ABSTRACT
Background: When exposed to events that transgress one’s moral beliefs, a plethora of negative consequences may follow, which are captured by the concept of moral injury (MI). Despite its relevance to experiences of healthcare workers during a global health emergency, there is lack of validated MI instruments adapted to the healthcare setting.
Objective: The present study aims to provide a validation of the Italian version of the Moral Injury Events Scale (MIES) adjusted to the healthcare setting by assessing its factor structure, internal consistency and construct validity.
Methods: A sample of 794 healthcare workers (46% nurses, 51% female) engaged in hospital facilities during the COVID-19 pandemic in Italy completed measures of MI, PTSD, anxiety, depression, burnout, meaning in life and positive affect.
Results: Using an exploratory structural equation modelling (ESEM) we assessed the scale factor structure for the entire sample and separately for nurse professional and female healthcare worker groups. Findings support a three-factor solution: Factor 1 ‘perceived transgressions by others’; Factor 2 ‘perceived transgressions by self’; and Factor 3 ‘perceived betrayals by others’. Findings also indicate some level of convergence with measures of PTSD, anxiety, depression and burnout.
Conclusion: Results suggest that the MIES may be useful in capturing unique experiences of moral injury amongst healthcare workers engaged in a global health emergency. The low range correlations with measures of psychological distress might potentially indicate that MI, which captures cognitive value judgements rather than manifest symptomatology, may uniquely explain a certain amount of variance. Implications for the development of new empirically derived and theoretical guided tools are discussed, highlighting the need for future research to examine the role of individualising and social binding moral principles in gaining a more nuanced understanding of moral injury experiences amongst healthcare professionals across different socio-cultural settings.
KEYWORDS: Moral Injury Events Scale, healthcare professionals, global health emergency, factor analysis, SEM, COVID-19
HIGHLIGHTS
The Italian validation of the MIES adapted to the healthcare setting yielded a three-factor structure: (a) ‘perceived transgressions by self’; (b) ‘perceived transgressions by others’; (c) ‘perceived betrayals by others’.
Findings suggest that the MIES may be useful in capturing unique experiences of moral injury amongst healthcare workers engaged in a global health emergency.
Future research should consider the role of individualising and social binding moral principles in shaping moral injury experiences among healthcare professionals across different socio-cultural settings.
Abstract
Antecedentes: Cuando una persona se ve expuesta a acontecimientos que transgreden sus creencias morales, puede sufrir una gran variedad de consecuencias negativas, que se recogen en el concepto de daño moral (Mi, por sus siglas en inglés). A pesar de su relevancia para las experiencias de los trabajadores sanitarios durante una emergencia sanitaria mundial, faltan instrumentos validados de MI adaptados al entorno sanitario.
Objetivo: El presente estudio tiene como objetivo proporcionar una validación de la versión italiana de la Escala de Eventos de Daño Moral (MIES) ajustada al ámbito sanitario mediante la evaluación de su estructura factorial, consistencia interna y validez de constructo.
Métodos: Una muestra de 794 trabajadores sanitarios (46% enfermeras, 51% mujeres) que trabajaban en establecimientos hospitalarios durante la pandemia COVID-19 en Italia completaron medidas de MI, TEPT, ansiedad, depresión, burnout, sentido de la vida y afecto positivo.
Resultados: Mediante un modelo exploratorio de ecuaciones estructurales (ESEM) evaluamos la estructura factorial de la escala para toda la muestra y por separado para los grupos de profesionales de enfermería y de trabajadoras sanitarias. Los resultados apoyan una solución de tres factores: Factor 1 ‘transgresiones percibidas por otros’; Factor 2 ‘transgresiones percibidas por uno mismo’; y Factor 3 ‘traiciones percibidas por otros’. Los resultados también indican cierto nivel de convergencia con las medidas de TEPT, ansiedad, depresión y burnout.
Conclusiones: Los resultados sugieren que el MIES puede ser útil para captar experiencias únicas de daño moral entre los trabajadores sanitarios que participan en una emergencia sanitaria mundial. Las correlaciones de bajo rango con las medidas de malestar psicológico podrían indicar que el MI, que capta los juicios de valor cognitivos en lugar de la sintomatología manifiesta, puede explicar de forma específica una cierta cantidad de varianza. Se discuten las implicaciones para el desarrollo de nuevas herramientas derivadas empíricamente y guiadas teóricamente, destacando la necesidad de que la investigación futura examine el papel de los principios morales individualizadores y socialmente vinculantes para obtener una comprensión más matizada de las experiencias de daño moral entre los profesionales sanitarios en diferentes entornos socioculturales.
PALABRAS CLAVE: Escala de eventos de daño moral, profesionales de la salud, emergencia sanitaria mundial, análisis factorial, SEM, COVID-19
Abstract
背景:当接触到违反道德信仰的事件时,可能会产生大量负面后果,这些后果被道德伤害(MI)的概念所体现。尽管它与全球健康紧急情况下医护人员的经历相关,缺乏适用于医护环境的经过验证的 MI 工具。
目的:本研究旨在通过评估因素结构、内部一致性和结构效度,对适应医护环境的意大利语版道德伤害事件量表(MIES)进行验证。
方法:意大利 COVID-19 疫情期间在医院机构工作的 794 名医护人员(46% 是护士,51% 是女性)样本完成了 MI、PTSD、焦虑、抑郁、倦怠、生活意义和积极情感的测量。
结果:使用探索性结构方程模型 (ESEM),我们评估了整个样本的标度因素结构,并分别评估了专业护士和女性医护人员群体的标度因素结构。调查结果支持三因素解决方案:因素 1‘他人认为有违规行为’; 因素2‘自我感知的违规行为’; 因素 3‘感知到他人的背叛’。研究结果还表明,与PTSD、焦虑、抑郁和倦怠的衡量标准有一定程度的收敛性。
结论:结果表明,MIES 可能有助于捕捉参与全球健康紧急情况的医护人员的独特道德伤害经历。与心理困扰测量值的低范围相关性可能表明,MI(捕捉认知价值判断而不是表现症状)可能唯一地解释一定量的方差。讨论了开发新的实证衍生和理论指导工具的含义,强调未来研究需要检验个体化和社会约束道德原则的作用,以更细致地了解不同社会文化背景的医护专业人员的道德伤害经历。
关键词: 道德伤害事件量表, 医护专业人员, 全球突发健康事件, 因素分析, SEM, COVID-19
1. Introduction
Morality is a fundamental dimension of social life, a compass that guides social interactions across contexts and groups (Haidt, 2008). Foundational building blocks of morality, such as caring for the vulnerable, sensing fairness and judging others’ harmful actions are hardwired into our brains as they enable us to live with others in large social groups, which is crucial for individual and social wellbeing. Indeed, theoretical perspectives (Graham et al., 2013; Haidt & Joseph, 2007) posit that moral principles such as caring, fairness or loyalty to common values generate automatic responses of disapprobation of unjustified harm and/or unfair treatment of others. In the same lines, independent studies have shown that when one is exposed to events that transgress one’s moral beliefs, a plethora of negative consequences may be experienced, which are captured by the concept of Moral Injury (MI, Litz et al., 2009). First examined in military personnel (Nash et al., 2013), MI has been proposed as a framework to account for a range of negative psychological consequences reported by individuals working in high-stake occupational settings, from police forces, to humanitarian aid, social welfare services (Griffin et al., 2019; Molendijk, 2022; Williamson et al., 2021), and more recently healthcare workers (Dean et al., 2019; Murray et al., 2018). Despite the conceptual appeal and the growing evidence base, there is lack of validated instruments, especially regarding MI in the healthcare setting (Williamson et al., 2021). The present study provides an initial validation of the Italian version of the Moral Injury Events Scale (MIES, Nash et al., 2013) and assesses the psychometric properties of the scale adjusted to the healthcare setting in the context of the global COVID-19 pandemic.
