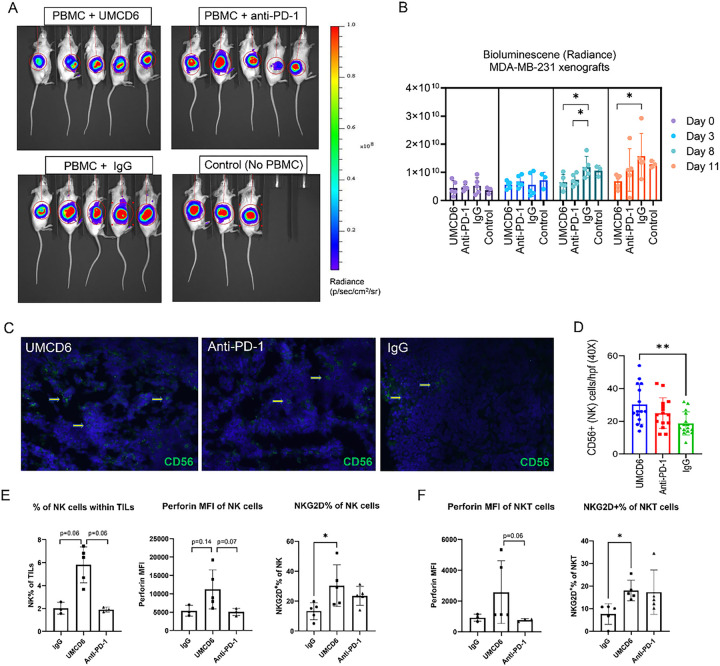
Figure 2. The effect of UMCD6 is more sustained than pembrolizumab in the killing of MDA-MB-231-derived xenograft tumors by PBMC.
A and B: We conducted a short-term in vivo experiment in which SCID/mice were first inoculated with MDA-MB-231 breast cancer cells, then administered 10×106 human PBMCs and antibodies (UMCD6, pembrolizumab or IgG; 100 μg). Both UMCD6 and pembrolizumab enhanced tumor killing by PBMC at day 8 compared to IgG control (*p < 0.05), but only UMCD6 showed statistical significance at day 11 (*p < 0.05). Data represents mean of 4–5 animals ± SD. C: Representative pictures of tumor tissues immunostained for CD56 (human NK cell marker) at day 12 after treatment with UMCD6. D: Immunofluorescence of tumor sections stained for the presence of NK cells showed that mice administered UMCD6 had an increased number of tumor-infiltrating NK cells compared to IgG control group (40X). E: Characterization of tumor-infiltrating lymphocytes (TILs) by flow cytometry shows that tumor-infiltrating NK cells are found in higher proportions in mice treated with UMCD6. NK cells are more abundant in UMCD6-treated mice (average of 5.8% among TILs) compared with IgG (2.01%) and anti-PD-1 (1.92%). Moreover, tumor-infiltrating NK cells from UMCD6-treated xenografts express higher levels of the activating receptor NKG2D (*p < 0.05 vs IgG). F: Similarly, NKG2D expression in tumor-infiltrating NKT cells is significantly elevated upon treatment with UMCD6 (*p < 0.05 vs IgG), accompanied with an increase in perforin expression (ns).