Abstract
This study aimed to compare the peri-procedural success and complication rate within a large registry of intra-cardiac echocardiography (ICE)- vs. transesophageal echocardiography (TEE)-guided left atrial appendage occlusion (LAAO) procedures with a Watchmann FLX device. Data from 772 LAAO procedures, performed at 26 Italian centers, were reviewed. Technical success was considered as the final implant of a Watchmann FLX device in LAA; the absence of pericardial tamponade, peri-procedural stroke and/or systemic embolism, major bleeding and device embolization during the procedure was defined as a procedural success. One-year stroke and major bleeding rates were evaluated as outcome. ICE-guided LAA occlusion was performed in 149 patients, while TEE was used in 623 patients. Baseline characteristics were similar between the ICE and TEE groups. The technical success was 100% in both groups. Procedural success was also extremely high (98.5%), and was comparable between ICE (98.7%) and TEE (98.5%). ICE was associated with a slightly longer procedural time (73 ± 31 vs. 61.9 ± 36 min, p = 0.042) and shorter hospital stay (5.3 ± 4 vs. 5.8 ± 6 days, p = 0.028) compared to the TEE group. At one year, stroke and major bleeding rates did not differ between the ICE and TEE groups. A Watchmann FLX device showed high technical and procedural success rate, and ICE guidance does not appear inferior to TEE.
Keywords: intra-cardiac, transesophageal, echocardiography, left atrial appendage occlusion
1. Introduction
Atrial fibrillation (AF) is the most common cardiac arrhythmia, affecting 3–5% of people older than 65 years [1,2]. Oral anticoagulation is mandatory in patients with AF in order to minimize the risk of thromboembolic events. Nevertheless, nearly 40% of patients at risk of stroke do not receive any form of oral anticoagulation in the real world [3,4,5]. Percutaneous left atrial appendage occlusion (LAAO) has been demonstrated as a viable alternative for thromboembolic event prevention in patients with absolute/relative contraindications to (novel) oral anticoagulants (NOACs) [6]. The procedural safety of LAAO is a key element, as it may affect the procedural results and patient follow-up. It is also crucial in order to propose a similar procedure as an alternative to NOACs also in patients that can tolerate NOACs. Many elements may affect procedural safety. Significant advances have been registered within intra-procedural imaging and technological improvements of the dedicated devices.
In last years, new devices or new versions of past devices have emerged. Watchman FLX represents an upgrade of the Watchman family devices. In comparison to the old version of the device, Watchman FLX has greater flexibility and reduced height, with a higher number of anchoring elements, improved fabric coverage and a closed distal end. All these modifications are aimed for an easier implantation, safer recapture and repositioning, with the potential for reduction in the follow-up of device-related thrombosis and peri-device leaks. The high flexibility of the device permits for a significant oversize (in order to limit the device embolization risk), without increasing the risk of perforation. Watchmann FLX has demonstrated optimal safety and efficacy results, with a low rate of procedural complications.
On the other hand, intra-procedural imaging may significantly affect procedural outcome. The optimal way to guide an LAAO procedure has not been completely defined. The use of fluoroscopy without other imaging modality should be strongly discouraged, as it is inadequate for a detailed guidance of an LAAO procedure. Transesophageal echocardiography (TEE) has been the most common imaging modality adopted for LAAO guidance. It is well known by many cardiologists in the context of standardized imaging and optimal visualization of the LAA, atrial septum, left and right atria. Nevertheless, the needed general anesthesia and dedicated operator are two main limits of TEE use. Moreover, interference with fluoroscopy, as well as the potential for upper gastrointestinal tract damage, is another factor that may affect TEE use. Intra-cardiac echocardiography (ICE) has been developed as an alternative to TEE for LAAO procedure guidance. ICE probes are commonly advanced through the right femoral vein, and positioned close to the structure of interest for an LAAO in the right and, after transeptal puncture, in the left atria.
Available data suggest that ICE is not inferior to TEE for guiding LAAO procedures, both for immediate results (procedural success and peri-procedural complications) and long-term patient outcomes [7,8,9]. A large registry has specifically demonstrated that the Amulet device implantation under ICE guidance is not inferior to TEE in terms of procedural safety and patient outcomes [10].
In the present work, we aim to compare ICE to TEE guidance for an LAAO procedure within a large Italian registry of LAAO procedures performed with the Watchmann FLX device.
