Abstract
Introduction:
The internet is emerging as a source of information for patients with inflammatory bowel disease (IBD). However, it is not always reliable and may cause anxiety. We aim to assess patients' information habits and patients' and professionals' perceptions of a national website integrated as an educational resource for the IBD unit.
Methods:
Patients aged 18–65 years, comfortable with the internet, and attending follow-ups at participating IBD units (March–June 2019) and their professionals were invited to evaluate a recommended website through an online survey.
Results:
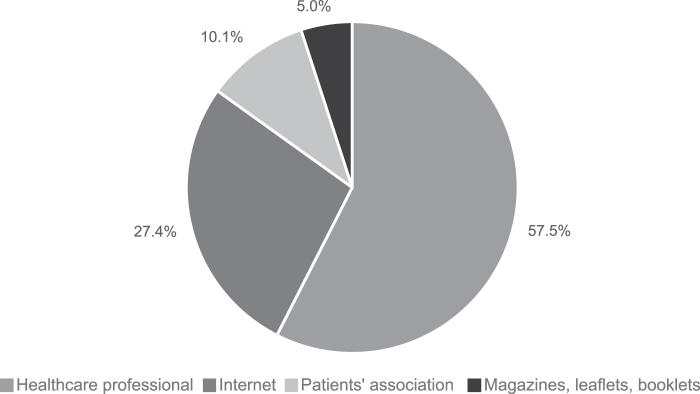
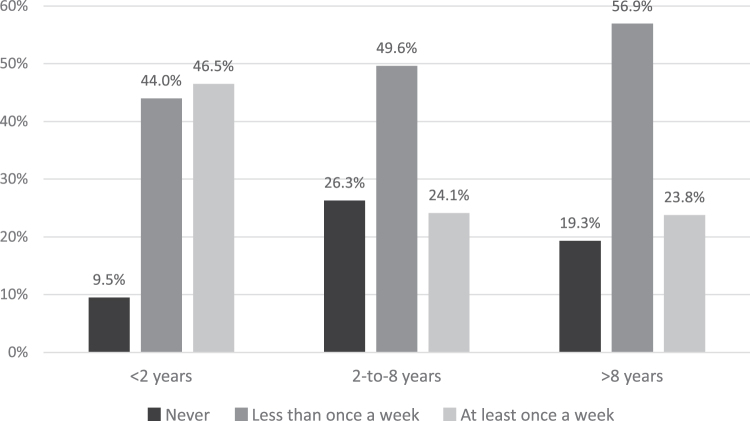
Three hundred eighty-nine patients and 95 professionals completed the survey. The internet (n = 109; 27.4%) was the second preferred source of information after the health care team (n = 229; 57.5%). Eighty percent of patients searched the internet for information on their disease and 28.6% did so at least once a week (n = 114), especially newly diagnosed ones (<2 years). Patients valued a website recommended by their professional (n = 379; 95.2%) and endorsed by the National Working Group (n = 377; 94.7%). They would attend online educational initiatives on the website (n = 279; 70.1%) and complete periodical surveys to improve its usefulness (n = 338; 84.9%). According to IBD professionals, this type of website is the best patient source of supplementary information (n = 76; 80%) and they “prescribe” it to most patients (67.0 ± 25.2%), especially the newly diagnosed patients (52.7 ± 26.5%). It effectively integrates routine face-to-face education (n = 95; 100%).
Conclusions:
Patients of IBD units, especially newly diagnosed ones, appreciate a trusted e-Health resource to back up professional information. The favorable opinion of patients and professionals will allow its use in training interventions.
Keywords: inflammatory bowel disease, patient education, digital health resources, website, digital health, online health, web application, e-Health, telemedicine
Introduction
Inflammatory bowel disease (IBD), including Crohn's disease (CD) and ulcerative colitis (UC), are chronic disabling disorders of the gastrointestinal tract that affect 0.3–0.5% of the population worldwide, impacting on almost aspect of their lives.1,2 Patient education and empowerment are paramount in high-quality inflammatory bowel disease (IBD) care.3–6
The ECCO Consensus on IBD patients' needs in health quality of care7 stressed that “Quality of Health Care depends on the level of disease information available to the patient”; and more recently, the ECCO position article on the quality of care standards includes the need for educational support in all quality indicators.3 In fact, patient education is associated with better disease coping, improved treatment adherence and disease outcomes, and reduced health care resource use.8,9
Traditionally, patient education has been delivered by the clinician in face-to-face sessions,10 through information leaflets, or in patients' association meetings. However, these approaches are insufficient to cover current patient educational needs. Recently, in the IBD2020 Global Forum quality of care survey11 carried out in eight European countries, including Spain, patients reported that within 3 months after diagnosis they had not had an in-depth conversation with their health care provider (HCP) about the basic features of their illness, therapeutic goals, or risks and benefits of the treatment options.
