Abstract
BACKGROUND
Developmental venous anomalies (DVAs) are congenital anatomical variants of the normal deep parenchymal veins. DVAs are occasionally found incidentally on brain imaging, and most cases are asymptomatic. However, they rarely cause central nervous disorders. Herein, a case of mesencephalic DVA that caused aqueduct stenosis and hydrocephalus and discuss its diagnosis and treatment is reported.
OBSERVATIONS
The patient was a 48-year-old female who presented with depression. Computed tomography and magnetic resonance imaging (MRI) of the head revealed obstructive hydrocephalus. Contrast-enhanced MRI revealed an abnormally distended linear region with enhancement on the top of the cerebral aqueduct, which was confirmed as a DVA by digital subtraction angiography. An endoscopic third ventriculostomy (ETV) was performed to improve the patient’s symptoms. Intraoperative endoscopic imaging showed obstruction of the cerebral aqueduct by the DVA.
LESSONS
This report describes a rare case of obstructive hydrocephalus caused by DVA. It highlights the usefulness of contrast-enhanced MRI for diagnosing cerebral aqueduct obstructions due to DVAs and the effectiveness of ETV as a treatment option.
Keywords: mesencephalic developmental venous anomalies, endoscopic third ventriculostomy, obstructive hydrocephalus
ABBREVIATIONS: CSF = cerebrospinal fluid, DVA = developmental venous anomaly, ETV = endoscopic third ventriculostomy, MRI = magnetic resonance imaging, VP = ventriculoperitoneal
Developmental venous anomalies (DVAs), previously termed venous angiomas, are congenital anatomical variants of the normal deep parenchymal veins. They were first reported by Wolf et al.1 in 1967 and were renamed DVAs in 1986 by Lasjaunisas et al.2 because of their benign nature. They are occasionally discovered incidentally during brain imaging, and most patients with DVAs are asymptomatic. However, some reports have shown that they can cause central nervous disorders.3 Hemorrhage, infarction, or seizure onset are common symptoms of DVA.4
Mechanical (obstructive or compressive) complications due to DVAs are rare,5 and only a few cases of obstructive hydrocephalus caused by DVA have been reported. Herein, we report a case of mesencephalic DVA that caused aqueductal stenosis and hydrocephalus and discuss its diagnosis. This article also highlights the effectiveness of contrast magnetic resonance imaging (MRI) for diagnosing cerebral aqueductal stenosis due to DVAs and its treatment.
Illustrative Case
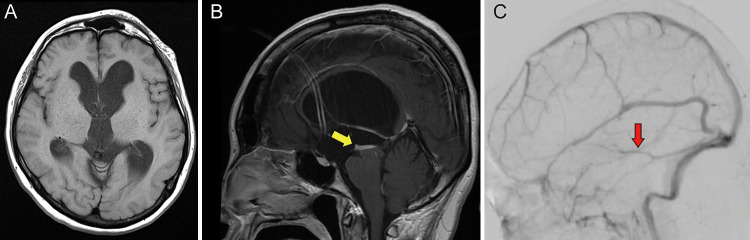
A 48-year-old female presented with a history of depression and had no associated complaints of headache, blurred vision, nausea, or vomiting. Head computed tomography and MRI showed dilation of the bilateral and third ventricles. However, the fourth ventricle was not dilated, indicating noncommunicating hydrocephalus in the cerebral aqueduct (Fig. 1A). Additional imaging studies were performed to investigate the cause of the obstruction. Contrast-enhanced MRI showed an abnormally distended linear region with enhancement on the top of the cerebral aqueduct (Fig. 1B), which was confirmed as a DVA on digital subtraction angiography (Fig. 1C).
FIG. 1.
A: Preoperative axial T1-weighted MR image showing that the bilateral temporal horns and third ventricle are dilated. The Evans index is 0.44. B: Preoperative sagittal T1-weighted contrast-enhanced MR image. The DVA directly above the cerebral aqueduct is observed as the abnormal distended linear region with enhancement (yellow arrow). The fourth ventricle is not dilated. An enhancing structure within the frontal horn is aliasing. C: Preoperative digital subtraction angiography shows a mesencephalic DVA (red arrow).
