Abstract
Objectives
To compare the development of white spot lesions (WSLs) during fixed orthodontic therapy among a conventional three-step bonding system, a self-etching primer bonding system, and a one-step adhesive bonding system.
Materials and Methods
Seventy-five patients were randomly allocated into three groups (group 1, conventional bonding system, n = 25; group 2, self-etch primer, n = 25; group 3, primer mixed with adhesive composite, n = 25). Quantitative light-induced fluorescence (QLF) was used to assess WSL parameters. Images were captured and then analyzed before treatment and at 2 months and 4 months after bond up. Lesion area (pixels), mean fluorescence loss (ΔF), and the number of newly developed WSLs were compared within and among the three groups. The significance level was P ≤ .05.
Results
The mean increase in lesion area was 31.3 ± 2.8 pixels, 38.4 ± 4.3 pixels, and 119.5 ± 5.3 pixels for groups 1, 2, and 3, respectively (P ≤ .001). For ΔF, the loss was 3.3% ± 0.3%, 4.4% ± 0.2%, and 6.6% ± 0.2% for groups 1, 2, and 3, respectively. These changes were significantly different (P ≤ .01 to P ≤ .001). The incidence of newly developed lesions was 9.5 WSLs in group 1, 10 WSLs in group 2, and 15.9 WSLs in group 3.
Conclusions
The lack of primer contributed to the development of a larger number of and more severe WSLs.
Keywords: Self-etch primer, One-step adhesive, Conventional bonding system, WSLs, QLF
INTRODUCTION
Enamel demineralization may occur in association with orthodontic therapy. Enamel demineralization or white spot lesions (WSLs) may develop wherever bacterial plaque stays on the enamel surface for an extended period.1 This is partly because of the increased sites of food stagnation and acid formation created by attachments, bands, and archwires during fixed orthodontic therapy.
Successful fixed orthodontic treatment relies on the ability of the appliance adhesive system to withstand stresses from mastication and orthodontic forces.2 Phosphoric acid etchant increases the wettable enamel surface by removal of the outer surface of enamel.3 Primer application, which is a low-viscosity unfilled resin, is an important step in bonding; it can properly seal the smooth enamel surface to eliminate WSL formation.4 Exclusion of the priming step was shown to cause air bubbles and a weak bond between the brackets and tooth surface.5
Recently, different types of adhesive systems have been marketed to reduce the steps of conventional bonding procedures (etching + primer + bonding composite). One of these systems includes the primer with the etching agent to reduce the bonding procedure to two steps instead of three.6 Another system includes the primer with the bonding composite.7
By decreasing the number of procedures required for bonding of appliances, clinicians are capable of saving time and decreasing the potential for errors and contamination during the bonding process.8 In addition, the application of acidic primers reduced the quantity of remnant adhesive that stayed on the enamel surface following debonding.9,10 There are very few studies that have been conducted on the effect of the different bonding systems on WSL development.11,12
Specific Objectives
The current study was designed as a randomized clinical trial to evaluate the incidence and severity of enamel demineralization in fixed orthodontic appliance patients, among different bonding systems, using quantitative light-induced fluorescence (QLF).
MATERIALS AND METHODS
Trial Design and Any Changes After Trial Commencement
This was a prospective randomized clinical trial with three arms. The methods were not changed after trial initiation.
Participants, Eligibility Criteria, and Setting
This study was conducted at the postgraduate Dental Teaching Clinics, Jordan University of Science and Technology. Ethical approval was obtained from the Institutional Review Board of Jordan University of Science and Technology and King Abdullah University Hospital (Institutional Review Board No. 1/146/2021, NCT05738356). All participants were informed verbally and in writing about the study and received an informed consent letter to read and sign.
The inclusion criteria were healthy patients of both sexes aged 17–25 years, with mild-to-moderate crowding (≤5 mm), optimum oral hygiene (as determined by clinical examination: Plaque Index13 ≤1, Gingival Index14 ≤1, and a score <1.5 of the plaque surface area [ΔR30] value in the QLF images), maximum of three restored teeth, absence of defective enamel formation in the form of hypocalcification or hypoplasia, and no salivary gland diseases. Of the 200 patients examined, 75 fulfilled the selection criteria and agreed to participate in the study.