They also complained that their last follow-up visit was too short to discuss all relevant issues and they wished their HCP had relied more on new technologies. The internet has opened up new ways to search for information,11,12 although it is not always reliable and can even become a source of anxiety.12
Thus, there is a need for high-quality websites endorsed by the professional IBD team and scientific organizations providing patient-oriented information7,13,14 as a back up to medical visits. Generally, patients prefer the medical information given by their HCP,7 but to our knowledge, no published studies have explored perceptions of IBD patients on education actively provided by their IBD team by means of a national specialized web application.
Therefore, we conducted a study aimed at (1) assessing patients' preferences and needs of disease-related education and current sources of information; (2) determining the acceptance level of information obtained from a specific web resource endorsed by the Spanish Working Group on Crohn's Disease and Ulcerative Colitis (GETECCU); and (3) evaluating the utility and acceptability of educational interventions and periodical web-based surveys carried out on this platform, tailoring the information to the real needs of patients.
Methods
In October 2017, GETECCU released a national IBD patient education website, called G-Educainflamatoria.15 As per recommendations,7,14 professionals working in IBD units were directly involved in development of an educational web app that would be easy to understand, regularly updated, and tailored to the real needs of patients. Content web quality scored 70 (excellent) on the DISCERN instrument,16 and readability, assessed using the Simple Measure Of Gobbledygook (SMOG) test,17 achieved an approximate SMOG level of 7 (7th grade, junior high school).
This means that over 90% of the website information can be easily understood by the average patient. The website included IBD-related information for patients in the form of written texts, infographics, and educational videos (YouTube channel) and a web forum for patients to ask clinicians questions.
STUDY DESIGN, POPULATION, AND DATA COLLECTION
This was a multicenter, observational cross-sectional study carried out in 33 IBD units across Spain that were invited to use and evaluate the G-Educainflamatoria website15 as an educational tool to integrate routine face-to-face patient education. The study was approved by the corresponding Clinical Research Ethics Committees.
IBD patients between 18 and 65 years of age, attending routine follow-ups at participating IBD units from March to June 2019, were proposed to participate in the study if they had access to the internet and felt comfortable using it. They were invited to browse the website and fill out an anonymous opinion survey. Upon informed consent signature, participants received a link and a password to the online survey (hosted at SurveyMonkey18), where they received instructions on how to complete the questionnaire.
SAMPLE SIZE
In Spain, no nationwide IBD prevalence studies were available at the time of sample size calculation, so prevalence was estimated from a study that had been recently published in Catalonia19 and from European epidemiologic data,20 which indicated that IBD affects 500–600 individuals per 100,000 inhabitants, providing an estimated IBD population in Spain of 300,000 patients. As the proportion of IBD patients who use the internet is currently unknown, we conservatively estimated a 50% prevalence of possible users of an official IBD information website based on the results of a previous study.12 Thus, to obtain representative results with a 95% confidence level and 5% precision, a sample size of 384 patients was estimated.
About 370 professionals were using G-Educainflamatoria at the time of the survey, so a representative sample of 95 professionals was calculated. Participating professionals are listed in Supplementary Data S1. Surveyed HCPs were not involved in the development of the website.
QUESTIONNAIRE
Two independent survey questionnaires were developed: one aimed at patients and the other at IBD professionals. Both questionnaires were structured in two parts: one recorded characteristics of patients or professionals and the other assessed their perceptions regarding the website (Supplementary Data S2).
The understandability and ease of completion of the questionnaire were first evaluated in a pilot study of 15 subjects (5 research staff members and 10 IBD patients) and subsequently improved.
STATISTICAL ANALYSES
Statistical analyses were performed using SPSS 23 (IBM, Armonk, NY). Continuous data are described using means and standard deviations and qualitative data using frequencies and percentages. Characteristics of the groups were compared using Student's t-test or the Mann–Whitney U test, depending on whether data were normally distributed. Continuous variables with more than two categories were compared using analysis of variance (ANOVA). Fisher's exact test or the chi-square test was used for analysis of categorical variables. A p-value of <0.05 was considered statistically significant.
Comparative subanalyses of the patient survey were performed for sex, years since diagnosis (<2, 2–8, and ≥8 years), type of diagnosis (Crohn's or colitis), surgical status (operated vs. nonoperated), treatment (untreated, mesalazine, azathioprine–methotrexate, and biologic), and educational level (elementary school, high school, vocational school, and university). Comparative subanalyses of professionals included sex, years of experience (<2, 2–5, 5–10, and ≥10 years), and role [physician, nurse, or other]).