2. Methods
2.1. Study Population
We prospectively enrolled 772 patients that underwent LAA occlusion procedures at 26 Italian centers, between October 2018 and September 2021. Procedural and follow-up data were collected. Patients with non-valvular atrial fibrillation, a CHA2DS2-VASc score ≥ 2 and relative/absolute contra-indication for NOACs were included. The CHA2DS2-VASc [11] and HAS-BLED [12] scores were calculated. Informed consent was collected from each patient. The local ethics Committee “(Comitato Etico Area Vasta Nord Ovest)” approved this study.
2.2. Device and Implantation Procedure
All procedures were performed with the Watchmann FLX device (Boston Scientific, Marlborough, MA, USA). The device was recapturable and repositionable at any moment. A higher number of open-frame cells increases device conformability, while a closed end facilitates device implantation when the length of the LAA is limited (minimum required length is 50% of the device size). The risk of perforation is limited by the presence of an atraumatic distal end with a fluoroscopic marker. This design permits for device advancement within the LAA when partially exposed in a “ball” configuration. Still, the polyester fabric coverage has been extended to minimize peri-device leaks. The device is available in five sizes, namely 20, 24, 27, 31 and 35 mm for LAA ostia sizes ranging from 14 mm to 31.5 mm.
Preprocedural evaluation and planning was performed with transesophageal echocardiography (TEE) or cardiac computed tomography (CT), according to the local practice. LAA dimensions and morphology were evaluated, as well as the morphology of intertribal septum and fossa ovalis. The landing zone (LZ) was measured at the LAA ostium, from the level of the circumflex coronary artery to a point 1-to-2 cm distal to the left upper pulmonary vein ridge. Three-dimensional reconstruction was used. The device sizing was selected according to the maximal LAA LZ diameter, with target oversizing between 10% and 30%. Patients with LAA thrombosis were excluded.
TEE or ICE were used during the procedure for guidance of the different phases, namely transseptal puncture, LAA morphology and size reevaluation, LAA incanulation, device delivery and implantation (after an assessment of the position and stability, leak absence). Procedural complications were promptly evaluated. TEE procedures required general anesthesia. ICE procedures required an adjunctive ipsilateral femoral vein access and were performed under local anesthesia. An alternative use of ICE or TEE was left to the operator discretion and TEE/ICE availability.
For optimal ICE guidance, an ICE probe was advanced into the left atrium during every ICE-guided procedure, through the first transseptal puncture, as described elsewhere.
Technical success was defined as the final deployment of the device inside an LAA, fully meeting the PASS criteria (position: device at the LAA ostium; anchor: fixation anchors engaged/stable device; size: 8 to 20% device compression; seal: device spans the ostium, all lobes covered). Procedural success was defined as technical success without major procedure-related complications (pericardial tamponade requiring drainage, stroke, systemic embolism, major bleeding and device embolization requiring surgical removal, absence of a final leak > 5 mm). Major bleedings were defined according to the International Society on Thrombosis and Haemostasis criteria [12]. Events were labeled as peri-procedural if they occurred within 7 days of the procedure or pre-discharge.
2.3. Follow-Up
Follow-up was performed by clinical visits or telephonic follow-up. No oral anticoagulation therapy was administered after the procedure. Different pharmacological schemes were adopted after the procedure. The most common scheme included dual antiplatelet therapy with aspirin (100 mg/die) plus clopidogrel (75 mg/24 h) for 30 to 180 days after the procedure. According to operators’ discretion, in patients with high bleeding risk, a single antiplatelet agent was prescribed with/without adjunction of a prophylactic dose of low-molecular-weight heparin for the first month after the implant procedure.
Stroke, transitory ischemic attacks (TIA), systemic embolism, major/minor hemorrhage and death from cardiac or any cause were considered as events. Patients that had a one year follow-up were considered for the outcome analysis.
2.4. Statistical Analysis
Continuous data were expressed as the mean ± standard deviation. The procedural success rate was calculated as a percentage over the total number of procedures. For proportions, numbers and percentages were used. The differences between TEE and ICE groups were evaluated with the Student t-test for continuous variables. Binary logistic regression analysis was used to evaluate the occurrence of complications in the TEE and ICE groups, respectively. The odds ratios and 95% confidence intervals were calculated. Events curves were analyzed using the Kaplan–Meier estimate. The differences in survival curves were tested with a log-rank test. Statistical analysis was performed using SPSS® (version 19, SPSS, Chicago, IL, USA). A p-value less than 0.05 was considered significant.