MI has been proposed to describe a trauma- and stressor-related phenomenon that involves exposure to potentially morally injurious events (PMIEs) that transgress deeply held moral values or violate one’s conscience and integrity (Zerach & Levi-Belz, 2021). Such events may be ‘self-referring’, including perpetrating acts of commission and omission (e.g. failing to prevent expected malfeasance, Jordan et al., 2017) or ‘other-referring’, which may involve direct and indirect exposure to others’ transgressive behaviours (e.g. others’ perceived immoral decisions or betrayal). Scientific inquiry and interest in the phenomenon of moral injury in the healthcare setting has intensified especially during the COVID-19 pandemic (for reviews see Čartolovni et al., 2021; Riedel et al., 2022; Ter Heide & Olff, 2023), with a plethora of papers recognising the uniqueness of the moral and ethical challenges faced by healthcare workers worldwide (Fino et al., 2020; Fino, Bonfrate, et al., 2021; Fino, Fino, et al., 2021; Greenberg et al., 2020). As a health emergency frequently implies a significant disbalance between needs and resources, the weighty responsibility of triage decisions (e.g. witnessing or deciding on who deserves a bed in intensive care and who doesn’t) can seriously impinge on one’s ethical and moral imperatives of providing care to all those who need it. Indeed, exposure to the suffering of COVID-19 patients, amidst overwhelmed facilities and lack of resources, left healthcare workers torn between the moral and ethical duty to provide care and the impossibility of doing so because of objective constraints, with serious implications for their psychological wellbeing. Consistently, research from different parts of the world has documented high levels of anxiety, depression, posttraumatic stress and burnout as well as symptoms of moral injury and unsettling levels of suicides amongst healthcare professionals during the pandemic (Pappa et al., 2020). Within the healthcare workforce, nurses, female healthcare workers and those engaged in the frontlines seem to be especially vulnerable to such negative outcomes (Fino et al., 2019; García-Fernández et al., 2020; Smith et al., 2023).
While the well-known constructs of burnout and vicarious traumatisation in healthcare may capture a great part of the emotional and psychological challenges involved in the daily practice of the caretaking profession (Bordoagni et al., 2021; Fino et al., 2019), it has been argued that they do not account for the entire range and complexity of trauma responses experienced by healthcare workers. Although some of the manifestations may look alike, it has been highlighted that the concept of moral injury refers to the challenge of knowing exactly what patients need in terms of care, but being unable to provide it due to constraints that remain beyond one’s control. Similarly, while exposure to traumatic events might be life-threatening for the person, when exposed to PMIEs a moral dissonance is experienced, whereby the person feels that their moral values and deeply held beliefs of right and wrong are challenged (Litz et al., 2009). As suggested by the growing evidence base and the evident conceptual appeal, MI is a useful construct especially in terms of capturing experiences of healthcare professionals who are seldom required to work under emergency circumstances. However, concerns have been raised regarding the clarity of the construct and its operationalisation in the healthcare setting (Čartolovni et al., 2021; Griffin et al., 2019), especially, considering the lack of validated instruments in this domain.
Initial evidence on MI experiences and symptoms among healthcare professionals during the COVID-19 pandemic has recently come from diverse country contexts including China (Zhizhong et al., 2020), the US (Hines et al., 2021), Canada (Berkhout et al., 2022), England (Hegarty et al., 2022), Romania (Maftei & Holman, 2021) and Israel (Zerach & Levi-Belz, 2021). Although several tools specific for healthcare settings that assessing exposure to and impact of MI are being developed (Mantri et al., 2020), the MIES scale originally created and tested on military personnel (Nash et al., 2013) remains the most used measure for assessing exposure and response to PMIEs across a variety of occupational categories including healthcare professionals (Hines et al., 2021; Maftei & Holman, 2021; Williamson et al., 2021). Notably, previous validation studies of the MIES yielded inconsistent factor structures, reflecting differential experiences of MI across professional groups, that may be related to differences in contexts, job roles and demographic profiles impacting the exposure to and experience of PMIEs (Bryan et al., 2016; Morris et al., 2022; Papazoglou et al., 2019; Plouffe et al., 2021; Richardson et al., 2020). For instance, the original Nash et al. (2013) study on military personnel identified a two-factor model of (1) ‘transgressions by self or others’ and (2) ‘betrayal by leaders’. However, Bryan et al. (2016) found an optimal fit using a three-factor structure representing ‘transgressions by others’, ‘transgressions by self’ and ‘betrayal by leaders’ among military personnel. More recently, Richardson et al. (2020) and Plouffe et al. (2021) found support for an alternative two-factor structure representing ‘transgressions and betrayals by others’ and ‘transgressions by self’ in the armed forces.
To our knowledge, only one study (Morris et al., 2022) has examined the MIES factor structure in a sample of professionals working in a healthcare setting, providing some support for the alternative two-factor model of ‘transgressions and betrayals by others’ and ‘transgressions by self’ (Plouffe et al., 2023; Richardson et al., 2020). Despite the recent explosion of studies using the MIES in healthcare settings, an investigation of psychometric properties of the scale amongst healthcare professionals active during the COVID-19 pandemic is currently lacking. Moreover, considering the ongoing debates about the MIES factor structure and its utility, an exploration of the psychometric properties of the Italian version of the scale with a sample of healthcare professionals engaged during the COVID-19 pandemic is relevant and timely. To our knowledge, this is the first study examining the psychometric properties of the Italian version of the MIES adapted for the healthcare setting in the context of a global pandemic. The aim of the present study was to provide an initial validation of the Italian version of the MIES adjusted to the healthcare setting, through the assessment of its factor structure and internal consistency. We also examine convergent and discriminant validity of the scale by determining whether the MIES is positively correlated with constructs that are associated with MI (e.g. depression, anxiety, PTSD, burnout symptomatology) and negatively correlated with constructs such as meaning in life and positive affect, in line with previous research (Nash et al., 2013). We also test the scale’s validity across separate groups of nurse professionals and female healthcare workers, who are considered as the most vulnerable to pandemic related distress (Smith et al., 2023).