Results
PATIENTs' SURVEY
Of the 850 patients invited to participate, 462 completed the questionnaire (response rate, 54%). However, 64 patients started but did not finish the survey and were therefore excluded, so the final sample comprised 398 patients. Patient characteristics are listed in Table 1.
Table 1.
Patient Characteristics
| VARIABLE | GLOBAL (n = 398) |
|---|---|
| Age (in years, mean + SD) | 42.9 ± 11.8 |
| Male | 45.5 ± 12.0 |
| Female | 41.0 ± 11.3 |
| Sex, n (%) | |
| Male | 170 (42.7) |
| Female | 229 (57.3) |
| Disease, n (%) | |
| Crohn's disease | 232 (58.3) |
| Ulcerative colitis | 166 (41.7) |
| Time since diagnosis (years), n (%) | |
| <2 | 84 (21.1) |
| Between 2 and 8 | 133 (33.4) |
| >8 | 181 (45.5) |
| Surgery, n (%) | |
| Yes | 81 (20.4) |
| No | 317 (79.6) |
| Current treatment, n (%) | |
| No treatment | 45 (11.3) |
| Mesalazine | 95 (23.9) |
| Azathioprine–methotrexate | 105 (26.4) |
| Biologics | 153 (38.4) |
| Educational level, n (%) | |
| Elementary | 22 (5.5) |
| Secondary | 84 (21.1) |
| Vocational secondary | 168 (42.2) |
| University | 124 (31.2) |
Results presented as n (%) unless otherwise stated.
SD, standard deviation.
SOURCES OF INFORMATION AND FREQUENCY OF INTERNET SEARCHES
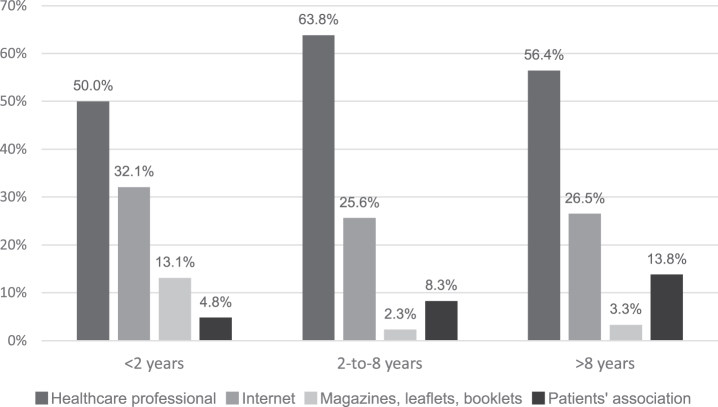
Patients preferred to receive information about their illness from their reference HCP (physician or nurse), while the internet was the second preferred choice among the currently available ones (Fig. 1), especially among newly diagnosed patients who consult the internet and read written resources significantly more frequently than the other groups, but are less interested in patient associations (p = 0.001; Fig. 2).
Fig. 1.
Overall patients' preferred source of information on IBD. IBD, inflammatory bowel disease.
Fig. 2.
Patients’ preferred source of information by time since diagnosis. Newly diagnosed patients (< 2 years) are more inclined to perform internet searches.
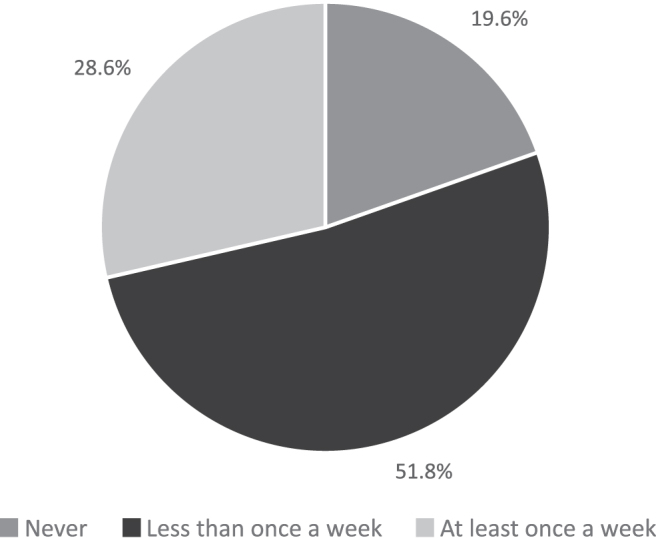
About 80% of patients searched the internet for information on IBD. Almost a third of the sample consulted the internet at least once a week (Fig. 3), with newly diagnosed patients (<2 years) consulting it more frequently, once a week or more (Fig. 4).
Fig. 3.
Overall frequency of internet searches about IBD.
Fig. 4.