3. Results
3.1. Patient Population
The baseline characteristics, as well indications for LAAO, are displayed in Table 1 (overall population, TEE and ICE groups, respectively).
Table 1.
Clinical details of patients undergoing an ICE- or TEE-guided LAAO procedure.
| Patient | ALL (n = 772) | ICE (n = 149) | TEE (623) | p |
|---|---|---|---|---|
| Age | 76.5 ± 8.3 | 77 ± 7.5 | 76.3 ± 8 | ns |
| Male, % | 509 (65%) | 97 (65%) | 407 (65%) | ns |
| CHA2DS2VASC | 4.14 ± 1.47 | 4.2 ± 1.8 | 4.1 ± 1.4 | ns |
| HASBLED | 3.69 ± 1.1 | 3.5 ± 1.4 | 3.7 ± 1.1 | ns |
| Creatinine | 1.4 ± 1 | 1.3 ± 1.1 | 1.44 ± 1.2 | ns |
| eGFR | 59 ± 30 | 60 ± 28 | 58.4 ± 28 | ns |
| LVEF | 52 ± 10 | 54 ± 11 | 51 ± 11 | ns |
| BMI | 26.5 ± 3 | 26 ± 4 | 26.7 ± 4.4 | ns |
| Permanent AF, % | 376 (48%) | 72 (48%) | 304 (48%) | ns |
| Diabetes | 264 (33%) | 45 (30%) | 219 (34%) | ns |
| Arterial hypertension | 606 (78%) | 115 (77%) | 491 (78%) | ns |
| Previous stroke | 106 (13%) | 19 (12%) | 87 (13%) | ns |
| GI bleeding | 240 (30%) | 40 (26%) | 200 (31%) | ns |
| Intra-cranial/subdural bleeding | 115 (14%) | 25 (16%) | 90 (14%) | ns |
| Severe CKD | 126 (16%) | 18 (12%) | 108 (17%) | ns |
| Hematologic disorder | 102 (13%) | 28 (18%) | 74 (11%) | 0.038 |
| Ischemic stroke in OACs | 54 (7%) | 8 (5.5%) | 46 (7.3%) | ns |
| DAPT+OACs | 7 (0.9%) | 2 (1.3%) | 5 (0.8%) | ns |
| Very high bleeding risk | 122 (15%) | 25 (16%) | 97 (15%) | ns |
AF: atrial fibrillation; BMI: body mass index; CKD: chromic kidney disease; DAPT: dual antiplatelet therpy; GFR: glomerular filtration rate; GI: gastrointestinal; ICE: intra-cardiac echocardiography; LAAO: left atrial appendage occlusion; LVEF: left ventricular ejection fraction; OACs: oral anticoagulants; TEE: transesophageal echocardiography.
Of the total of 772 procedures, ICE-guided LAA occlusion was performed in 149 patients, while TEE was used in 623 patients. Clinical characteristics and indications for the procedure were similar between the groups, but patients in the ICE group had a higher prevalence of hematologic disorders. About 50% of the patients had a permanent AF, without any difference between TEE and ICE patients. CHA2DS2-VASc was 4.1 and HAS-BLED 3.6, with no differences between TEE and ICE patients. Of patients, 91% in the TEE group and 8% of ICE patients underwent pre-procedural three-dimensional TEE, while pre-procedural CCT was performed in 10% of the patients in the TEE group and 94% of ICE patients, respectively.
3.2. Procedural Results and In-Hospital Outcomes
Table 2 shows procedural characteristics, complication rate and in-hospital outcomes across the entire population and within the TEE and ICE groups, respectively.
Table 2.