The patient underwent endoscopic third ventriculostomy (ETV), which was performed without complication. Intraoperative endoscopic imaging showed obstruction of the cerebral aqueduct by the DVA (Fig. 2). At the 6-month follow-up visit, the patient’s symptoms of depression had improved without any other medication. MRI showed that the size of the bilateral lateral ventricles was slightly reduced; the Evans Index decreased from 0.44 to 0.42. Therefore, we hypothesized that hydrocephalus due to obstruction of the cerebral aqueduct by DVA might have resulted in depression symptoms, which improved after releasing the fluid buildup by ETV.
FIG. 2.
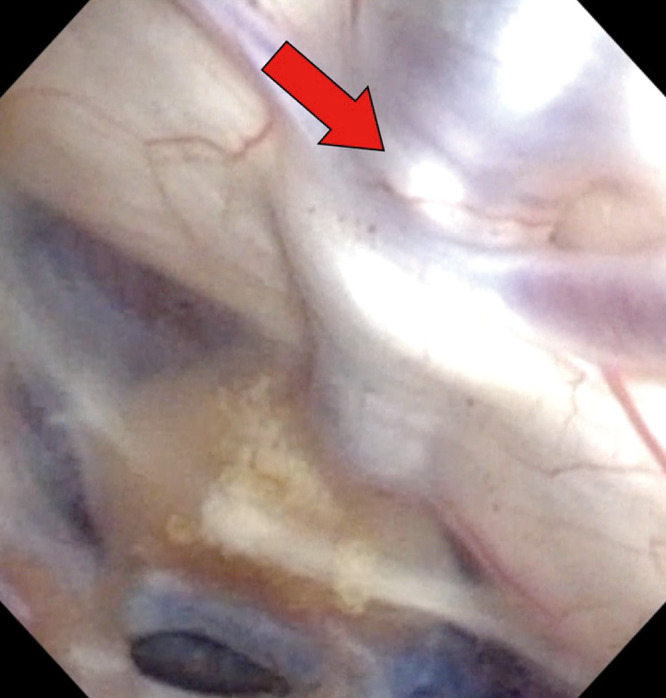
Intraoperative endoscopic view showed dilated veins of the DVA covering entry into the cerebral aqueduct (red arrow).
Discussion
Observations
This case shows that mesencephalic DVA can lead to obstructive hydrocephalus, which can be revealed by contrast-enhanced MRI. It also shows that ETV is an effective treatment option for this condition.
The pathological mechanism of symptomatic DVAs can be divided into two subsets, including those caused by 1) an imbalance of either the inflow or outflow in DVAs and 2) compression or obstruction of intracranial structures.5 An imbalance of the flow in DVAs can cause cranial hemorrhage or venous infarction.3 Additionally, DVAs can cause focal seizures because increased inflow or restricted outflow may result in cortical hyperemia and dysfunction.5–7 Mechanical complications and obstruction caused by DVAs due to their atypical locations can lead to various symptoms, including headaches and vertigo.5 However, obstructive hydrocephalus secondary to physical obstruction of DVAs is rare, and only 16 cases have been reported in the existing literature (Table 1).8–22
TABLE 1.