Frequency of internet searches about IBD by time since diagnosis. Newly diagnosed patients (< 2 years) consulting it more frequently). (p £ 0.001 for all comparisons).
TOP TRENDING TOPICS
The topics most searched on the web were treatments (n = 295; 74.1%), symptoms (n = 261; 65.6%), nutrition (n = 255; 64.1%), and IBD extraintestinal manifestations (n = 205; 51.5%), while <20% of patients searched for information on diagnostic tests, vaccines and prevention, and surgery.
Patient information needs according to patient profile are reported in Supplementary Data S3.
PATIENTs' PERCEPTIONS OF THE EDUCATIONAL WEB APP
The survey comprised a series of questions aimed at investigating patients' views on the website. Results are shown in Table 2.
Table 2.
Patients' Opinions on the G-Educainflamatoria Website
| PATIENTs' PERCEPTIONS OF THE G-EDUCAINFLAMATORIA WEBSITE (n = 398) | ||||
|---|---|---|---|---|
| Do you think it is important that your doctor or nurse recommends a quality website? (score from 1 to 5, where 1 is “not important at all” and 5 is “very important”) | ||||
| 1 | 2 | 3 | 4 | 5 |
| 0 (0) | 2 (0.5) | 17 (4.3) | 87 (21.9) | 292 (73.3) |
| The G-Educainflamatoria website hosts a forum where patients can ask questions and IBD professionals answer them. Would you use it to consult a specialist if you needed information? | ||||
| No | 58 (14.6) | |||
| Yes | 340 (85.4) | |||
| Do you find the G-Educainflamatoria content easy to understand? (score from 1 to 5, where 1 is “very difficult to understand” and 5 is “very easy to understand”) | ||||
| 1 | 2 | 3 | 4 | 5 |
| 5 (1.3) | 8 (2.0) | 32 (8.0) | 151 (37.9) | 202 (50.8) |
| On the G-Educainflamatoria home page, there is a search engine for searching information. Do you think it is useful? (score from 1 to 5, where 1 is “I do not think it is useful” and 5 is “it is very useful”) | ||||
| 1 | 2 | 3 | 4 | 5 |
| 4 (1.0) | 5 (1.3) | 43 (10.8) | 151 (37.9) | 195 (49.0) |
| Score the usefulness of the G-Educainflamatoria website content from 1 to 5 (where 1 is “it does not seem to be useful at all” and “it seems very useful for learning about my disease”). | ||||
| 1 | 2 | 3 | 4 | 5 |
| 2 (0.5) | 4 (1.0) | 29 (7.3) | 142 (35.7) | 221 (55.5) |
| Score from 1 to 5 the confidence you get from knowing that the G-Educainflamatoria webpage is endorsed by the IBD National Scientific Organization and that it is recommended by your medical team (where 1 is “I do not feel confident at all” and 5 is “I feel reassured and very confident with a website recommended by my medical team”). | ||||
| 1 | 2 | 3 | 4 | 5 |
| 2 (0.5) | 4 (1.0) | 15 (3.8) | 34 (8.5) | 343 (86.2) |
| Would you like to see the website information organized by topic menus, such as a “Newly diagnosed” menu or “Perianal disease” menu or “Disease acceptance” menu? | ||||
| No | 33 (8.3) | |||
| Yes | 365 (91.7) | |||
| Which topic menu would you like to find in G-Educainflamatoria? (Multiple choices were allowed) | ||||
| Newly diagnosed | 338 (84.9) | |||
| Nutrition and diet | 338 (84.9) | |||
| Emotional well-being | 318 (79.9) | |||
| IBD follow-up and checkups | 239 (60.1) | |||
| Women and IBD | 179 (45.0)a | |||
| Would you like to take part in virtual educational activities on the G-Educainflamatoria website with the aim of improving aspects related to your disease (adherence, nutrition, healthy lifestyle, etc.) or would you prefer to attend them in person? | ||||
| On the online platform | 279 (70.1) | |||
| In person | 103 (25.9) | |||
| It does not matter to me | 16 (4.0) | |||
| Would you be willing to periodically answer questions aimed at assessing your viewpoint or degree of knowledge about specific aspects of your disease? | ||||
| Yes | 338 (84.9) | |||
| No | 40 (10.1) | |||
| It depends on the topics; I would decide on the spot | 20 (5.0) | |||
Results presented as n (%) unless otherwise stated.
After adjusting by sex, 96.6% of women wished a “Women and IBD” menu existed.
IBD, inflammatory bowel disease.
Almost all respondents agreed on the importance of their care team informing them about a quality web app endorsed by IBD scientific societies (score of 4–5 on a 5-point Likert scale, n = 379; 95.2%), and this made them feel reassured and confident in the content of the website (scores 4–5, n = 377; 94.7%). In their opinion, the information was easy to understand (score 4–5, n = 353; 88.7%), especially for recently diagnosed patients (<2 years) (n = 82; 97.6%).
