, although not PHAB accreditation.15,29
Although some previous studies have attributed the likelihood of accreditation uptake to the presence of an LBoH,3, 4, 5 the LHDs with no LBoH among the sample for this study did not perform less well on their accreditation scores than those having an LBoH. This may be explained by many variations that exist in the roles and characteristics of LBoH across LHDs. The mere presence of LBoH is unlikely to increase accreditation performance scores if the LBoH is not committed to supporting LHDs’ quality improvement efforts and essential PH services with the LHD. Another possible explanation is that the standalone agencies may be more likely to encounter challenges in pursuing accreditation than state-governed or shared-governed agencies that may have better resources, especially when the state has an accreditation policy that supports LHDs operating under them.
Previous studies suggest that the presence of LBoH positively associates with per capita spending and may thus influence LHDs’ activities and their performance.5, 6, 7,28 The results of this study support this previous evidence and further suggest that when established to play a vital role with an LHD, LBoHs appear to be a potentially important partner and benefit to the LHD's performance and thus its ability to serve its community. In particular, the degree of LBoH authority, especially the budget-related activities, can have a positive influence on an LHD's performance. LBoHs can influence LHDs’ activities in several ways, including the authority to recommend or establish agencies’ priorities and budget approval.7 One study suggests that LHDs rely on LBoH's input on resource allocation decisions to support LHDs’ programs and activities.23 The observed increase in average accreditation performance score by almost 1% when budget-related activities under LBoH authority increases by one unit may indicate the effectiveness in LBoHs’ roles when helping to set and support LHDs’ priorities. This may also indicate that LBoH budget advice can be supportive of LHDs’ quality improvement efforts, especially when LBoHs utilize their authority effectively in support of LHD programs and activities.15,19, 20, 21
Although the analyses in this study suggest allowing LBoHs more authority on budget-related activities, such broad power over LHDs’ budget policy could lead to an unfavorable outcome, especially if the LBoH is not committed to the shared responsibilities of the agency's quality improvement efforts to support community health outcomes. Previous studies have reported low performance of LBoHs in accreditation prerequisite activities (community health assessment, community health improvement planning, and strategic planning) and underutilization of the boards in agencies’ efforts to improve community health outcomes.7,8 A recent study found significant gaps in LBoH participation in the quality improvement efforts of LHDs.30 Insights from these previous studies indicate that a lack of LBoH engagement in an LHD's quality improvement efforts may inhibit performance in accreditation. However, as suggested in our study, LBoHs can seemingly play a role in strengthening LHDs’ performance in PHAB accreditation when LBoH statutory powers are used for the common good of the agency and the community they serve. This is supported by research showing that LBoHs engaged in quality improvement functions are likely to support LHDs’ accreditation activities.31 In addition, because resource availability is a major factor for successful accreditation,32,33 when LBoHs support LHD accreditation, both LBoH and LHD leadership can engage in mutual collaboration on strategic planning and resource management to ensure successful accreditation. Therefore, for the positive association found in this study to be meaningful to PH practice and LHD accreditation performance, LBoHs must see the broader authority on budget policy as a shared responsibility, together with the agency, to improve LHDs’ ability to provide the essential PH services.
The findings of this study also present implications for policy. The study supports PH leaders’ efforts to understand how LHDs’ governing structures as well as the authority and functions of LBoHs may influence LHDs’ effectiveness, efficiency, and potential community health outcomes. The legal powers and functions of LBoHs as governing boards can influence LHDs’ policy decision making on finances, accreditation, and other areas that are central to LHD performance. The National Association of Local Boards of Health, which serves as a voice for the nation's boards that govern PH agencies, developed a model of 6 functions of PH governance to strengthen and improve governance.11,34 These 6 functions include policy development and resource stewardship. Resource stewardship entails PH governance to develop or approve a budget that aligns with the agency's identified needs. It also encourages PH governance that advocates for necessary funding to sustain LHD activities, when appropriate, and the exercising of fiduciary care of the funds entrusted to the agencies.11 These responsibilities require an understanding of how the authority entrusted to LBoHs affects LHD activities, and the implication for LHDs’ accreditation performance is important for evidence-based strategies and policy to improve LHDs’ performance. The results of this study suggest that involving LBoHs in collaborative, budget-related decision making could be one possible strategy to improve LHDs’ performance by broadening the responsibility for and influence of the LHD through LBoH partners that are ideally committed to collaboratively achieving better population health outcomes.