Sample Size Calculation
Sample size calculation was conducted using G*power 3.1.9.4, assuming a small effect size (.25) based on the study by Albhaisi et al.,15 which showed that a total sample size of 408 teeth in 17 subjects at least, at a conventional alpha level (.05) and desired power (1 – β) of .90, should be recruited in the study. Assuming a 15% attrition rate, three patients were added. An additional five patients were recruited to compensate for the other variables, making a total sample of 25 patients in each group.
Randomization (Random Number Generation, Allocation Concealment, and Implementation)
The participants were randomly assigned into three study groups according to a simple randomization method using the research randomizer website (www.random.org/sequences/).16 The groups were as follows: group 1, conventional bonding system; group 2, self-etch adhesive system; and group 3, one-step adhesive system.
Blinding
This was a double-blinded study. The first author (Dr Horan) captured and analyzed QLF images and performed data assessment and analysis. A research assistant coded and saved the images while they were being captured. The images were then analyzed on a different occasion.
Intervention
All patients were bonded with fixed appliances (Legend, GC Orthodontics, Alsip, Ill) by the same clinician (Dr Horan).
In group 1, patients received treatment with a conventional three-step adhesive (3M Transbond XT, 3M Unitek, Monrovia, CA). This group comprised 25 participants (11 males and 14 females, with a mean age of 19.6 years). The teeth were etched with 37% phosphoric acid, washed, and dried, followed by application of bonding agent. The adhesive was placed on the base of the bracket. Group 2 comprised 25 patients who received self-etch primer (3M Transbond Plus, 3M Unitek). This group included 10 male and 15 female participants with a mean age of 17.0 years. The seal between the acid and primer compartments was broken to mix them according to the manufacturer’s instructions. The mixture was applied to the tooth surface in an area confined to the area of the bracket base. Then, the adhesive was applied to the bracket base and bonded to the tooth surface. Group 3 comprised 25 patients who received the one-step adhesive system (GC Ortho Connect, GC Orthodontics, Breckerfeld, Germany). This group included 10 male and 15 female participants with a mean age of 18.0 years. The teeth were etched with 37% phosphoric acid, washed, and dried, and then the adhesive was applied to the bracket base and bonded to the tooth surface according to the manufacturer’s recommendations.
All participants received the same orthodontic toothbrush, interdental brushes, and toothpaste (sodium fluoride 0.24% 1.1 mg fluoride ion in 1 g; Colgate Max Fresh, Colgate, New York, NY). Strict oral hygiene regime instructions and dietary advice were given. The risks associated with poor oral hygiene practice while undergoing orthodontic treatment were explained to all participants.
Fluorescence images of all patients were recorded for the maxillary and mandibular anterior and premolar teeth at the start of the study (T0) and at 2 months (T1) and 4 months (T2) from the beginning of the study using a QLF system (Inspektor Research Systems BV, Amsterdam, The Netherlands). The images were captured using customized software (QA2, version 1.27; Inspektor Research Systems BV) using a Canon EOS 550D with Canon 60-mm f/2.8 USM macro lens and Biluminator Tube with the following specifications: 112-mm length and 70-mm diameter, blue illumination 12 high-performance light-emitting diode (LED), white illumination four LED, and QLF special high-pass yellow filter system. Three images were captured on each occasion (frontal, right, and left) for every patient to examine the extent of mineral content for all bonded teeth.
The size and orientation of the images were adjusted through a special application of the software. All of the QLF images were taken with the patients seated in a dental chair with a fixed position.
Outcomes (Primary and Secondary) and Any Changes After Trial Commencement
The QLF images were judged visually for signs of decalcification, which appeared as dark areas surrounded by bright green fluorescing sound tooth tissue. The QLF images were then analyzed using customized software (QA2 version 1.27) to calculate the primary outcomes: the average lesion fluorescence loss (ΔF%) reflecting mineral loss in percentage, the surface area of the WSL (in pixels), and the incidence of newly developed lesions. The secondary outcome included the deepest point in the lesion, expressed as ΔFMax (%).
