Summary
The gut–liver axis plays a prominent role in the pathogenesis and therapy of metabolic diseases such as diabetes. The intestinal specific origin of several hormones that guide both inter- and post-prandial metabolism of carbohydrates and lipids, drives the attention of scientists and clinicians on the gut as a major site to intervene with novel diagnostic or prognostic markers. The role of intestinal ecology in the metabolic syndrome was postulated when gut microbiota was directly connected with inflammation, hyperinsulinemia, and diabetes. There have been several discoveries with the role of gut microbiota and gut–liver axis in diabetes. Also, there are several trials ongoing on the therapeutic efficacy of probiotic administration in diabetes and its complications. Here we point to the metabolic action of microbiota and discuss the actual state of the art on gut microbiota as a novel prognostic biomarker with a putative therapeutic role in diabetes.
Keywords: Fatty liver, Metabolic syndrome, Obesity, Prebiotics, Probiotics
Search strategy and selection criteria.
Preclinical and clinical studies for this review were identified by searches of PubMed, and references from relevant articles were found using the search terms “gut microbiota”, “diabetes”, “prebiotics” “probiotics”, “antidiabetic drugs”. We reviewed identified studies that reported the associations between Gut Microbiota and diabetes pathogenesis, as well as between gut microbiota and outcomes related to diabetes therapies. Abstracts and reports from meetings were included only when they related directly to previously published work. Only articles and/or reviews published in English for the past 20 years were included, and we also reviewed the references of all included papers and relevant reviews. To avoid data entry errors and to establish inter-rater reliability data extraction was performed by at least two authors.
Introduction
The gastrointestinal tract represents the widest and the most dynamic interface between our immune system and microorganisms, both pathogenic and symbiotic. The gut is populated by a very high number of commensal microorganisms such as bacteria, viruses, protozoa, and fungi, which constitute the gut microbiota (GM) and live in a sophisticated equilibrium with the host, from which they get energy through substrates provided by food. Diet and lifestyle, as well as drugs and toxic exposure, collectively called ‘exposome’, lead to inter-individual differences that may explain different responses to similar pathogenic stimuli, diet or medications, and diverse susceptibility toward a range of diseases. Indeed, on the one hand, the GM is fundamental for physiological metabolic processes, on the other hand, recent evidence suggests that alterations in its composition, termed dysbiosis, could be implicated in the pathogenesis of metabolic disorders, cardiovascular diseases, intestinal bowel diseases, and colorectal cancer. For these reasons, the scientific community is now focusing on the correlation between pathological conditions and dysbiosis, to discover whether it is biunivocal or causal, how genetics and environmental stimuli impact on its composition, or if the microbiota is able to influence susceptibility to diseases and responsiveness to a specific treatment. Consequently, the question is if individual microbiota fingerprint may bona fide accurately identify individuals with onset of diabetes and metabolic diseases, as well as predict the response to lifestyle and medical therapeutic interventions.
The metabolic action of gut microbiota
Recent data have updated the number of bacteria inhabiting the human body to 3·8·1013, a number of the same order of human cells. The vast majority is represented by Firmicutes (gram-positive) and Bacteroidetes (gram-negative), which respectively cover 60–80% and 20–30% of the whole GM, along with Proteobacteria and Actinobacteria.1 A high number of bacterial species in the microbiota has been shown to be a protective factor against metabolic diseases such as obesity, metabolic syndrome (MetS), and type-2 diabetes (T2D). Furthermore, in obese individuals, a lower microbial diversity, hence a lower metagenomic makeup, increases the risk of weight gain, adiposity, insulin resistance, and inflammation compared with those who show a higher number of genes.2
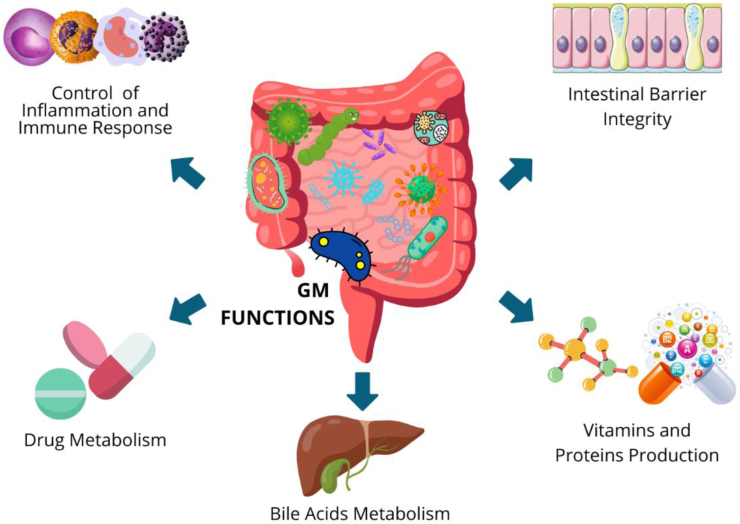
The GM is involved in the production of secondary bile acids (BAs)3 and protein catabolism, degradation of xenobiotics, production of water-soluble vitamins, but it is gaining relevance not only for its crucial role in the development and maintenance of proper functioning of innate and adaptive immunity and gut-associated lymphoid tissue (GALT), but also for its implication in the process of energy extraction from otherwise indigestible foods (Fig. 1).
Fig. 1.
Gut microbiota functions. The Gut microbiota is involved in the production of secondary bile acids (BAs) and protein catabolism, degradation of xenobiotics, production of water-soluble vitamins, in the control of inflammation and immune response, and in the maintenance of intestinal barrier integrity.
Indeed, GM makes possible intestinal plant fibers fermentation, leading to the production of short-chain fatty acids (SCFAs), such as butyrate, propionate, and acetate. SCFAS are peculiar metabolites involved in the physiological activity of colonic cells and in the regulation of appetite, insulin response, and inflammatory processes. Impaired SCFAs levels have been shown to be involved in the pathogenesis of metabolic, cardiovascular, and oncological diseases.4
Propionate and butyrate exert an anti-obesogenic action stimulating leptin and anorexigenic hormones synthesis5 while acetate predominantly presents obesogenic properties inducing ghrelin secretion and promoting fat storage.6 Emerging evidence from animal models and humans points to a reduction in butyrate-producing species, such as Faecalibacterium prausnitzii and Roseburia intestinalis, as one of the most important microbiota-related features responsible for the onset and development of T2D.7 Furthermore, mice treated with tributyrin, a butyrate precursor drug, displayed a protection from obesity, insulin resistance, and liver steatosis.8 Intriguingly, obese subjects treated with vancomycin, an antibiotic inhibiting the growth of butyrate-producers, steadily develop insulin resistance.9 On the other hand, a mice study observed that propionate induced the production of glucagon and fatty acid-binding protein 4 (FABP4) impairing insulin signaling10 and in humans promoted post-prandial increase of norepinephrine, glucagon, and FABP4 plasma levels, promoting insulin resistance.10
In eubiosis, Bacteroides vulgatus and Bacteroides dorei preserve the intestinal wall integrity by upregulating tight junctions expression, and reducing lipopolysaccharide (LPS) production.11 Akkermansia muciniphila has been shown to stimulate mucin production in mice, thereby contributing to strengthening the intestinal epithelial barrier, and thickening of the colonic mucus, increasing the physical distance between the intestinal epithelium and pathogens. Lactobacillus plantarum PS128 increases the level of mucins, too. Dysbiosis instead, contributes to increased intestinal permeability and consequent translocation of bacteria and bacterial LPS into the bloodstream. This process, also known as metabolic endotoxemia, has been proposed to explain the state of chronic low-grade inflammation involved in the pathogenesis of insulin resistance and MetS, major risk factors for the development of T2D and cancer.12
Gut microbiota in obesity and diabetes
Diabetic patients’ GM displays a prevalence of pathogenic and opportunistic gram-negative species at the expense of commensal ones. Indeed, an increase in pathogenic bacteria, such as Enterobacteriaceae, various Clostridiales, Escherichia coli, Bacteroides caccae, and Lactobacilli, as well as Prevotella copri and Bacteroides vulgates, have been found in the microbiota of diabetic patients. Bacteroidetes are gram negatives whose presence correlates with increased LPS, while their decrease is associated with lower metabolic endotoxemia and reduced inflammatory status as well as Proteobacteria are highly pro-inflammatory.13 It is well-known that this subclinical pro-inflammatory status due to LPS-dependent production of inflammatory cytokines, such as Interleukin-1 (IL-1), IL-6, and Tumour Necrosis Factor-α (TNF-α), drives the development of insulin resistance and T2D.