Patients would be willing to attend educational initiatives on the website (preferred option over in-person activities) and to answer periodical surveys aimed at investigating their perceptions or assessing their degree of knowledge about different aspects of the disease (Table 2).
Comments and suggestions were also collected (selected comments are reported in Supplementary Data S4). Comments were generally positive, and the web app was perceived to be useful and reliable because it was developed and recommended by IBD professionals. Participants valued the initiative of collecting patients' perceptions, insisting on the need to keep the website updated. The general tone was of gratitude and compliments for a job well done.
PROFESSIONALs' SURVEY
Ninety-five professionals completed the survey (Table 3). According to 80% of respondents, a specialized IBD website endorsed by scientific societies is the most appropriate source of supplementary information for patients among those currently available in the clinical practice, and all participants emphasized that it was crucial to proactively recommend it (Table 4).
Table 3.
Characteristics of Professionals
| VARIABLE | GLOBAL (n = 95) |
|---|---|
| Age, years | 43.3 ± 10.1 |
| Sex | |
| Male | 25 (26) |
| Female | 70 (74) |
| Professional role | |
| Doctor | 64 (67) |
| Nurse | 25 (26) |
| Other | 6 (6) |
| Experience (n = 94) | |
| <2 years | 10 (11) |
| Between 2 and 5 years | 13 (14) |
| Between 5 and 10 years | 24 (26) |
| >10 years | 47 (50) |
Results presented as n (%) unless otherwise stated.
Table 4.
Professionals' Views on Sources of Information for Patients
| SOURCES OF INFORMATION (n = 95) | ||||
|---|---|---|---|---|
| Choose among the educational methods currently available the option you consider most appropriate for providing extra support to your patients' education | ||||
| Leaflets and booklets provided by the IBD unit | 4 (4) | |||
| Website recommended by the IBD unit and endorsed by IBD professionals who keep it updated | 76 (80) | |||
| Explanation given by the doctor/nurse at the patient's request | 13 (14) | |||
| Periodic face-to-face meetings organized by the IBD unit or patients' associations | 2 (2) | |||
| Score from 1 to 5 the importance of supporting IBD education of patients from their own IBD unit (where 1 is “not important at all” and 5 is “very important”). | ||||
| 1 | 2 | 3 | 4 | 5 |
| 0 (0) | 0 (0) | 0 (0) | 12 (13) | 83 (87) |
Results presented as n (%) unless otherwise stated.
Almost all professionals (n = 93; 99%) agreed on the importance of being able to recommend such an educational instrument to their patients, which would enhance the quality of health care (n = 95; 100%) (Supplementary Data S5).
Participants “prescribed” the website to most patients (67.0 ± 25.2% doctors' own estimation) and the main “indication” was recommending it to newly diagnosed patients (52.7 ± 26.5% doctors' own estimation) perceived as a group with greater informational needs (Supplementary Data S5).
Participants considered website content to be of high quality (score 4–5, n = 94; 99%) and easy for patients to understand (score 4–5, n = 91; 96%). They agreed on the importance of offering a forum for patients to consult their HCPs (score 4–5, n = 84; 88%) and nearly 97% (n = 88) would recommend it to professionals of other IBD units (score 4–5) (Supplementary Data S5).
HCP open-handed comments on G-Educainflamatoria were generally positive, participants found the website useful, the importance of maintaining up-to-date information was stressed, and the importance of collecting patients' perspectives was appreciated (selected comments are presented in Supplementary Data S4).
Discussion
IBD patients, especially the newly diagnosed patients, have many doubts about their illness; however, time limits imposed by routine health care make it difficult to fully cover patient's information needs. We proposed that in the internet era, face-to-face education could be integrated with e-Health technologies, so a group of specialists from the IBD National Working Group (GETECCU) developed an IBD patient information website to fulfill this need.
In this study, we found that patients (1) appreciate and rely on information obtained from the website endorsed by the national IBD organization; (2) are willing to respond to surveys on their perceptions or degree of knowledge of topics related to their disease; (3) are interested in participating in web-based educational activities; and (4) are willing to contribute to web content design by giving their feedback.
This can establish a positive web interaction that may empower patients and improve disease control. IBD professionals also believe that an official educational website is an appropriate tool for integrating routine face-to-face patient education and they actually “prescribe” it in their daily routine, especially to newly diagnosed patients.
IBD patients are taking control of their disease, and the demand for information is growing.21 A recent study carried out by GETECCU in collaboration with the Spanish Confederation of Associations of Patients with Crohn's and Ulcerative Colitis (ACCU) developed a series of quality indicators also based on patients' perceptions. One of the most important items was acquiring sufficient information about their illness,22 so delivering adequate patient-oriented information should be a priority for IBD units.
