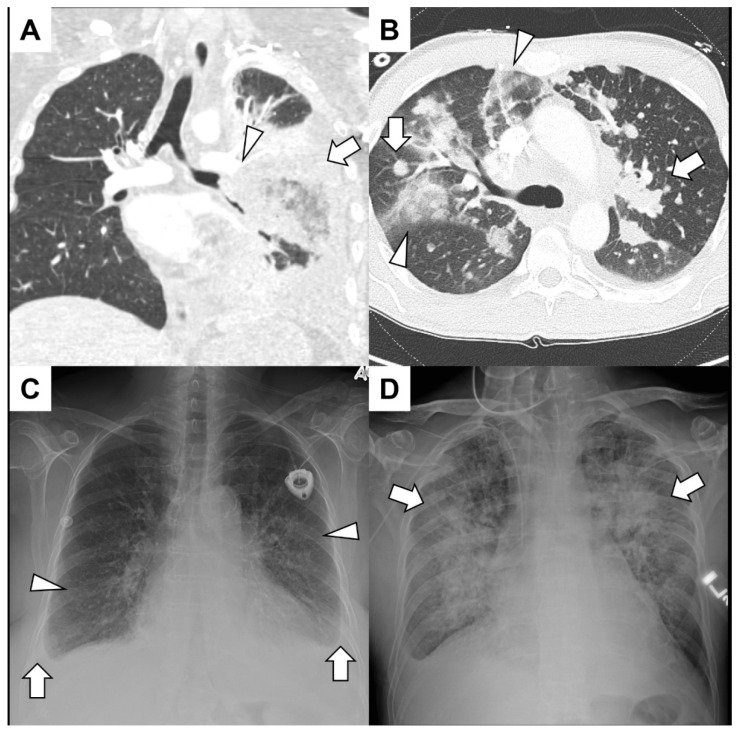
Figure 1.
(A) A young man with acute lymphoid leukemia presented with significant hemoptysis. He had both neutropenia and lymphopenia due to recent treatments. A CT angiogram showed irregular soft-tissue encasement of the lower-order branches of the left pulmonary artery (arrowhead) and consolidation (arrow) and air bronchograms in the left lower lobe. Bronchoscopy revealed that the left lower lobe collapsed without endobronchial lesions. Surgical intervention with left lower lobectomy confirmed invasive mucormycosis and left pulmonary artery branches were full of thrombi. (B) A middle-aged man with adenoid cystic cancer presented with hemoptysis mixed with mucus over the previous few weeks. A CT angiogram excluded pulmonary emboli but showed diffuse nodules and mass-like consolidation (arrows) along with ground glass infiltrates peripherally (arrowhead). No endobronchial component was identified, and since the hemoptysis was of a small volume, no further intervention was warranted. (C) An elderly woman with a history of Hodgkin lymphoma presented with hemoptysis, dyspnea and a syncopal episode. A chest radiograph demonstrated bilateral infiltrates (arrowheads) and small bilateral effusion (arrows) with blunting of the costophrenic angles. She had volume overload with pulmonary edema, and an echocardiogram demonstrated severe aortic valve stenosis. (D) A patient with acute myelogenous leukemia after hematopoietic allogenic stem cell transplantation from a matched sibling presented with hemoptysis and epistaxis. A chest radiograph showed bilateral diffuse infiltrates (arrows), and a bronchoscopy revealed blood-tinged secretions throughout the tracheobronchial tree. He had diffuse alveolar hemorrhage due to thrombotic microangiopathy related to calcineurin inhibitors.