Abstract
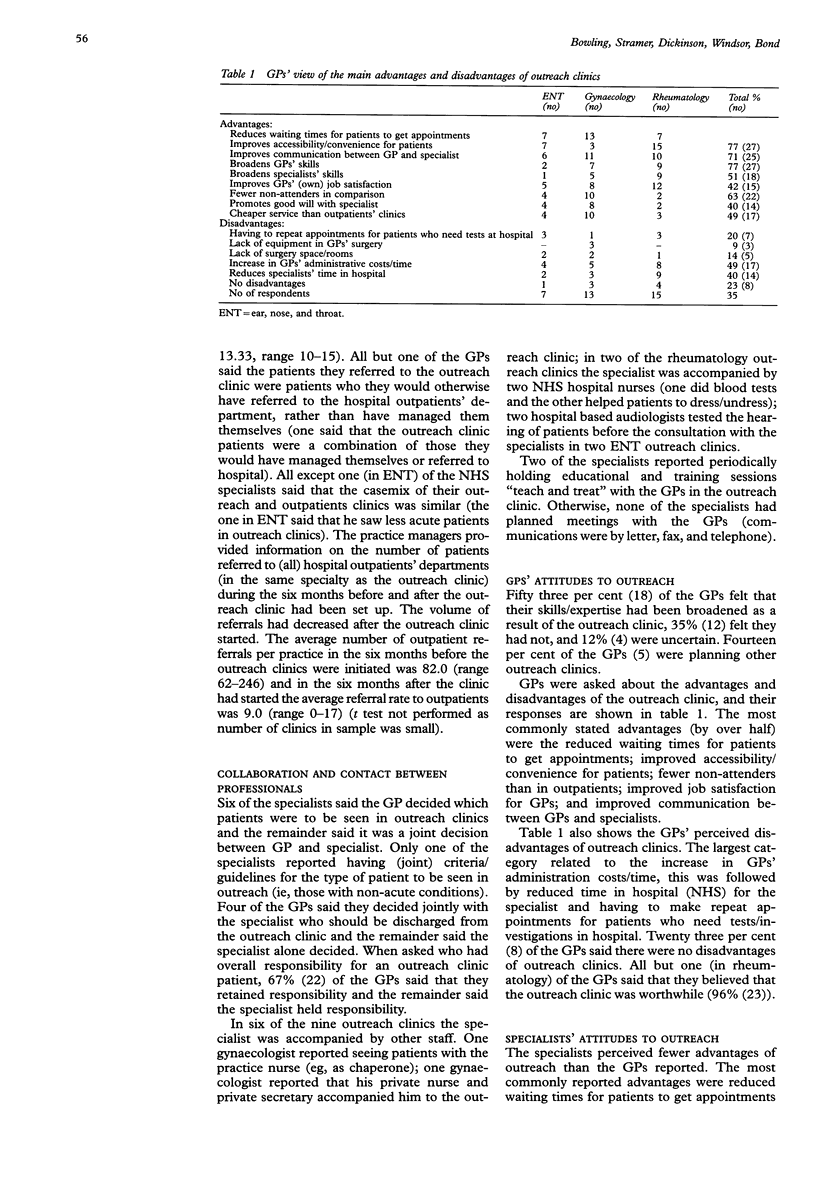
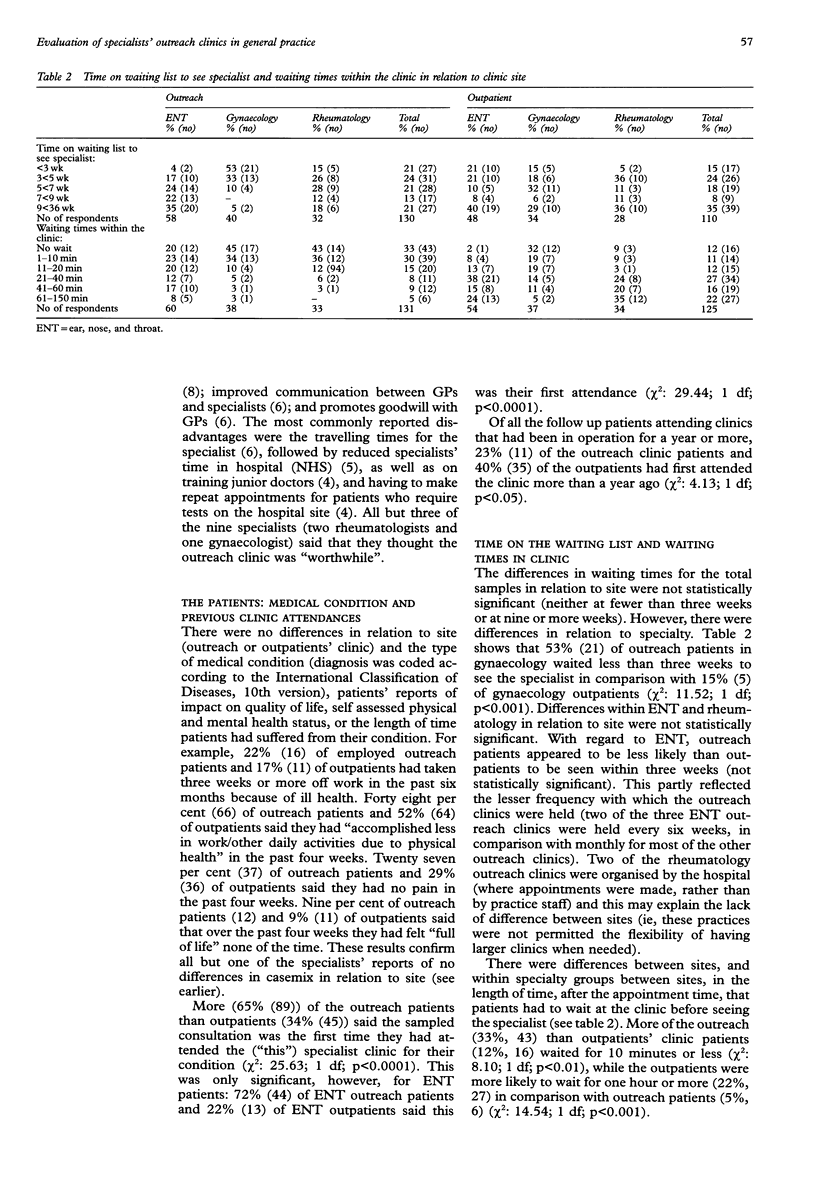
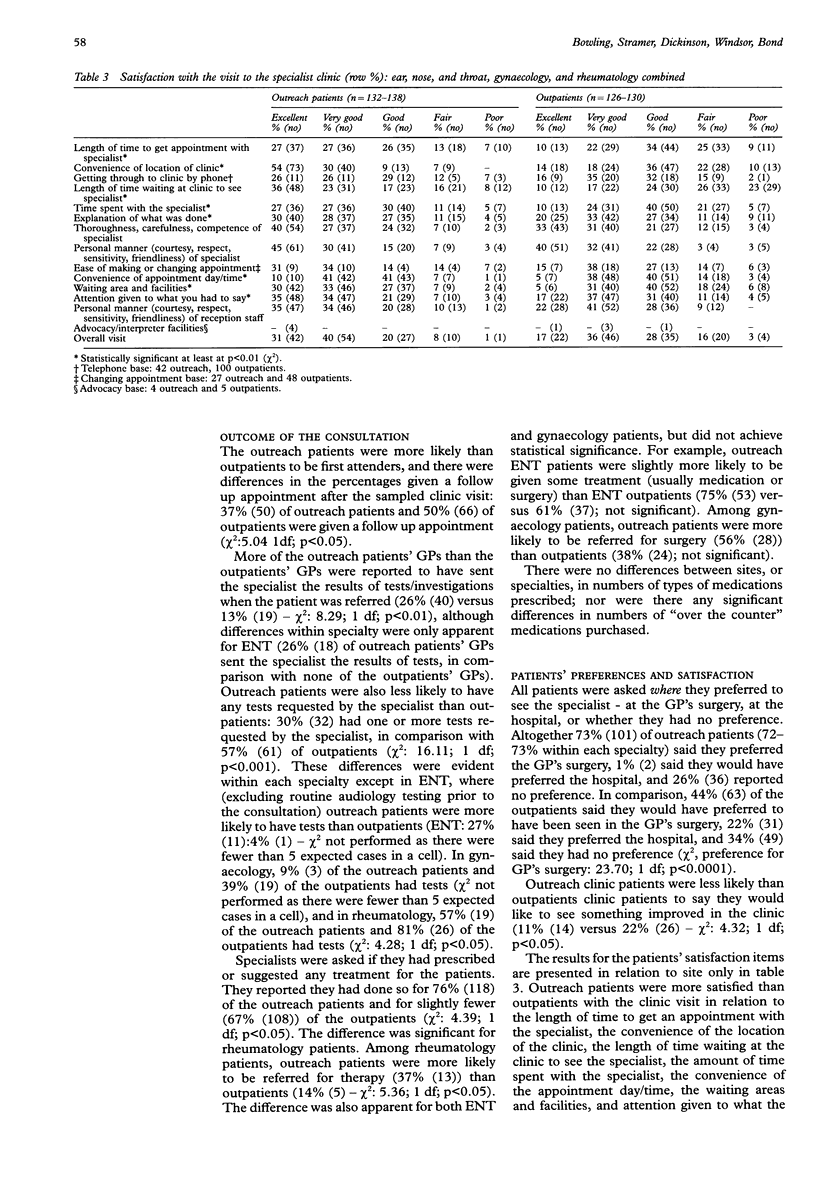
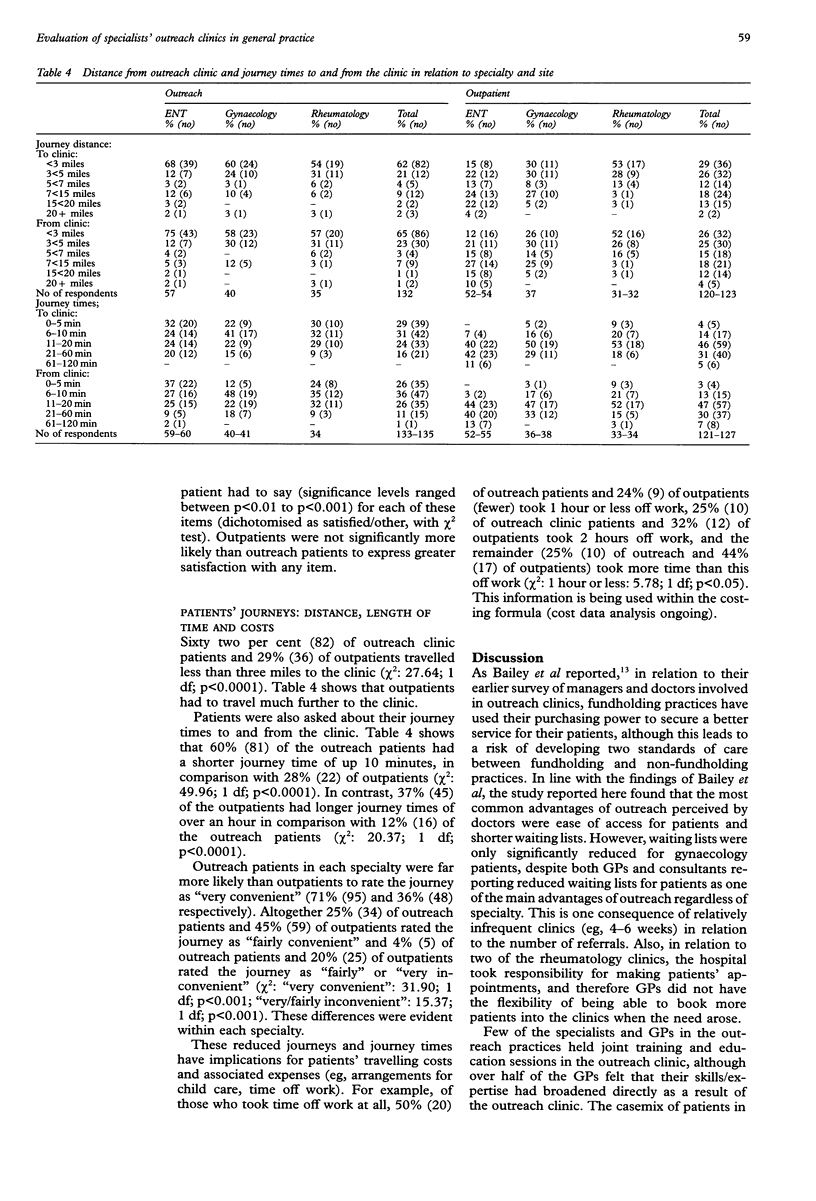
OBJECTIVES: The wider study aimed to evaluate specialists' outreach clinics in relation to their costs, processes, and effectiveness, including patients' and professionals' attitudes. The data on processes and attitudes are presented here. DESIGN: Self administered questionnaires were drawn up for patients, their general practitioners (GPs) and specialists, and managers in the practice. Information was sought from hospital trusts. The study formed a pilot phase prior to a wider evaluation. SETTING: Nine outreach clinics in general practices in England, each with a hospital outpatient department as a control clinic were studied. SUBJECTS: The specialties included were ear, nose, and throat surgery; rheumatology; and gynaecology. The subjects were the patients who attended either the outreach clinics or hospital outpatients clinics during the study period, the outreach patients' GPs, the outreach patients' and outpatients' specialists, the managers in the practices, and the NHS trusts which employed the specialists. MAIN OUTCOME MEASURES: Process items included waiting lists, waiting times in clinics, number of follow up visits, investigations and procedures performed, treatment, health status, patients' and specialists' travelling times, and patients' and doctors' attitudes to, and satisfaction with, the clinic. RESULTS: There was no difference in the health status of patients in relation to the clinic site (ie, outreach and hospital outpatients' clinics) at baseline, and all but one of the specialists said there were no differences in casemix between their outreach and