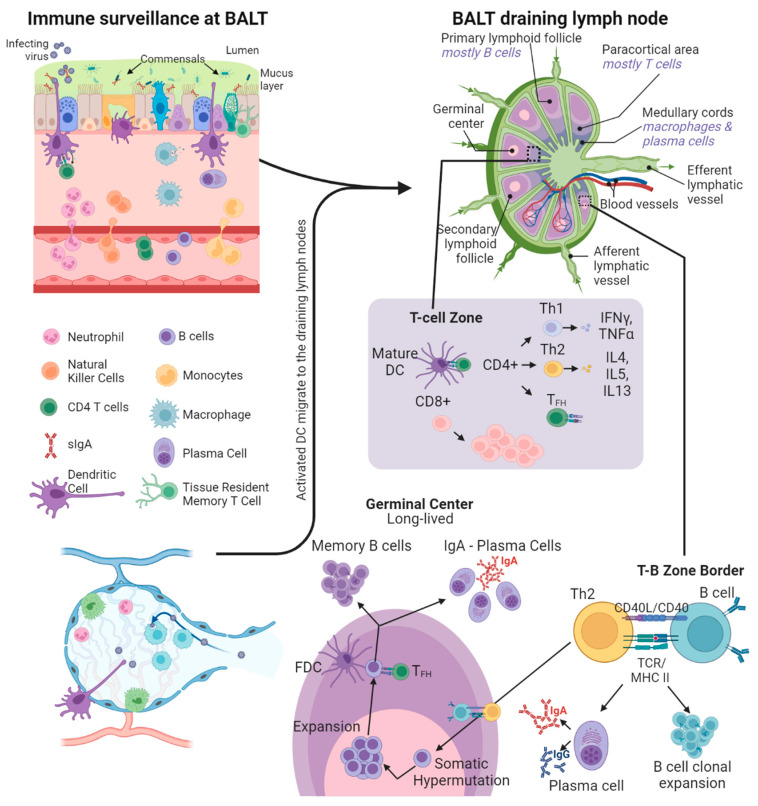
Figure 2.
Immune surveillance at the respiratory mucosa. Within the mucus layer are innate immune factors such as antimicrobial peptides, proteases, complement system factors, and secretory IgA and IgM antibodies. The dendritic cells (DCs) in the airways become activated on antigen capture and traffic to draining lymph nodes via afferent lymphatics. In T cell zones, the DCs present the antigens on MHC class II receptors to CD4+ T cells and on MHC class I receptors to CD8+ T cells, along with CD80/CD86 co-stimulation. This antigen presentation by DCs promotes the maturation and expansion of naive CD4+ and CD8+ T cells. CD4+ T cells with Th1 polarization assist in the maturation of cell-based cytotoxic immune responses, whereas Th2 polarized CD4+ T follicular helper (TFH) cells migrate to the T-B zone border and assist in the maturation of B cells by TCR-MHC II engagement and CD40/CD40L co-stimulation. The T-B cell pairing causes B cell migration to the germinal centers and their clonal expansion. Within the germinal centers, activated B cells (assisted by follicular dendritic cells (FDC) and TFH) undergo somatic hypermutation followed by further expansion. Through this iterative cycle B cells with high affinity to the target antigen are selected, followed by class-switching to either plasma cells or memory B cells, which traffic back to the site of infection in the respiratory mucosa. Created with BioRender.com.