However, some conflicting evidence about the dysbiotic profile associated with diabetes and the relative abundance or reduction of certain genera suggests that these alterations are more species-specific than genus-specific and that the effect of individual strains is often enhanced when other species coexist in a kind of microbiotic cocktail. For instance, although Clostridium is usually considered as a pathogenic genus, some Clostridium species are essential for the hepatic BAs metabolism and for their synthesis from cholesterol. Among BAs main functions, their involvement in glucose metabolism and energy homeostasis is one of the most complex one. BAs encompass a range of different molecules, essential for lipophilic nutrient absorption and can be metabolized by specific intestinal microorganisms. Indeed, BAs deconjugation and biotransformation depend on species owning unique BA enzymatic activity, namely bile salt hydrolase activities [reviewed in3]. BAs themselves possess antimicrobial effects and act as ligands for FXR (Farnesoid X Receptor), a nuclear receptor involved in BAs homeostasis, carbohydrate metabolism, insulin response, and intestinal innate immune response.14 In the ileum, BAs-activated FXR primes a negative feedback mechanism inhibiting hepatic de novo synthesis of BAs, inhibiting gluconeogenesis, and activating glycogen-synthesis in the liver, increasing energy expenditure in muscle and brown adipose tissue, and inducing pancreatic beta cells to produce insulin.15 Thus, dysbiosis impairs BAs homeostasis and FXR activation causing loss of digestive, metabolic, and bacteriostatic control functions and leading to dyslipidaemia and chronic low-grade inflammation, which are peculiar features of the MetS, preluding to diabetes.15
The genus Lactobacillus has shown a positive association to T2D, although some species show anti-inflammatory properties. For instance, Lactobacillus induce the production of the anti-inflammatory IL-10, which improves insulin sensitivity in muscle, while inhibit proinflammatory cytokines IL-1β, Monocyte Chemoattractant Protein-1 (MCP-1), IL-8, Interferon-γ (IFN-γ), and C-reactive Protein synthesis. In addition, a clinical trial (IRCT2017082733941N5) showed that probiotic supplementation decreases insulin resistance by increasing pathways of glucose metabolism and insulin sensitivity beneficial effects on glycaemic control, HDL-cholesterol, total-/HDL-cholesterol ratio, biomarkers of inflammation and oxidative stress in diabetic patients.16 These results are very intriguing if one considers that low HDL-cholesterol is also a putative predictive marker of hepatocellular carcinoma in fatty liver and diabetes.17 Furthermore, although the Bacteroidetes to Firmicutes ratio has been a valid measure of dysbiosis status over the years, more recent studies and meta-analyses have questioned its tout-court utility in assessing the microbiota of diabetic subjects since, although a reduced ratio has been described in obese and metabolic subjects, its increase has instead been positively correlated with reduced glucidic tolerance [reviewed in18] (Table 1). Finally, in the assessment of specific characteristics of dysbiosis in diabetic disease, some contradictory results may also arise from the effects of antidiabetic therapy.
Table 1.
Gut microbiota in obesity and diabetes.
| Disease | Taxa features | Function features |
|---|---|---|
| Obesity (mouse and human studies) |
 Firmicutes:Bacteroidetes ratio Firmicutes:Bacteroidetes ratio |
More effective at extracting energy from nutrients breakdown |
| Diabetes (human study) |
 Enterobacteriaceae, Clostridiales, Escherichia coli, Bacteroides caccae Enterobacteriaceae, Clostridiales, Escherichia coli, Bacteroides caccae
|
pathogenic bacteria |
| Diabetes (human study) |
 Bacteroides vulgates Bacteroides vulgates |
 LPS LPS |
| Diabetes (human study) |
 Lactobacillus Lactobacillus |
 IL-10; IL-10; IL-1β, MCP-1, IL-8, IFN-γ, CRP IL-1β, MCP-1, IL-8, IFN-γ, CRP |
Abbreviations: LPS, lipopolysaccharides; IL-10, Interleukin-10; IL-1β, Interleukin-1β; MCP-1, Monocyte Chemoattractant Protein-1; IFN-γ, Interferon-γ; CRP, C-reactive Protein.
Gut microbiota as a predictor of diagnosis or biomarker of prognosis in diabetes
A specific gut metagenomic linkage group related to T2D risk was established and taxonomic analysis identified a list of microbial risk markers encompassing moderate dysbiosis, a decrease in butyrate producers, an increase in a range of opportunistic pathogens, an enrichment of microbial functions related to resistance to sulphate reduction and oxidative stress.19 Recent data have also strongly suggested that inter-individual variations in the GM may not only be predictive of disease development but also account for different responses to nutritional strategies. Precision nutrition studies are consistently showing that the GM composition of each individual is crucial for tailoring dietary advices for each patient, and that the observed inter-individual variability in postprandial blood glucose from the same meal may be attributed to differences in GM. The PREVIEW study, until now the largest intervention in overweight or obese adults with pre-diabetes undergoing an 8-week low energy diet (LED) for weight loss, showed that the decrease in body fat during the LED could be predicted by the baseline features of the GM.20 In another study, a high inter-individual variability in post-meal glucose that could be predicted by specific clinical and microbiome features was observed in a cohort of 800 people and further validated in an additional cohort of 100 people.21 Moreover, the PREDICT study has shown that the GM composition explains 7·5% of postprandial triglycerides levels, 6·4% of postprandial glycaemia and 5·8% of postprandial C-peptide, without adjusting for any other individual characteristics in over 1000 twins and unrelated individuals, and further validated in a US cohort of 100 people.22
While some microbes, such as Prevotella copri and Blastocystis spp., have been shown to be indicators of favourable postprandial glucose metabolism, overall microbiome composition seems to be predictive for a large panel of cardiometabolic blood markers including fasting and postprandial glycaemic, lipemic and inflammatory indices.23 Notably, when obese individuals are subjected to caloric restriction, insulin sensitivity appears to be better in those with a higher abundance of Akkermansia muciphila,24 as well as Parabacteroides distasonis has been associated with improved insulin sensitivity in obese human subjects.25
Gut microbiota and antidiabetic drugs
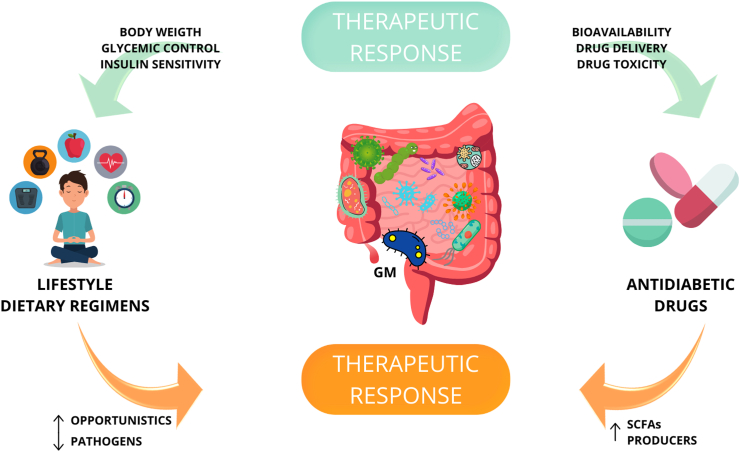
The therapeutic efficacy and potential side effects following the administration of antidiabetic drugs is also influenced by resident microbiota (Fig. 2) and the presence of certain genera/species could predict whether subjects will experience side effects as well response to probiotic supplementation. Orally administered drugs pass through the intestinal tract interacting with millions of resident microbes. A systematic analysis of 271 orally-administered drugs calculated that 66% are metabolized by at least one bacterial strain.26 Therefore, understanding this bidirectional interaction and how it affects clinical outcomes of antidiabetic drugs may pave the way for the development of innovative strategies for T2D treatment. Studies assessing whether and how antidiabetic drugs alter GM composition and which species are responsible for individual response to antidiabetic drugs are emerging.
Fig. 2.
