Abstract
Purpose
Nonsuicidal self-injury (NSSI) is related to childhood trauma, negative life events, and coping style, but the interaction among these factors and the mechanism by which they interact in adolescents with depressive disorder remain unclear. This paper explores how these factors interact to influence NSSI and provides evidence to develop prevention efforts and interventions for adolescents with depressive disorder with NSSI.
Patients and Methods
A cross-sectional design and convenient sampling method were used in this study. The Childhood Trauma Questionnaire, Adolescent Self-Rating Life Events Checklist, Trait Coping Style Questionnaire, and Adolescent Nonsuicidal Self-injury Assessment Questionnaire were completed by 540 adolescents with depressive disorder. Descriptive analysis, chi-square tests, t-tests, Pearson correlations, and serial mediation analyses were used in the data analysis.
Results
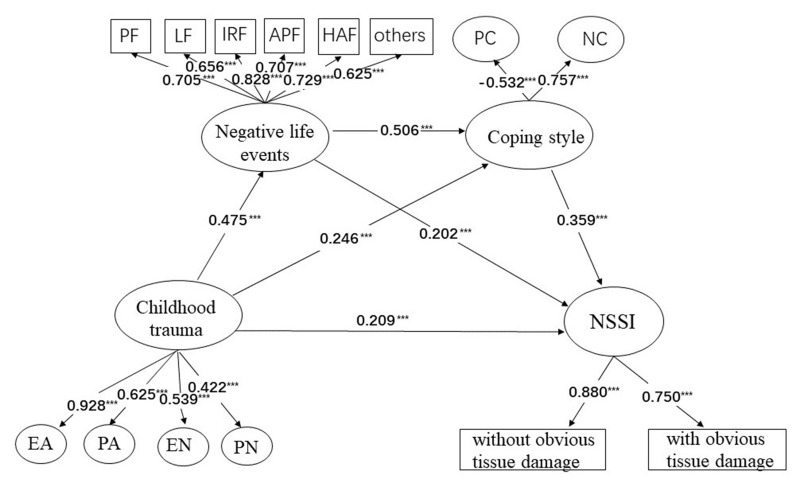
A total of 398 (79.442%) adolescents with depressive disorders reported experiences of NSSI. The results of serial mediation analyses determined that childhood trauma has a direct (estimate = 0.209, 95% CI: 0.063, 0.334) and indirect (estimate = 0.271, 95% CI: 0.199, 0.371) impact on NSSI. The indirect impact of childhood trauma on NSSI through negative life events alone (estimate = 0.096, 95% CI: 0.007, 0.169), coping styles alone (estimate = 0.088, 95% CI: 0.034, 0.183), and negative life events on coping styles (estimate = 0.086, 95% CI: 0.042, 0.162) was significant.
Conclusion
This study demonstrates that screening for childhood trauma should be considered when preventing and treating NSSI behavior in adolescents with depressive disorder. Managing negative life events and coping style may mitigate the negative impact of childhood trauma on NSSI behavior in adolescents with depressive disorder.
Keywords: childhood trauma, NSSI, negative life event, coping styles, depressive disorder
Introduction
Nonsuicidal self-injury (NSSI) behavior is defined as direct, intentional, repeated injury to one’s own tissues and organs without the purpose of suicide, which is not accepted and recognized by society, and it is an important mental health problem for adolescents.1 The first onset of NSSI is usually between the ages of 12 and 14, and it is common in adolescents.2,3 The worldwide prevalence of NSSI in children and adolescents is approximately 19.5%.4 In China, the prevalence of NSSI in adolescents ranges from 11.5% to 41.5%.5 NSSI behavior is rarely manifested in isolation,6 and studies have shown that NSSI behavior and depressive disorders often occur simultaneously.7 The proportion of adolescents with NSSI who have experienced suicidal ideation is up to 70% or more,8 thus, it is considered a significant predictor of suicidal behavior in adolescents.9 Given the high prevalence rate of NSSI among adolescents and its serious effects, identifying high-risk factors for NSSI is important for initiating early preventive interventions.
National and international studies have shown that childhood trauma is an independent risk factor for NSSI behavior, and childhood trauma experience is significantly and positively correlated with the occurrence or frequency of NSSI in adolescents.10–12 Childhood trauma is defined as a substantial or potentially harmful act to the physical or mental health of a child by an individual who has the responsibility or duty to supervise or raise the child, including sexual abuse (SA), physical abuse (PA), emotional abuse (EA), emotional neglect (EN), and physical neglect (PN).13 Childhood trauma is a global problem that not only causes physical and psychological trauma that stays with children throughout their lives, but also imposes a heavy emotional and economic burden on parents, schools, and society. In recent years, reports of childhood trauma have been increasing, and in July 2016, the World Health Organization reported that 1/4 of adults reported PA in childhood, and 1/5 of women and 1/13 of men reported EA in childhood; Devi et al pointed out that EA and PN were the most common types of childhood trauma.14 As opposed to individuals who grew up happily in childhood, individuals who experienced childhood trauma exhibit a variety of psychological and behavioral problems in adulthood, such as anxiety, NSSI, suicide, posttraumatic stress disorder, bulimia, alcohol abuse and substance abuse.15,16 Duke showed that any type of childhood trauma increased the risk of NSSI by 2.7 to 6.1 times.17 A German survey showed that approximately 65% of individuals in the NSSI group had experienced at least one type of childhood trauma, and approximately 50% had experienced multiple types of childhood trauma.18
Increasing evidence suggests that the more negative life events and psychological feelings are experienced by adolescents with depressive disorders, the higher the frequency of NSSI.19 Negative life events refer to psychological stress caused by various problems encountered by individuals in life and unpleasant emotional experiences that have negative effects on individuals, such as anxiety and depression.20 Based on the cumulative adversity model, there is continuity between early adversity and recent stressful life events; on the one hand, childhood trauma experiences can lead to an increasing sensitivity of individuals to adult negative life events, as evidenced by a greater impact at lower levels of stressful situations.21 On the other hand, individuals with childhood trauma develop a characteristic psychological and behavioral pattern that makes them more likely to experience negative life events, or the adverse life circumstances in which they lived during childhood continue to hinder their development in adulthood. Meanwhile, a study of US Middle school students shows that childhood trauma will exacerbate the adverse effects of recent stressful events in adolescent girls.22 Adolescents are in an important period of cognitive and emotional development, often facing many adverse psychological stresses, such as lack of understanding, too much pressure in life, as well as academic pressure, social phobia, and parental reprimand. The accumulation of negative life events reduces individuals’ well-being, making them more susceptible to the control of adverse emotions, which may be relieved by self-injury when they face stress that they cannot cope with. Therefore, this study formulated hypothesis 1: Negative life events will serve as a mediator between childhood trauma and NSSI (childhood trauma → negative life events → NSSI).