Procedural details of the TEE- or ICE-guided LAAO procedures, respectively.
| ALL | ICE | TEE | p | |
|---|---|---|---|---|
| Patients | 772 | 149 | 623 | |
| Pericardial effusion | 15 (1.9%) | 3 (2%) | 12 (1.9%) | NS |
| Pericardial tamponade | 4 (0.5%) | 1 (0.55%) | 3 (0.47%) | NS |
| Stroke | 2 (0.25%) | 0 (0%) | 2 (0.31%) | NS |
| TIA | 1 (0.13%) | 0 (0%) | 1 (0.15%) | NS |
| Device embolization | 0 (0%) | 0 (0%) | 0 (0%) | NS |
| Peri-device leak > 5 mm | 0 (0%) | 0 (0%) | 0 (0%) | NS |
| Major bleeding | 5 (0.6%) | 1 (0.6%) | 4 (0.63%) | NS |
| Death | 0 (0%) | 0 (0%) | 0 (0%) | NS |
| Technical success | 772 (100%) | 149 (100%) | 623 (100%) | NS |
| Procedural success | 763 (98.5%) | 147 (98.7%) | 616 (98.5%) | NS |
| Fluoroscopy time | 18.7 ± 14 | 24 ± 15 | 17 ± 13 | 0.031 |
| Procedure time | 63.8 ± 34 | 73 ± 31 | 61.9 ± 36 | 0.042 |
| Contrast volume | 92.11 ± 58 | 107 ± 53 | 88 ± 59 | 0.071 |
| In-hospital stay (days) | 5.6 ± 5 | 5.3 ± 4 | 5.8 ± 6 | 0.028 |
ICE: intra-cardiac echocardiography; LAAO: left atrial appendage occlusion; TIA: transitory ischemic attack; TEE: transesophageal echocardiography.
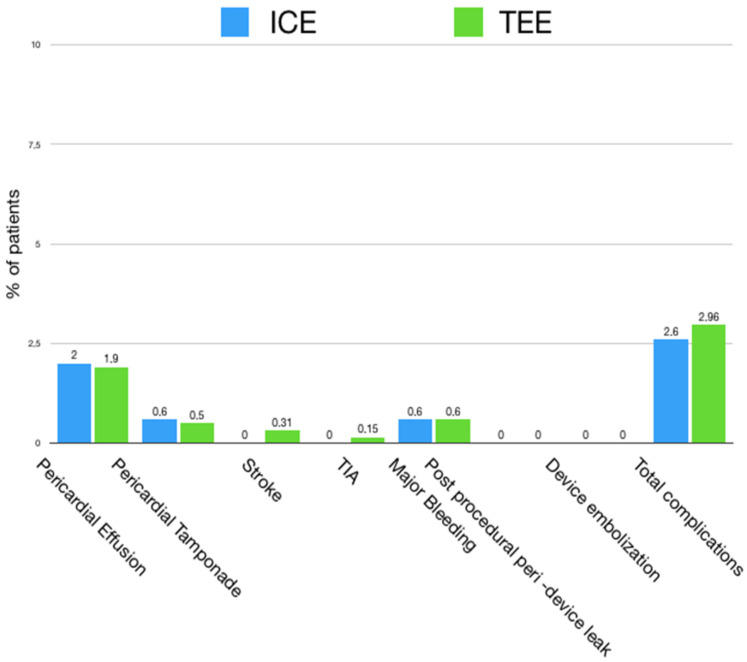
The use of ICE was associated with longer procedural (73 ± 31 vs. 61.9 ± 36 min, p = 0.042) and fluoroscopy times (24 ± 15 vs. 17 ± 13 min, p = 0.031) in comparison to the ICE group. On the other side ICE patients had shorter hospital stay (5.3 ± 4 vs. 5.8 ± 6 days, p = 0.028). No differences in the number of attempts for device positioning, as well as the number of device opened, were assessed between the ICE and TEE groups. The overall technical success was 100%, with the final fully meeting the PASS criteria for all procedures. Procedural success was similarly high, with no differences between the TEE (98.5%) and ICE (98.7%) groups and a complication rate of 1.5% for the TEE vs. 1.3% for the ICE, respectively. The most common complication was major pericardial effusion for both groups, followed by major bleeding. Of the pericardial effusions, 25% required drainage, 0.55% in the ICE group and 0.47% in the TEE group. Any case of device embolization was reported, as well as any case of peri-device leak > 5 mm that occurred. Procedural complications in the ICE- vs. TEE-guided procedure groups are visualized in Figure 1.
Figure 1.
Procedural complications for ICE- (light blue) vs. TEE (green)-guided LAAO procedures. ICE: intra-cardiac echocardiography; LAAO: left atrial appendage occlusion; TEE: transesophageal echocardiography, TIA: transient ischemic attack.