Reported cases of obstructive hydrocephalus due to aqueductal stenosis caused by DVAs
| Authors & Year | Age (yrs) | Sex | Sx | Imaging | Treatment | Outcome | |
|---|---|---|---|---|---|---|---|
| Giannetti et al., 20088 |
42 |
M |
Headache, behavior abnormality |
CT, MRI |
ETV |
Improvement in Sxs & images |
|
| |
18 |
M |
Headache |
CT, MRI |
ETV |
Improvement in Sxs & images |
|
| Cavallo et al., 20199 |
37 |
F |
Headache, vertigo |
MRI, angiography, endoscopy |
ETV |
Improvement in Sxs & images |
|
| Paulson et al., 201210 |
0 (3 days) |
F |
Macrocephaly |
MRI |
VP shunt |
Improvement in Sxs & images |
|
| Avman et al., 198011 |
35 |
F |
Headache |
Angiography, direct exploration |
Stenting |
Improvement in Sxs & images |
|
| Watanabe et al., 199112 |
39 |
M |
Headache |
MRI |
VP shunt |
Improvement in Sxs & images |
|
| Oka et al., 199313 |
43 |
F |
Seizure |
MRI, angiography, endoscopy |
ETV |
Improvement in images |
|
| Blackmore et al., 199614 |
16 |
F |
Headache |
MRI |
None |
No treatment |
|
| Bannur et al., 200215 |
11 |
M |
Headache |
MRI |
VP shunt |
Improvement in Sxs & images |
|
| Yagmurlu et al., 200516 |
7 |
F |
Headache |
MRI |
None |
No treatment |
|
| Guhl et al., 201117 |
0 (10 mos) |
F |
Macrocephaly |
MRI |
VP shunt |
Improvement in images |
|
| Inoue et al., 201318 |
10 |
M |
Headache, nausea |
MRI, endoscopy |
ETV |
Improvement in Sxs & images |
|
| Low & Seow, 202019 |
13 |
F |
Headache |
MRI |
ETV |
Improvement in Sxs & images |
|
| Kita et al., 201920 |
83 |
M |
Hakim’s triad |
MRI, endoscopy |
ETV |
Improvement in Sxs & images |
|
| Sato et al., 200421 |
28 |
F |
Headache, diplopia |
MRI, endoscopy |
ETV |
Improvement in Sxs & images |
|
| Xian et al., 202022 | 47 | M | Memory impairment | MRI, endoscopy | ETV | Improvement in Sxs & images |
CT = computed tomography; Sx = symptom.
Previously reported cases involved infants and older individuals (age range, 0–83 years), and the most common symptom was headache which was associated with increased intracranial pressure. The patients presented with headaches in 11 of the 16 cases. Other symptoms included behavioral abnormalities, vertigo, macrocephaly, seizures, nausea, Hakim’s triad, diplopia, and memory impairment. Cerebrospinal fluid (CSF) diversion procedures, such as ventriculoperitoneal (VP) shunting and ETV, were performed to treat hydrocephalus except in two cases that involved no treatment because the patients had mild symptoms. VP shunting and ETV were performed in four and nine cases, respectively. Although no long-term follow-up reports were available, patients’ symptoms improved in all cases involving treatment.
Lessons
Contrast-enhanced MRI can reveal aqueduct obstruction and its causes. Cerebral aqueductal stenosis is caused by several central nervous system disorders such as tumors, infection, hemorrhage, head trauma, and vascular lesions.23 In the present case, an abnormally distended linear region above the cerebral aqueduct was observed on contrast-enhanced MRI, and DVA was confirmed on angiography. Thus, DVA should be considered among the differential diagnoses when interpreting contrast magnetic resonance images in cases involving cerebral aqueductal stenosis.
Interventions that directly target symptomatic DVAs should ideally be avoided because removal of DVAs leads to venous infarction of the surrounding normal brain.4,24 Safer treatment options for obstructive hydrocephalus caused by DVAs are CSF shunting and ETV. However, the failure rate of CSF shunting has been reported to be higher than that of ETV in adult patients with aqueductal stenosis.24,25 Additionally, ETV is preferable to CSF shunting because it prevents various CSF shunting-related complications, such as infection or malfunction.
Furthermore, it is conceivable that obstructive hydrocephalus caused by DVAs has a prolonged course, especially in adult patients, because DVAs are congenital vascular variants. Chronic ventriculomegaly can cause loss of involved brain compliance, which makes treatment by shunting difficult.25 Therefore, ETV is considered a better treatment option. ETV was performed in the present case with a good outcome, and the patient had an uneventful course without complications. This article highlights the effectiveness of ETV as a treatment option for obstructive hydrocephalus due to cerebral aqueductal stenosis caused by DVAs.
In conclusion, although DVAs are benign vascular malformations, their presence around the cerebral aqueduct can cause obstructive hydrocephalus. Contrast-enhanced brain MRI is useful for diagnosing obstructive hydrocephalus due to cerebral aqueductal obstruction caused by DVAs, and ETV is an effective treatment option for this rare condition.