Recent studies have shown that negative coping (NC) is an independent risk factor for NSSI in adolescent patients with depressive disorder, and NC is associated with the increased risk of NSSI.23,24 Coping style refers to the behavior or reaction process taken by individuals to relieve tension after experiencing stress events, which can be divided into positive coping (PC) and NC.25 PC styles include solving problems, seeking support, and seeking help; NC styles include avoidance, fantasy, self-blame, and drug abuse. The coping style of patients with depressive disorder is relatively singular. They are not good at using external resources, and they are more inclined to choose NC styles such as escape. Castro et al found in a group of Chilean adolescents that people who adopted NC styles were three times more likely to have NSSI behavior than those who presented PC styles in the face of stressful events.26 In addition, childhood trauma has a significant impact on coping styles, and individuals who have experienced childhood trauma tend to respond negatively with regard to coping styles. On the one hand, childhood trauma will lead to developmental disadvantages, thereby making individuals in many fields dangerous, and the resulting disadvantages persist steadily throughout developmental maturation and affect the subsequent development of other functions, including deficits in coping styles. On the other hand, childhood trauma is an unhealthy environmental factor imposed on individuals by parents or caregivers, and children in this environment may form problems such as poor interpersonal trust and learned helplessness; thus, they likely adopt NC styles, such as smoking, alcohol abuse, drug dependence or NSSI to release and compensate for the emptiness and insecurity in their hearts.11,24,27,28 Therefore, the study formulated hypothesis 2: Coping style will serve as a mediator between childhood trauma and NSSI (childhood trauma → coping style → NSSI).
Based on psychological stress theory, stress comprises three parts: stressors, mediators, and stress responses. A stressor is any event that forces a person to adapt or change. Childhood trauma refers to exposure to negative stressful events during childhood, which are also known as early stress; negative life events, as stressors that occur in life, are defined in terms of concepts derived from stress.29 Mediating factors include personality, cognition, coping style, social support, and genetics; stress response results from a stressor in the presence of multiple mediating factors. In combination with the present study, whether stressors (childhood trauma and negative life events) can be causative factors is influenced by the way individuals cope with the stressors; when the intensity of stress exceeds the adaptability and coping ability of the individual, and when the individual cannot effectively solve the problem, psychological discomfort occurs, resulting in a stress response (NSSI behavior). Therefore, this study formulated hypothesis 3: Negative life events and coping style jointly play a chain mediating role in the relationship between childhood trauma and NSSI (childhood trauma → negative life events→ coping style → NSSI).
Materials and Methods
Study Population
From September to December 2022, 540 adolescents with depressive disorder from the psychiatric department of Renmin Hospital of Wuhan University were selected by convenient sampling.
The inclusion criteria were as follows: (1) diagnosed by two experienced psychiatrists in accordance with the Diagnostic and Statistical Manual of Mental Disorders, fifth edition, diagnostic criteria for depressive disorder; (2) age between 12 and 24 years;30 (3) participants (or relatives of patients) signed a written informed consent form; (4) participants could understand the content of the questionnaire and fill it out truthfully. The exclusion criteria were as follows: (1) serious adverse drug reactions or serious somatic diseases; (2) accompanied with severe psychotic symptoms, such as hallucinations and delusions; (3) alcohol and substance addiction.
The researcher collected the data by distributing a paper version of the questionnaire. Participants were invited to fill out the questionnaire in a quiet space, and any questions about the questionnaire during the filling process were answered patiently by the researcher; the filling process took approximately 20–30 min. The data were collected and checked by the researcher, and if evident omissions or logical errors were observed, the study participants were asked to fill in or correct them on the spot; after the data were collected, they were double checked and entered into the software.
Patient and Public Involvement
Participants were not involved in the design, conduct, reporting or dissemination plans of our research. There are no plans to distribute the study findings to the participants.
Measurements
The Childhood Trauma Questionnaire (CTQ) consists of 28 items in five factors, including childhood PA, EA, SA, PN, and EN.31 Each item is ranked on a 5-point Likert-type scale, ranging from 1 (never) to 5 (always). When the value of EA ≥ 13 or PA ≥ 10 or SA ≥8 or EN ≥ 15 or PN ≥ 10, the patient was considered to have a history of childhood abuse.32 In China, it has been demonstrated to have good reliability and validity.33
Life events were measured by using the Adolescent Self-Rating Life Events Checklist (ASLEC),34 which consisted of 27 items in six factors, including interpersonal relationship factor (IRF), academic pressure factor (APF), punishment factor (PF), loss factor (LF), health adaptation factor (HAF), and other factors. Each item was evaluated on a six-point Likert scale, ranging from 0 (did not occur) to 5 (extremely severe), and a higher score indicated greater stress. In this study, the Cronbach’s α of the ASLEC scale was 0.916.
The Trait Coping Style Questionnaire (TCSQ) was used to measure coping strategies, which consisted of 20 items in two factors, including PC and NC. Each item is ranked on a 5-point Likert-type scale, ranging from 1 (absolutely no) to 5 (absolutely yes). The TCSQ score was equal to the score of the PC style minus the score of the NC style. If the TCSQ score is positive, then the PC style is dominant, and if the TCSQ score is negative, then the NC style is dominant. The Cronbach’s α of the two dimensions was 0.825 and 0.812.
The Adolescent Nonsuicidal Self-injury Assessment Questionnaire (ANSAQ) consisted of 12 items in two factors, including self-injury behavior without evident tissue damage and self-injury behavior with evident tissue damage. The ANSAQ investigated the frequency of 12 NSSI behaviors.35 A cumulative frequency of various self-injury behaviors≥ 5 times was defined as being associated with NSSI behavior. Each item was ranked on a five-point Likert scale, ranging from 1 (never) to 5 (always). The higher the total score, the more serious the NSSI behavior. In this study, the Cronbach’s α of the ANSAQ scale was 0.881.