Limitations
This study has limitations because the limited sample size for modeling performance scores hampered the model's ability to show significance. More statistical power and less need for multiple imputation would have been preferred. The cross-sectional data also limited our ability to infer a causal relationship between LBoH authority and LHDs’ performance scores in PHAB accreditation. Some potentially influential factors were unobserved, such as individual jurisdiction variation and differences in make-up or membership of individual LBoHs—factors that may have impacted LHD performance. Future study should explore, for example, how LBoH contributions to LHDs’ performance in PHAB accreditation differs when LBoHs are composed entirely of elected officials, are more inclusive of health experts, and are elected or appointed or as they change (perhaps owing to the influence of the pandemic) over time. In addition, results about accredited LHDs in this study may not be generalizable to nonaccredited health departments. Nevertheless, the analysis in this study provides insight into the understanding of the influence of LHD governance structure and the LBoH authority level. This insight could guide evidence-based strategies and policies on LHDs’ performance in PHAB accreditation assessments.
Conclusions
This study shows that LBoHs with authority over budget-related activities are positively associated with LHD performance scores in PHAB accreditation. A broader LBoH authority on budget-related activities should be seen as shared responsibility for budget policy and strategic planning that enhances LHDs’ performance in accreditation and agency efforts to improve community health outcomes. The findings contribute to the existing body of knowledge regarding the impact of LHDs’ governing authorities on quality improvement in PH. Such insight can be used to guide strategies and policies that benefit LHDs’ accreditation uptake and improved performance scores, which may in turn serve to support their communities’ health more effectively.
Acknowledgments
ACKNOWLEDGMENTS
The authors thank the Public Health Accreditation Board (PHAB) for access to PHAB accreditation assessment data. The use of these data does not imply PHAB's endorsement of the research, research methods, or the conclusions contained in the work. This study did not involve human subjects; hence, it did not require an IRB review.
Declarations of interest: none.
CRediT AUTHOR STATEMENT
Oluwatosin O. Dada: Conceptualization, Data curation, Formal analysis, Methodology, Writing - original draft, Writing - review & editing. Betty Bekemeier: Supervision, Writing - review & editing. Abraham Flaxman: Supervision, Writing - review & editing. A.B. de Castro: Writing - review & editing.
REFERENCES
- 1.National Association of County & City Health Officials (NACCHO) National Association of County & City Health Officials (NACCHO); Washington, DC: 2005. Operational definition of a functional local health department.https://www.naccho.org/uploads/downloadable-resources/Operational-Definition-of-a-Functional-Local-Health-Department.pdf Published November. [Google Scholar]
- 2.Institute of Medicine, The Future of the Public’s Health in the 21st Century, 2003, National Academies Press; Washington DC. https://www.ncbi.nlm.nih.gov/books/NBK221239/. Accessed April 13, 2019.