In the detected lesions, the fluorescence loss and lesion area were determined using the system’s analysis software. A patch was drawn around the lesion site with its borders on sound enamel (Figure 1). Inside this patch, the fluorescence level of the sound tissue was reconstructed by using the fluorescence radiance of the surrounding sound enamel (Figure 2). Then, the percentage difference between the reconstructed and the original fluorescence levels was calculated. Contour points were used to outline the lesion surface area in pixels2.17
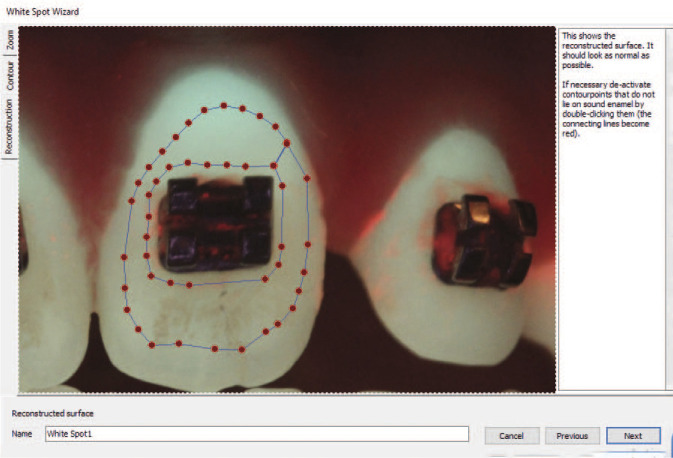
Figure 1.
Quantitative light-induced fluorescence image of a white spot lesion showing the fluorescence radiance reconstruction patch with all its borders on sound enamel.
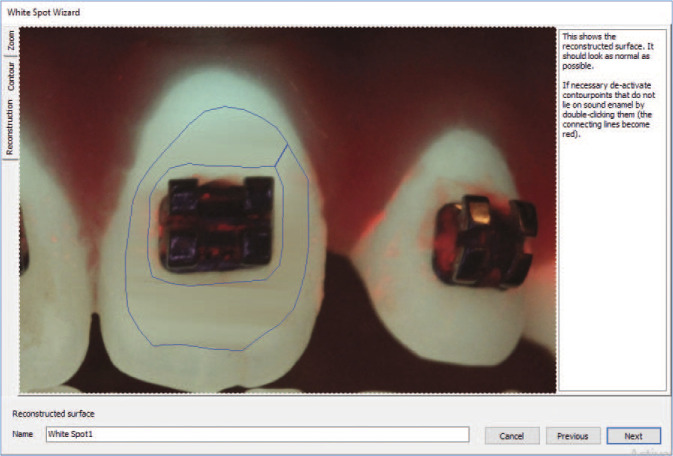
Figure 2.
Quantitative light-induced fluorescence image of a white spot lesion after reconstruction of the fluorescence radiance from the surrounding sound enamel.
Statistical Analysis (Primary and Secondary Outcomes, Subgroup Analyses)
Twenty pictures were randomly selected from the patient list and reanalyzed after a 20-day interval to determine measurement error in this study. The method error was calculated using the Dahlberg18 double determination formula. The Houston19 coefficient of reliability was also calculated, which was greater than 90%. The Dahlberg error values were 0.8% for ΔF and 12.6 pixels for lesion area.
The mean and standard deviation (SD) for all measured parameters at the start of the study (T0) and at 2 months (T1) and 4 months (T2) were calculated using the Statistical Package for Social Science software (SPSS version 28, Chicago, Ill).
Split-plot analysis of variance for repeated measures was used to check differences within and among the three groups regarding lesion area, depth, and mineral change. To check which group was different from the others, Tukey’s test was used.
The chi-square test was used to detect whether there was a significant increase in the number of newly developed WSLs in each group and to compare the incidence of new lesions during the treatment among the three groups. The incidence was calculated by dividing the number of newly developed WSLs by the number of patients in that group. The P value was set at .05.