2. Methods
2.1. Participants and procedure
Inclusion criteria were working as a professional nurse and/or as healthcare worker in a healthcare facility, in Italy. Data were collected via an online questionnaire distributed between April 2021 and June 2022, as the second wave of COVID-19 was spreading across European countries (Our World in Data, 2021). In Italy, the daily incidence of confirmed cases accelerated rapidly in April reaching a peak of 95 per 100,000 by mid-December and resulting in about 2.1 COVID-19-related deaths per 100,000 per day, a value greater than the first wave’s (1.35 per 100,000). A targeted recruitment strategy was employed including calls for participation published on healthcare institutions’ websites as well as on social media channels (i.e. WhatsApp groups of healthcare workers). While this strategy may have its limitations regarding the generalizability of results, it may represent an effective way of reaching difficult-to-reach groups, such as professional nurses working in healthcare facilities during a challenging period like that of COVID-19 pandemic. The online questionnaire did not include attention checks, which may represent a limitation, despite its completion did not require more than 15 min in order not to tax participants’ cognitive resources. Also, there was no possibility for an external verification of participants’ professional status beyond their self-reports.
Data were initially inspected and cleaned for entry errors, outliers, and missing values. Rows with more than 50% of missing values on the MIES scale were deleted. Of a total of 907 participants that responded to the call, 794 participants completed all measures and there were no missing data patterns. Hence, our final sample consisted of 794 participants (47% professional nurses, 51% female, age range 22–65 years old) that were included in the final analyses. Most of participants (92%) were active healthcare workers serving in healthcare facilities located in the Emilia-Romagna region of Italy, whereas the remaining part (0.8%) were based in northern, central, and southern regions of Lombardy, Lazio, and Campania. In terms of professional category, almost half of the sample (n = 371) identified as professional nurse (79% female and 21% male) whereas the remaining part identified as ‘Other’, including various professional categories such as medical doctors, social workers, radiologists, physiotherapists, rehabilitation specialists, obstetricians, oncologists, dieticians, etc. Half of our sample (N = 409) was composed of female healthcare workers, 71% of whom identified as nurses and the remaining part as belonging to other professional categories. The study was approved by the Ethical committee of the University of Bologna and all participants provided written informed consent.
2.2. Measures
Moral Injury was assessed using the Moral Injury Events Scale developed by Nash et al. (2013), which is an 11-item questionnaire tapping on exposure to (a) perceived transgressions referring to self (e.g. ‘I acted in ways that violated my own moral code or values’); (b) perceived transgressions of others (e.g. ‘I am troubled by having witnessed others’ immoral acts’); and (c) perceived betrayal by others (e.g. ‘I feel betrayed by fellow colleagues whom I once trusted’). Two additional items that measure trust in leaders and in one’s own moral integrity are included and are reverse scored. MIES items are scored on a 6-point Likert-type scale ranging from 1(strongly disagree) to 6 (strongly agree) and averaged such that higher mean scores represent greater intensity of event experiences. The measure was translated and back translated in accordance with gold standard translation practices (Bontempo, 1993) and discrepancies were rectified jointly by the research team and independent bilingual individuals experienced in working in healthcare (the Italian version of the MIES can be found at Supplementary Material S1). The items were adapted to tap on experiences of healthcare workers during the outbreak of the COVID-19.
We assessed depression symptoms with the Patient Health Questionnaire–9 (PHQ-9; Spitzer et al., 1999), which measures depressive symptoms in the last 14 days. Item responses were scored on a scale ranging from 1 (not at all) to 4 (nearly every day) and were summed, such that higher scores reflect greater depression symptom severity.
Anxiety symptoms were evaluated with the seven-item Generalised Anxiety Disorder Scale (GAD-7; Spitzer et al., 2006), which measures symptom severity over the past 14 days. Item responses are scored on a scale ranging from 1 (not at all) to 4 (nearly every day) and are summed with higher total scores representing more severe anxiety.
To assess PTSD symptom severity the 20-item PTSD Checklist for the DSM-5 (PCL-5; Weathers et al., 2013) was used. Responses were scored on a 5-point Likert scale ranging from 1 (not at all) to 5 (extremely) and were summed to create a total score, with higher values indicating greater PTSD symptom severity.
Symptoms of burnout were assessed through six items selected from the Copenhagen Psychosocial Questionnaire (COPSOQ, Kristensen et al., 2005). Participants responded to items on a 5-point scale ranging from 1 (to a very small extent) to 5 (to a very large extent). Responses were summed to create a total score, with higher scores representing greater burnout symptom severity.
Meaning in life was measured through the Meaning in Life Questionnaire (MLQ, Steger et al., 2006), which is a 10-item scale assessing how much respondents feel their lives have meaning and how much respondents strive to find meaning and understanding in their lives. Items are scored on a 6-point Likert-type scale ranging from 0 (I don’t agree) to 5 (I totally agree). A total score was derived from the sum of all items with higher values indicating higher levels of meaning in life.
We used five items from the Positive and Negative Affect Schedule (PANAS-SF, Watson et al., 1988) to assess positive affect. Participants responded to items on a scale ranging from 1 (not at all) to 7 (very much) and responses were averaged, such that higher mean scores reflect greater levels of positive affect.
2.3. Statistical analysis
Data analysis was performed in several steps. First, we assessed the psychometric properties of MIES, thus means, standard deviation, median, skewness, and kurtosis were calculated together with inter-item correlations. Second, the MIES factor structure was evaluated through confirmatory factor analysis conducted in Mplus with the Maximum likelihood with robust standard errors (MLR) estimator (Muthén & Muthén, 2017). Three separate models were tested: (a) the original two-factor model of Nash et al. (2013) with factors representing Perceived Transgressions (by self or others) and Perceived Betrayal by leaders; (b) the alternative two-factor model from Morris et al. (2022), with factors representing Transgressions by Self and Transgressions by Others (transgressions and betrayals); and (c) the three-factor model of Bryan et al. (2016) with factors representing Transgressions by Self, Transgressions by Others and Betrayal by Others. Model fit was evaluated using the chi-square test, root mean square error of approximation (RMSEA), comparative fit index (CFI), and Tucker–Lewis index (TLI). RMSEA values < .06 reflect good fit and values between .07 and .08 reflect satisfactory fit. CFI and TLI values between .90 and .95 reflect acceptable and above .95 reflect excellent fit (Perry et al., 2015). In addition, ESEM analyses were conducted using a multiple-groups procedure whereby analysis was performed on two further samples separately, one comprising nurse professionals and the other comprising female healthcare workers only. This approach is widely used for the measurement invariance testing of attitudinal measures (Brown, 2006). Last but not least, Cronbach’s alpha was used to assess the internal consistency of the scale and its subscales and convergent and discriminant validity was evaluated by determining if the MIES correlated positively with constructs associated with MI (e.g. depression, anxiety, PTSD, burnout symptomatology) and negatively with constructs such as meaning in life, positive affect.
3. Results
3.1. Preliminary analysis
Descriptive statistics of the MIES scale is reported in Table 1. To evaluate normality, skewness and kurtosis indices were investigated. As in the original study by Nash et al. (2013), we found low item-total correlations for item 10 and no correlation for item 11 (See Table 1). These results suggest that these items were not successfully measuring the same underlying global construct. Hence, they were excluded from further analyses for the same reasons reported by Nash et al. (2013).
Table 1.