IBD e-Health resources are generally part of telehealth programs; however, only a few initiatives are accessible in routine care.10 The G-Educainflamatoria web app15 is currently integrated into the routine care of 73 IBD units (Supplementary Data S6), hosting >300 educational entries and self-control tools23 developed and supervised by GETECCU. It has its own YouTube channel, with about 70 informative videos, many of which are animated presentations on a wide range of topics. Videos of patients communicating positive messages or telling their own experiences are also available.
The website was released in October 2017, 18 months after we surveyed users, both patients and IBD professionals, on their impressions to improve our design and content and adjust them to patients' needs. Collected feedback about web app use and menu organization was subsequently implemented to improve patients' experience. “Prescription” menus were created for special groups, such as “newly diagnosed patients” or “women and IBD,” according to patients' wishes and following published recommendations.24 Indeed, a new version of the app has recently been released (Supplementary Data S7). Quality surveys are scheduled periodically to gather users' feedback and consistently update the website in response to patients' needs.
Patients generally prefer receiving information from their IBD team in person, but as the internet is a growing source of information,11,25,26 patients have shown in this survey that such an online educational tool is acceptable and appreciated.
Based on our results, we may venture to state that certain features of our educational website foster a positive perception among patients: the IBD National Working Group (GETECCU) is directly involved in the development and promotion of the website; surveys are performed to collect patients' opinions and their feedback is promptly integrated to improve their experience; the level of written comprehension was assessed with validated instruments before the contents were made available to ensure that virtually all users understand the information; and a web forum is available for patients and caregivers to ask questions. It is known that there are topics that are embarrassing for patients to talk about,27 thus allowing for anonymous questioning in the web forum may help patients to address these doubts.
Newly diagnosed patients are more inclined to perform internet searches. This is consistent with findings from a study carried out in the United States by Bernstein et al,11 who reported that less than half of patients were completely satisfied with the information they were given at the time of IBD diagnosis and a quarter were clearly unsatisfied. Authors suggest that supplementing physician–patient consultations with well-designed written information or a website recommendation could foster more effective communication and education.
Indeed, in their study, patients rated these sources of information as highly acceptable. This is true for our survey too, and in response, we created an ad hoc menu for this patient group, and we will develop future website activities and surveys especially directed to this population.
Access to a quality web app helped foster digital education and patient support especially in the present context of the COVID-19 pandemic, which has reinforced the concept of remote patient care. As routine consultations with IBD professionals were largely replaced by telephone or e-mail contacts during the first year of the pandemic, this web app has acted as an additional powerful patient-oriented tool.
Although pandemic restrictions are relaxing, we firmly believe that new follow-up protocols relying on the internet will be permanently integrated into future routine clinical practice. Thus, we believe that the use of e-Health educational resources that offer this kind of professional involvement will increase significantly in IBD units in the immediate future.
Our study has some limitations. Collecting data from internet users involves a systematic bias as certain segments of the population do not have internet access, such as those with lower socioeconomic status. Nonetheless, this bias appears to be rapidly reducing: in 2017, 83.4% of Spanish households had internet access.28 Our study did not explore the effect of socioeconomic status.
However, we speculated that there could be a systematic bias toward more highly educated patients. Almost one-third of respondents had a university education, which is comparable with the national rate (30.1%, at the second trimester of 2019). Secondary education levels among our sample are also comparable with the general population rate (63.3% vs. 68.6%),28 so it seems that educational bias is not an issue in our series.
Recruiting patients in IBD units can also introduce a bias as these units concentrate on a selected group of patients who may have more severe disease and are generally more informed and eager to understand their disease compared with patients followed in a gastroenterologist's office or primary care. This may potentially limit the generalizability of our results to an unfiltered patient group. However, we have demonstrated the feasibility of recruiting an online cohort of IBD patients to study relevant patient-reported perceptions.
Recruitment of almost 400 participants from 33 IBD units over a 3-month period provides strong evidence of the interest of the IBD patient community in participating in such a project. Longitudinal follow-up of this large diverse cohort of participants will help clarify the complex associations between health education and behaviors, medical treatments, and disease course measured by patient-reported outcomes.
Moreover, we have also designed a scalable modular platform, upon which interventional studies and translational studies can be built using the contact information of study participants for future evaluation of health–behavior intervention outcomes.
In conclusion, we strongly believe that e-Health can backup IBD care in the internet era. Patients trust an IBD educational web app recommended by their clinicians and endorsed by scientific societies as very useful and reliable. These e-Health resources may be of particular interest to newly diagnosed patients, given their increased need for information and regular use of the internet for their health searches.