Statistical Analysis
SPSS version 26.0 and Mplus version 8.3 were used to analyze the data. Questionnaires with missing values associated with four or more variables were considered invalid, whereas for questionnaires with less than or equal to four missing item responses, missing values were treated by using the mean completion method. All data used in the analysis were normally distributed. Qualitative data were described by frequency and proportion. Quantitative data were statistically described by the mean and standard deviation (SD); summative score values for each scale were calculated, and the relationship among variables was examined via Pearson correlation analysis.
Mplus was used to perform structural equation model (SEM) analysis. Childhood trauma and NSSI were considered independent and dependent variables, respectively. Life events and coping style were considered mediating variables. In the SEM analysis I conducted, grounded in the Coping Style Theory,36 it’s posited that individuals’ coping styles are not static or fixed when facing stress. Instead, an individual may adjust based on specific situations and the individual’s psychological state, simultaneously exhibiting both positive and negative coping strategies. This suggests that when studying an individual’s coping style, it’s crucial to delve into the intricate interplay between positive and negative coping strategies, rather than perceiving them as separate or opposing tactics. Consequently, in this study, both the positive and negative coping, despite being at opposite ends of the spectrum, were integrated into a single latent variable. According to conventional standards, χ2/df < 3, root mean square error of approximation (RMSEA) < 0.08, comparative fit index (CFI) and Tucker‒Lewis fit index (TLI) > 0.90 indicate acceptable standards. The deviation-corrected bootstrap method (5000 repeated samples) was used to test the mediating effect. Direct effects, indirect effects, and total effects were calculated. The mediation effect ratio was calculated as total indirect effects divided by total effects. A two-sided P value of <0.05 indicated significant differences.
Results
Sample Characteristics and Preliminary Analyses
A total of 540 questionnaires were distributed, and 501 questionnaires were returned and considered valid (effective response rate: 92.8%). Thus, 501 adolescents with depressive disorders were enrolled in this study, with an average age of 19.03 ± 3.14 years, including 180 (35.9%) boys and 321 (64.1%) girls. A total of 398 (79.442%) patients had NSSI behavior, and 103 (20.56%) did not. Among the participants, 162 (32.3%) experienced EA, 97 (19.4%) experienced PA, 63 (12.6%) experienced SA, 253 (50.5%) experienced EN, and 198 (39.5%) experienced PN. The TCSQ score is negative (−9.27 ± 11.84), which indicates that the NC style is dominant. Differences in gender, age, childhood trauma, negative life events, and coping styles between participants with and without NSSI are shown in Table 1.
Table 1.
Differences in Gender, Age, Childhood Trauma, Negative Life Events and Coping Styles Between Participants with and without NSSI (n = 501)
| Variables | N | NSSI | Non-NSSI | t/x2 | p |
|---|---|---|---|---|---|
| Gender | 10.397 | 0.001 | |||
| Female | 321(64.1%) | 269(83.8%) | 52(16.2%) | ||
| Male | 180(35.9%) | 129(71.7%) | 51(28.3%) | ||
| Age | 19.03±3.14 | 18.75±3.07 | 20.13±3.16 | 4.058 | <0.001 |
| Childhood trauma | 54.10±13.13 | 55.45±13.42 | 48.90±10.45 | −5.320 | <0.001 |
| EA | 10.86±4.62 | 11.36±4.72 | 8.91±3.60 | −5.747 | <0.001 |
| PA | 7.45±3.50 | 7.78±3.68 | 6.16±2.34 | −5.506 | <0.001 |
| SA | 5.98±2.52 | 6.06±2.67 | 5.65±1.80 | −1.858 | 0.064 |
| EN | 14.09±5.37 | 14.48±5.26 | 12.58±5.54 | −3.136 | <0.05 |
| PN | 8.95±3.39 | 9.14±3.44 | 8.22±3.10 | −2.604 | <0.05 |
| Negative life events | 40.95±22.68 | 44.38±22.35 | 27.71±18.86 | −7.687 | <0.001 |
| PF | 6.82±6.48 | 7.54±6.74 | 4.07±4.42 | −6.291 | <0.001 |
| LF | 6.42±5.82 | 6.96±5.95 | 4.32±4.71 | −4.790 | <0.001 |
| IRF | 8.88±5.05 | 9.58±4.88 | 6.17±4.80 | −6.348 | <0.001 |
| APF | 8.79±4.98 | 9.47±4.86 | 6.15±4.54 | −6.279 | <0.001 |
| HAF | 8.14±4.64 | 8.77±4.50 | 5.71±4.36 | −6.199 | <0.001 |
| Others | 1.90±1.64 | 2.05±1.65 | 1.30±1.49 | −4.207 | <0.001 |
| Coping styles | −9.27±11.84 | −10.95±11.05 | −2.76±12.56 | 6.513 | <0.001 |
| PC | 25.74±7.12 | 25.01±6.88 | 28.58±7.31 | 4.640 | <0.001 |
| NC | 35.01±7.02 | 35.95±6.65 | 31.34±7.26 | −5.851 | <0.001 |
Abbreviations: EA, emotional abuse; PA, physical abuse; SA, sexual abuse; EN, emotional neglect; PN, physical neglect; PF, punishment factor; LF, loss factor; IRF, interpersonal relationship factor; APF, academic pressure factor; HAF, health adaptation factor; Others, other factors; PC, positive coping; NC, negative coping.
Correlation Analysis of Major Study Variables
Correlations among study variables are shown in Table 2. The strongest correlation was found between PF and LF (r = 0.722, P < 0.001). The correlation between PN and PC style was the weakest (r = −0.106, P < 0.05).
Table 2.
