Abstract
We present the case of a 4-year-old boy with annular, pruritic macules on the face who did not respond to the application of topical immunosuppressive therapy for atopic dermatitis.
In this case report, we emphasize how pruritic annular macules that are not responsive to immunosuppressants should always be suspected of being tinea incognita.
Key words: rash, atopic dermatitis, dermatophytosis, calcineurin inhibitors, griseofulvin
Introduction
We present the case of a 4-year-old boy with annular, pruritic macules on the face who was not responsive to the application of topical immunosuppressive therapy for atopic dermatitis.
Clinically, annular, pruritic macules with a cracked surface and crusted, raised borders slowly enlarging were observed on the boy’s cheeks. Dermatoscopy showed centrifugal extension and border hyperactivity, represented by multiple peripheral pustules, mainly follicular. At last, microscopy of skin scrapings, showing fungal hyphae, permitted the diagnosis of tinea incognita.
We highlight the need to always suspect tinea incognita in pruritic, annular macules not responsive to immunosuppressants.
Case Report
A 4-year-old Nigerian boy presented with a disfiguring, intensely pruritic facial rash accompanied by generalized pruritus and flexural eczema. The patient had had atopic dermatitis since the age of two. He applied emollients twice daily and tacrolimus ointment 0.03% three times a week on the most affected areas, such as flexural folds, the face, and the neck. On clinical examination, chronic eczema with diffuse xerosis, as well as lichenification and hyperpigmentation of the knee fold and inner elbow, were noticed. On his face, widely extended, persistently enlarging annular-to-polycyclic macules, not responsive to topical immunosuppressants, were observed. Lesions were flat, with a smooth, translucent, partially cracked surface and crusted, raised borders (Figure 1). Dermatoscopical examination revealed tiny satellite pustules outlying the periphery of facial lesions, suggesting hyperactivity at the border of lesions (Figure 2). Also, occasional scratch marks and erosions were noticed.
The patient denied exacerbation of skin rash with sun exposure, while he reported no benefit with tacrolimus application. His medical history was unremarkable except for atopic dermatitis, and he was not taking any systemic medications. A skin scraping was performed and underwent direct microscopical examination. A microscopic sample examination identified elements of a fungal infection consistent with tinea faciei incognita.1,2 The rash cleared after three weeks on griseofulvin (20 mg/kg/die), leaving tissue scarring, especially on his chin (Figure 3).
Discussion
Tinea incognita is a dermatophyte infection of the skin, exacerbated by the administration of systemic or topical immunosuppressants such as corticosteroids and calcineurin inhibitors.2,3
Figure 1.

Annular, pruritic macules on a 4-year-old boy with a cracked surface and crusted, raised borders slowly enlarging.
Figure 2.
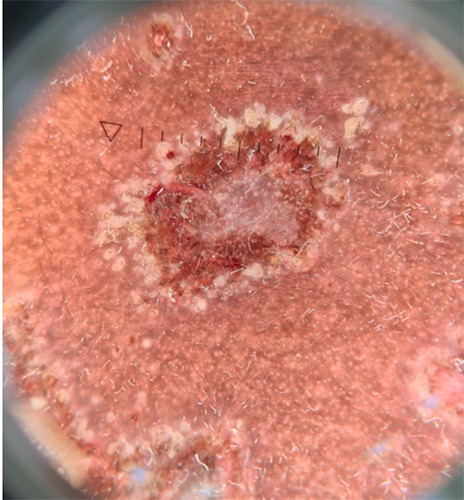
Dermoscopical image of an annular lesion showing centrifugal extension and border hyperactivity, represented by multiple peripheral pustules, mainly follicular.
Figure 3.

Resolution of the cutaneous rash after griseofulvin therapy, leaving disfiguring scar tissue.
Unlike classical tinea corporis, which presents typical welldelimited ringworm patches that are scaly and erythematous, tinea incognita is less scaly and less delimited.3,4 Notably, tinea incognita has a tendency for centrifugal extension with hyperactivity at the border of lesions.5,6 This allows tinea incognita to reach a wide extension, forming polymorphous annular-to-serpiginous configurations, often pustular and inflamed.6,7 Additionally, in high Fitzpatrick skin types, intense pigmentation causing a lack of erythema increases diagnostic difficulty.6-9
Tinea incognita represents indeed a challenging dermatological entity in all skin types. This dermatophytosis is often misdiagnosed as eczematous exacerbation, psoriasis, subacute or discoid cutaneous lupus, earning it the name “great imitator”, as well as syphilis.1-4
Increased awareness of the different clinical pictures assumed by tinea incognita in all skin types is needed, though its highly aspecific and polymorphic clinical presentation mostly requires confirmatory direct microscopic skin examination for identification of fungal elements. However, despite being very simple and easy to adopt, this is a non-universally available technique.
Conclusions
In conclusion, pruritic, annular macules not responsive to immunosuppressants should always raise the suspicion of tinea incognita, which must be investigated and ruled out to avoid infection persistence. Indeed, neglected superficial dermatophytosis could also possibly invade hair follicles and deeper tissues and cause permanent scarring, which must be prevented.
Funding Statement
Funding: none.
References
- 1.Nenoff P, Krüger C, Schaller J, et al. Mycology - an update part 2: dermatomycoses: clinical picture and diagnostics. J Dtsch Dermatol Ges 2014;12:749-77. [DOI] [PubMed] [Google Scholar]
- 2.Turra N, Navarrete J, Magliano J, Bazzano C. Follicular tinea faciei incognita: the perfect simulator. An Bras Dermatol 2019;94:372-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ive FA, Marks R. Tinea incognita. Br Med J 1968;3:149-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Herzum A, Molle MF, Cozzani E, et al. Pruritic erythematous macules in a patient with systemic sarcoidosis: a quiz. Acta Derm Venereol 2021;101:adv00531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Romano C, Maritati E, Gianni C. Tinea incognita in Italy: a 15-year survey. Mycoses 2006;49:383-7. [DOI] [PubMed] [Google Scholar]
- 6.Del Boz J, Crespo V, Rivas-Ruiz F, de Troya M. Tinea incognita in children: 54 cases. Mycoses 2011;54:254-8. [DOI] [PubMed] [Google Scholar]
- 7.Sonthalia S, Ankad BS, Goldust M, Jha AK. Dermoscopy - a simple and rapid in vivo diagnostic technique for tinea incognita. An Bras Dermatol 2019;94:612-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mitchell KN, Tay YK, Heath CR, Silverberg NB. Review article: emerging issues in pediatric skin of color, part 2. Pediatr Dermatol 2021;38:30-6. [DOI] [PubMed] [Google Scholar]
- 9.Bakos RM, Leite LL, Reinehr C, Escobar GF. Dermoscopy of skin infestations and infections (entomodermoscopy) - part II: viral, fungal and other infections. An Bras Dermatol 2021;96:746-58. [DOI] [PMC free article] [PubMed] [Google Scholar]