Microbiota involvement in therapeutic response. Different individual susceptibility to a given pharmacological or nutritional strategy depends on microbiota composition. At the same time, lifestyle and dietary regimens, as well as some antidiabetics drugs, are responsible for modification in microbiota composition.
α-glucosidase inhibitors reduce postprandial hyperglycaemia inhibiting carbohydrate hydrolysis by binding to human intestinal maltase-glucoamylase and sucrase-isomaltase and may have beneficial effects on glycaemic control via GM. Do et al. demonstrated that voglibose administration decreased Firmicutes to Bacteroidetes ratio ameliorating blood glucose and lipid metabolism.27 In mice study, acarbose treatment promoted microbial shift increasing SCFAs concentration and the lifespan of the mice.28 Pre-diabetic patients treated with acarbose displayed Lactobacillus, Faecalibacterium, and Dialister up-regulation and Butyricicoccus, Phascolarctobacterium, and Ruminococcus reduction.29 Furthermore, in T2D patients, acarbose administration enhanced the presence of Bifidobacterium longum and reduced LPS levels.30
Several mice studies observed that GM regulated glucose homeostasis and satiety via GLP-1, an incretin hormone secreted by intestinal L cells.31 In line with this, GLP-1 receptor agonists, a class of antidiabetic drugs, are able to induce changes in the Firmicutes to Bacteroidetes ratio modifying the GM composition.32 In mice study, liraglutide administration promoted the expression of SCFAs-producing bacteria such as Bacteroides, Lachnospiraceae and Bifidobacterium.33 Furthermore, administration of liraglutide results in a reduction of Proteobacteria and an increase of Akkermansia muciniphila.34
Pioglitazone, a thiazolidinedione, as well as DPP-4 inhibitors, such as sitagliptin and vildagliptin, also show the ability to modulate GM.35 DPP-4 inhibitors reduce blood glucose blocking the degradation of GLP-1 and they restored the GM composition increasing the abundance of Bacteroidetes.36 In rats, the administration of sitagliptin increased Firmicutes and Tenericutes expression while vildagliptin treatment reduced Firmicutes to Bacteroidetes ratio and increased Lactobacilli spp. and propionate production.37
SGLT-2 inhibitors increase urinary glucose excretion to reduce plasma glucose. Several studies observed that SGLT-2 inhibitors did not produce changes in GM composition.38 Conversely, in diabetic mice, Lee et al. showed that dapagliflozin treatment reduced Firmicutes to Bacteroidetes ratio and Oscillospira, while increased Akkermansia muciniphila.39 However, further studies are needed to clarify the impact of SGLT-2 inhibitors on GM.
Gut microbiota and metformin
Metformin is the most studied antidiabetic oral drug. It is now well established that some of its therapeutic effects are mediated by the GM as confirmed by the reduced different antidiabetic effects achieved by its intravenous administration. Clostridium bartlettii, known to have a negative correlation with markers of insulin resistance, has been shown to have metformin-induced decreased abundance.40 Conversely, naïve T2D patients treated with metformin display an enrichment of Parabacteroides distasonis.25 Metformin has also been associated to the strengthening of tight junction. It has also been shown that the metformin-associated microbiota is more similar to healthy patients than untreated diabetics and there are indeed specific microbiotic clusters able to predict the efficacy of metformin therapy in diabetic patients: an increased presence of Prevotella copri appears to limit the ability of reducing glycated hemoglobin (HbA1c).41 Similarly, an increased presence of Streptococcus parasanguinis before starting antidiabetic treatment is predictive of metformin-associated side effects.42 Since this increase is associated with the use of proton pump inhibitors and anti-platelet therapy, data on the GM composition could also be key to understand how therapeutic failure or enhancement occur in patients on polypharmacological treatments.
Beside the influence of the GM on patients’ responsiveness when subjected to metformin treatment, data have consistently shown that metformin itself alters the GM composition. increasing Enterobacteriales and Akkermansia muciniphila.43 A randomized controlled trial (RCT) study reported that metformin increases Escherichia coli and Ruminococcus torques while decreases the relative abundance of Intestinibacter bartlettii and Roseburia intestinalis at 6th and 12th months in overweight and obese cancer survivors, respectively.44 Metagenomic shotgun sequencing revealed that metformin treatment in combination with a hypocaloric diet induces significant changes in the relative abundance of over 80 bacterial strains, especially belonging to Firmicutes and Proteobacteria, compared to the placebo group.40 Moreover, in diabetic patients subjected to metformin treatment an enrichment in Escherichia40 and Akkermansia muciniphila,40 with a reduction in Intestinibacter were observed compared to naïve patients. An enrichment of Enterobacteriaceae, such as Salmonella, Klebsiella, Shigella and Escherichia, were found in two independent T2D cohort of European women7 and Nordic/Scandinavian45 patients treated with metformin, while Clostridium and Eubacterium relative abundance was lower.7 In another cohort of Colombian patients, metformin significantly enriched the Prevotella and Megasphaera genus while reducing Clostridiaceae 02d06, Oscillospira and Barnesiellaceae46 In a small Japanese cohort of T2D patients on metformin, no changes in relative abundance were observed and this was probably due to the short term metformin treatment before metagenomic analysis; however, Bacteroides and Escherichia positively correlated with metformin treatment while a negative correlation was observed with Faecalibacterium and Ruminocococus.47 Several mechanisms have been hypothesized linking metformin action on the GM and the improvement of glucose tolerance. In line with studies reporting the higher abundance of Akkermansia,40,46 it has been shown that metformin use was functionally associated with a higher production of SCFAs.40,45,48
These data, together with the fact that metformin itself is able to strengthen the intestinal barrier and decrease LPS translocation by enhancing the intestinal expression of TJ proteins, indicate that metformin indirectly ameliorates insulin resistance also by modulating GM composition, SCFAs levels, improving the intestinal barrier integrity. Intriguingly, in a murine model of obstructed BA flow, FXR activation by the novel ligand TC-100, prevents intestinal mucosal damage and is associated with an enrichment of Akkermansia muciniphila,49 suggesting once again that intestinal barrier preservation plays a more general metabolic role controlling intestinal inflammation that could likely be extended to the management of adiposopathy, chronic low grade systemic inflammation and, finally, glucose tolerance.
Functionally, metformin therapy has been also associated with higher levels of serum BAs compared to placebo, displaying a significant negative correlation with HbA1c.40 Several studies have shown the important role that FXR plays in suppressing bacterial overgrowth in the ileum14 and preserving the intestinal barrier integrity also via modulating the GM composition in different experimental conditions.49,50 Moreover, an in vivo experiment using an intestinal agonist for FXR resulted in GLP-1 secretion, intestinal microbial shift, and improved glucose tolerance in mice.51 Unfortunately, these effects were reversed by antibiotic treatment,51 suggesting GM involvement. However, effects of FXR activation are controversial. Firstly, future studies will eventually highlight the role that the FXR-target enterokine fibroblast growth factor 19 (FGF19) and its sister hormone FGF21 would directly play in GM composition given their relevant endocrine actions in obesity and lipid/glucose metabolism.52, 53, 54 Second, in vivo and human data have shown that metformin can inhibit BA intestinal reuptake, most probably through the inhibition of the apical sodium-dependent bile acid transporter (ASBT). This results in an increased intestinal BAs pool, which has been associated with the inhibition of the BA-dependent FXR control of BA homeostasis, and an increased activation of the luminal TGR5 pathway, thereby resulting in GLP-1 secretion, regulating glucose metabolism. Lastly, metagenomic and meta-metabolomic analysis have shown that metformin increases the intestinal level of glycoursodeoxycholic acid while decreases the abundance of species of Bacteroides fragilis and, consequently, bile salt hydrolase activity in the intestine of individuals with T2D.55
Unfortunately, if some of the beneficial effects of metformin on glucose metabolism are mediated by the GM, also some of its side effects may be due to GM alterations. For example, excess in metformin-induced Escherichia enrichment may result in abdominal discomfort,56 resembling symptoms associated to irritable bowel syndrome. On a different angle, modulation of GM composition via probiotics directly influences FXR transcriptional actions in the gut–liver axis.57 Furthermore, when metformin was used in healthy subjects without changes in glycaemic homeostasis, it was associated to an enrichment of Escherichia, Shigella spp., and Bilophila wadsworthia, together with a decrease in Clostridium spp. and Intestinibacter spp.,58 indicating that GM composition shift was ascribable to metformin itself, rather than merely reflecting effects on glucose homeostasis.