Correlations Between Significantly Different Factors in Participants with or Without NSSI (N = 501)
| EA | PA | EN | PN | PF | LF | IRF | APF | HAF | others | NC | PC | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PA | 0.577** | |||||||||||
| EN | 0.502** | 0.350** | ||||||||||
| PN | 0.394** | 0.262** | 0.639** | |||||||||
| PF | 0.323** | 0.298** | 0.235** | 0.239** | ||||||||
| LF | 0.333** | 0.249** | 0.270** | 0.254** | 0.722** | |||||||
| IRF | 0.388** | 0.272** | 0.176** | 0.150** | 0.587** | 0.537** | ||||||
| APF | 0.296** | 0.216** | 0.099* | 0.064 | 0.478** | 0.449** | 0.576** | |||||
| HAF | 0.274** | 0.192** | 0.162** | 0.120** | 0.543** | 0.531** | 0.579** | 0.544** | ||||
| Others | 0.259** | 0.202** | 0.104* | 0.090* | 0.466** | 0.425** | 0.531** | 0.439** | 0.419** | |||
| NC | 0.345** | 0.229** | 0.179** | 0.149** | 0.245** | 0.211** | 0.447** | 0.371** | 0.361** | 0.280** | ||
| PC | −0.227** | −0.163** | −0.234** | −0.106* | −0.122** | −0.129** | −0.263** | −0.247** | −0.264** | −0.227** | −0.402** | |
| NSSI | 0.412** | 0.281** | 0.169** | 0.171** | 0.311** | 0.237** | 0.420** | 0.349** | 0.348** | 0.294** | 0.390** | −0.310** |
Notes: **P < 0.01; *P<0.05.
Multiple Mediation Analyses Among Variables of Adolescents with Depressive Disorder
The final SEM based on the hypothesis is shown in Figure 1. The fitting results of this model were as follows: χ2/df = 138.782/69 =2.011, P <0.001, RMSEA = 0.045, CFI = 0.975, TLI = 0.967. Such results indicate a good fit. The SEM is shown in Figure 1. The standardized parameters of each path are shown in Table 3. The results of the mediating effect analysis shown in Table 3 indicated that childhood trauma has a direct effect on NSSI (Bootstrap 95% CI: 0.063, 0.344). In addition, three indirect effect pathways have been shown to influence the relationship between childhood trauma and NSSI. First, the mediating effect value of hypothesis 1 (childhood trauma → negative life events → NSSI) was 0.096 (Bootstrap 95% CI: 0.07, 0.169). Second, the mediating effect value of hypothesis 2 (childhood trauma → coping style → NSSI) was 0.088 (bootstrap 95% CI: 0.034, 0.183). Third, the mediating effect value of hypothesis 3 (childhood trauma → negative life events → coping style → NSSI) was 0.086 (Bootstrap 95% CI: 0.042, 0.162).
Figure 1.
Structural equation model of NSSI, with standardized path coefficients and significance level.
Note: ***P < 0.001.
Table 3.
Multiple Mediation Analysis Among Variables of Adolescents with Depressive Disorder
| Relationship | Estimate | S.E. | P | 95% CI |
|---|---|---|---|---|
| CT-N | 0.475 | 0.049 | <0.001 | 0.375, 0.565 |
| N-C | 0.506 | 0.065 | <0.001 | 0.382, 0.642 |
| CT-C | 0.246 | 0.066 | <0.001 | 0.116, 0.374 |
| C-NSSI | 0.359 | 0.102 | <0.001 | 0.198, 0.591 |
| N- NSSI | 0.202 | 0.083 | 0.015 | 0.016, 0.342 |
| CT-N- NSSI | 0.096 | 0.041 | 0.018 | 0.007, 0.169 |
| CT-C- NSSI | 0.088 | 0.040 | 0.026 | 0.034, 0.183 |
| CT-N-C- NSSI | 0.086 | 0.032 | 0.006 | 0.042, 0.162 |
| Total indirect effect | 0.271 | 0.044 | <0.001 | 0.199, 0.371 |
| Total effect | 0.480 | 0.053 | <0.001 | 0.373, 0.582 |
| Direct | 0.209 | 0.069 | 0.002 | 0.063, 0.334 |
Abbreviations: CT, Childhood trauma = emotional abuse + physical abuse + emotional neglect+ physical neglect; N, Negative life events; C, Coping styles.
Discussion
To the best of our knowledge, this study is the first to explore the multiple effects of childhood trauma, negative life events, and coping styles on NSSI. In this study, 398 adolescents with depressive disorders and NSSI accounted for 79.442% of the total study population, and significant differences in psychosocial factors were observed. Childhood trauma, negative life events, and coping styles not only independently predict NSSI, but also indirectly predict NSSI through a chain mediating effect. This finding provides a comprehensive understanding of adolescents with depressive disorders and NSSI related psychosocial factors, and it may provide a reference for the prevention and control of NSSI in adolescents with depressive disorders.
Effect of Childhood Trauma on NSSI
Consistent with previous studies, adolescents exposed to adverse childhood experiences have an increased risk of NSSI.37 Our research also shows that adolescents with depressive disorders with NSSI are more likely to have adverse childhood experiences than those without NSSI. However, no association between SA and NSSI was found in the current study. In a study by Liu H, people who reported SA in childhood had a higher risk of NSSI related thoughts and behavior.38 This finding is inconsistent with the current research results. Given the Chinese tradition of sexual conservatism, disclosing experiences of SA may bring stigma and negative reactions to the victim; thus, study participants tend to be secretive in their responses to questions about SA.
Moreover, it was found that childhood trauma can affect NSSI through multiple mediating factors, such as negative life events and coping style, which may be explained in some studies that have examined psychological changes that occur in individuals after experiencing abuse. Based on the developmental psychopathology theory of NSSI behavior,39 childhood traumatic experiences will destroy the motivation, attitude, and emotion of individuals, leading to the lack of adaptability of individuals. When faced with negative life events, adolescents with depressive disorders are more likely to be powerless and often resort to NC styles such as self-blame, withdrawal, and avoidance to cope with external environmental stresses and internal psychological conflicts, and they use NSSI behavior as an alternative compensatory coping strategy.
The high prevalence of adverse childhood experiences in adolescents with depressive disorders and abuse events is unpredictable, and they often encounter it without psychological preparation, which has a significant and far-reaching impact on children. Screening for the identification of adverse childhood experiences should be a priority, and it should extend beyond the hospital to the community and family to reduce the impact of adverse childhood experiences on patients.