- 3.Scutchfield FD, Knight EA, Kelly AV, Bhandari MW, Vasilescu IP. Local public health agency capacity and its relationship to public health system performance. J Public Health Manag Pract. 2004;10(3):204–215. doi: 10.1097/00124784-200405000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Mays GP, McHugh MC, Shim K, et al. Institutional and economic determinants of public health system performance. Am J Public Health. 2006;96(3):523–531. doi: 10.2105/AJPH.2005.064253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhandari MW, Scutchfield FD, Charnigo R, Riddell MC, Mays GP. New data, same story? Revisiting studies on the relationship of local public health systems characteristics to public health performance. J Public Health Manag Pract. 2010;16(2):110–117. doi: 10.1097/PHH.0b013e3181c6b525. [DOI] [PubMed] [Google Scholar]
- 6.Mays GP, Halverson PK, Baker EL, Stevens R, Vann JJ. Availability and perceived effectiveness of public health activities in the nation's most populous communities. Am J Public Health. 2004;94(6):1019–1026. doi: 10.2105/ajph.94.6.1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones JA, Fenton GD. Composition and duties of local boards of health: findings from a 2011 national survey. J Public Health Manag Pract. 2012;18(6):609–614. doi: 10.1097/PHH.0b013e31825fba97. [DOI] [PubMed] [Google Scholar]
- 8.Patton D, Moon CE, Jones J. Describing local boards of health: insights from the 2008 National Association of Local Boards of Health Survey. Public Health Rep. 2011;126(3):410–419. doi: 10.1177/003335491112600315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hays SP, Toth J, Poes MJ, Mulhall PF, Remmert DM, O'Rourke TW. Public health governance and population health outcomes. Front Public Health Serv Syst Res. 2012;1(1):4. doi: 10.13023/FPHSSR.0101.04. [DOI] [Google Scholar]
- 10.Newman SJ, Leep CJ. A look at local public health governance: findings from the 2015 local board of health national profile. J Public Health Manag Pract. 2016;22(6):609–611. doi: 10.1097/PHH.0000000000000476. [DOI] [PubMed] [Google Scholar]
- 11.National Association of Local Boards of Health (NALBOH) National Association of County & City Health Officials (NACCHO); Washington, DC: 2012. The governance functions.https://cdn.ymaws.com/nalboh.site-ym.com/resource/resmgr/Docs/Governance_Functions.pdf Published November. [Google Scholar]
- 12.Eger RJ, III, Fortner CK, Hepburn VA, Slade CP. Does institutional structure effect public health expenditures? Public Budgeting & Finance. 2011;31(4):136–147. doi: 10.1111/j.1540-5850.2011.00996.x. [DOI] [Google Scholar]
- 13.Hyde JK, Shortell SM. The structure and organization of local and state public health agencies in the U.S.: a systematic review. Am J Prev Med. 2012;42(5):S29–S41. doi: 10.1016/j.amepre.2012.01.021. (suppl 1) [DOI] [PubMed] [Google Scholar]
- 14.Shah GH, Corso L, Sotnikov S, Leep CJ. Impact of local boards of health on local health department accreditation, community health assessment, community health improvement planning, and strategic planning. J Public Health Manag Pract. 2019;25(5):423–430. doi: 10.1097/PHH.0000000000000847. [DOI] [PubMed] [Google Scholar]
- 15.Thielen L, Dauer E, Burkhardt D, Lampe S, VanRaemdonck L. An examination of state laws and policies regarding public health agency accreditation prerequisites. J Public Health Manag Pract. 2014;20(1):111–118. doi: 10.1097/PHH.0b013e3182a505c9. [DOI] [PubMed] [Google Scholar]
- 16.Yeager VA, Ye J, Kronstadt J, Robin N, Leep CJ, Beitsch LM. National voluntary public health accreditation: are more local health departments intending to take part? J Public Health Manag Pract. 2016;22(2):149–156. doi: 10.1097/PHH.0000000000000242. [DOI] [PubMed] [Google Scholar]
- 17.The Public Health National Center for Innovations . The Public Health National Center for Innovations; Alexandria, VA: 2020. The 10 essential public health services.https://phnci.org/uploads/resource-files/EPHS-English.pdf Published. [Google Scholar]
- 18.About. Public Health Accreditation Board. https://phaboard.org/accreditation-background/. Updated 2023. Accessed January 5, 2021.