outpatients' clinics. Patients preferred, and were more satisfied with, care in specialists' outreach clinics in general practice, in comparison with outpatients' clinics. The outreach clinics were rated as more convenient than outpatients' clinics in relation to journey times; those outreach patients in work lost less time away from work than outpatients' clinic patients due to the clinic attendance. Length of time on the waiting list was significantly reduced for gynaecology patients; waiting times in clinics were lower for outreach patients than outpatients across all specialties. In addition, outreach patients were more likely to be first rather than follow up attenders; rheumatology outreach patients were more likely than hospital outpatients to receive therapy. GPs' referrals to hospital outpatients' clinics were greatly reduced by the availability of outreach clinics. Both specialists and GPs saw the main advantages of outreach clinics in relation to the greater convenience and better access to care for patients. Few of the specialists and GPs in the outreach practices held formal training and education sessions in the outreach clinic, although over half of the GPs felt that their skills/expertise had broadened as a result of the outreach clinic. CONCLUSIONS: The processes of care (waiting times, patient satisfaction, convenience to patients, follow up attendances) were better in outreach than in outpatients' clinics. However, waiting lists were only significantly reduced for gynaecology patients, despite both GPs and consultants reporting reduced waiting lists for patients as one of the main advantages of outreach. Whether these improvements merit the increased cost to the specialists (in terms of their increased travelling times and time