Negative Life Events Act as a Mediator Between Childhood Trauma and NSSI
The current study found that negative life events can partly explain the relationship between childhood trauma and NSSI, which is the indirect path. Individuals with a history of childhood trauma often exhibit a lower capacity for environmental adaptation, demonstrating a relatively lower resilience to negative life events, such individuals experience a higher incidence of negative life events during adulthood,40,41 which are viewed as potential risk factors for adolescent NSSI behaviors.42 Adolescents are at a turning point in their life development. Since the emergence of COVID-19, social isolation caused by concomitant home isolation, infected family and friends, family economic pressure caused by property loss, uncertainty about the future, and anxiety and fear of infection have had serious negative effects on the physical and mental health of adolescents.43 In particular, adolescents with depressive disorders have weak psychological self-regulation and low psychological resilience compared with normal people, and they are vulnerable to adverse events. Any negative life events will remarkably change the overall function and the level of consciousness of adolescents with depressive disorder, leading to poor social adaptive behavior. One of the pathological manifestations is NSSI.44,45
In addition, this study shows that adolescents with depressive disorders and NSSI behavior will experience more negative life events, and they are under greater pressure than non-NSSI.46 Patients with NSSI have significantly higher scores on all dimensions of the negative life event scale and a higher degree of impact than non-NSSI patients. Negative life events may be used as a potential predictor of NSSI. Therefore, considerable attention should be given to adolescents with depressive disorders, particularly those who have recently experienced more negative life events. Schools and families should make concerted efforts to provide a good parenting environment for adolescents to prevent possible negative life events, such as being wronged, unjustified punishment, and scolding. Furthermore, adolescents should be provided with targeted help, cultivate adaptive coping styles, and emotion regulation methods to reduce NSSI behavior.
Coping Style Act as a Mediator Between Childhood Trauma and NSSI
The current study found that coping style can partly explain the relationship between childhood trauma and NSSI, which is the indirect path. Childhood trauma significantly impacts coping styles, with individuals who have experienced childhood trauma often resorting to maladaptive coping.24 Such adverse childhood experiences may diminish the opportunities for adolescents to develop healthy coping skills and problem-solving abilities, thus potentially lacking effective coping strategies when faced with life’s challenges. Consistent with Williams F’s research, adolescents with NSSI were more likely to adopt NC styles than those without NSSI.47 Compas B E argues that the coping styles of primary school students are mostly emotional, whereas the coping styles of adolescents are diversified.48 The NC styles of venting emotions and spiritual sustenance are more frequently used in early adolescence than in mid-adolescence; the former is mostly manifested as being indifferent and trying to change the status quo, whereas the latter is characterized by adolescents who often compare with their less fortunate peers or escape.
Adolescence is a critical period of physical and psychological development, and the behavior mode is gradually solidified. Therefore, the coping mode adopted in this period still has an important impact on their adult life. NSSI is a maladaptive coping strategy, and adolescents with depressive disorders use coping styles that do not effectively address problems when faced with negative life events, resulting in more negative emotions. As adverse emotions accumulate, adolescents may regulate strong emotional responses through NSSI behavior.
Therefore, early development and training of teenagers’ ability to deal with problems on their own, guiding them to correctly understand life events and stress, and correct and positive ways of coping when faced with stressful life events may reduce anxiety, reduce the occurrence of NSSI, and mitigate or avoid various adverse effects on their long-term lives.
Negative life Events and Coping Style Act as Chain Mediators in the Relationship Between Childhood Trauma and NSSI
Consistent with the findings of SHENK, adolescents with a history of childhood trauma, when facing negative life events in the future, demonstrate a direct association between their maladaptive emotional coping styles and the occurrence of NSSI behaviors.49 Adverse childhood experiences may negatively impact adolescents’ psychological adaptability,50 such early developmental deficiencies might leave individuals lacking appropriate coping mechanisms and resources when facing subsequent negative life events. In the absence of healthy coping skills, individuals may be more inclined to engage in NSSI behaviors as a strategy to cope with life stresses and negative emotions.51 Although NSSI may provide temporary emotional release for adolescents with depressive disorders, it falls within the domain of negative coping strategies and may lead individuals into a vicious cycle of negative coping and continued NSSI.52 Over time, this vicious cycle could further deteriorate individuals’ psychological states and social functioning, potentially triggering more severe psychological and social disorders.
In addition, this pathway may be explained by physiological studies. Early childhood experiences are crucial factors in personal growth and development, and adverse childhood experiences may affect neurodevelopment, especially in brain regions associated with emotional regulation and stress responses. The study by Li YY found that individuals with a history of childhood trauma are associated with a persistent increase in the activity of the hypothalamic-pituitary-adrenal (HPA) axis system,53 stress caused by negative life events leads to the activation of the HPA axis.54 Overactivity of the HPA axis may further impair the normal emotional regulation ability of adolescent individuals with depression,55 leading to a higher propensity for negative emotional reactions such as anxiety, pessimism, or anger. Such negative emotional reactions may further influence individuals’ coping mechanisms, making adolescents with depressive disorders more inclined towards negative coping styles, such as NSSI.
The covert nature of NSSI behaviors, coupled with the predominant reluctance among adolescents with depressive disorders exhibiting NSSI to actively seek help, poses certain challenges for the prevention of such behaviors. Therefore, to support the psychological well-being and enhance the coping skills of this particular demographic, it is imperative to continually advance and implement preventative intervention measures targeting the psychological and behavioral issues and mental disorders among children and adolescents. This encompasses not only intensifying psychological counseling for key populations but also developing more effective intervention and treatment strategies. Through these comprehensive measures, more holistic support can be provided for children and adolescent individuals with depressive disorders, promoting a more positive coping style in the face of life’s stresses and challenges.
Clinical Implications
First, our results highlight the importance of childhood trauma in depressed adolescents with NNSI behavior. Prevention of childhood trauma may be considered in the prevention of NSSI. Currently, child parent psychotherapy (CCP) facilitates the establishment of positive, secure, and intimate interactive relationships between parents and children and reduces the incidence of traumatic events in childhood.56 While CPP demonstrates potential benefits, reducing the occurrence of childhood traumatic events is a complex issue that not only relies on a singular treatment method but also requires comprehensive interventions such as family support, community engagement, and legal protection. Furthermore, we found that negative life events and coping style were mediators of the association between childhood trauma and NSSI. For adolescents with depressive disorder who have experienced childhood trauma, it may be possible to intervene with negative life events and coping style to reduce the relationship between childhood trauma and NSSI. Strengthen education on adolescent mental health issues helps them learn to effectively manage emotions and cope with stress, thereby reducing the threshold for the occurrence of negative life events.57 Accepting negative emotions is a focal point in cognitive behavioral therapy (CBT) research.58 When confronted with negative events, it is important to assist adolescents with depressive disorders in learning to express their feelings and negative emotions, as well as accepting their presence. Moreover, it is essential to help them find suitable ways to release emotions, such as through writing, drawing, exercising, or having conversations with close friends.