- 19.Chen LW, Nguyen A, Jacobson JJ, Gupta N, Bekmuratova S, Palm D. Relationship between quality improvement implementation and accreditation seeking in local health departments. Am J Public Health. 2015;105(suppl 2):S295–S302. doi: 10.2105/AJPH.2014.302278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shah GH, Beatty K, Leep C. Do PHAB accreditation prerequisites predict local health departments’ intentions to seek voluntary national accreditation? Front Public Health Serv Syst Res. 2013;2(3):4. doi: 10.13023/FPHSSR.0203.04. [DOI] [Google Scholar]
- 21.Luo H, Sotnikov S, McLees A, Stokes S. Factors driving the adoption of quality improvement initiatives in local health departments: results from the 2010 profile study. J Public Health Manag Pract. 2015;21(2):176–185. doi: 10.1097/PHH.0000000000000113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dada OO, Bekemeier B, Flaxman A, de Castro AB. Associations between local health department expenditures on foundational capabilities and PHAB accreditation standards scores. Front Public Health. 2022;10 doi: 10.3389/fpubh.2022.861587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baum NM, DesRoches C, Campbell EG, Goold SD. Resource allocation in public health practice: a national survey of local public health officials. J Public Health Manag Pract. 2011;17(3):265–274. doi: 10.1097/PHH.0b013e318207599c. [DOI] [PubMed] [Google Scholar]
- 24.National Association of County & City Health Officials (NACCHO) National Association of County & City Health Officials (NACCHO); Washington, DC: 2016. National profile of local health departments.http://nacchoprofilestudy.org/wp-content/uploads/2017/10/ProfileReport_Aug2017_final.pdf Published. [Google Scholar]
- 25.Annual report. America's Health Rankings. https://www.americashealthrankings.org/explore/annual/measure/PH_funding/state/ALL. Updated 2022. Accessed July 19, 2020.
- 26.Dada OO, Bekemeier B, Flaxman A, de Castro B. Local health departments’ characteristics and their performance scores in PHAB accreditation standards. J Public Health Manag Pract. 2022;28(4):375–383. doi: 10.1097/PHH.0000000000001458. [DOI] [PubMed] [Google Scholar]
- 27.Public Health Accreditation Board (PHAB). https://phaboard.org/. Accessed July 2, 2020.
- 28.Mays GP, Smith SA. Evidence links increases in public health spending to declines in preventable deaths. Health Aff (Millwood) 2011;30(8):1585–1593. doi: 10.1377/hlthaff.2011.0196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Matthews GW, Markiewicz M, Beitsch LM. Legal frameworks supporting Public Health Department accreditation: lessons learned from 10 states. J Public Health Manag Pract. 2012;18(1):E8–E16. doi: 10.1097/PHH.0b013e31822f62b0. [DOI] [PubMed] [Google Scholar]
- 30.Nguyen TH, Shah GH, Schwartz RD, Jones JA. Factors associated with continuous improvement by local boards of health. J Public Health Manag Pract. 2019;25(5):415–422. doi: 10.1097/PHH.0000000000001009. [DOI] [PubMed] [Google Scholar]
- 31.Shah GH, Sotnikov S, Leep CJ, Ye J, Corso L. Local boards of health characteristics influencing support for health department accreditation. J Public Health Manag Pract. 2018;24(3):263–270. doi: 10.1097/PHH.0000000000000623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leider JP, Kronstadt J, Yeager VA, et al. Application for public health accreditation among U.S. local health departments in 2013 to 2019: impact of service and activity mix. Am J Public Health. 2021;111(2):301–308. doi: 10.2105/AJPH.2020.306007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shah GH, Leep CJ, Ye J, Sellers K, Liss-Levinson R, Williams KS. Public Health Agencies’ level of engagement in and perceived barriers to PHAB National Voluntary Accreditation. J Public Health Manag Pract. 2015;21(2):107–115. doi: 10.1097/PHH.0000000000000117. [DOI] [PubMed] [Google Scholar]
- 34.Carlson V, Chilton MJ, Corso LC, Beitsch LM. Defining the functions of public health governance. Am J Public Health. 2015;105(suppl 2):S159–S166. doi: 10.2105/AJPH.2014.302198. [DOI] [PMC free article] [PubMed] [Google Scholar]