RESULTS
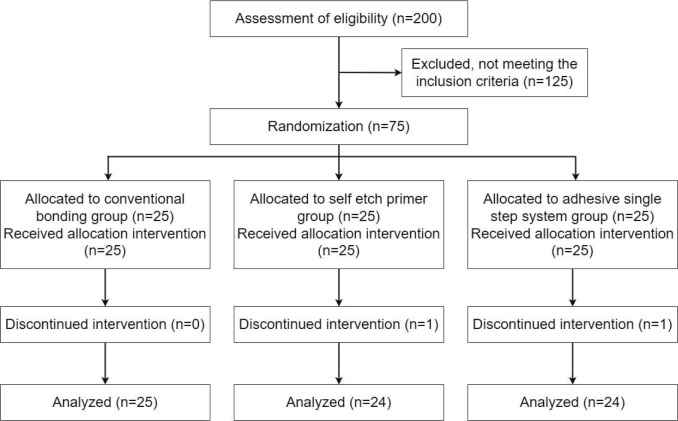
Participant Flow
Twenty-five subjects in group 1, 24 subjects in group 2, and 24 subjects in group 3 continued the treatment and were analyzed. Two patients were dropped, one in group 2 and one in group 3, because they did not show up for their scheduled appointments (Figure 3).
Figure 3.
Flowchart of patient allocation and dropout.
Baseline Data
The total sample had an age range of 17–25 years. The baseline data for all of the measured variables of the WSLs are shown in Table 1.
Table 1.
Mean and SD of Lesion Area, Mean and Maximum Fluorescence Loss, in the Three Groups at the Measured Time Points, Including Changes Over Time in Each Group, Significance, and Confidence Intervals (CIs)
|
|
T0 |
T1 |
T2 |
Difference |
95% CI |
|||||||
|
T0–T1 |
T0–T2 |
T1–T2 |
T0–T1 |
T0–T2 |
T1–T2 |
|||||||
|
Lower |
Upper |
Lower |
Upper |
Lower |
Upper |
|||||||
| Lesion area (pixels) | ||||||||||||
| G1 | 13.5 ± 32.9 | 45.1 ± 58.2 | 44.8 ± 52.3 | −31.6 ± 2.8*** | −31.3 ± 2.8*** | 0.290 ± 2.8NS | −37.1 | −26.1 | −36.9 | −25.7 | −5.2 | 5.8 |
| G2 | 8.8 ± 44.4 | 50.8 ± 89.3 | 47.1 ± 79 | −42 ± 4.8*** | −38.4 ± 4.3*** | 3.6 ± 5.1NS | −51.4 | −32.5 | −46.8 | −30 | −6.5 | 13.7 |
| G3 | 4.8 ± 18.8 | 115 ± 121.6 | 124.3 ± 113.2 | −110.2 ± 5.7*** | −119.5 ± 5.3*** | −9.3 ± 6NS | −121.3 | −99.1 | −130.0 | −109.1 | −21.0 | 2.4 |
| Mean fluorescence loss (ΔF) | ||||||||||||
| G1 | −4.2 ± 6.2 | −8.1 ± 4.3 | −7.6 ± 3.7 | 3.9 ± 0.3*** | 3.3 ± 0.3*** | −0.6 ± 0.2* | 3.3 | 4.5 | 2.7 | 4.0 | −1 | −0.1 |
| G2 | −1.8 ± 3.5 | −6.7 ± 3.8 | −6.2 ± 3.7 | 4.9 ± 0.3*** | 4.4 ± 0.2*** | −0.5 ± 0.3* | 4.4 | 5.4 | 4.0 | 4.9 | −1 | −0.0 |
| G3 | −1 ± 2.5 | −7.4 ± 2.6 | −7.6 ± 2.5 | 6.4 ± 0.2*** | 6.6 ± 0.2*** | 0.2 ± 0.1NS | 6.0 | 6.7 | 6.3 | 7.0 | −0.1 | 0.5 |
| Maximum fluorescence loss (ΔF-Max) | ||||||||||||
| G1 | −7.5 ± 13.2 | −16.4 ± 12.6 | −14.0 ± 10.9 | 8.9 ± 0.8*** | 6.5 ± 0.7*** | −2.4 ± 0.7*** | 7.4 | 10.4 | 5.0 | 8.0 | −3.8 | −1.1 |
| G2 | −2.7 ± 6.5 | −11.7 ± 9.5 | −9.9 ± 8.6 | 8.9 ± 0.5*** | 7.1 ± 0.5*** | −1.8 ± 0.6*** | 7.9 | 10.0 | 6.2 | 8.1 | −3.0 | −0.7 |
| G3 | −1.3 ± 3.5 | −12.9 ± 7.2 | −13.6 ± 7.1 | 11.5 ± 0.4*** | 12.3 ± 0.4*** | 0.7 ± 0.4NS | 10.8 | 12.3 | 11.5 | 13.0 | −0.1 | 1.5 |
P < .05, *** P < 0.001, NS = Not significant.