Limitations
This research has several limitations. First, although this study uses evaluation tools with good reliability and validity, they are all self- evaluations, and patient choices may be influenced by social expectations, investigation bias, and recall bias, resulting in a lack of objectivity. Comprehensive information can be obtained through interviews, expert judgment, or medical records. Second, this study used convenient sampling to collect data from a hospital in Wuhan, China, which may limit the generalizability of the findings. Third, this study used a cross-sectional survey approach and lacked extension on the timeline. NSSI behavior in adolescents with depressive disorders is dynamic and changing in nature; therefore, future studies should consider exploring deeper relationships through a longitudinal design.
Conclusion
The high prevalence of NSSI behavior in adolescents with depression should be given considerable attention. The results of this study showed that adolescents with depressive disorders and NSSI behavior were significantly different from those without NSSI behavior in childhood PA, EA, PN, EN, interpersonal relationships, academic pressure, punishment, loss, HAF, PC, and NC. Childhood trauma, negative life events, and coping styles not only independently predict NSSI but also indirectly predict NSSI through a chain mediating effect. In addition, the results of this study may provide insights into the prevention and intervention of NSSI behavior based on psychosocial factors. Further research must be conducted to investigate the mechanism of action of protective factors for NSSI behavior to provide reliable, effective, and accessible psychological interventions for patients.
Acknowledgments
We sincerely thank Dr. Lijun Kang and Dr. Chang Shu for their help in editing.
Funding Statement
This work was supported by grants from The Interdisciplinary Innovative Talents Foundation from Renmin Hospital of Wuhan University (grant numbers: JCRCGW-2022-010), the Clinical Nursing Special Research and Cultivation Fund Project of Wuhan University (grant numbers: LCHL202301), the Key opening projects of Hubei Province (grant numbers: 2021KFH012, 2022KFH001), and the Research project of Wuhan Nursing Association (grant numbers: WHHL202202).
Ethics Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Renmin Hospital of Wuhan University (NO: WCRY2020-K004). Participants gave informed consent to participate in the study before taking part.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Buelens T, Luyckx K, Kiekens G, Gandhi A, Muehlenkamp JJ, Claes L. Investigating the DSM-5 criteria for non-suicidal self-injury disorder in a community sample of adolescents. J Affect Disord. 2020;260:314–322. doi: 10.1016/j.jad.2019.09.009 [DOI] [PubMed] [Google Scholar]
- 2.Bjärehed J, Lundh LG. Deliberate self-harm in 14-year-old adolescents: how frequent is it, and how is it associated with psychopathology, relationship variables, and styles of emotional regulation? Cogn Behav Ther. 2008;37(1):26–37. doi: 10.1080/16506070701778951 [DOI] [PubMed] [Google Scholar]
- 3.Briere J, Rickards S. Self-awareness, affect regulation, and relatedness: differential sequels of childhood versus adult victimization experiences. J Nerv Ment Dis. 2007;195(6):497–503. doi: 10.1097/NMD.0b013e31803044e2 [DOI] [PubMed] [Google Scholar]
- 4.Lim KS, Wong CH, McIntyre RS, et al. Global lifetime and 12-month prevalence of suicidal behavior, deliberate self-harm and non-suicidal self-injury in children and adolescents between 1989 and 2018: A meta-analysis. Int J Environ Res Public Health. 2019;16(22):4581. doi: 10.3390/ijerph16224581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kang N, Jiang Y, Ren Y, et al. Distress intolerance mediates the relationship between child maltreatment and nonsuicidal self-injury among Chinese adolescents: a three-wave longitudinal study. J Youth Adolesc. 2018;47(10):2220–2230. doi: 10.1007/s10964-018-0877-7 [DOI] [PubMed] [Google Scholar]
- 6.Klonsky ED. The functions of deliberate self-injury: a review of the evidence. Clin Psychol Rev. 2007;27(2):226–239. doi: 10.1016/j.cpr.2006.08.002 [DOI] [PubMed] [Google Scholar]
- 7.Auerbach RP, Kim JC, Chango JM, et al. Adolescent nonsuicidal self-injury: examining the role of child abuse, comorbidity, and disinhibition. Psychiatry Res. 2014;220(1–2):579–584. doi: 10.1016/j.psychres.2014.07.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lüdtke J, In-Albon T, Schmeck K, Plener PL, Fegert JM, Schmid M. Nonsuicidal self-injury in adolescents placed in youth welfare and juvenile justice group homes: associations with mental disorders and suicidality. J Abnorm Child Psychol. 2018;46(2):343–354. doi: 10.1007/s10802-017-0291-8 [DOI] [PubMed] [Google Scholar]
- 9.Siu AMH. Self-harm and suicide among children and adolescents in Hong Kong: a review of prevalence, risk factors, and prevention strategies. J Adolesc Health. 2019;64(6s):S59–s64. doi: 10.1016/j.jadohealth.2018.10.004 [DOI] [PubMed] [Google Scholar]
- 10.Wan Y, Chen J, Sun Y, Tao F. Impact of childhood abuse on the risk of non-suicidal self-injury in mainland Chinese adolescents. PLoS One. 2015;10(6):e0131239. doi: 10.1371/journal.pone.0131239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu RT, Scopelliti KM, Pittman SK, Zamora AS. Childhood maltreatment and non-suicidal self-injury: a systematic review and meta-analysis. Lancet Psychiat. 2018;5(1):51–64. doi: 10.1016/S2215-0366(17)30469-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brunstein Klomek A, Snir A, Apter A, et al. Association between victimization by bullying and direct self injurious behavior among adolescence in Europe: a ten-country study. Eur Child Adolesc Psychiatry. 2016;25(11):1183–1193. doi: 10.1007/s00787-016-0840-7 [DOI] [PubMed] [Google Scholar]