3.3. Follow-Up
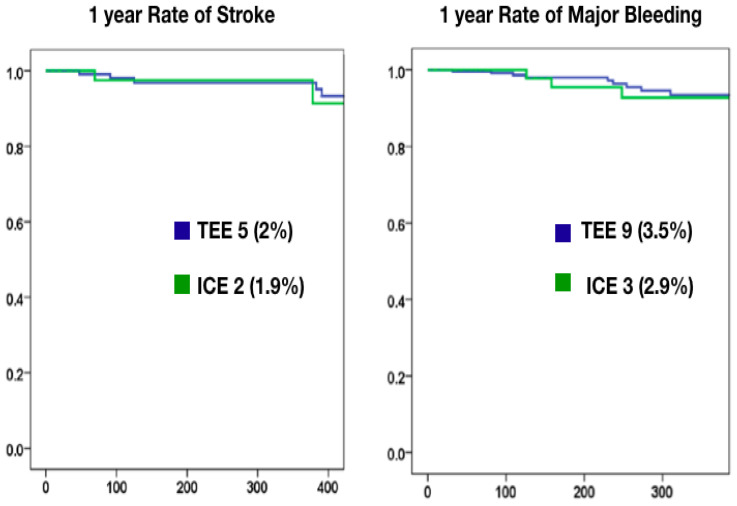
One year follow-up data were available for 342 patients, with 102 in the ICE group. The rate of stroke (1.9% in the ICE group vs. 2% in the TEE group, p = ns) and major bleeding (2.9% in the ICE group vs. 3.7% in the TEE group) were similar between the ICE and TEE groups (Figure 2, Table 3).
Figure 2.
Kaplan–Meier curves at one year for stroke (left) and major bleeding (right) for ICE- vs. TEE-guided LAAO procedures. ICE: intra-cardiac echocardiography; LAAO: left atrial appendage occlusion; TEE: transesophageal echocardiography.
Table 3.
One year follow-up results in patients that underwent an ICE- or TEE-guided LAAO procedure.
| ALL (n = 342) | ICE (n = 102) | TEE (n = 240) | p | |
|---|---|---|---|---|
| Stroke | 7 (2%) | 2 (1.9%) | 5 (2%) | NS |
| TIA | 2 (0.5%) | 0 (0%) | 2 (0.8%) | NS |
| Death | 11 (3.2%) | 3 (2.9%) | 8 (3.3%) | NS |
| Major bleeding | 12 (3.5%) | 3 (2.9%) | 9 (3.7%) | NS |
ICE: intracardiac echocardiography; LAAO: left atrial appendage occlusion; TIA: transitory ischemic attack; TEE: transesophageal echocardiography.
4. Discussion
This large, multicenter, Italian registry on LAA occlusion with a Watchman FLX device has two main messages: (a) a Watchman FLX device ensures high procedural safety and technical success; (b) ICE intra-procedural guidance for LAA occlusion does not appear to be inferior to TEE in terms of procedural complications and one year follow-up outcomes.
In the last 20 years, LAAO has been demonstrated as a viable alternative to (N)OACS in NVAF patients with absolute/relative contraindications to anticoagulation. Specifically, LAA occlusion reduces about 70% of the rate of cerebral embolism as compared to historical NVAF populations without OAC, at the same time warranting a 60% reduction in the rate of hemorrhagic events as compared to historical populations under OAC treatment [13].
In this context, procedural safety is a key element. LAAO history has been characterized by progressive amelioration of the procedural safety profile, making LAAO more attractive. A low rate of procedural complications is crucial in order to implement LAAO in current clinical practice as a potential alternative to NOACs, also in patients who could tolerate this therapy.
Two main procedural aspects need full consideration regarding procedural safety. The first element is about technical equipment and, specifically, the device. Different devices have been developed. The Watchmann family devices have been the most studied devices both, in randomized trials [14] and registries [6]. Watchman FLX is the last version of this family of devices, which has been developed with the intent to optimize procedural results in comparison to its previous version and other devices. Thanks to its improved flexibility and reduced height, this device has a wide range of size adaptations, allowing for a high grade of oversize without affecting the procedural safety. This characteristic, along with the presence of an additional row of 18 J-shaped anchors, has the advantage of minimizing the risk of device embolization, with any case of device embolization in the present registry. Still, the flexibility and closed distal end simplify implantation, allowing for full and safe recapture and repositioning. The device full coverage, finally, is intended to reduce peri-device leaks and device-related thrombosis.