The mean (SD), median, skewness, kurtosis, and item-total correlations (ITC) of MIES items.
| MIES items | Mean | SD | Median | Skewness | Kurtosis | ITC | |
|---|---|---|---|---|---|---|---|
| 1 | I saw things that were morally wrong. | 3.82 | 1.66 | 4.00 | −0.49 | −1.04 | .664** |
| 2 | I am troubled by having witnessed others’ immoral acts. | 3.18 | 1.85 | 3.00 | 0.08 | −1.50 | .720** |
| 3 | I acted in ways that violated my own moral code or values. | 2.47 | 1.70 | 2.00 | 0.73 | −0.91 | .756** |
| 4 | I am troubled by having acted in ways that violated my own morals or values. | 2.50 | 1.73 | 2.00 | 0.68 | −0.99 | .764** |
| 5 | I violated my own morals by failing to do something that I felt I should have done. | 2.50 | 1.75 | 2.00 | 0.66 | −1.05 | .776** |
| 6 | I am troubled because I violated my morals by failing to do something that I felt I should have done. | 2.91 | 1.85 | 2.00 | 0.33 | −1.40 | .704** |
| 7 | I feel betrayed by leaders who I once trusted. | 3.28 | 1.91 | 4.00 | 0.06 | −1.50 | .660** |
| 8 | I feel betrayed by fellow staff members who I once trusted. | 3.08 | 1.84 | 3.00 | 0.16 | −1.47 | .666** |
| 9 | I feel betrayed by others outside the health system who I once trusted. | 3.07 | 1.81 | 3.00 | 0.26 | −1.35 | .413** |
| 10 | I trust my leaders and fellow staff members to always live up to their core values. | 3.92 | 1.66 | 4.00 | −0.45 | −1.08 | −.289** |
| 11 | I trust myself to always live up to my own moral code. | 4.08 | 1.48 | 4.00 | −0.26 | −1.15 | −.058 |
3.2. The MIES factor structure
Given the inconsistent MIES factor structures yielded across studies on military and healthcare professional groups (Bryan et al., 2016; Morris et al., 2022; Nash et al., 2013; Plouffe et al., 2021; Richardson et al., 2020), three separate SEM models were investigated. The first model reflected the original two-factor structure found in Nash et al. (2013) with the factors ‘perceived transgressions by self and others’ and ‘perceived betrayal by others’. For the entire sample, fit indices indicated poor model fit: χ2(26) = 525.56, p < .001, RMSEA = 0.156 (90% CI [0.144 0.167]), CFI = 0.850, TLI = 0.792. The next model represented the alternative two-factor model with factors being ‘perceived transgressions by self’ and ‘perceived transgression and betrayal by others’, which had received support in prior studies with both military (Plouffe et al., 2021; Richardson et al., 2020) and healthcare personnel (Morris et al., 2022). The indices of model fit were also poor, χ2 (26) = 642.02, p < .001, RMSEA = 0.173 (90% CI [0.161 0.184]), CFI = 0.815, TLI = 0.744. Finally, we tested the three-factor model found by Bryan et al. (2016) among military forces, including ‘perceived transgressions by self’, ‘perceived transgression by others’ and ‘perceived betrayal’ as separate factors. The fit indices suggested an acceptable but not outstanding fit to the data, χ2(25) = 357.17, p < .001, CFI = 0.935, TLI = 0.907 (see Table 2). We retested the three SEM models with groups of professional nurses and female healthcare workers separately. Like the full sample, we found poor fit for the two-factor models and acceptable fit for the three-solution model across both groups (see Table 2).
Table 2.
SEM model assessment across samples.
| Model Type | χ2 | df | χ2/df | CFI | TLI | RMSEA | SRMR | AIC | BIC | aBIC |
|---|---|---|---|---|---|---|---|---|---|---|
| Total sample (n = 794) | ||||||||||
| Original 2 factor Model | 525.560 | 26 | 20.21 | 0.850 | 0.792 | 0.156 [0.144 0.167] | 0.069 | 25945.02 | 26075.98 | 25987.07 |
| Alternate 2 factor Model | 642.020 | 26 | 24.69 | 0.815 | 0.744 | 0.173 [0.161 0.184] | 0.080 | 24290.51 | 24420.9 | 24331.98 |
| The 3 factor Model | 357.175 | 25 | 14.28 | 0.935 | 0.907 | 0.129 [0.118 0.140] | 0.040 | 24134.60 | 24270.24 | 24178.15 |
| Professional Nurses (n = 371) | ||||||||||
| Original 2 factor Model | 418.622 | 26 | 16.10 | 0.813 | 0.741 | 0.202 [0.185 0.219] | 0.082 | 11671.77 | 11781.43 | 11692.59 |
| Alternate 2 factor Model | 460.126 | 26 | 17.69 | 0.793 | 0.713 | 0.212 [0.195 0.229] | 0.111 | 11713.28 | 11822.93 | 11734.09 |
| The 3 factor Model | 164.380 | 25 | 6.57 | 0.934 | 0.904 | 0.123 [0.105 0.141] | 0.046 | 11419.53 | 11533.10 | 11441.09 |
| Female HCW (n = 409) | ||||||||||
| Original 2 factor Model | 473.348 | 26 | 18.20 | 0.798 | 0.720 | 0.205 [0.189 0.221] | 0.084 | 13004.95 | 13117.33 | 13028.48 |
| Alternate 2 factor Model | 539.901 | 26 | 20.76 | 0.768 | 0.678 | 0.220 [0.204 0.236] | 0.117 | 13071.50 | 13183.89 | 13095.04 |
| The 3 factor Model | 165.097 | 25 | 6.60 | 0.937 | 0.909 | 0.117 [0.100 0.134] | 0.042 | 12698.70 | 12815.09 | 12723.07 |
Note: χ2: Chi Square; df: degrees of freedom; CFI: Comparative Fit Index; TLI: Tucker Lewis Index; RMSEA: Root Mean Square Error of Approximation; SRMR: Standardised Root Mean Square Residual; AIC: Akaike Information Criteria; BIC: Bayesian Information Criteria; aBIC: sample-size adjusted BIC; For TLI and CFI, values between .90 and .95 reflect acceptable fit and values ≥.95 indicates excellent fit; For SRMR and RMSEA, ≤.06 indicate good fit, ≤.08 indicates satisfactory fit.
To improve model fit, we followed best-practice recommendations on model modification (Cole et al., 2007; Nye, 2022; Nye et al., 2016), based on which correlation of measurement errors may be necessary and justified in CFA models, particularly when: (1) measures include similarly worded items (or synonym/antonyms) that are likely to share additional variance above and beyond that accounted for by the latent factor because the meaning, connotation, or interpretation of these items may be more similar than other items assessing the same construct; (2) they improve the fit of models that are well-grounded in preexisting theory; (3) they are kept at a minimum and (4) they are estimated on a large sample and/or cross-validated in separate samples. Based on these recommendations, we freed the residual correlation between two items with very close wording (MIES 5, ‘I violated my own morals by failing to do something that I felt I should have done’ and MIES 6, ‘I am troubled because I violated my morals by failing to do something that I felt I should have done’), which load on the same factor ‘Perceived transgressions by self’, and estimated the three models again for the entire sample and across samples of professional nurses and female healthcare workers separately.