Numbers Analyzed for Each Outcome, Estimation and Precision, and Subgroup Analyses
Preexisting vs newly developed white spot lesions.
The total number of WSLs pretreatment was 193 lesions in group 1, 101 in group 2, and 75 in group 3, with a mean of 7.7, 4.2, and 3.1 teeth per patient in groups 1, 2, and 3, respectively.
After 4 months of the experiment, the number of new WSLs in group 1 was 238 (with an incidence of 9.5 per patient), in group 2 was 240 teeth (incidence: 10 teeth/patient), and 383 teeth in group 3 (incidence: 15.9 teeth/patient). The incidence of WSLs in all groups was significant (P ≤ .001). Group 2 showed a significantly higher incidence than group 1 (P < .05). Group 3 exhibited a significantly higher incidence than the other two groups (P < .001).
Changes in WSL parameters.
The mean and SD of the measured variables at T0, T1, and T2 for each group; the difference between T0, T1, and T2 for all of the variables; and significant changes within each group are shown in Table 1. Figures 4, 5, and 6 show the WSL parameters for the 3 groups at T0, T1, and T2. Group 3 exhibited larger lesion areas and deeper lesions than groups 1 and 2 (P < .001).
Figure 4.
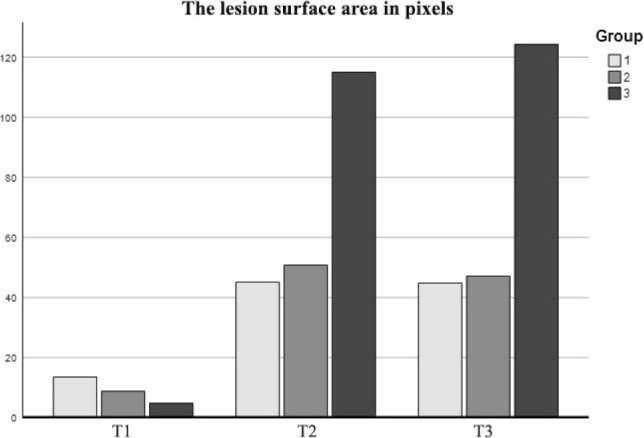
Comparison of lesion area among the three groups at all time points.
Figure 5.
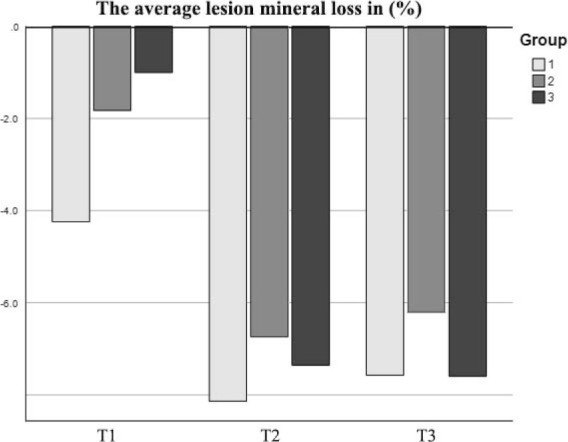
Comparison of mean fluorescence loss among the three groups at all time points.
Figure 6.