- 13.Li W, Yang J, Gao L, Wang X. Childhood maltreatment and adolescents’ aggression: a moderated mediation model of callous-unemotional traits and friendship quality. Child Maltreat. 2021;2021:10775595211046550. [DOI] [PubMed] [Google Scholar]
- 14.Devi F, Shahwan S, Teh WL, et al. The prevalence of childhood trauma in psychiatric outpatients. Ann Gen Psychiatry. 2019;18:15. doi: 10.1186/s12991-019-0239-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gould F, Clarke J, Heim C, Harvey PD, Majer M, Nemeroff CB. The effects of child abuse and neglect on cognitive functioning in adulthood. J Psychiatr Res. 2012;46(4):500–506. doi: 10.1016/j.jpsychires.2012.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murray LK, Nguyen A, Cohen JA. Child sexual abuse. Child Adolesc Psychiatr Clin N Am. 2014;23(2):321–337. doi: 10.1016/j.chc.2014.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duke NN, Pettingell SL, McMorris BJ, Borowsky IW. Adolescent violence perpetration: associations with multiple types of adverse childhood experiences. Pediatrics. 2010;125(4):e778–786. doi: 10.1542/peds.2009-0597 [DOI] [PubMed] [Google Scholar]
- 18.Brown RC, Heines S, Witt A, et al. The impact of child maltreatment on non-suicidal self-injury: data from a representative sample of the general population. BMC Psychiatry. 2018;18(1):181. doi: 10.1186/s12888-018-1754-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shao C, Wang X, Ma Q, Zhao Y, Yun X. Analysis of risk factors of non-suicidal self-harm behavior in adolescents with depression. Ann Palliat Med. 2021;10(9):9607–9613. doi: 10.21037/apm-21-1951 [DOI] [PubMed] [Google Scholar]
- 20.Kendler KS, Gardner CO. Depressive vulnerability, stressful life events and episode onset of major depression: a longitudinal model. Psychol Med. 2016;46(9):1865–1874. doi: 10.1017/S0033291716000349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harkness KL, Bruce AE, Lumley MN. The role of childhood abuse and neglect in the sensitization to stressful life events in adolescent depression. J Abnorm Psychol. 2006;115(4):730–741. doi: 10.1037/0021-843X.115.4.730 [DOI] [PubMed] [Google Scholar]
- 22.Rudolph KD, Flynn M. Childhood adversity and youth depression: influence of gender and pubertal status. Dev Psychopathol. 2007;19(2):497–521. doi: 10.1017/S0954579407070241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lin MP, You J, Ren Y, et al. Prevalence of nonsuicidal self-injury and its risk and protective factors among adolescents in Taiwan. Psychiatry Res. 2017;255:119–127. doi: 10.1016/j.psychres.2017.05.028 [DOI] [PubMed] [Google Scholar]
- 24.Wan Y, Chen R, Wang S, et al. Associations of coping styles with nonsuicidal self-injury in adolescents: do they vary with gender and adverse childhood experiences? Child Abuse Negl. 2020;104:104470. doi: 10.1016/j.chiabu.2020.104470 [DOI] [PubMed] [Google Scholar]
- 25.Lazarus RS. From psychological stress to the emotions: a history of changing outlooks. Ann Rev Psychol. 1993;44(1). doi: 10.1146/annurev.ps.44.020193.000245 [DOI] [PubMed] [Google Scholar]
- 26.Castro K, Kirchner T. Coping and psychopathological profile in nonsuicidal self-injurious chilean adolescents. J Clin Psychol. 2018;74(1):147–160. doi: 10.1002/jclp.22493 [DOI] [PubMed] [Google Scholar]
- 27.Yılmaz Irmak T, Aksel Ş, Thompson D. Coping strategies and depression among college students following child sexual abuse in Turkey. J Child Sex Abus. 2016;25(8):881–894. doi: 10.1080/10538712.2016.1236871 [DOI] [PubMed] [Google Scholar]
- 28.Runtz MG, Schallow JR. Social support and coping strategies as mediators of adult adjustment following childhood maltreatment. Child Abuse Negl. 1997;21(2):211–226. doi: 10.1016/S0145-2134(96)00147-0 [DOI] [PubMed] [Google Scholar]
- 29.Williamson DE, Birmaher B, Ryan ND, et al. The stressful life events schedule for children and adolescents: development and validation. Psychiatry Res. 2003;119(3):225–241. doi: 10.1016/S0165-1781(03)00134-3 [DOI] [PubMed] [Google Scholar]
- 30.Snow KJ, Cruz AT, Seddon JA, et al. Adolescent tuberculosis. Lancet Child Adolt Health. 2020;4(1):68–79. doi: 10.1016/S2352-4642(19)30337-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Burgermeister D. Childhood adversity: a review of measurement instruments. J Nurs Meas. 2007;15(3):163–176. doi: 10.1891/106137407783095766 [DOI] [PubMed] [Google Scholar]
- 32.Bernstein DP, Fink L, Handelsman L, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry. 1994;151(8):1132–1136. [DOI] [PubMed] [Google Scholar]
- 33.Zhao XF, Zhang YL, Lin L, Zhou YF, Lin HZ, Yang SC. Reliability and validity of the Chinese version of childhood trauma questionmaire. Chin J Clinical Rehabilitation. 2005;20:105–107. [Google Scholar]
- 34.C C. Assessment of major life events for Hong Kong adolescents: the Chinese adolescent life event scale. Am J Community Psychol. 1997;25:1. [DOI] [PubMed] [Google Scholar]
- 35.Wan YH, Liu W, Hao RH, Tao FB. Development and evaluation on reliability and validity of adolescent non-suicidal self-injury assessment questionnaire. Chin J Sch Health. 2018;39(2):170–173. [Google Scholar]
- 36.Connor-Smith JK, Flachsbart C. Relations between personality and coping: a meta-analysis. J Pers Soc Psychol. 2007;93(6):1080–1107. doi: 10.1037/0022-3514.93.6.1080 [DOI] [PubMed] [Google Scholar]