The second main aspect for improving procedural safety lays on accurate pre- and intra-procedural imaging. Pre-procedural-computed tomography or 3D high-quality TEE are essential. They inform about interatrial septum anatomy and its spatial relationship with the LAA (in order to optimize transseptal puncture), and must give full elucidation of LAA morphology. LAA has a wide variety of anatomical aspects, width of its neck, length, orientation and the presence of additional lobes must be fully analyzed before the procedure.
Intra-procedural imaging guides the procedure, from transeptal puncture to the device implantation and final assessment. TEE has historically been considered the gold standard for intra-procedural guidance. TEE certainly has a high definition of the right and left atria, atrial septum and left atrial appendage anatomy, and it is an imaging modality that is well known by many invasive cardiologists with largely standardized imaging. Nevertheless TEE may be affected by some limitations. First, TEE requires general anesthesia with a longer patient turnover and increased procedural time, implying the presence of an anesthesiologist. Still, general anesthesia may be harmful in fragile patients and may require intensive care monitoring after the procedure. Finally, TEE and endotracheal intubation may contribute to complications such as the injuries and bleeding of gastroesophageal and respiratory tract, laryngospasm and bronchospasm. requiring additional intervention and prolonged hospitalization [15]. ICE has been proposed as an alternative to TEE for LAA occlusion procedure guidance, and its use has been validated in large cohorts of patients. It has been demonstrated that even if ICE may result in an inferior image quality, this does not affect the procedural success and patient outcomes. What is crucial to implement for ICE use, along with the quality of pre-procedural evaluation, is placement of the ICE probe in left atrium (through the same transseptal puncture performed for device positioning). With the ICE probe in the left atrium, imaging quality is not inferior or even superior to TEE [16].
In this registry, ICE did not appear inferior to TEE in terms of procedural safety and follow-up results, using a very-well-performing device. The procedural success appears to be extremely high. In particular, the absence of device embolization and peri-device major leaks attest the high performance of this device, not affected by the choice of ICE or TEE guidance. TEE has lower fluoroscopy time, procedural time and contrast volume vs. ICE in this registry. These differences are likely linked to a higher standardization and operators experience with TEE guidance. A longer procedural time may be reduced in the future by higher operator experience, and, in any case, is counterbalanced by a lower cathlab turnover time and less invasiveness than ICE.
Still, one year thromboembolic and hemorrhagic event rates are extremely low, both in the ICE and TEE groups, if related to the CHA2DS2-VASc and HAS-BLED scores of the studied population.
These considerations pave the way for broader indications for an LAAO procedure. First, randomized trials are ongoing, evaluating the comparison between novel anticoagulants and LAAO. The results are awaited in the next months, and it is likely that many patients could also tolerate oral anticoagulant therapy, a potential candidate for LAAO. In this context, there is potential for a larger use of a combined procedure of LAAO and AF ablation. Patients that undergo AF ablation are also natural candidates to LAAO if this procedure shows good safety and efficacy [17].
As for many other fields of clinical practice, it is likely that artificial intelligence will impact on the indications and the way cardiac structural intervention performance. Some experience of pre-procedural planning and procedure simulation driven by artificial intelligence has been already published for LAAO [18,19]. In the future, artificial intelligence systems will have a key role in every aspect of patient care, from accurate patients selection, suggestion of best device and best imaging modality choice, with fine and accurate prediction of procedural results and patient outcomes.
5. Study Limitations
The main limitation of this study is the lack of randomization between ICE and TEE use. In this series, ICE was used mainly at centers with a high volume of LAA occlusion procedures. Follow-up data were available only for patients that achieved 1 year follow-up, which is actually about half of the study population. The study is largely underpowered to draw a definite conclusion about the follow-up.
6. Conclusions
A Watchmann FLX device has very high technical and procedural success rates. ICE guidance does not appear inferior to TEE in terms of procedural results and outcomes.