spent away from their hospital base) and whether the development of what is, in effect, two standards of care between practices with and without outreach can be stemmed and the standard of care raised in all practices (eg, by sharing outreach clinics between GPs in an area) remain the subject of debate. As the data were based on the pilot study, the results should be viewed with some caution, although statistical power was adequate for comparisons of sites if not specialties.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bailey J. J., Black M. E., Wilkin D. Specialist outreach clinics in general practice. BMJ. 1994 Apr 23;308(6936):1083–1086. doi: 10.1136/bmj.308.6936.1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beardshaw V., Gordon P., Plamping D. Primary care development zones. BMJ. 1993 Jan 30;306(6873):323–325. doi: 10.1136/bmj.306.6873.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowling A., Jacobson B., Southgate L., Formby J. General practitioners' views on quality specifications for "outpatient referrals and care contracts". BMJ. 1991 Aug 3;303(6797):292–294. doi: 10.1136/bmj.303.6797.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowling A. What things are important in people's lives? A survey of the public's judgements to inform scales of health related quality of life. Soc Sci Med. 1995 Nov;41(10):1447–1462. doi: 10.1016/0277-9536(95)00113-l. [DOI] [PubMed] [Google Scholar]
- Creed F., Marks B. Liaison psychiatry in general practice: a comparison of the liaison-attachment scheme and shifted outpatient clinic models. J R Coll Gen Pract. 1989 Dec;39(329):514–517. [PMC free article] [PubMed] [Google Scholar]
- Dornan C., Fowler G., Mann J. I., Markus A., Thorogood M. A community study of diabetes in Oxfordshire. J R Coll Gen Pract. 1983 Mar;33(248):151–155. [PMC free article] [PubMed] [Google Scholar]