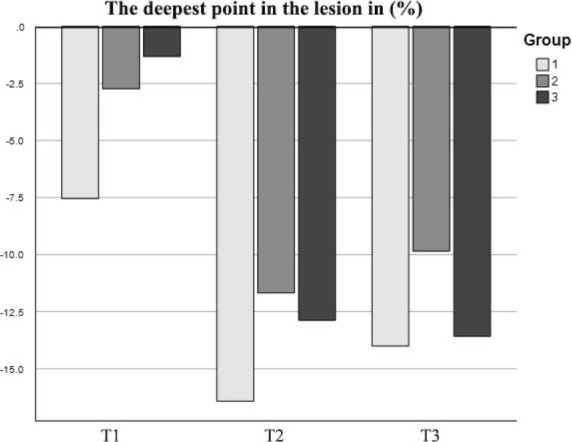
Comparison of maximum fluorescence loss among the three groups at all time points.
Harm.
No harm to the participants was observed in the three study groups.
DISCUSSION
Main Findings in the Context of the Evidence, Interpretation
Different orthodontic appliances and materials vary in the hazards they pose for obstructing oral hygiene methods, subsequently resulting in the development of WSLs. Various studies have evaluated conventional orthodontic bonding systems and their effect on teeth.20–22 However, only a few studies have compared the risk for developing WSLs among different orthodontic bonding agents.23,24 The expanding demand for the use of one-step adhesive systems in orthodontic treatment during the last decades indicates the appropriate assessment of these bonding materials in all aspects of orthodontic therapy. Although the one-step adhesive system was reported to exhibit the least shrinkage compared with other commonly used orthodontic adhesives,25 the effect on the development of WSLs has not been previously investigated.
The patients in this study were monitored for 4 months for the development of WSLs. Four months might be perceived to be a short duration. However, this period was considered adequate to fulfill the objective of the study due to the previously reported, rapid development of WSLs, which might develop within 1 month of beginning fixed appliance therapy.26
Each of the participating patients had a minimum of one WSL before treatment; other studies reported a similar pretreatment prevalence.27 Such a high prevalence of WSLs in studies could be attributed to the fact that QLF can detect very small amounts of demineralization. After 4 months of orthodontic treatment, there was a high incidence of new WSLs; the increased number of WSLs in all groups was significant, and this was in agreement with all previous studies for both conventional bonding and self-etch primer methods.28,29 The one-step adhesive system group was the worst, considering the number of newly developed WSLs, mineral loss, and lesion area; this could be attributed to the absence of the primer layer.4,30,31
Self-etch primer was reported to be a more conservative approach, contributing to a smaller amount of enamel demineralization and less entry of adhesive into the enamel surface compared with the conventional phosphoric acid system.32 However, in this study, it exhibited slightly wider and deeper lesions than the conventional bonding system but showed less area and lesion depth than the one-step adhesive system.
Orthodontic attachments are considered chief plaque-retentive areas. Hence, care should be taken during bonding to confine the etched area to the minimum required and to use primer. Further research, over a longer period of time, is needed to extract more solid evidence regarding the development of WSLs in orthodontic treatment using different bonding systems.
Limitations
The shortcoming of this study was the short duration of 4 months, which did not allow for long-term evaluation of enamel demineralization.
Generalizability
The generalizability of these results might be limited because this research was undertaken in a single dental hospital by 1 clinician (Dr Horan).
CONCLUSIONS
All three study groups showed a significantly increased incidence of WSLs during the study period.
More WSLs occurred in the group using a one-step adhesive system than in the other two groups.
Enamel demineralization and lesion area were significantly greater in the group using the one-step adhesive system compared with the groups using the self-etch primer and the conventional bonding system.
ACKNOWLEDGMENTS
The authors thank Dr Ziad Albuhaisi for his support during image analysis. Our thanks also go to Dr Dana Alshboul and Dr Homam Alsamman for helping with patient recruitment, randomization, blinding, and managing the appointments. In addition, we thank all the patients who participated in the study for their participation and cooperation.