Abbreviations
| CCT | Cardiac computed tomography |
| ICE | Intra-cardiac echocardiography |
| LAAO | Left atrial appendage occlusion |
| NVAF | Non-valvular atrial fibrillation |
| OACs | Oral anticoagulants |
| TIA | Transitory ischemic attacks |
| TEE | Transesophageal echocardiography |
Author Contributions
L.E.P.: data collection, manuscript first draft writing. C.T. (Claudio Tondo): data collection, manuscript review; G.F.: data collection, manuscript review; A.N.: data collection, manuscript review; F.R.: data collection, manuscript review; M.C. (Marco Contarini): data collection, manuscript review; G.G.: data collection, manuscript review; C.G.: data collection, manuscript review; G.C. (Gavino Casu): data collection, manuscript review; M.R.R.: data collection database organization, statistical analysis; P.M.: data collection, manuscript review; L.L.: data collection, manuscript review; G.C. (Giuseppe Caramanno): data collection, manuscript review; S.G.: data collection, manuscript review; P.P.: data collection, manuscript review; M.C. (Mauro Chiarito): data collection, manuscript review; C.T. (Corrado Tamburino): data collection, manuscript review; S.B.: database ideation, data collection, supervision of manuscript writing. All authors contributed to data collection at their center, and a national database was completed under the supervision of S.B. and L.E.P., who performed data analysis. The first draft of the manuscript was written by L.E.P., with the supervision of S.B. All authors commented on the previous versions of the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee (protocol code 20205; date of approval 09-09-2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data set may be requested to pastormerlo@ftgm.it.
Conflicts of Interest
Berti is a proctor for Abbott, Boston Scientific and Edwards Lifesciences. The other authors declare that they have no conflicts of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Go A.S., Hylek E.M., Phillips K.A., Chang Y., Henault L.E., Selby J.V., Singer D.E. Prevalence of diagnosed atrial fibrillation in adults: National implications for rhythm management and stroke prevention: The anticoagulation and risk factors in atrial fibrillation (ATRIA) Study. JAMA. 2001;285:2370–2375. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 2.Zoni-Berisso M., Lercari F., Carazza T., Domenicucci S. Epidemiology of atrial fibrillation: European perspective. Clin. Epidemiol. 2014;6:213–220. doi: 10.2147/CLEP.S47385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kakkar A.K., Mueller I., Bassand J.-P., Fitzmaurice D.A., Goldhaber S.Z., Goto S., Haas S., Hacke W., Lip G.Y.H., Mantovani L.G., et al. Risk profiles and antithrombotic treatment of patients newly diagnosed with atrial fibrillation at risk of stroke: Perspectives from the international, observational, prospective GARFIELD registry. PLoS ONE. 2013;8:e6347. doi: 10.1371/journal.pone.0063479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marini C., De Santis F., Sacco S., Russo T., Olivieri L., Totaro R., Carolei A. Contribution of Atrial Fibrillation to Incidence and Outcome of Ischemic Stroke: Results From a Population-Based Study. Stroke. 2005;36:1115–1119. doi: 10.1161/01.STR.0000166053.83476.4a. [DOI] [PubMed] [Google Scholar]
- 5.Hart R.G., Pearce L.A., Aguilar M.I. Meta-analysis: Antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann. Intern. Med. 2007;146:857–867. doi: 10.7326/0003-4819-146-12-200706190-00007. [DOI] [PubMed] [Google Scholar]
- 6.Boersma L.V., Ince H., Kische S., Pokushalov E., Schmitz T., Schmidt B., Gori T., Meincke F., Protopopov A.V., Betts T., et al. Efficacy and safety of left atrial appendage closure with WATCHMAN in patients with or without contraindication to oral anticoagulation: 1-Year follow-up outcome data of the EWOLUTION trial. Heart Rhythm. 2017;14:1302–1308. doi: 10.1016/j.hrthm.2017.05.038. [DOI] [PubMed] [Google Scholar]