The therapeutic value of harnessing gut microbiota
Gut microbiota and lifestyle
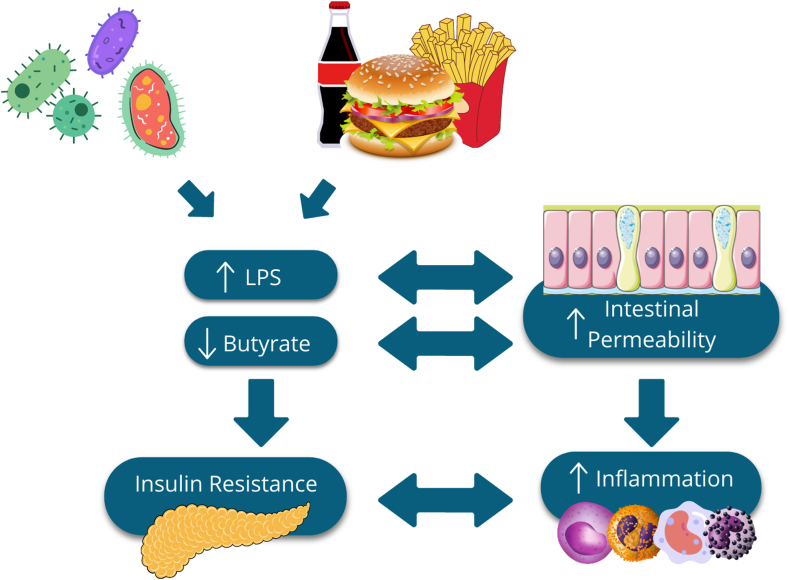
A cornerstone of the antidiabetic strategy recommends combining drugs with a healthier diet and a less sedentary lifestyle. In clinical practice, when suggesting these nonpharmacological strategies, perhaps still unconsciously, one is already attempting a shaping of the GM that could enhance the therapeutic effects of the drugs. Arumugam et al.59 postulated the existence of three different microbiota enterotypes characterized by different species composition and specifically by an enrichment of Bacteroides, Prevotella, and Ruminococcus, respectively. Each enterotype has been associated to a specific dietary regimen: the first one appears to be related to Western diet, a high saturated fat diet, correlated with higher inflammatory profile, blood LPS levels and endotoxemia, and lower species diversity of microbiota, features also found in overweight and obese subjects. In contrast, a Mediterranean-type diet, low in saturated fatty acids (FAs) and refined sugars but rich in fibers and unsaturated FAs, has been associated to enterotype II and has been shown to positively modulate the microbiota, providing protection toward MetS, T2D, cardiovascular diseases and cancer60; dietary fibers reduce intestinal permeability and consequently the pro-inflammatory state associated with endotoxemia (Fig. 3). Furthermore, since fibers intake is associated with increased butyrate production, this mechanism could probably explain the preventive effect of a fiber-rich Mediterranean diet. Finally, the third cluster is less frequent in the population and less constant in its composition and is not so closely associated with a specific dietary profile. Although the multitude of associations to different clinical conditions does not make enterotype classification sufficiently specific as a standalone diagnostic marker of any disease, the different efficacy achieved by a given nutritional intervention in different enterotypes confirms the hypothesis that everyone should be offered a personalized strategy, ‘tailor-made’ according to the composition of her/his microbiota.
Fig. 3.
Dysbiosis in Diabetes Pathogenesis. Increase in Gram negative species and high-fat diet led to translocation of bacterial lipopolysaccharide (LPS) into the bloodstream. In diabetics also a reduction in butyrate producer species is observed. These are the main consequences of diabetes-associated dysbiosis, that affect gut wall integrity, leading to endotoxemia and chronic inflammation. Reduction in butyrate level also leads to insulin resistance because of a reduction in Glucagon-like peptide-1 (GLP-1) pathway activation, in fatty acids oxidation, and in thermogenetic energy expenditure. Insulin resistance and chronic inflammation self-feed, worsening dysbiosis and accelerating diabetes clinical progression, with nerves and vessels involvement that also affects the intestinal epithelium.
Also, physical activity could influence the composition of the GM. High intensity training negatively affects the digestive system, causing dysbiosis and “exercise-induced gastrointestinal syndrome”. Conversely, moderate-intensity exercise does not affect the diversity of the GM but beneficially impacts on its composition, increasing the relative abundance of Akkermansia muciniphila and Oscillospira, with an increase in SCFAs and lactic acid-production.61
Diabetes and prebiotic and probiotic administration
Beside the above-mentioned shift in GM composition due to antidiabetic drug administration, several studies have focused on the probiotics administration as adjuvant strategies to improve insulin sensitivity. Moreover, side effects of probiotics are minimal and do not affect therapeutic adherence.62 Probiotics reshape the GM composition through a multilevel action, including, but not limited to, the inhibition of alpha–glucosidase activity, lactic acid production, strengthening of the intestinal barrier, immune-modulation, SCFAs production, and regulation of BAs metabolism.35 Treatment with probiotics, in particular some Lactobacillus and Bifidobacterium strains, can also improve lipid profile and reduce fasting glycaemia, insulinemia, and HbA1c levels.63 Administration of Akkermansia muciniphila has also been proposed as an antidiabetic strategy in light of its ability to regenerate the intestinal barrier, reduce inflammation, and improve metabolic processes.64
Beside a considerable number of studies on the effects of individual strains administration in diabetic patients, the administration of a cocktail of probiotics has been shown to be more effective in improving fasting plasma glucose and oxidative stress.65 Anyhow, although data from murine models have largely shown beneficial effects, the administration of probiotics in humans seems less impactful on glycaemic control, especially when compared to the gold standard anti-diabetic therapies, suggesting that this strategy only can be adjuvant and not curative itself.
Among the most studied prebiotics, there are complex carbohydrates, polyphenols, and polyunsaturated FAs, which increase stool consistency and can be fermented to SCFAs. For example, oligo-fructose has shown positive effects on glucose homeostasis, inflammation and leptin sensitivity, GLP-1 production, intestinal epithelial integrity.15 Berberine, resveratrol, alliin, capsaicin, betacyanin, and cranberry proanthocyanins have also shown antidiabetic effects.35 The ability of prebiotics in potentiate drug therapy has been widely demonstrated, and therefore, combining drug therapy with prebiotics and probiotics could significantly improve hyperglycaemia and obesity.66 Also in this field, enterotypes may be used in the prediction of therapeutic success. Enterotype 1 (Bacteroides) seems to better respond to the intake of capsaicin, a prebiotic found in chili peppers, that has shown positive effects in controlling obesity, cardiovascular diseases, and cancer while arabinoxylan, a hemicellulose recently proposed as a prebiotic, shows its protection toward weight gain only in subjects with a high pre-treatment Prevotella:Bacteroides ratio.67
Diabetes and fecal microbiota transplantation (FMT)
Another strategy to harness the microbiota as an adjuvant strategy in the treatment of diabetes is FMT, also known as stool transplantation: the transfer of stools from a healthy donor into another subject’s gastrointestinal tract, aiming to change the recipient’s GM gaining health benefit.68 For instance, FMT is currently one of the most successful therapy for recurrent and refractory Clostridium Difficile Infection (CDI),69 even in immunodepressed70 or with underlying comorbidities patients. Given its successful exploitation, researcher and clinicians are considering its potential beyond the application in CDI, to treat other medical conditions implying dysbiosis. Emerging evidence is consistently showing that FMT may not only improve insulin sensitivity, but also alter the natural course of type I diabetes by modulating autoimmunity. Plenty of preclinical data have been published in the last years and, despite model-related difference, have consistently shown the advantage of FMT in the improvement of insulin resistance, weight gain, cardio metabolism, and liver steatosis.