REFERENCES
- 1. Gorelick L, Geiger AM, Gwinnett AJ. Incidence of white spot formation after bonding and banding. Am J Orthod. 1982;81:93–98. doi: 10.1016/0002-9416(82)90032-x. [DOI] [PubMed] [Google Scholar]
- 2. Mohammed RE, Abass S, Abubakr NH, Mohammed ZM. Comparing orthodontic bond failures of light-cured composite resin with chemical-cured composite resin: a 12-month clinical trial. Am J Orthod Dentofacial Orthop. 2016;150:290–294. doi: 10.1016/j.ajodo.2016.02.013. [DOI] [PubMed] [Google Scholar]
- 3. Buonocore MG. A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res. 1955;34:849–853. doi: 10.1177/00220345550340060801. [DOI] [PubMed] [Google Scholar]
- 4. Frazier MC, Southard TE, Doster PM. Prevention of enamel demineralization during orthodontic treatment: an in vitro study using pit and fissure sealants. Am J Orthod Dentofacial Orthop. 1996;110:459–465. doi: 10.1016/s0889-5406(96)70050-1. [DOI] [PubMed] [Google Scholar]
- 5. Miller CC, Burnside G, Higham SM, Flannigan NL. Quantitative light-induced fluorescence-digital as an oral hygiene evaluation tool to assess plaque accumulation and enamel demineralization in orthodontics. Angle Orthod. 2016;86:991–997. doi: 10.2319/092415-648.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bishara SE, Ajlouni R, Laffoon JF, Warren JJ. Comparison of shear bond strength of two self-etch primer/adhesive systems. Angle Orthod. 2006;76((1)):123–126. doi: 10.1043/0003-3219(2006)076[0123:COSBSO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7. Elkalza AR, Mostafa D. Laboratory evaluation of shear bond strength of three different bonding systems for orthodontic brackets. Egypt Orthod J. 2018;53:55–60. [Google Scholar]
- 8. Choi A, Yoo KH, Yoon SY, Park BS, Kim IR, Kim YI. Anti-microbial and remineralizing properties of self-adhesive orthodontic resin containing mesoporous bioactive glass. Materials. 2021;14:3550. doi: 10.3390/ma14133550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bishara SE, Gordan VV, VonWald L, Olson ME. Effect of an acidic primer on shear bond strength of orthodontic brackets. Am J Orthod Dentofacial Orthop. 1998;114:243–247. doi: 10.1016/s0889-5406(98)70205-7. [DOI] [PubMed] [Google Scholar]
- 10. Bishara SE, VonWald L, Laffoon JF, Warren JJ. Effect of a self-etch primer/adhesive on the shear bond strength of orthodontic brackets. Am J Orthod Dentofacial Orthop. 2001;119:621–624. doi: 10.1067/mod.2001.113269. [DOI] [PubMed] [Google Scholar]
- 11. Montasser MA, El-Wassefy NA, Taha M. In vitro study of the potential protection of sound enamel against demineralization. Prog Orthod. 2015;16:1–6. doi: 10.1186/s40510-015-0080-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Paschos E, Rosenbeck KA, Huth KC, Rudzki I, Wichelhaus A, Kunzelmann KH. Evaluation of the effect of bracket-periphery treatment on prevention of enamel demineralization by consecutive μCT scans. Clin Oral Investig. 2015;19:1519–1526. doi: 10.1007/s00784-014-1351-x. [DOI] [PubMed] [Google Scholar]
- 13. Silness J, Löe H. Periodontal disease in pregnancy II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964;22:121–135. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 14. Löe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967;38:610–616. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 15. Albhaisi Z, Al-Khateeb SN, Alhaija ESA. Enamel demineralization during clear aligner orthodontic treatment compared with fixed appliance therapy, evaluated with quantitative light-induced fluorescence: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 2020;157:594–601. doi: 10.1016/j.ajodo.2020.01.004. [DOI] [PubMed] [Google Scholar]
- 16. Random sequence generator Available at: www.random.org/sequences/, accessed December 1, 2021.