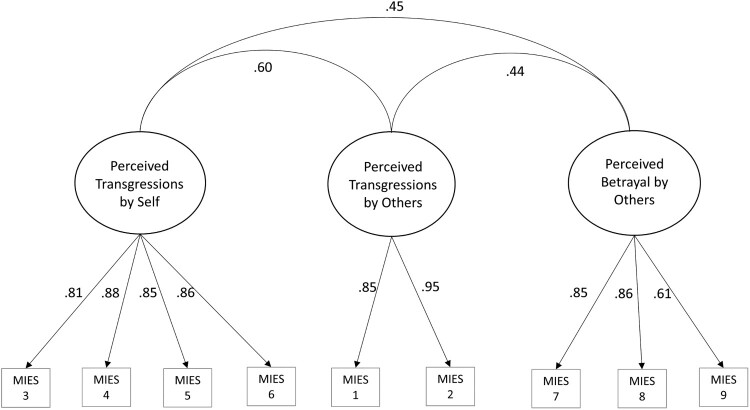
Results of the modified model estimated on the entire sample indicated an excellent model fit for the three-factor solution (χ2(24) = 89.554, p < .001, CFI = 0.980, TLI = 0.971), while two-factor models yielded poor fit indices (see Table 3). These results were replicated for models estimated separately on samples of nurse professionals and female health workers. The three-factor solution was thus confirmed with Factor 1 ‘perceived transgressions by others’ composed of items 1 and 2; Factor 2 ‘perceived transgressions by self’ composed of items 3–6; and Factor 3 ‘perceived betrayals by others’ composed of items 7–9. All factors had high item loadings (see Figure 1 for item loadings for each factor and factor correlation coefficients).
Table 3.
Modified SEM model assessment.
| Model Type | χ2 | df | χ2/df | CFI | TLI | RMSEA | SRMR | AIC | BIC | aBIC |
|---|---|---|---|---|---|---|---|---|---|---|
| Total sample (n = 794) | ||||||||||
| Original 2 factor Model | 533.563 | 25 | 21.34 | 0.848 | 0.782 | 0.160 [0.148 0.172] | 0.082 | 24469.51 | 24605.14 | 24513.05 |
| Alternate 2 factor Model | 746.273 | 25 | 29.85 | 0.785 | 0.690 | 0.191 [0.179 0.203] | 0.096 | 24619.75 | 24755.39 | 24331.98 |
| The 3 factor Model | 89.554 | 24 | 3.73 | 0.980 | 0.971 | 0.059 [ 0.046 0.072] | 0.043 | 23887.91 | 24028.23 | 23932.96 |
| Professional Nurses (n = 371) | ||||||||||
| Original 2 factor Model | 265.488 | 25 | 10.61 | 0.824 | 0.747 | 0.161 [0.144 0.179] | 0.081 | 11520.17 | 11633.74 | 11541.73 |
| Alternate 2 factor Model | 299.239 | 25 | 11.96 | 0.799 | 0.711 | 0.172 [0.155 0.190] | 0.112 | 11554.57 | 11668.14 | 11576.13 |
| The 3 factor Model | 60.082 | 24 | 2.50 | 0.974 | 0.960 | 0.064 [0.044 0.084] | 0.046 | 11254.64 | 11372.13 | 11276.94 |
| Female HCW (n = 409) | ||||||||||
| Original 2 factor Model | 305.877 | 25 | 12.23 | 0.811 | 0.727 | 0.166 [0.150 0.183] | 0.083 | 12836.07 | 12952.40 | 12860.38 |
| Alternate 2 factor Model | 346.203 | 25 | 13.84 | 0.783 | 0.688 | 0.177 [0.161 0.194] | 0.113 | 12873.69 | 12990.02 | 12897.99 |
| The 3 factor Model | 53.966 | 24 | 2.24 | 0.980 | 0.970 | 0.055 [0.036 0.075] | 0.042 | 12501.94 | 12622.27 | 12527.08 |
Note: Values in bold indicate adequate model fit. χ2: Chi Square; df: degrees of freedom; CFI: Comparative Fit Index; TLI: Tucker Lewis Index; RMSEA: Root Mean Square Error of Approximation; SRMR: Standardised Root Mean Square Residual; AIC: Akaike Information Criteria; BIC: Bayesian Information Criteria; aBIC: sample-size adjusted BIC; For TLI and CFI, values between .90 and .95 reflect acceptable fit and values ≥.95 indicates excellent fit; For SRMR and RMSEA, ≤.06 indicate good fit,≤.08 indicates satisfactory fit.
Figure 1.
MIES three-factor model for professionals in healthcare setting.
3.3. Internal consistency and construct validity
The internal consistency of the total MIES and individual subscales was high, with a Cronbach’s α ranging from .84 to .92 (see Table 4 for Cronbach’s α values of all measures). To assess construct validity, we examined the association of the MIES with the other measures included in the study. As expected, the MIES total score and each of the subscales were positively correlated with measures of depression (PHQ-9), anxiety (GAD-7), PTSD (PCL-5) and burnout symptoms (COPSOQ), all ps < 0.01 (see Table 4). Also, higher values on MIES total score and subscales were associated with lower values on the Meaning in Life scale (MIL) and positive affectivity, all ps < 0.01 (see Table 3).
Table 4.
Bivariate correlations between all study variables.
| M(SD) | α | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Total MIES | 3.9 (1.2) | 0.85 | 1 | ||||||||
| 2. Transgressions by self (MIES) | 4.4 (1.4) | 0.90 | .884** | 1 | |||||||
| 3. Transgressions by others (MIES) | 3.8 (1.4) | 0.92 | .755** | .568** | 1 | ||||||
| 4. Betrayal by others (MIES) | 3.9 (1.2) | 0.84 | .744** | .430** | .382** | 1 | |||||
| 5. Depression | 17.3 (4.7) | 0.87 | .328** | .251** | .242** | .301** | 1 | ||||
| 6. Anxiety | 14.2 (4.4) | 0.89 | .303** | .239** | .219** | .272** | .778** | 1 | |||
| 7. PTSD | 38.6 (14.4) | 0.94 | .341** | .272** | .237** | .308** | .715** | .753** | 1 | ||
| 8. Burnout | 15.7 (4.2) | 0.80 | .366** | .262** | .290** | .347** | .648** | .621** | .629** | 1 | |
| 9. Meaning in life | 46.6 (11.1) | 0.74 | −.132** | −.088* | −.098** | −.140** | −.255** | −.201** | −.170** | −.235** | 1 |
| 10. Positive affect | 3.9 (1.2) | 0.85 | −.246** | −.151** | −.161** | −.295** | −.493** | −.413** | −.385** | −.403** | .243** |
Note: *p < .05, **p < .01, ***p < .001.
4. Discussion
The focus of the present study was evaluating psychometric properties of the Italian version of the MIES adapted to the healthcare setting in a sample of active healthcare workers during the COVID-19 pandemic in Italy. This is the first study to assess the factor structure of the MIES in healthcare workers engaged in a global health emergency, providing a validation of the Italian version of the MIES.