Acknowledgments
We would like to thank Editage for English language editing.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Hiraga, Hayashi, Oshima. Acquisition of data: Hiraga, Hayashi, Oshima, Kondo. Analysis and interpretation of data: Hiraga, Hayashi, Oshima. Drafting the article: Hiraga, Oshima, Kanamori. Critically revising the article: Hiraga, Oshima, Saito. Reviewed submitted version of manuscript: Hiraga, Oshima, Kanamori, Saito. Approved the final version of the manuscript on behalf of all authors: Hiraga. Statistical analysis: Hiraga, Oshima. Administrative/technical/material support: Hiraga, Hayashi, Oshima. Study supervision: Hiraga, Oshima, Saito.
References
- 1. Wolf PA, Rosman NP, New PFJ. Multiple small cryptic venous angiomas of the brain mimicking cerebral metastases. A clinical, pathological, and angiographic study. Neurology. 1967;17(5):491–501. doi: 10.1212/wnl.17.5.491. [DOI] [PubMed] [Google Scholar]
- 2. Lasjaunias P, Burrows P, Planet C. Developmental venous anomalies (DVA): the so-called venous angioma. Neurosurg Rev. 1986;9(3):233–242. doi: 10.1007/BF01743138. [DOI] [PubMed] [Google Scholar]
- 3. Aoki R, Srivatanakul K. Developmental venous anomaly: benign or not Benign. Neurol Med Chir (Tokyo) 2016;56(9):534–543. doi: 10.2176/nmc.ra.2016-0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hon JML, Bhattacharya JJ, Counsell CE, et al. The presentation and clinical course of intracranial developmental venous anomalies in adults: a systematic review and prospective, population-based study. Stroke. 2009;40(6):1980–1985. doi: 10.1161/STROKEAHA.108.533034. [DOI] [PubMed] [Google Scholar]
- 5. Pereira VM, Geibprasert S, Krings T, et al. Pathomechanisms of symptomatic developmental venous anomalies. Stroke. 2008;39(12):3201–3215. doi: 10.1161/STROKEAHA.108.521799. [DOI] [PubMed] [Google Scholar]
- 6. Morioka T, Hashiguchi K, Nagata S, et al. Epileptogenicity of supratentorial medullary venous malformation. Epilepsia. 2006;47(2):365–370. doi: 10.1111/j.1528-1167.2006.00429.x. [DOI] [PubMed] [Google Scholar]
- 7. Dussaule C, Masnou P, Nasser G, et al. Can developmental venous anomalies cause seizures? J Neurol. 2017;264(12):2495–2505. doi: 10.1007/s00415-017-8456-5. [DOI] [PubMed] [Google Scholar]
- 8. Giannetti AV, Rodrigues RBM, Trivelato FP. Venous lesions as a cause of sylvian aqueductal obstruction: case report. Neurosurgery. 2008;62(5):E1167–E1168. doi: 10.1227/01.neu.0000325882.21118.7d. [DOI] [PubMed] [Google Scholar]
- 9. Cavallo C, Faragò G, Broggi M, Ferroli P, Acerbi F. Developmental venous anomaly as a rare cause of obstructive hydrocephalus. J Neurosurg Sci. 2019;63(5):600–606. doi: 10.23736/S0390-5616.16.03465-2. [DOI] [PubMed] [Google Scholar]
- 10. Paulson D, Hwang SW, Whitehead WE, Curry DJ, Luerssen TG, Jea A. Aqueductal developmental venous anomaly as an unusual cause of congenital hydrocephalus: a case report and review of the literature. J Med Case Rep. 2012;6:7. doi: 10.1186/1752-1947-6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Avman N, Dinçer C. Venous malformation of the aqueduct of Sylvius treated by interventriculostomy: 15 years follow-up. Acta Neurochir (Wien) 1980;52(3-4):219–224. doi: 10.1007/BF01402077. [DOI] [PubMed] [Google Scholar]