- 17. Al-Khateeb S, Tarazi S, Al Maaitah E, Al-Batayneh O, Abu Alhaija ES. Does acid etching enhance remineralization of arrested white spot lesions? Eur Arch Paediatr Dent. 2014;15:413–419. doi: 10.1007/s40368-014-0131-2. [DOI] [PubMed] [Google Scholar]
- 18.Dahlberg G. Statistical Methods for Medical and Biological Students. London: G. Allen & Unwin Ltd; 1940. [Google Scholar]
- 19. Houston WJB. The analysis of errors in orthodontic measurements. Am J Orthod. 1983;83:382–390. doi: 10.1016/0002-9416(83)90322-6. [DOI] [PubMed] [Google Scholar]
- 20. Artun J, Brobakken B. Prevalence of carious white spots after orthodontic treatment with multibonded appliances. Eur J Orthod. 1986;8:229–234. doi: 10.1093/ejo/8.4.229. [DOI] [PubMed] [Google Scholar]
- 21. Julien KC, Buschang PH, Campbell PM. Prevalence of white spot lesion formation during orthodontic treatment. Angle Orthod. 2013;83:641–647. doi: 10.2319/071712-584.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Brown MD, Campbell PM, Schneiderman ED, Buschang PH. A practice-based evaluation of the prevalence and predisposing etiology of white spot lesions. Angle Orthod. 2016;86:181–186. doi: 10.2319/041515-249.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Paschos E, Kleinschrodt T, Clementino-Luedemann T, et al. Effect of different bonding agents on prevention of enamel demineralization around orthodontic brackets. Am J Orthod Dentofacial Orthop. 2009;135:603–612. doi: 10.1016/j.ajodo.2007.11.028. [DOI] [PubMed] [Google Scholar]
- 24. Visel D, Jäcker T, Jost-Brinkmann PG, Präger TM. Demineralization adjacent to orthodontic brackets after application of conventional and self-etching primer systems. J Orofac Orthop. 2014;75:358–373. doi: 10.1007/s00056-014-0233-9. [DOI] [PubMed] [Google Scholar]
- 25. Rasmussen MJ, Togrye C, Trojan TM, Tantbirojn D, Versluis A. Post-gel shrinkage, elastic modulus, and stress generated by orthodontic adhesives. Angle Orthod. 2020;90:278–284. doi: 10.2319/032719-233.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Øgaard B, Rølla G, Arends J. Orthodontic appliances and enamel demineralization: part 1. Lesion development. Am J Orthod Dentofacial Orthop. 1988;94:68–73. doi: 10.1016/0889-5406(88)90453-2. [DOI] [PubMed] [Google Scholar]
- 27. Boersma JG, Van der Veen MH, Lagerweij MD, Bokhout B, Prahl-Andersen B. Caries prevalence measured with QLF after treatment with fixed orthodontic appliances: influencing factors. Caries Res. 2005;39:41–47. doi: 10.1159/000081655. [DOI] [PubMed] [Google Scholar]
- 28. Tufekci E, Dixon JS, Gunsolley JC, Lindauer SJ. Prevalence of white spot lesions during orthodontic treatment with fixed appliances. Angle Orthod. 2011;81:206–210. doi: 10.2319/051710-262.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ghiz MA, Ngan P, Kao E, Martin C, Gunel E. Effects of sealant and self-etching primer on enamel decalcification. Part II: an in-vivo study. Am J Orthod Dentofacial Orthop. 2009;135:206–213. doi: 10.1016/j.ajodo.2007.02.060. [DOI] [PubMed] [Google Scholar]
- 30. Øgaard B. Prevalence of white spot lesions in 19-near-olds: a study on untreated and orthodontically treated persons 5 years after treatment. Am J Orthod Dentofacial Orthop. 1989;96:423–427. doi: 10.1016/0889-5406(89)90327-2. [DOI] [PubMed] [Google Scholar]
- 31. Donly KJ, Ruiz M. In vitro demineralization inhibition of enamel caries utilizing an unfilled resin. Clin Prev Dent. 1992;14:22–24. [PubMed] [Google Scholar]
- 32. Cal-Neto JP, Miguel JAM. Scanning electron microscopy evaluation of the bonding mechanism of a self-etching primer on enamel. Angle Orthod. 2006;76:132–136. doi: 10.1043/0003-3219(2006)076[0132:SEMEOT]2.0.CO;2. [DOI] [PubMed] [Google Scholar]