Given the inconsistent results on the MIES factor structure found in previous research across different professional groups (Bryan et al., 2016; Morris et al., 2022; Nash et al., 2013; Richardson et al., 2020) proposing alternative two-and three-factor models, we tested three different models across the entire sample and separate groups composed of professional nurses and female healthcare workers respectively. The current study found an excellent fit for a three-factor solution, with high internal consistency of all factors. Factor 1 comprised four items related to ‘transgressions committed by the self’; Factor 2 comprised two items that reflected ‘transgressions committed by others’; and Factor 3 comprised three items reflecting ‘betrayal by others’ within and outside healthcare setting. Differently from the original two-factor structure of Nash et al. (2013) in which items were loaded onto two factors of ‘transgressions’ (by self and other) and ‘betrayal by others’, our findings offer support for a further differentiation between ‘transgressions of self’ and ‘transgressions by others’, consistent with the factor analysis of Bryan et al. (2016) on a sample of military personnel. The divergence from the Nash et al. (2013) model, regarding the further separation of a unified factor of transgressions into ‘transgressions of self’ and ‘transgressions of others’, is in line with psychometric research on alternative PMIE instruments, suggesting factor structures that also differentiate between transgressions commissioned by ‘self’ or witnessed transgressions by ‘others’ (Chaplo et al., 2019).
Our findings did not support the alternative two-factor model found recently by Morris et al. (2022) in a sample of healthcare workers which identified factors like ‘transgressions of self’ and ‘transgressions and betrayal of others’. Reasons for the divergencies in these models are likely to be complex and perhaps related to the differential exposure to and experience of PMIEs, which may be rooted in differences in setting and sample composition across these studies. For instance, differently from Morris et al. (2022) who examined experiences of healthcare professionals in a secure mental health setting, we examined exposure to PMIEs during the global COVID-19 pandemic in the hospital setting. The uniqueness of the moral challenges faced by healthcare workers engaged during the COVID-19 pandemic has been eloquently captured by a wealth of recent literature (Čartolovni et al., 2021; Riedel et al., 2022) describing the desolation of COVID-19 patients; the plight of family members concerned for their loved ones who may have no chance of receiving healthcare or proper burial practices; the distress of doctors and nurses exposed to such human suffering while no cure is available; the responsibility of difficult decision making and communicating bad news to patients and families. Such events impinge on one’s moral and ethical imperatives of care, fairness, respect for common norms/values, hence it is probable that the scale and nature of challenges faced by healthcare workers during the pandemic may account for the differences in our results. In particular, the evidence of a separate factor of ‘betrayal by others’ found in our study, may be attributed to the salience of trusting relationships with colleagues and senior reference figures in a health emergency context where tough decisions need to be made and communicated to patients and families. While experiences of healthcare workers in a secure mental health setting may be relatable, it can be argued that differences in the scope and intensity of exposure to PMIEs during a global pandemic may account for divergencies in the factor structure found across these two studies.
In addition, our samples differed in terms of size and professional categories included. For instance, the predominance of our participants identified as professional nurses (47%) compared to 28% in the study of Morris et al. (2022). It has been widely supported that amongst healthcare professionals, nurses have been the most affected by pandemic related distress (García-Fernández et al., 2020). Hence, differences in professional group representation may further account for differences in participants’ experiences leading to different factor structures found across these studies. The fact that we found further confirmation of the three-factor solution across separate groups of nurse professionals and female healthcare workers further supports the cross-validation of the three-factor structure of the MIES adapted to the hospital setting.
It should also be noted that what humans consider to be right or wrong (i.e. moral behaviour) varies from culture to culture, hence divergences in the factor structure of MIES as shown by existing research may be also attributed to socio-cultural differences across study populations. According to theoretical perspectives on morality (e.g. the Moral Foundations Theory; Graham et al., 2013; Haidt & Joseph, 2007), moral principles such as ‘care/harm’ or ‘fairness/justice’ are considered as ‘individualizing foundations’ since they are all relate to individual rights, whereas other moral principles such as showing loyalty to common values and respect for authority (i.e. moral foundations of ‘loyalty/betrayal’, ‘authority/subversion’) are defined as ‘socially binding foundations’ since they bind people together in groups and point at disapproval reactions to instances of unjustified breach of social norms on loyalty to common values or respected authority. From this perspective, it can be argued that existing differences in reported factor structures of the scale that may evidence (or not) a third separate factor related to ‘betrayal by others’ may be attributed to a certain extent to socio-cultural differences in terms of individualising or socially binding social and moral norms. It can also be speculated that a MI instrument which clearly identifies factors relating to transgressions of both individualising and socially binding moral norms may offer the most ecologically valid measure to use across different socio-cultural settings and professional categories. In this sense, compared to the alternative two-factor model by Morris et al. (2022) that conflates transgressions and betrayals by others in the same factor, the three-factor solution found in our study may offer the most ecologically valid model to capture MI experiences of healthcare workers. Furthermore, compared to the original two-factor model by Nash et al. (2013) in which transgressions by self and others load into the same factor ‘transgressions’, the three-factor solution found in our study, may be best set to capture fine grained differences in PMIEs referring to committed and witnessed transgressions, as reported by other studies (Chaplo et al., 2019).
Our results also showed that the MIES was internally consistent. Convergent validity was evaluated through correlations with PTSD, depression, anxiety, and burnout symptomatology. As anticipated, the MIES was correlated positively with these measures, which is in line with research demonstrating that individuals who have been exposed to PMIEs tend to experience adverse mental health outcomes (Bryan et al., 2018; Chaplo et al., 2019; Easterbrook et al., 2023). Although significant positive correlations with depression, anxiety, PTSD and burnout do suggest a certain level of convergence, it should be noted that they are somewhat low. This is in line with similarly low magnitude correlations between MIES and PTSD (range 0.28–0.41), anxiety (range 0.28–0.31) and depression (range 0.21–0.40) reported by previous validation studies (Nash et al., 2013; Plouffe et al., 2021; Zerach & Levi-Belz, 2021). This might speak towards a certain amount of variance uniquely explained by the construct of MI, which is likely to capture cognitive value judgements rather than manifest symptomatology. Alternatively, low correlations with psychological distress items might reflect a certain amount of resilience (i.e. exposure to transgressions might not necessarily lead to distress just as traumatic exposure does not evoke manifest symptoms in the majority of exposed subjects). Similarly, low range correlations with measures of meaning in life and positive affect seem to suggest a low level of divergence, as they do show significant negative associations, but are of small effect sizes. While low range negative correlations with positive affect and meaning in life measures are also in line with evidence from previous studies (see Nash et al., 2013), they might be explained by nurses experiencing their work as inherently meaningful during the pandemic, even though they might have had moral concerns regarding the implementation of pandemic-related measures. Other studies on frontline healthcare workers carried out during the pandemic (Berkhout et al., 2022; Fino et al., 2020; Fino, Fino, et al., 2021) have highlighted the importance of being helpful and responding to emotional needs of suffering patients and distressed family members as a protective factor against distress, while operating in a highly challenging emergency context marked by an unprecedented disbalance between needs and resources.
5. Conclusions
The present study suggests that the MIES can be useful to capture moral injury amongst healthcare workers engaged in global health emergency, albeit more studies may be needed to explore its appropriateness, and new tools putatively required to gain a more nuanced understanding of the experience of PMIEs amongst healthcare workers across different socio-cultural and professional settings. In particular, developing an understanding of the role of individualising and socially binding moral foundations in the experience of MI in the healthcare setting would be warranted. Such an understanding would be crucial to designing effective MI tools and to scaling up efforts to prevent its occurrence as well as mitigate its impact in the workplace.