- 37.Yang J, Chen Y, Yao G, et al. Key factors selection on adolescents with non-suicidal self-injury: a support vector machine based approach. Front Public Health. 2022;10:1049069. doi: 10.3389/fpubh.2022.1049069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu H, Wang W, Yang J, Guo F, Yin Z. The effects of alexithymia, experiential avoidance, and childhood sexual abuse on non-suicidal self-injury and suicidal ideation among Chinese college students with a history of childhood sexual abuse. J Affect Disord. 2021;282:272–279. doi: 10.1016/j.jad.2020.12.181 [DOI] [PubMed] [Google Scholar]
- 39.Yates TM. The developmental psychopathology of self-injurious behavior: compensatory regulation in posttraumatic adaptation. Clin Psychol Rev. 2004;24(1):35–74. doi: 10.1016/j.cpr.2003.10.001 [DOI] [PubMed] [Google Scholar]
- 40.Glaser JP, van Os J, Portegijs PJ, Myin-Germeys I. Childhood trauma and emotional reactivity to daily life stress in adult frequent attenders of general practitioners. J Psychosom Res. 2006;61(2):229–236. doi: 10.1016/j.jpsychores.2006.04.014 [DOI] [PubMed] [Google Scholar]
- 41.Fontenelle LF, Muhlbauer JE, Albertella L, Eppingstall J. Traumatic and stressful life events in hoarding: the role of loss and deprivation. Eur J Psychotraumatol. 2021;12(1):1947002. doi: 10.1080/20008198.2021.1947002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jiang Z, Wang Z, Diao Q, et al. The relationship between negative life events and non-suicidal self-injury (NSSI) among Chinese junior high school students: the mediating role of emotions. Ann Gen Psychiatry. 2022;21(1):45. doi: 10.1186/s12991-022-00423-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bhatia R. Editorial: effects of the COVID-19 pandemic on child and adolescent mental health. Curr Opin Psychiatry. 2020;33(6):568–570. doi: 10.1097/YCO.0000000000000651 [DOI] [PubMed] [Google Scholar]
- 44.Zhang L, Chen M, Yao B, Zhang Y. Aggression and non-suicidal self-injury among depressed youths: the mediating effect of resilience. Iran J Public Health. 2021;50(2):288–296. doi: 10.18502/ijph.v50i2.5342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gámez-Guadix M, Wachs S, Wright M. “Haters back off!” Psychometric properties of the coping with cyberhate questionnaire and relationship with well-being in Spanish adolescents. Psicothema. 2020;32(4):567–574. doi: 10.7334/psicothema2020.219 [DOI] [PubMed] [Google Scholar]
- 46.Nock MK, Joiner TE, Gordon KH, Lloyd-Richardson E, Prinstein MJ. Non-suicidal self-injury among adolescents: diagnostic correlates and relation to suicide attempts. Psychiatry Res. 2006;144(1):65–72. doi: 10.1016/j.psychres.2006.05.010 [DOI] [PubMed] [Google Scholar]
- 47.Williams F, Hasking P. Emotion regulation, coping and alcohol use as moderators in the relationship between non-suicidal self-injury and psychological distress. Prev Sci. 2010;11(1):33–41. doi: 10.1007/s11121-009-0147-8 [DOI] [PubMed] [Google Scholar]
- 48.Compas BE, Connor-Smith JK, Saltzman H, Thomsen AH, Wadsworth ME. Coping with stress during childhood and adolescence: problems, progress, and potential in theory and research. Psychol Bull. 2001;127(1):87–127. doi: 10.1037/0033-2909.127.1.87 [DOI] [PubMed] [Google Scholar]
- 49.Shenk CE, Noll JG, Cassarly JA. A multiple mediational test of the relationship between childhood maltreatment and non-suicidal self-injury. J Youth Adolesc. 2010;39(4):335–342. doi: 10.1007/s10964-009-9456-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Evans GW, Li D, Whipple SS. Cumulative risk and child development. Psychol Bull. 2013;139(6):1342–1396. doi: 10.1037/a0031808 [DOI] [PubMed] [Google Scholar]
- 51.Chapman AL, Gratz KL, Brown MZ. Solving the puzzle of deliberate self-harm: the experiential avoidance model. Behav Res Ther. 2006;44(3):371–394. doi: 10.1016/j.brat.2005.03.005 [DOI] [PubMed] [Google Scholar]
- 52.Nock MK. Why do people hurt themselves? New insights into the nature and functions of self-injury. Curr Dir Psychol Sci. 2009;18(2):78–83. doi: 10.1111/j.1467-8721.2009.01613.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li YY, Hu ZZ, Huang ZL, Yang SR. 应激在抑郁症失眠中的作用和常用应激动物模型的睡眠特点 [Role of stress in depression insomnia and sleep characteristics of commonly used animal stress models]. Yao Xue Xue Bao. 2012;47(1):1–6. Chinese. [PubMed] [Google Scholar]
- 54.Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocr Rev. 2000;21(1):55–89. doi: 10.1210/edrv.21.1.0389 [DOI] [PubMed] [Google Scholar]
- 55.Dienes KA, Hazel NA, Hammen CL. Cortisol secretion in depressed, and at-risk adults. Psychoneuroendocrinology. 2013;38(6):927–940. doi: 10.1016/j.psyneuen.2012.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lieberman AF, Van Horn P, Ippen CG. Toward evidence-based treatment: child-parent psychotherapy with preschoolers exposed to marital violence. J Am Acad Child Adolesc Psychiatry. 2005;44(12):1241–1248. doi: 10.1097/01.chi.0000181047.59702.58 [DOI] [PubMed] [Google Scholar]
- 57.Gress‐Smith JL, Roubinov DS, Andreotti C, Compas BE, Luecken LJ. Prevalence, severity and risk factors for depressive symptoms and insomnia in college undergraduates. Stress Health. 2015;31(1):63–70. doi: 10.1002/smi.2509 [DOI] [PubMed] [Google Scholar]
- 58.Ballesio A, Bacaro V, Vacca M, et al. Does cognitive behaviour therapy for insomnia reduce repetitive negative thinking and sleep-related worry beliefs? A systematic review and meta-analysis. Sleep Med Rev. 2021;55:101378. doi: 10.1016/j.smrv.2020.101378 [DOI] [PubMed] [Google Scholar]