Human data are finally becoming available and confirming the enormous amount of pre-clinical data publish in the last decade. A recent study compared the effects of FMT from donors who underwent bariatric surgery and donors with MetS. While a reduction in inflammatory indices was observed in the recipients from bariatric patients, a decrease in insulin sensitivity and an increase in secondary BAs was displayed in those transplanted from metabolic patients,71 highlighting the fact that different conditions may benefit in different way from FTM. Currently, several Phase 1 and 2 clinical trials are studying how harnessing the microbiota could benefit patients affected by obesity, T2D and MetS (Table 2). The field is eagerly awaiting results, but the published results so far are promising. A study published in the 2019 (NCT01765517) has shown the benefit of a multi-strain probiotic supplementation over 6 months as a monotherapy in decreasing HOMA-IR in T2D patients.72 Another study (NCT03100162) has shown the beneficial dose-dependent effects of a lyophilizate powder containing live multispecies probiotic bacteria on cardiometabolic parameters and gut permeability of obese post-menopausal women.73 As demonstrated by other studies showing only a modest effect of GM manipulation on insulin resistance in T2D,74 it is clear now that success of microbial modulation depends on the tested strains, on its composition and diversity, on the patients pre-existing microbial diversity and his genetic fingerprint. However, there are some risks related to FMT that should be taken into account. Major concerns regard the transfer of infectious disease or the promotion of dysbiotic status which could promote the development of disorders linked to GM. Furthermore, in 2016, two cases of peripheral neuropathy have been correlated to FMT.75
Table 2.
Diabetes and probiotic clinical trials.
| Trial identifier | Trail phase (status) | Title | Conditions | Interventions |
|---|---|---|---|---|
| Diabetes Mellitus type 2 | ||||
| NCT01765517 | Completed | Study to Explore the Effects of Probiotics on Endotoxin Levels in Type 2 Diabetes Mellitus Patients | Diabetes Mellitus Type 2 |
|
| NCT02728414 | Unknown | Probiotics Effect on Glucose and Lipid Metabolism and Gut Microbiota in Patients With Type 2 Diabetes | Diabetes Mellitus, Type 2 |
|
| NCT03377946 | Unknown | Effect of Probiotics on Pre-diabetes and Diabetes in China | Diabetes Mellitus, Type 2 |
|
| NCT04089280 | Completed | Probiotics in Metformin Intolerant Patients With Type 2 Diabetes |
|
|
| NCT05418179 | Recruiting | Effect of Probiotic Supplementation on Fecal Microbiota, Nutritional Status, Metabolic and Inflammatory Parameters in Patients With Type 2 Diabetes Mellitus | Type 2 Diabetes Mellitus |
|
| NCT04988594 | Completed | Effects of Yogurt With Probiotics in Adults With Type 2 Diabetes Mellitus | Type 2 Diabetes |
|
| NCT05066152 | Completed | The Effect of Single Probiotic on Metabolic Control in Type 2 Diabetes | Type 2 Diabetes |
|
| NCT03434860 | Completed | Effect of Probiotic on Insulin Resistance in Type 2 Diabetes Patients |
|
|
| NCT04191525 | Completed | Phase II Clinical Trial to Evaluate the Efficacy and Safety of the Treatment With BPL-1 in Adult Patients With Type 2 Diabetes Mellitus | Type 2 Diabetes |
|
| NCT01250106 | Unknown | Probiotics as a Novel Approach to Modulate Gut Hormone Secretion and Risk Factors of Type 2 Diabetes and Complications |
|
Dietary Supplement: Lactobacillus reuteri |
| NCT03239366 | Unknown | A Study to Evaluate the Effect of BioK+ 50B® on Glycemic Control in a Type 2 Diabetes Population | Type 2 Diabetes |
|
| NCT00413348 | Unknown | Type 2 Diabetes and the Effect of Probiotics |
|
|
| NCT01620125 | Completed | Metabolic Control Before and After Supplementation With Lactobacillus Reuteri DSM 17938 in Type 2 Diabetes Patients |
|
Dietary Supplement: Lactobacillus reuteri DSM 17938 |
| NCT01752803 | Unknown | RCT Examining Effects of Probiotics in T2DM Individuals |
|
|
| NCT00699426 | Completed | The Effect of Nexium and Probiotics on Insulin Secretion and Cardiovascular Risk Factors in Patients With Type 2 Diabetes | Type 2 Diabetes |
|
| NCT02274272 | Completed | Effects of Genmont Probiotic on Improve the Level of Blood Glucose and Other Diabetic Associate Parameter in Type 2 Diabetes Patients | Type 2 Diabetes |
|
| NCT04296825 | Completed | Effect of Camel Milk With Probiotic on Type 2 Diabetes Mellitus | Type 2 Diabetes |
|
| NCT04201938 | Completed | Effect of Probiotic Co-administration With Omega-3 Fatty Acids on Obesity Parameters and Insulin Resistance |
|
|
| NCT05076656 | Completed | Epigenetic and Microbiota Modifications |
|
|
| NCT02469558 | Completed | Probiotics in Diabesity: A Pilot Study |
|
|
| NCT02144948 | Completed | Investigation of the Effect of E.-Coli-Nissle as Supporting Therapy to Standard Care of Diabetes Mellitus Type II | Diabetes type 2 | Drug: e.-coli-nissle |
| NCT01836796 | Completed | Metabolic Effects of Lactobacillus Reuteri DSM 17938 in Type 2 Diabetes | Diabetes type 2 |
|
| NCT00068094 | Terminated | The Effect of Good Bacteria on Nonalcoholic Fatty Liver Disease in Diabetics |
|
Drug: Probiotic-containing powde |
| NCT03037918 | Completed | Effect of Yakult Ingestion on Diet-induced Insulin Resistance in Humans |
|
Dietary Supplement: Yakult light |
| NCT01235026 | Unknown | Synbiotics and Low Grade Inflammation in Obese Subjects |
|
|
| NCT00655798 | Completed | Effect of Nutritional Interventions on Inflammatory Status in Healthy Overweight Men |
|
|
| NCT04767789 | Active, not recruiting | Clinical Trial to Evaluate the Efficacy and Safety of the Probiotic Strains Limosilactocillus Reuteri DSM 32910 and Lacticaseibacillus Paracasei DSM 32851 on Glucose Homeostatis in Prediabetic Adults |
|
|
| NCT04341571 | Active, not recruiting | Effect of Probiotics vs Metformin on Glycemic Control, Insulin Sensitivity and Insulin Secretion in Prediabetes. |
|
|
| NCT04428606 | Completed | Study to Determine the Effect of Synbiotics in Patients With Pre-diabetes | PreDiabetes |
|
| NCT04863313 | Recruiting | Effect of a Probiotic on the Glycemic Profile and the Fecal Microbiota of Prediabetic Subjects (PREDIABETCARE) |
|
|
| Diabetes Mellitus type 1 | ||||
| NCT04579341 | Recruiting | Probiotics Supplementation Effect on Glucose Homeostasis in Children With Type 1 Diabetes | Diabetes Mellitus, Type 1 | Dietary Supplement: Probiotics |
| NCT03880760 | Completed | The Effect of Probiotics on Type 1 Diabetes Mellitus in Children | Diabetes Mellitus, Type 1 |
|
| NCT03032354 | Unknown | Probiotics in Newly Recognized Type 1 Diabetes | Diabetes Mellitus, Type 1 |
|
| NCT03423589 | Completed | Modulation of Type 1 Diabetes Susceptibility Through the Use of Probiotics | Diabetes Mellitus, Type 1 | Dietary Supplement: VSL#3 |
| NCT03556631 | Completed | Effect of Live Combined Bifidobacterium and Lactobacillus on Glycemic Control and Other Outcomes in Type 1 Diabetes | Diabetes Mellitus, Type 1 | Drug: live combined Bifidobacterium and Lactobacillus Tablets |
| NCT04141761 | Active, not recruiting | Probiotics in Newly Diagnosed T1D | Type 1 Diabetes Mellitus |
|
| NCT03961347 | Recruiting | Lactobacillus Johnsonii Supplementation in Adults With T1D | Type 1 Diabetes Mellitus |
|
| NCT04335656 | Recruiting | Reducing Innate Inflammation in New Onset Type 1 Diabetes | Type 1 Diabetes Mellitus |
|
| NCT03961854 | Recruiting | Lactobacillus Johnsonii in Children and Adolescents With T1D | Type 1 Diabetes Mellitus |
|
| NCT04769037 | Recruiting | Supplementation With B. Infantis for Mitigation of Type 1 Diabetes Autoimmunity | Type 1 Diabetes Mellitus |
|
Conclusions
In this narrative review, we discussed the potential of the GM manipulation in diabesity focusing on the comprehension of the metabolic action of GM. The role of intestinal ecology in the metabolic syndrome has been recently postulated for the connection between GM with inflammation, hyperinsulinemia, metabolic-associated fatty liver disease (MAFLD) and diabetes. There have been several discoveries on GM and gut–liver axis modulation in diabetes. Also, there are several trials ongoing on the therapeutic efficacy of probiotic administration in diabetes and its complications. We pointed to GM as a novel prognostic biomarker in diabetes and proposed the need of further future studies to depict a final scenario for the putative therapeutic role of GM modulation with prebiotics and probiotics in diabetes and MAFLD.