Supplementary Material
Acknowledgements
We are grateful to all healthcare workers who participated in the study while being dedicated to delivering the highest quality care for all patients and families.
Funding Statement
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available on request from the first author [EF].
References
- Berkhout, S. G., Billings, J., Abou Seif, N., Singleton, D., Stein, H., Hegarty, S., Ondruskova, T., Soulios, E., Bloomfield, M. A. P., Greene, T., Seto, A., Abbey, S., & Sheehan, K. (2022). Shared sources and mechanisms of healthcare worker distress in COVID-19: A comparative qualitative study in Canada and the UK. European Journal of Psychotraumatology, 13(2), 2107810. 10.1080/20008066.2022.2107810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bontempo, R. (1993). Translation fidelity of psychological scales: An item response theory analysis of an individualism-collectivism scale. Journal of Cross-Cultural Psychology, 24(2), 149–166. 10.1177/0022022193242002 [DOI] [Google Scholar]
- Bordoagni, G., Fino, E., & Agostini, A. (2021). Burnout, attachment and mentalization in nursing students and nurse professionals. Healthcare, 9, 1576. 10.3390/healthcare9111576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, T. A. (2006). Confirmatory factor analysis for applied research. Guilford. [Google Scholar]
- Bryan, C. J., Bryan, A. O., Anestis, M. D., Anestis, J. C., Green, B. A., Etienne, N., Morrow, C. E., & Ray-Sannerud, B. (2016). Measuring moral injury: Psychometric properties of the Moral Injury Events Scale in two military samples. Assessment, 23(5), 557–570. 10.1177/1073191115590855 [DOI] [PubMed] [Google Scholar]
- Bryan, C. J., Bryan, A. O., Roberge, E., Leifker, F. R., & Rozek, D. C. (2018). Moral injury, posttraumatic stress disorder, and suicidal behavior among national guard personnel. Psychological Trauma: Theory, Research, Practice, and Policy, 10(1), 36–45. 10.1037/tra0000290 [DOI] [PubMed] [Google Scholar]
- Čartolovni, A., Stolt, M., Scott, P., & Suhonen, R. (2021). Moral injury in healthcare professionals: A scoping review and discussion. Nursing Ethics, 28(5), 590–602. 10.1177/0969733020966776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaplo, S. D., Kerig, P., & Wainryb, C. (2019). Development and validation of the moral injury scales for youth. Journal of Traumatic Stress, 32(3), 448–458. 10.1002/jts.22408 [DOI] [PubMed] [Google Scholar]
- Cole, D. A., Ciesla, J. A., & Steiger, J. H. (2007). The insidious effects of failing to include design-driven correlated residuals in latent-variable covariance structure analysis. Psychological Methods, 12(4), 381–398. 10.1037/1082-989X.12.4.381 [DOI] [PubMed] [Google Scholar]
- Dean, W., Talbot, S., & Dean, A. (2019). Reframing clinician distress: Moral injury not burnout. Federal Practitioner, 36(9), 400–402. [PMC free article] [PubMed] [Google Scholar]
- Easterbrook, B., Plouffe, R. A., Houle, S. A., Liu, A., McKinnon, M. C., Ashbaugh, A. R., Mota, N., Afifi, T. O., Enns, M. W., Richardson, J. D., & Nazarov, A. (2023). Moral injury associated with increased odds of past-year mental health disorders: A Canadian Armed Forces examination. European Journal of Psychotraumatology, 14(1), 1. 10.1080/20008066.2023.2192622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fino, E., Bonfrate, I., Fino, V., Bocus, P., Russo, P. M., & Mazzetti, M. (2021). Harnessing distress to boost growth in frontline healthcare workers during COVID-19 pandemic: The protective role of resilience, emotion regulation and social support. Psychological Medicine, 1–3. 10.1017/S0033291721000519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fino, E., Di Campli, S., Patrignani, G., & Mazzetti, M. (2019). The modulating role of gender and aggression in emotional reactions of nursing students: A cross-sectional study. Journal of Advanced Nursing, 75(7), 1462–1472. 10.1111/jan.13936 [DOI] [PubMed] [Google Scholar]
- Fino, E., Fino, V., Bonfrate, I., Russo, P. M., & Mazzetti, M. (2021). Helping patients connect remotely with their loved ones modulates distress in healthcare workers: Tend-and-befriend hypothesis for COVID-19 front liners. European Journal of Psychotraumatology, 12(1), 1968141. 10.1080/20008198.2021.1968141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fino, E., Fino, V., Mazzetti, M., & Russo, P. M. (2020). Tending and mending: Affiliative responses to the COVID-19 pandemic by healthcare professionals in Italy. Psychological Trauma: Theory, Research, Practice, and Policy, 12, S171–S173. 10.1037/tra0000827 [DOI] [PubMed] [Google Scholar]
- García-Fernández, L., Romero-Ferreiro, V., López-Roldán, P. D., Padilla, S., Calero-Sierra, I., Monzó-García, M., Pérez-Martín, J., & Rodriguez-Jimenez, R. (2020). Mental health impact of COVID-19 pandemic on Spanish healthcare workers. Psychological Medicine, 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham, J., Haidt, J., Koleva, S., Motyl, M., Iyer, R., Wojcik, S., & Ditto, P. H. (2013). Moral foundations theory: The pragmatic validity of moral pluralism. Advances in Experimental Social Psychology, 47, 55–130. 10.1016/B978-0-12-407236-7.00002-4 [DOI] [Google Scholar]
- Greenberg, N., Docherty, M., Gnanapragasam, S., & Wessely, S. (2020). Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ (Clinical Research Ed.), 368, m1211. 10.1136/bmj.m1211 [DOI] [PubMed] [Google Scholar]
- Griffin, B. J., Purcell, N., Burkman, K., Litz, B. T., Bryan, C. J., Schmitz, M., Villierme, C., Walsh, J., & Maguen, S. (2019). Moral injury: An integrative review. Journal of Traumatic Stress, 32(3), 350–362. 10.1002/jts.22362 [DOI] [PubMed] [Google Scholar]
- Haidt, J. (2008). Morality. Perspectives on Psychological Science, 3(1), 65–72. 10.1111/j.1745-6916.2008.00063.x [DOI] [PubMed] [Google Scholar]
- Haidt, J., & Joseph, C. (2007). The moral mind: How 5 sets of innate moral intuitions guide the development of many culture-specific virtues, and perhaps even modules. In Carruthers P., Laurence S., & Stich S. (Eds.), The innate mind (Vol. 3, pp. 367–391). Oxford University Press. [Google Scholar]
- Hegarty, S., Lamb, D., Stevelink, S. A. M., Bhundia, R., Raine, R., Doherty, M. J., Scott, H. R., Marie Rafferty, A., Williamson, V., Dorrington, S., Hotopf, M., Razavi, R., Greenberg, N., & Wessely, S. (2022). ‘It hurts your heart’: Frontline healthcare worker experiences of moral injury during the COVID-19 pandemic. European Journal of Psychotraumatology, 13(2), 2128028. 10.1080/20008066.2022.2128028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hines, S. E., Chin, K. H., Glick, D. R., & Wickwire, E. M. (2021). Trends in moral injury, distress, and resilience factors among healthcare workers at the beginning of the COVID-19 pandemic. International Journal of Environmental Research and Public Health, 18(2), 488. 10.3390/ijerph18020488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan, A. H., Eisen, E., Bolton, E., Nash, W. P., & Litz, B. T. (2017). Distinguishing war-related PTSD resulting from perpetration- and betrayal-based morally injurious events. Psychological Trauma: Theory, Research, Practice, and Policy, 9(6), 627–634. 10.1037/tra0000249 [DOI] [PubMed] [Google Scholar]