- Goldberg D., Jackson G. Interface between primary care and specialist mental health care. Br J Gen Pract. 1992 Jul;42(360):267–269. [PMC free article] [PubMed] [Google Scholar]
- Grace J. F., Armstrong D. Reasons for referral to hospital: extent of agreement between the perceptions of patients, general practitioners and consultants. Fam Pract. 1986 Sep;3(3):143–147. doi: 10.1093/fampra/3.3.143. [DOI] [PubMed] [Google Scholar]
- Harris A. Specialist outreach clinics. BMJ. 1994 Apr 23;308(6936):1053–1053. doi: 10.1136/bmj.308.6936.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hull F. M., Westerman R. F. Referral to medical outpatients department at teaching hospitals in Birmingham and Amsterdam. Br Med J (Clin Res Ed) 1986 Aug 2;293(6542):311–314. doi: 10.1136/bmj.293.6542.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss F., McNicol M. Secondary care beyond Tomlinson: an opportunity to be seized or squandered? BMJ. 1992 Nov 14;305(6863):1211–1214. doi: 10.1136/bmj.305.6863.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parkerson G. R., Jr, Broadhead W. E., Tse C. K. The Duke Severity of Illness Checklist (DUSOI) for measurement of severity and comorbidity. J Clin Epidemiol. 1993 Apr;46(4):379–393. doi: 10.1016/0895-4356(93)90153-r. [DOI] [PubMed] [Google Scholar]
- Strathdee G., Williams P. A survey of psychiatrists in primary care: the silent growth of a new service. J R Coll Gen Pract. 1984 Nov;34(268):615–618. [PMC free article] [PubMed] [Google Scholar]
- Sullivan F. M., Hoare T., Gilmour H. Outpatient clinic referrals and their outcome. Br J Gen Pract. 1992 Mar;42(356):111–115. [PMC free article] [PubMed] [Google Scholar]