Outstanding questions
The mechanisms through which intestinal dysbiosis is associated with diabetes development or a poorer prognosis are intriguing. Despite the increasing need of larger-scale studies to postulate personalized approaches to patients, studying GM appears increasingly useful in understanding the variable risk of onset of metabolic diseases even when subjects make similar lifestyle choices. Harnessing the microbiota may represent a valuable tool for restoring eubiosis in dysmetabolic individuals and as an adjuvant approach to ameliorate response to pharmacological treatment and improve patients' compliance through the reduction of drugs' side effects. Several clinical trials are ongoing to reveal a role for prebiotics and/or probiotics administration in diabetes. However, more RCT studies focusing on GM should be carried out, for a range of reasons: biomarker discovery, identification of responder’s vs non-responders, overcoming the pitfalls currently characterizing pharmacological GM modulation, protocol standardization, evaluation of side effects. This novel approach could contribute to design a stronger strategy for personalized medicine in diabetes.
Contributors
Conceptualisation, A.M. and L.C; literature search, L.C., R.M.G and M.C; writing—original draft preparation, L.C. and R.M.G.; figures, L.C and R.M.G.; writing-review & editing: M.C. and A.M; funding acquisition, L.C., R.M.G. and A.M. M.C. and A.M. directly accessed and verified the underlying data reported in the manuscript. All authors have read and agreed to the published version of the manuscript.
Declaration of interests
All authors have nothing to disclosure.
Acknowledgements
Development of this manuscript was supported by funding received from the authors. A.M. is funded by National Recovery and Resilience Plan (NRRP), Mission 4 Component 2 Investment 1.3–Call for tender No. 341 of 15 March 2022 of Italian Ministry of University and Research funded by the European Union—NextGeneration EU; Project code PE00000003, Concession Decree No. 1550 of 11 October 2022 adopted by the Italian Ministry of University and Research, CUP D93C22000890001, Project title “ON Foods–Research and innovation network on food and nutrition Sustainability, Safety and Security—Working ON Foods”. L.C. is funded under the National Recovery and Resilience Plan (NRRP), Mission 4 Component 2 Investment 1.3–Call for tender No. 341 of 15 March 2022 of Italian Ministry of University and Research funded by the European Union—NextGeneration EU; Award Number: Project code PE0000015, Concession Decree No. 1243 of 2 August 2022 adopted by the Italian Ministry of University and Research, CUP H33C22000680006, Project title “Ageing well in an ageing society–A novel public-private alliance to generate socioeconomic, biomedical and technological solutions for an inclusive Italian ageing society– AGE-IT”. R.M.G. is funded by PON “RICERCA E INNOVAZIONE” 2014–2020–Innovazione (D.M. 10 AGOSTO 2021, N. 1062). The funders had no role in paper design, data collection, data analysis, interpretation, writing of the paper.
A special thanks to Roberta Le Donne for her support.
References
- 1.Pitocco D., Di Leo M., Tartaglione L., et al. The role of gut microbiota in mediating obesity and diabetes mellitus. Eur Rev Med Pharmacol Sci. 2020;24(3):1548–1562. doi: 10.26355/eurrev_202002_20213. [DOI] [PubMed] [Google Scholar]
- 2.Le Chatelier E., Nielsen T., Qin J., et al. Richness of human gut microbiome correlates with metabolic markers. Nature. 2013;500(7464):541–546. doi: 10.1038/nature12506. [DOI] [PubMed] [Google Scholar]
- 3.Gadaleta R.M., Cariello M., Crudele L., Moschetta A. Bile salt hydrolase-competent probiotics in the management of IBD: unlocking the ‘bile acid code’. Nutrients. 2022;14(15):3212. doi: 10.3390/nu14153212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu P., Wang Y., Yang G., et al. The role of short-chain fatty acids in intestinal barrier function, inflammation, oxidative stress, and colonic carcinogenesis. Pharmacol Res. 2021;165 doi: 10.1016/j.phrs.2021.105420. [DOI] [PubMed] [Google Scholar]
- 5.Xiong Y., Miyamoto N., Shibata K., et al. Short-chain fatty acids stimulate leptin production in adipocytes through the G protein-coupled receptor GPR41. Proc Natl Acad Sci U S A. 2004;101(4):1045–1050. doi: 10.1073/pnas.2637002100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perry R.J., Peng L., Barry N.A., et al. Acetate mediates a microbiome-brain-β-cell axis to promote metabolic syndrome. Nature. 2016;534(7606):213–217. doi: 10.1038/nature18309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karlsson F.H., Tremaroli V., Nookaew I., et al. Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature. 2013;498(7452):99–103. doi: 10.1038/nature12198. [DOI] [PubMed] [Google Scholar]
- 8.Vinolo M.A.R., Rodrigues H.G., Festuccia W.T., et al. Tributyrin attenuates obesity-associated inflammation and insulin resistance in high-fat-fed mice. Am J Physiol Endocrinol Metab. 2012;303(2):E272–E282. doi: 10.1152/ajpendo.00053.2012. [DOI] [PubMed] [Google Scholar]
- 9.Vrieze A., Out C., Fuentes S., et al. Impact of oral vancomycin on gut microbiota, bile acid metabolism, and insulin sensitivity. J Hepatol. 2014;60(4):824–831. doi: 10.1016/j.jhep.2013.11.034. [DOI] [PubMed] [Google Scholar]
- 10.Tirosh A., Calay E.S., Tuncman G., et al. The short-chain fatty acid propionate increases glucagon and FABP4 production, impairing insulin action in mice and humans. Sci Transl Med. 2019;11(489) doi: 10.1126/scitranslmed.aav0120. [DOI] [PubMed] [Google Scholar]
- 11.Yoshida N., Emoto T., Yamashita T., et al. Bacteroides vulgatus and Bacteroides dorei reduce gut microbial lipopolysaccharide production and inhibit atherosclerosis. Circulation. 2018;138(22):2486–2498. doi: 10.1161/CIRCULATIONAHA.118.033714. [DOI] [PubMed] [Google Scholar]
- 12.Crudele L., Piccinin E., Moschetta A. Visceral adiposity and cancer: role in pathogenesis and prognosis. Nutrients. 2021;13(6):2101. doi: 10.3390/nu13062101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pedersen H.K., Gudmundsdottir V., Nielsen H.B., et al. Human gut microbes impact host serum metabolome and insulin sensitivity. Nature. 2016;535(7612):376–381. doi: 10.1038/nature18646. [DOI] [PubMed] [Google Scholar]
- 14.Inagaki T., Moschetta A., Lee Y.K., et al. Regulation of antibacterial defense in the small intestine by the nuclear bile acid receptor. Proc Natl Acad Sci U S A. 2006;103(10):3920–3925. doi: 10.1073/pnas.0509592103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scheithauer T.P.M., Rampanelli E., Nieuwdorp M., et al. Gut microbiota as a trigger for metabolic inflammation in obesity and type 2 diabetes. Front Immunol. 2020;11 doi: 10.3389/fimmu.2020.571731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raygan F., Rezavandi Z., Bahmani F., et al. The effects of probiotic supplementation on metabolic status in type 2 diabetic patients with coronary heart disease. Diabetol Metab Syndr. 2018;10:51. doi: 10.1186/s13098-018-0353-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crudele L., De Matteis C., Piccinin E., et al. Low HDL-cholesterol levels predict hepatocellular carcinoma development in individuals with liver fibrosis. JHEP Rep. 2023;5(1) doi: 10.1016/j.jhepr.2022.100627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gurung M., Li Z., You H., et al. Role of gut microbiota in type 2 diabetes pathophysiology. eBioMedicine. 2020;51 doi: 10.1016/j.ebiom.2019.11.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Qin J., Li Y., Cai Z., et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature. 2012;490(7418):55–60. doi: 10.1038/nature11450. [DOI] [PubMed] [Google Scholar]