- 7.Nielsen-Kudsk J.E., Berti S., De Backer O., Aguirre D., Fassini G., Cruz-Gonzalez I., Grassi G., Tondo C. Use of Intracardiac Compared with Transesophageal Echocardiography for Left Atrial Appendage Occlusion in the Amulet Observational Study. JACC Cardiovasc. Interv. 2019;12:1030–1039. doi: 10.1016/j.jcin.2019.04.035. [DOI] [PubMed] [Google Scholar]
- 8.Alkhouli M., Chaker Z., Alqahtani F., Raslan S., Raybuck B. Outcomes of Routine Intracardiac Echocardiography to Guide Left Atrial Appendage Occlusion. JACC Clin. Electrophysiol. 2020;6:393–400. doi: 10.1016/j.jacep.2019.11.014. [DOI] [PubMed] [Google Scholar]
- 9.Ribeiro J.M., Teixeira R., Puga L., Costa M., Gonçalves L. Comparison of intracardiac and transoesophageal echocardiography for guidance of percutaneous left atrial appendage occlusion: A meta-analysis. Echocardiography. 2019;36:1330–1337. doi: 10.1111/echo.14415. [DOI] [PubMed] [Google Scholar]
- 10.Berti S., Pastormerlo L.E., Santoro G., Brscic E., Montorfano M., Vignali L., Danna P., Tondo C., Rezzaghi M., D’Amarigo G., et al. Intracardiac Versus Transesophageal Echocardiographic Guidance for Left Atrial Appendage Occlusion: The LAAO Italian Multicenter Registry. JACC Cardiovasc. Interv. 2018;11:1086–1092. doi: 10.1016/j.jcin.2018.05.008. [DOI] [PubMed] [Google Scholar]
- 11.Lip G.Y., Nieuwlaat R., Pisters R., Lane D.A., Crijns H.J. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: The euro heart survey on atrial fibrillation. Chest. 2010;137:263–272. doi: 10.1378/chest.09-1584. [DOI] [PubMed] [Google Scholar]
- 12.Pisters R., Lane D.A., Nieuwlaat R., de Vos C.B., Crijns H.J., Lip G.Y. A novel user friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: The Euro Heart Survey. Chest. 2010;138:1093–1100. doi: 10.1378/chest.10-0134. [DOI] [PubMed] [Google Scholar]
- 13.Schulman S., Kearon C. Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J. Thromb. Haemost. 2005;3:692–694. doi: 10.1111/j.1538-7836.2005.01204.x. [DOI] [PubMed] [Google Scholar]
- 14.Reddy V.Y., Doshi S.K., Kar S., Gibson D.N., Price M.J., Huber K., Horton R.P., Buchbinder M., Neuzil P., Gordon N.T., et al. 5-Year Outcomes After Left Atrial Appendage Closure: From the PREVAIL and PROTECT AF Trials. J. Am. Coll. Cardiol. 2017;70:2964–2975. doi: 10.1016/j.jacc.2017.10.021. [DOI] [PubMed] [Google Scholar]
- 15.Lennon M.J., Gibbs N.M., Weightman W.M., Leber J., Ee H.C., Yusoff I.F. Transesophageal echocardiographyrelated gastrointestinal complications in cardiac surgical patients. J. Cardiothorac. Vasc. Anesth. 2005;19:135–141. doi: 10.1053/j.jvca.2005.01.020. [DOI] [PubMed] [Google Scholar]
- 16.Korsholm K., Jensen J.M., Nielsen-Kudsk J.E. Intracardiac echocardiography from the Left Atrium for Procedural Guidance of Transcatheter Left Atrial Appendage Occlusion. JACC Cardiovasc. Interv. 2017;10:2198–2206. doi: 10.1016/j.jcin.2017.06.057. [DOI] [PubMed] [Google Scholar]
- 17.Şaylık F., Çınar T., Akbulut T., Hayıroğlu M.İ. Comparison of catheter ablation and medical therapy for atrial fibrillation in heart failure patients: A meta-analysis of randomized controlled trials. Heart Lung. 2023;57:69–74. doi: 10.1016/j.hrtlng.2022.08.012. [DOI] [PubMed] [Google Scholar]
- 18.Michiels K., Heffinck E., Astudillo P., Wong I., Mortier P., Bavo A.M. Automated MSCT Analysis for Planning Left Atrial Appendage Occlusion Using Artificial Intelligence. J. Interv. Cardiol. 2022;2022:5797431. doi: 10.1155/2022/5797431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hayıroğlu M.İ., Altay S. The Role of Artificial Intelligence in Coronary Artery Disease and Atrial Fibrillation. Balkan Med. J. 2023;40:151–152. doi: 10.4274/balkanmedj.galenos.2023.06042023. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data set may be requested to pastormerlo@ftgm.it.