- 12. Watanabe A, Ishii R, Kamada M, Suzuki Y, Hirano K, Okamura H. Obstructive hydrocephalus caused by an abnormal vein in the aqueduct. Case report. J Neurosurg. 1991;75(6):960–962. doi: 10.3171/jns.1991.75.6.0960. [DOI] [PubMed] [Google Scholar]
- 13. Oka K, Kumate S, Kibe M, Tomonaga M, Maehara F, Higashi Y. Aqueductal stenosis due to mesencephalic venous malformation: case report. Surg Neurol. 1993;40(3):230–235. doi: 10.1016/0090-3019(93)90072-9. [DOI] [PubMed] [Google Scholar]
- 14. Blackmore CC, Mamourian AC. Aqueduct compression from venous angioma: MR findings. AJNR Am J Neuroradiol. 1996;17(3):458–460. [PMC free article] [PubMed] [Google Scholar]
- 15. Bannur U, Korah I, Chandy MJ. Midbrain venous angioma with obstructive hydrocephalus. Neurol India. 2002;50(2):207–209. [PubMed] [Google Scholar]
- 16. Yagmurlu B, Fitoz S, Atasoy C, Erden I, Deda G, Unal O. An unusual cause of hydrocephalus: aqueductal developmental venous anomaly. Eur Radiol. 2005;15(6):1159–1162. doi: 10.1007/s00330-004-2356-7. [DOI] [PubMed] [Google Scholar]
- 17. Guhl S, Kirsch M, Lauffer H, Fritsch M, Schroeder HWS. Unusual mesencephalic developmental venous anomaly causing obstructive hydrocephalus due to aqueductal stenosis. J Neurosurg Pediatr. 2011;8(4):407–410. doi: 10.3171/2011.7.PEDS114. [DOI] [PubMed] [Google Scholar]
- 18. Inoue K, Yoshioka F, Nakahara Y, Kawashima M, Matsushima T. Obstructive hydrocephalus following aqueductal stenosis caused by supra- and infratentorial developmental venous anomaly: case report. Childs Nerv Syst. 2013;29(2):329–334. doi: 10.1007/s00381-012-1934-2. [DOI] [PubMed] [Google Scholar]
- 19. Low SYY, Seow WT. Biventricular hydrocephalus secondary to aqueductal developmental venous anomaly. J Clin Neurosci. 2020;76:240–243. doi: 10.1016/j.jocn.2020.04.039. [DOI] [PubMed] [Google Scholar]
- 20. Kita D, Park C, Hayashi Y. Aqueductal developmental venous anomaly presenting with mimic symptoms of idiopathic normal pressure hydrocephalus in an elderly patient: a case report. NMC Case Rep J. 2019;6(3):83–86. doi: 10.2176/nmccrj.cr.2018-0244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sato S, Sonoda Y, Kuroki R, Kayama T. [A rare case of aqueductal stenosis due to venous angioma]. Article in Japanese. No To Shinkei. 2004;56(12):1042–1046. [PubMed] [Google Scholar]
- 22. Xian Z, Fung SH, Nakawah MO. Obstructive hydrocephalus due to aqueductal stenosis from developmental venous anomaly draining bilateral medial thalami: a case report. Radiol Case Rep. 2020;15(6):730–732. doi: 10.1016/j.radcr.2020.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Aoki N. Non tumoral aqueduct stenosis and normal pressure hydrocephalus in the elderly. J Neurol Neurosurg Psychiatry. 1987;50(5):648. doi: 10.1136/jnnp.50.5.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rammos SK, Maina R, Lanzino G. Developmental venous anomalies: current concepts and implications for management. Neurosurgery. 2009;65(1):20–29. doi: 10.1227/01.NEU.0000347091.06694.3E. discussion 29–30. [DOI] [PubMed] [Google Scholar]
- 25. Oi S, Shimoda M, Shibata M, et al. Pathophysiology of long-standing overt ventriculomegaly in adults. J Neurosurg. 2000;92(6):933–940. doi: 10.3171/jns.2000.92.6.0933. [DOI] [PubMed] [Google Scholar]