- 20.Jian C., Silvestre M.P., Middleton D., et al. Gut microbiota predicts body fat change following a low-energy diet: a PREVIEW intervention study. Genome Med. 2022;14(1):54. doi: 10.1186/s13073-022-01053-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zeevi D., Korem T., Zmora N., et al. Personalized nutrition by prediction of glycemic responses. Cell. 2015;163(5):1079–1094. doi: 10.1016/j.cell.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 22.Berry S.E., Valdes A.M., Drew D.A., et al. Human postprandial responses to food and potential for precision nutrition. Nat Med. 2020;26(6):964–973. doi: 10.1038/s41591-020-0934-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Asnicar F., Berry S.E., Valdes A.M., et al. Microbiome connections with host metabolism and habitual diet from 1,098 deeply phenotyped individuals. Nat Med. 2021;27(2):321–332. doi: 10.1038/s41591-020-01183-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dao M.C., Everard A., Aron-Wisnewsky J., et al. Akkermansia muciniphila and improved metabolic health during a dietary intervention in obesity: relationship with gut microbiome richness and ecology. Gut. 2016;65(3):426–436. doi: 10.1136/gutjnl-2014-308778. [DOI] [PubMed] [Google Scholar]
- 25.Haro C., Montes-Borrego M., Rangel-Zúñiga O.A., et al. Two healthy diets modulate gut microbial community improving insulin sensitivity in a human obese population. J Clin Endocrinol Metab. 2016;101(1):233–242. doi: 10.1210/jc.2015-3351. [DOI] [PubMed] [Google Scholar]
- 26.Zimmermann M., Zimmermann-Kogadeeva M., Wegmann R., Goodman A.L. Mapping human microbiome drug metabolism by gut bacteria and their genes. Nature. 2019;570(7762):462–467. doi: 10.1038/s41586-019-1291-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Do H.J., Lee Y.S., Ha M.J., et al. Beneficial effects of voglibose administration on body weight and lipid metabolism via gastrointestinal bile acid modification. Endocr J. 2016;63(8):691–702. doi: 10.1507/endocrj.EJ15-0747. [DOI] [PubMed] [Google Scholar]
- 28.Smith B.J., Miller R.A., Ericsson A.C., Harrison D.C., Strong R., Schmidt T.M. Changes in the gut microbiome and fermentation products concurrent with enhanced longevity in acarbose-treated mice. BMC Microbiol. 2019 Jun 13;19(1):130. doi: 10.1186/s12866-019-1494-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang X., Fang Z., Zhang C., et al. Effects of acarbose on the gut microbiota of prediabetic patients: a randomized, double-blind, controlled crossover trial. Diabetes Ther Res Treat Educ Diabetes Relat Disord. 2017;8(2):293–307. doi: 10.1007/s13300-017-0226-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Su B., Liu H., Li J., et al. Acarbose treatment affects the serum levels of inflammatory cytokines and the gut content of bifidobacteria in Chinese patients with type 2 diabetes mellitus. J Diabetes. 2015;7(5):729–739. doi: 10.1111/1753-0407.12232. [DOI] [PubMed] [Google Scholar]
- 31.Aoki R., Kamikado K., Suda W., et al. A proliferative probiotic Bifidobacterium strain in the gut ameliorates progression of metabolic disorders via microbiota modulation and acetate elevation. Sci Rep. 2017;7 doi: 10.1038/srep43522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhao L., Chen Y., Xia F., et al. A glucagon-like peptide-1 receptor agonist lowers weight by modulating the structure of gut microbiota. Front Endocrinol. 2018;9:233. doi: 10.3389/fendo.2018.00233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang Q., Xiao X., Zheng J., et al. Featured article: structure moderation of gut microbiota in liraglutide-treated diabetic male rats. Exp Biol Med Maywood NJ. 2018;243(1):34–44. doi: 10.1177/1535370217743765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moreira G.V., Azevedo F.F., Ribeiro L.M., et al. Liraglutide modulates gut microbiota and reduces NAFLD in obese mice. J Nutr Biochem. 2018;62:143–154. doi: 10.1016/j.jnutbio.2018.07.009. [DOI] [PubMed] [Google Scholar]
- 35.Adeshirlarijaney A., Gewirtz A.T. Considering gut microbiota in treatment of type 2 diabetes mellitus. Gut Microb. 2020;11(3):253–264. doi: 10.1080/19490976.2020.1717719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liao X., Song L., Zeng B., et al. Alteration of gut microbiota induced by DPP-4i treatment improves glucose homeostasis. eBioMedicine. 2019;44:665–674. doi: 10.1016/j.ebiom.2019.03.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yan X., Feng B., Li P., Tang Z., Wang L. Microflora disturbance during progression of glucose intolerance and effect of sitagliptin: an animal study. J Diabetes Res. 2016;2016 doi: 10.1155/2016/2093171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van Bommel E.J.M., Herrema H., Davids M., Kramer M.H.H., Nieuwdorp M., van Raalte D.H. Effects of 12-week treatment with dapagliflozin and gliclazide on faecal microbiome: results of a double-blind randomized trial in patients with type 2 diabetes. Diabetes Metab. 2020;46(2):164–168. doi: 10.1016/j.diabet.2019.11.005. [DOI] [PubMed] [Google Scholar]
- 39.Lee D.M., Battson M.L., Jarrell D.K., et al. SGLT2 inhibition via dapagliflozin improves generalized vascular dysfunction and alters the gut microbiota in type 2 diabetic mice. Cardiovasc Diabetol. 2018;17(1):62. doi: 10.1186/s12933-018-0708-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wu H., Esteve E., Tremaroli V., et al. Metformin alters the gut microbiome of individuals with treatment-naive type 2 diabetes, contributing to the therapeutic effects of the drug. Nat Med. 2017;23(7):850–858. doi: 10.1038/nm.4345. [DOI] [PubMed] [Google Scholar]
- 41.Hills R.D., Pontefract B.A., Mishcon H.R., Black C.A., Sutton S.C., Theberge C.R. Gut microbiome: profound implications for diet and disease. Nutrients. 2019;11(7):E1613. doi: 10.3390/nu11071613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Elbere I., Silamikelis I., Dindune I.I., et al. Baseline gut microbiome composition predicts metformin therapy short-term efficacy in newly diagnosed type 2 diabetes patients. PLoS One. 2020;15(10) doi: 10.1371/journal.pone.0241338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cao T.T.B., Wu K.C., Hsu J.L., et al. Effects of non-insulin anti-hyperglycemic agents on gut microbiota: a systematic review on human and animal studies. Front Endocrinol. 2020;11 doi: 10.3389/fendo.2020.573891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mueller N.T., Differding M.K., Zhang M., et al. Metformin affects gut microbiome composition and function and circulating short-chain fatty acids: a randomized trial. Diabetes Care. 2021;44(7):1462–1471. doi: 10.2337/dc20-2257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Huang F., Nilholm C., Roth B., et al. Anthropometric and metabolic improvements in human type 2 diabetes after introduction of an Okinawan-based Nordic diet are not associated with changes in microbial diversity or SCFA concentrations. Int J Food Sci Nutr. 2018;69(6):729–740. doi: 10.1080/09637486.2017.1408059. [DOI] [PubMed] [Google Scholar]
- 46.de la Cuesta-Zuluaga J., Mueller N.T., Corrales-Agudelo V., et al. Metformin is associated with higher relative abundance of mucin-degrading Akkermansia muciniphila and several short-chain fatty acid-producing microbiota in the gut. Diabetes Care. 2017;40(1):54–62. doi: 10.2337/dc16-1324. [DOI] [PubMed] [Google Scholar]
- 47.Li M., Li L., Li B., et al. Brown adipose tissue is the key depot for glucose clearance in microbiota depleted mice. Nat Commun. 2021;12(1):4725. doi: 10.1038/s41467-021-24659-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ejtahed H.S., Tito R.Y., Siadat S.D., et al. Metformin induces weight loss associated with gut microbiota alteration in non-diabetic obese women: a randomized double-blind clinical trial. Eur J Endocrinol. 2019;180(3):165–176. doi: 10.1530/EJE-18-0826. [DOI] [PubMed] [Google Scholar]