- Kristensen, T. S., Hannerz, H., Høgh, A., & Borg, V. (2005). The Copenhagen psychosocial questionnaire—a tool for the assessment and improvement of the psychosocial work environment. Scandinavian Journal of Work, Environment & Health, 31(6), 438–449. 10.5271/sjweh.948 [DOI] [PubMed] [Google Scholar]
- Litz, B. T., Stein, N., Delaney, E., Lebowitz, L., Nash, W. P., Silva, C., & Maguen, S. (2009). Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clinical Psychology Review, 29(8), 695–706. 10.1016/j.cpr.2009.07.003 [DOI] [PubMed] [Google Scholar]
- Maftei, A., & Holman, A. C. (2021). The prevalence of exposure to potentially morally injurious events among physicians during the COVID-19 pandemic. European Journal of Psychotraumatology, 12(1), 1898791. 10.1080/20008198.2021.1898791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantri, S., Lawson, J. M., Wang, Z., & Koenig, H. G. (2020). Identifying moral injury in healthcare professionals: The moral injury symptom Scale-HP. Journal of Religion and Health, 59(5), 2323–2340. 10.1007/s10943-020-01065-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molendijk, T. (2022). Warnings against romanticising moral injury. The British Journal of Psychiatry: The Journal of Mental Science, 220(1), 1–3. 10.1192/bjp.2021.114 [DOI] [PubMed] [Google Scholar]
- Morris, D. J., Webb, E. L., Trundle, G., & Caetano, G. (2022). Moral injury in secure mental healthcare: Part I: Exploratory and confirmatory factor analysis of the Moral Injury Events Scale. The Journal of Forensic Psychiatry & Psychology, doi: 10.1080/14789949.2022.2111318 [DOI] [Google Scholar]
- Murray, E., Krahé, C., & Goodsman, D. (2018). Are medical students in prehospital care at risk of moral injury? Emergency Medicine Journal, 35(10), 590–594. 10.1136/emermed-2017-207216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén, L. K., & Muthén, B. O. (2017). Mplus user’s guide (8th ed.). Muthén & Muthén. [Google Scholar]
- Nash, W. P., Marino Carper, T. L., Mills, M. A., Au, T., Goldsmith, A., & Litz, B. T. (2013). Psychometric evaluation of the Moral Injury Events Scale. Military Medicine, 178(6), 646–652. 10.7205/MILMED-D-13-00017 [DOI] [PubMed] [Google Scholar]
- Nye, C. D. (2022). Reviewer resources: Confirmatory factor analysis. Organizational Research Methods, 1–21. doi: 10.1177/10944281221120541 [DOI] [Google Scholar]
- Nye, C. D., Allemand, M., Gosling, S. D., Potter, J., & Roberts, B. W. (2016). Personality trait differences between young and middle-aged adults: Measurement artifacts or actual trends? Journal of Personality, 84(4), 473–492. [DOI] [PubMed] [Google Scholar]
- Papazoglou, K., Blumberg, D., Briones-Chiongbian, V., Russo, C., & Koskelainen, M. (2019). Exploring the roles of moral injury and personality in police traumatization. Crisis, Stress, and Human Resilience: An International Journal, 1(1), 32–56. [Google Scholar]
- Pappa, S., Ntella, V., Giannakas, T., Giannakoulis, V. G., Papoutsi, E., & Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain, Behavior, and Immunity, 88, 901–907. 10.1016/j.bbi.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry, J. L., Nicholls, A. R., Clough, P. J., & Crust, L. (2015). Assessing model fit: Caveats and recommendations for confirmatory factor analysis and exploratory structural equation modeling. Measurement in Physical Education and Exercise Science, 19(1), 12–21. 10.1080/1091367X.2014.952370 [DOI] [Google Scholar]
- Plouffe, R., Easterbrook, B., Liu, A., McKinnon, M., Richardson, J., & Nazarov, A. (2023). Psychometric evaluation of the Moral Injury Events Scale in two Canadian armed forces samples. Assessment, 30(1), 111–123. 10.1177/10731911211044198 [DOI] [PubMed] [Google Scholar]
- Richardson, C. B., Chesnut, R. P., Morgan, N. R., Bleser, J. A., Perkins, D. F., Vogt, D., Copeland, L. A., & Finley, E. (2020). Examining the factor structure of the Moral Injury Events Scale in a veteran sample. Military Medicine, 185(1–2), 75–83. [DOI] [PubMed] [Google Scholar]
- Riedel, P. L., Kreh, A., Kulcar, V., Lieber, A., & Juen, B. A. (2022). A scoping review of moral stressors, moral distress and moral injury in healthcare workers during COVID-19. International Journal of Environmental Research and Public Health, 19(3), 1666. 10.3390/ijerph19031666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, J., Korzuchowski, A., Memmott, C., Oveisi, N., Tan, H. L., & Morgan, R. (2023). Double distress: Women healthcare providers and moral distress during COVID-19. Nursing Ethics, 30(1), 46–57. 10.1177/09697330221114329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer, R. L., Kroenke, K., & Williams, J. B. (1999). Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA, 282, 1737–1744. [DOI] [PubMed] [Google Scholar]
- Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Steger, M. F., Frazier, P., Oishi, S., & Kaler, M. (2006). The meaning in life questionnaire: Assessing the presence of and search for meaning in life. Journal of Counseling Psychology, 53(1), 80–93. 10.1037/0022-0167.53.1.80 [DOI] [Google Scholar]
- Ter Heide, F. J. J., & Olff, M. (2023). Widening the scope: Defining and treating moral injury in diverse populations. European Journal of Psychotraumatology, 14(2), 2196899. 10.1080/20008066.2023.2196899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson, D., Clark, L. A., & Tellegen, A. (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. 10.1037/0022-3514.54.6.1063 [DOI] [PubMed] [Google Scholar]
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD checklist for DSM-5 (PCL-5) – standard [Measurement instrument]. https://www.ptsd.va.gov/
- Williamson, V., Murphy, D., Phelps, A., Forbes, D., & Greenberg, N. (2021). Moral injury: The effect on mental health and implications for treatment. The Lancet, 8(6), 453–454. [DOI] [PubMed] [Google Scholar]
- Zerach, G., & Levi-Belz, Y. (2021). Moral injury and mental health outcomes among Israeli health and social care workers during the COVID-19 pandemic: A latent class analysis approach. European Journal of Psychotraumatology, 12(1), 1945749. 10.1080/20008198.2021.1945749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhizhong, W., Koenig, H. G., Yan, T., Jing, W., Mu, S., Hongyu, L., & Guangtian, L. (2020). Psychometric properties of the moral injury symptom scale among Chinese health professionals during the COVID-19 pandemic. BMC Psychiatry, 20(1), 556. doi: 10.1186/s12888-020-02954-w [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available on request from the first author [EF].