Integrating patients' perceptions and preferences in the design and content of an e-Health portal intended to foster their education may make it more effective. Furthermore, these types of websites are welcomed by IBD HCPs and are routinely “prescribed,” especially to newly diagnosed patients. They are also ideal platforms for conducting online educational interventions and studies assessing patient knowledge.
Supplementary Material
Acknowledgments
The authors acknowledge the collaboration of Dr. Maria Giovanna Ferrario and Dr. Amanda López Picado and the Medical Statistics Consulting (Valencia) team in the data analysis and writing of this article. The first author (A.E.) is enrolled in a Health Sciences doctoral program at the University of Coruña and this article is part of her work in the program. The authors thank the Spanish Working Group on Crohn's Disease and Ulcerative Colitis (GETECCU) for promoting the G-Educainflamatoria web app and Abbvie, Chiesi, Ferring, Janssen, Sandoz, Kern, Adacyte, Pfizer, Takeda, Tillots, and Fresenius Kabi for support.
Contributor Information
Collaborators: on behalf of the G-Educainflamatoria—GETECCU Group
Authors' Contributions
A.E., M.C., and P.N. were responsible for the study concept and design, survey design, data collection, analysis and interpretation of data, and initial draft of the article. J.L.P., G.M., M.S.A., M.C.M.P., N.M., B.B., N.C., B.C., D.M.R., Y.S.O., P.C., M.C., A.M.L.C., and J.M. were responsible for the study concept and design, interpretation of data, and critical revision of the survey and article.
Disclosure Statement
A.E. has participated as a speaker, trainer, or consultant in projects funded by Takeda, Janssen, AbbVie, Pfizer, and MSD Spain. M.C. has participated as a speaker, trainer, or consultant in projects funded by MSD Spain, AbbVie, Takeda, Janssen, Pfizer, Dr. Falk, Faes Farma, Ferring, and Tillotts. N.M. has participated as a speaker in projects funded by Takeda, Janssen, and AbbVie. None of the other coauthors has any conflicts of interest to declare.
Funding Information
No funding was received for this article.
Supplementary Material
REFERENCES
- 1. Ng SC, Shi HY, Hamidi N, et al. . Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: A systematic review of population-based studies. Lancet 2017;390(10114):2769–2778; doi: 10.1016/s0140-6736(17)32448-0 [DOI] [PubMed] [Google Scholar]
- 2. Kaplan GG. The global burden of IBD: From 2015 to 2025. Nat Rev Gastroenterol Hepatol 2015;12(12):720–727; doi: 10.1038/nrgastro.2015.150 [DOI] [PubMed] [Google Scholar]
- 3. Fiorino G, Lytras T, Younge L, et al. . Quality of care standards in inflammatory bowel diseases: A European Crohn's and Colitis Organisation (ECCO) position paper. J Crohns Colitis 2020;14(8):1037–1048; doi: 10.1093/ecco-jcc/jjaa023 [DOI] [PubMed] [Google Scholar]
- 4. Kapasi R, Glatter J, Lamb CA, et al. . Consensus standards of healthcare for adults and children with inflammatory bowel disease in the UK. Frontline Gastroenterol 2020;11(3):178–187; doi: 10.1136/flgastro-2019-101260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lamb CA, Kennedy NA, Raine T, et al. . British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut 2019;68(Suppl. 3):s1–s106; doi: 10.1136/gutjnl-2019-318484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chen Y, Shen J. Core indicators of an evaluation and guidance system for quality of care in inflammatory bowel disease centers: A critical review. EClinicalMedicine 2022;46:101382; doi: 10.1016/j.eclinm.2022.101382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Elkjaer M, Moser G, Reinisch W, et al. . IBD patients need in health quality of care ECCO consensus. J Crohns Colitis 2008;2(2):181–188; doi: 10.1016/j.crohns.2008.02.001 [DOI] [PubMed] [Google Scholar]
- 8. Burisch J, Vegh Z, Pedersen N, et al. . Health care and patients' education in a European inflammatory bowel disease inception cohort: An ECCO-EpiCom study. J Crohns Colitis 2014;8(8):811–818; doi: 10.1016/j.crohns.2013.12.023 [DOI] [PubMed] [Google Scholar]
- 9. Colombara F, Martinato M, Girardin G, et al. . Higher levels of knowledge reduce health care costs in patients with inflammatory bowel disease. Inflamm Bowel Dis 2015;21(3):615–622; doi: 10.1097/mib.0000000000000304 [DOI] [PubMed] [Google Scholar]
- 10. Yin AL, Hachuel D, Pollak JP, et al. . Digital health apps in the clinical care of inflammatory bowel disease: Scoping review. J Med Internet Res 2019;21(8):e14630; doi: 10.2196/14630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bernstein K, Promislow S, Carr R, et al. . Information needs and preferences of recently diagnosed patients with inflammatory bowel disease. Inflamm Bowel Dis 2011;17:590–598; doi: 10.1002/ibd.21363 [DOI] [PubMed] [Google Scholar]
- 12. Selinger CP, Carbery I, Warren V, et al. . The relationship between different information sources and disease-related patient knowledge and anxiety in patients with inflammatory bowel disease. Aliment Pharmacol Ther 2017;45(1):63–74; doi: 10.1111/apt.13831 [DOI] [PubMed] [Google Scholar]
- 13. Langille M, Bernard A, Rodgers C, et al. . Systematic review of the quality of patient information on the internet regarding inflammatory bowel disease treatments. Clin Gastroenterol Hepatol 2010;8(4):322–328; doi: 10.1016/j.cgh.2009.12.024 [DOI] [PubMed] [Google Scholar]
- 14. Louis E, Dotan I, Ghosh S, et al. . Optimising the inflammatory bowel disease unit to improve quality of care: Expert recommendations. J Crohns Colitis 2015;9(8):685–691; doi: 10.1093/ecco-jcc/jjv085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. GETECCU. G-Educainflamatoria. Available from: https://educainflamatoria.com/ [Last accessed: December, 2022].