- 49.Marzano M., Fosso B., Colliva C., et al. Farnesoid X receptor activation by the novel agonist TC-100 (3α, 7α, 11β-Trihydroxy-6α-ethyl-5β-cholan-24-oic Acid) preserves the intestinal barrier integrity and promotes intestinal microbial reshaping in a mouse model of obstructed bile acid flow. Biomed Pharmacother Biomedecine Pharmacother. 2022;153 doi: 10.1016/j.biopha.2022.113380. [DOI] [PubMed] [Google Scholar]
- 50.Gadaleta R.M., Garcia-Irigoyen O., Cariello M., et al. Fibroblast Growth Factor 19 modulates intestinal microbiota and inflammation in presence of Farnesoid X Receptor. eBioMedicine. 2020;54 doi: 10.1016/j.ebiom.2020.102719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pathak P., Xie C., Nichols R.G., et al. Intestine farnesoid X receptor agonist and the gut microbiota activate G-protein bile acid receptor-1 signaling to improve metabolism. Hepatol Baltim Md. 2018;68(4):1574–1588. doi: 10.1002/hep.29857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gadaleta R.M., Moschetta A. Metabolic Messengers: fibroblast growth factor 15/19. Nat Metab. 2019;1(6):588–594. doi: 10.1038/s42255-019-0074-3. [DOI] [PubMed] [Google Scholar]
- 53.Degirolamo C., Sabbà C., Moschetta A. Therapeutic potential of the endocrine fibroblast growth factors FGF19, FGF21 and FGF23. Nat Rev Drug Discov. 2016;15(1):51–69. doi: 10.1038/nrd.2015.9. [DOI] [PubMed] [Google Scholar]
- 54.Crudele L., Garcia-Irigoyen O., Cariello M., et al. Total serum FGF-21 levels positively relate to visceral adiposity differently from its functional intact form. Front Endocrinol. 2023;14 doi: 10.3389/fendo.2023.1159127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sun L., Xie C., Wang G., et al. Gut microbiota and intestinal FXR mediate the clinical benefits of metformin. Nat Med. 2018;24(12):1919–1929. doi: 10.1038/s41591-018-0222-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Forslund K., Hildebrand F., Nielsen T., et al. Disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota. Nature. 2015;528(7581):262–266. doi: 10.1038/nature15766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Degirolamo C., Rainaldi S., Bovenga F., Murzilli S., Moschetta A. Microbiota modification with probiotics induces hepatic bile acid synthesis via downregulation of the Fxr-Fgf15 axis in mice. Cell Rep. 2014;7(1):12–18. doi: 10.1016/j.celrep.2014.02.032. [DOI] [PubMed] [Google Scholar]
- 58.Bryrup T., Thomsen C.W., Kern T., et al. Metformin-induced changes of the gut microbiota in healthy young men: results of a non-blinded, one-armed intervention study. Diabetologia. 2019;62(6):1024–1035. doi: 10.1007/s00125-019-4848-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Arumugam M., Raes J., Pelletier E., et al. Enterotypes of the human gut microbiome. Nature. 2011;473(7346):174–180. doi: 10.1038/nature09944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.De Matteis C., Crudele L., Battaglia S., et al. Identification of a novel score for adherence to the mediterranean diet that is inversely associated with visceral adiposity and cardiovascular risk: the chrono med diet score (CMDS) Nutrients. 2023;15(8):1910. doi: 10.3390/nu15081910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dziewiecka H., Buttar H.S., Kasperska A., et al. Physical activity induced alterations of gut microbiota in humans: a systematic review. BMC Sports Sci Med Rehabil. 2022;14(1):122. doi: 10.1186/s13102-022-00513-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tiderencel K.A., Hutcheon D.A., Ziegler J. Probiotics for the treatment of type 2 diabetes: a review of randomized controlled trials. Diabetes Metab Res Rev. 2020;36(1) doi: 10.1002/dmrr.3213. https://onlinelibrary.wiley.com/doi/10.1002/dmrr.3213 [cited 2021 Dec 13]. Available from: [DOI] [PubMed] [Google Scholar]
- 63.Salgaço M.K., Oliveira L.G.S., Costa G.N., Bianchi F., Sivieri K. Relationship between gut microbiota, probiotics, and type 2 diabetes mellitus. Appl Microbiol Biotechnol. 2019;103(23–24):9229–9238. doi: 10.1007/s00253-019-10156-y. [DOI] [PubMed] [Google Scholar]
- 64.Cani P.D., de Vos W.M. Next-generation beneficial microbes: the case of Akkermansia muciniphila. Front Microbiol. 2017;8:1765. doi: 10.3389/fmicb.2017.01765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Asemi Z., Zare Z., Shakeri H., Sabihi S., Esmaillzadeh A. Effect of multispecies probiotic supplements on metabolic profiles, hs-CRP, and oxidative stress in patients with type 2 diabetes. Ann Nutr Metab. 2013;63(1-2):1–9. doi: 10.1159/000349922. [DOI] [PubMed] [Google Scholar]
- 66.Reimer R.A., Grover G.J., Koetzner L., Gahler R.J., Lyon M.R., Wood S. Combining sitagliptin/metformin with a functional fiber delays diabetes progression in Zucker rats. J Endocrinol. 2014;220(3):361–373. doi: 10.1530/JOE-13-0484. [DOI] [PubMed] [Google Scholar]
- 67.Christensen L., Sørensen C.V., Wøhlk F.U., et al. Microbial enterotypes beyond genus level: Bacteroides species as a predictive biomarker for weight change upon controlled intervention with arabinoxylan oligosaccharides in overweight subjects. Gut Microb. 2020;12(1) doi: 10.1080/19490976.2020.1847627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gupta A., Khanna S. Fecal microbiota transplantation. JAMA. 2017;318(1):102. doi: 10.1001/jama.2017.6466. [DOI] [PubMed] [Google Scholar]
- 69.Svensson C.K., Cold F., Ribberholt I., et al. The efficacy of faecal microbiota transplant and rectal bacteriotherapy in patients with recurrent clostridioides difficile infection: a retrospective cohort study. Cells. 2022;11(20):3272. doi: 10.3390/cells11203272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Luo Y., Tixier E.N., Grinspan A.M. Fecal microbiota transplantation for clostridioides difficile in high-risk older adults is associated with early recurrence. Dig Dis Sci. 2020;65(12):3647–3651. doi: 10.1007/s10620-020-06147-z. [DOI] [PubMed] [Google Scholar]
- 71.de Groot P., Scheithauer T., Bakker G.J., et al. Donor metabolic characteristics drive effects of faecal microbiota transplantation on recipient insulin sensitivity, energy expenditure and intestinal transit time. Gut. 2020;69(3):502–512. doi: 10.1136/gutjnl-2019-318320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sabico S., Al-Mashharawi A., Al-Daghri N.M., et al. Effects of a 6-month multi-strain probiotics supplementation in endotoxemic, inflammatory and cardiometabolic status of T2DM patients: a randomized, double-blind, placebo-controlled trial. Clin Nutr Edinb Scotl. 2019;38(4):1561–1569. doi: 10.1016/j.clnu.2018.08.009. [DOI] [PubMed] [Google Scholar]
- 73.Szulińska M., Łoniewski I., van Hemert S., Sobieska M., Bogdański P. Dose-dependent effects of multispecies probiotic supplementation on the lipopolysaccharide (LPS) level and cardiometabolic profile in obese postmenopausal women: a 12-week randomized clinical trial. Nutrients. 2018;10(6):E773. doi: 10.3390/nu10060773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kobyliak N., Falalyeyeva T., Mykhalchyshyn G., Kyriienko D., Komissarenko I. Effect of alive probiotic on insulin resistance in type 2 diabetes patients: randomized clinical trial. Diabetes Metab Syndr. 2018;12(5):617–624. doi: 10.1016/j.dsx.2018.04.015. [DOI] [PubMed] [Google Scholar]
- 75.Didesch M.M., Averill A., Oh-Park M. Peripheral neuropathy after fecal microbiota transplantation for Clostridium difficile infection: a case report. PM R. 2016;8(8):813–816. doi: 10.1016/j.pmrj.2016.01.009. [DOI] [PubMed] [Google Scholar]