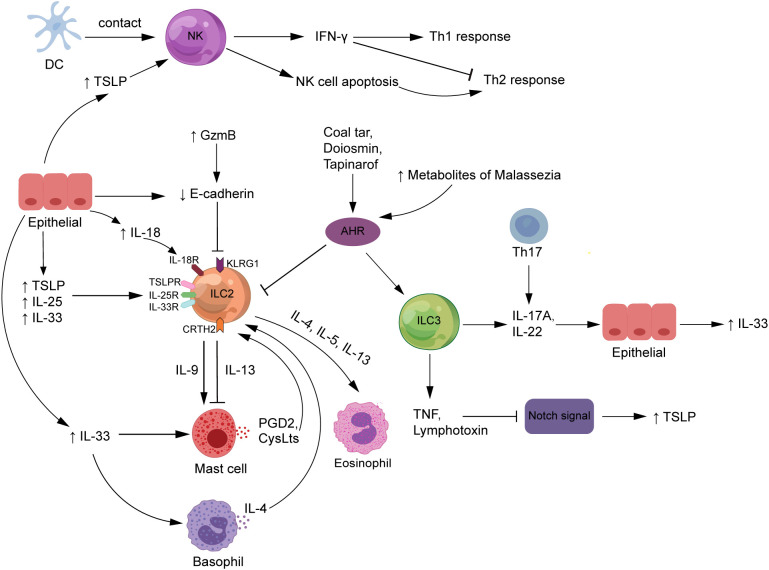
Figure 3.
The roles of ILCs in atopic dermatitis. NK cells are stimulated by DC exposure or high TSLP levels to enhance Th1 responses, attenuate Th2 responses by producing IFN-γ, and improve Th2-type immunity by promoting auto-apoptosis. The expression of TSLP, IL-33, and IL-25, released by epithelial cells and serve as major ILC2 activators, is increased in AD patients. The interaction of ILC2s with other innate immune cells, such as mast cells and basophils, is critical to the complex mechanics of AD. Also, ILC3s release IL-17A or IL-22, which contribute to the pathogenesis of AD. Increased GzmB expression and FLG deficiency in AD patients both enhance E-cadherin cleavage, which inhibits the interaction between E-cadherin and the KLRG1 receptor expressed on ILC2s, which would strengthen the body’s ILC2-related response. ILCs may trigger TSLP secretion by producing TNF and lymphotoxin to downregulate Notch signaling. In addition, diosmin, coal tar, and tapinarof inhibit the action of ILC2s but promote the function of ILC3s by activating the AHR signaling pathway. AHR, aryl hydrocarbon receptor; CRTH2, chemoattractant receptor-homologous molecule expressed on Th2 cells; CysLts, cysteinyl leukotrienes; DCs, dendritic cells; FLG, filaggrin; GzmB, granzyme B; IFN-γ, interferon-gamma; IL, interleukin; ILCs, innate lymphoid cells; KLRG1, killer cell lectin-like receptor G1; NK, natural killer; PDG2, prostaglandin D2; Th, T helper; TNF, tumor necrosis factor; TSLP, thymic stromal lymphopoietin.