- 16. Charnock D, Shepperd S, Needham G, et al. . DISCERN: An instrument for judging the quality of written consumer health information on treatment choices. J Epidemiol Community Health 1999;53(2):105–111; doi: 10.1136/jech.53.2.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hedman AS. Using the SMOG formula to revise a health-related document. Am J Health Educ 2008;39(1):61–64; doi: 10.1080/19325037.2008.10599016 [DOI] [Google Scholar]
- 18. Survey Monkey. Available from: https://es.surveymonkey.com/ [Last accessed: December, 2022].
- 19. Brunet E, Roig-Ramos C, Vela E, et al. . Prevalence, incidence and mortality of inflammatory bowel disease in Catalonia. A population-based analysis. Ann Med 2018;50(7):613–619; doi: 10.1080/07853890.2018.1523550 [DOI] [PubMed] [Google Scholar]
- 20. Burisch J, Jess T, Martinato M, et al. . The burden of inflammatory bowel disease in Europe. J Crohns Colitis 2013;7(4):322–337; doi: 10.1016/j.crohns.2013.01.010 [DOI] [PubMed] [Google Scholar]
- 21. Casellas F, Vicens DG, Menendez SR, et al. . Patients' perceptions, attitudes, and experiences about the management of mild-to-moderate ulcerative colitis. J Crohns Colitis 2014;8(9):1097–1107; doi: 10.1016/j.crohns.2014.02.013 [DOI] [PubMed] [Google Scholar]
- 22. Calvet X, Saldana R, Carpio D, et al. . Improving quality of care in inflammatory bowel disease through patients' eyes: IQCARO project. Inflamm Bowel Dis 2020;26(5):782–791; doi: 10.1093/ibd/izz126 [DOI] [PubMed] [Google Scholar]
- 23. Echarri A, Vera I, Ollero V, et al. . The Harvey-Bradshaw index adapted to a mobile application compared with in-clinic assessment: The MediCrohn study. Telemed J E Health 2020;26(1):80–88; doi: 10.1089/tmj.2018.0264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mitchell R, Kremer A, Westwood N, et al. . Talking about life and IBD: A paradigm for improving patient-physician communication. J Crohns Colitis 2009;3(1):1–3; doi: 10.1016/j.crohns.2008.07.002 [DOI] [PubMed] [Google Scholar]
- 25. Catalan-Serra I, Huguet-Malaves JM, Minguez M, et al. . Information resources used by patients with inflammatory bowel disease: Satisfaction, expectations and information gaps. Gastroenterol Hepatol 2015;38(6):355–363; doi: 10.1016/j.gastrohep.2014.09.003 [DOI] [PubMed] [Google Scholar]
- 26. Wong S, Walker JR, Carr R, et al. . The information needs and preferences of persons with longstanding inflammatory bowel disease. Can J Gastroenterol 2012;26(8):525–531; doi: 10.1155/2012/735386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fourie S, Norton C, Jackson D, et al. . ‘These discussions aren't happening’. Experiences of people living with inflammatory bowel disease talking about sexual well-being with healthcare professionals. J Crohns Colitis 2021; doi: 10.1093/ecco-jcc/jjab043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. National Institute of Statistics. Population of 16 years old and over by educational level reached, sex and age group. 2019. Available from: https://www.ine.es/jaxiT3/Tabla.htm?t=6369&L=1 [Last accessed: March, 2020].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.