Abstract
Introduction
Efficacious programmes require implementation at scale to maximise their public health impact. TransformUs is an efficacious behavioural and environmental intervention for increasing primary (elementary) school children’s (5–12 years) physical activity and reducing their sedentary behaviour within school and home settings. This paper describes the study protocol of a 5-year effectiveness–implementation trial to assess the scalability and effectiveness of the TransformUs programme.
Methods and analysis
A type II hybrid implementation–effectiveness trial, TransformUs is being disseminated to all primary schools in the state of Victoria, Australia (n=1786). Data are being collected using mixed methods at the system (state government, partner organisations), organisation (school) and individual (teacher, parent and child) levels. Evaluation is based on programme Reach, Effectiveness, Adoption, Implementation and Maintenance (RE-AIM) framework. RE-AIM domains are being measured using a quasi-experimental, pre/post, non-equivalent group design, at baseline, 12 and 24 months. Effectiveness will be determined in a subsample of 20 intervention schools (in Victoria) and 20 control schools (in New South Wales (NSW), Australia), at baseline, 12 and 24 months. Primary outcomes include TransformUs Reach, Adoption, Implementation and organisational Maintenance (implementation trial), and children’s physical activity and sedentary time assessed using accelerometers (effectiveness trial). Secondary outcomes include average sedentary time and moderate to vigorous-intensity physical activity on weekdays and during school hours, body mass index z-scores and waist circumference (effectiveness trial). Linear mixed-effects models will be fitted to compare outcomes between intervention and control participants accounting for clustering of children within schools, confounding and random effects.
Ethics and dissemination
The trial was approved by the Deakin University Human Research Ethics Committee (HEAG-H 28_2017), Victorian Department of Education, the NSW Department of Education, Australian Catholic University (2017-145R), Melbourne Archdiocese Catholic Schools and Catholic Schools NSW. Partners, schools/teachers and parents will provide an informed signed consent form prior to participating. Parents will provide consent for their child to participate in the effectiveness trial. Findings will be disseminated via peer-reviewed publications, scientific conferences, summary reports to schools and our partner organisations, and will inform education policy and practice on effective and sustainable ways to promote physical activity and reduce sedentary behaviours population-wide.
Trial registration number
Australian Clinical Trials Registration Registry (ACTRN12617000204347).
Keywords: PUBLIC HEALTH, Community child health, Schools
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Strengths include the hybrid effectiveness–implementation trial design undertaken in a real-world context, the inclusion of multiple levels of data collected at multiple time points, the use of robust frameworks to guide implementation and scale-up, and device-based measurement of children’s physical activity and sedentary time in the effectiveness trial.
Testing the hypothesised mediating and/or moderating relationships, such as organisational readiness for change, with implementation and effectiveness outcomes, will help understand primary barriers to, and facilitators of, implementation of school-based interventions, such as TransformUs.
Limitations include reliance on teacher self-reported implementation of the programme, although additional implementation data will be captured using Google Analytics (eg, use of the TransformUs website, professional development completed by teachers and which programme resources are downloaded).
Facilitation of programme dissemination activities via stakeholders and the research team may not reflect true real-world promotion, but will highlight practices required for sustainable scale-up.
Extended COVID-19 lockdowns and government restrictions in Australia meant on-site data collection in schools was prohibited in Victoria between 2020 and April 2023, and in New South Wales during 2021; nevertheless, the conduct of both an implementation and effectiveness trial will enable us to compare differences between schools to ascertain the level of implementation, ‘real-world’ programme impact and generalisability of results.
Introduction
Regular physical activity is beneficial for children’s cardiometabolic health (including lipids, adiposity and blood pressure)1 and mental health.2 Physical activity has also been positively associated with academic results, including cognitive skills (eg, executive functioning, attention, memory, comprehension), attitude (eg, motivation, self-concept, satisfaction and enjoyment), academic behaviour (eg, organisation), engagement in learning (eg, on-task time) and academic achievement (eg, standardised test scores).3–5 Few studies have examined the impact of prolonged sitting on children’s health, with the evidence still primarily observational and indeterminate.6 While there is currently insufficient evidence for a dose–response relationship between sedentary behaviour (defined as any waking behaviour characterised by an energy expenditure ≤1.5 metabolic equivalents while in a sitting, reclining or lying posture)7 and health outcomes in children and adolescents (aged 5–17 years), greater time spent sedentary has been linked to poorer health outcomes such as lower fitness, and poorer cardiometabolic and mental health in this population.8 There is some evidence that breaking up sedentary time may improve cognitive outcomes in children.9
In Australia, only 26% of children aged 5–12 years meet the government recommendation of at least 1 hour of moderate to vigorous-intensity physical activity (MVPA) every day.10 As part of the Australian 24-hour movement guidelines for children and young people (5–17 years) which integrate physical activity, sedentary behaviour and sleep, it is recommended that children reduce and break up prolonged sitting throughout the day.11 More than 60% of children’s class time is spent sitting12 and only 25–30% of morning recess and lunch breaks at school are spent in MVPA.13 Comprehensive school physical activity programmes that use whole-of-school approaches to promote activity and adopt active school environments (ie, active classrooms, active environments, quality physical education and sport) have been recommended to address low levels of physical activity among children.14 15 Whole-of-school approaches are also recommended within the WHO Global Action Plan for Physical Activity, as a way to promote enjoyment and participation in physical activity among youth.16
There are some examples of efficacious school-based approaches to promoting children’s physical activity17 and reducing sedentary behaviour,18 although the association between implementation fidelity and intervention outcomes is unclear.19 20 Most interventions target organised sport and physical education,21 yet interventions which provide sports and active equipment during recess, and incorporate playground markings can also successfully increase children’s physical activity.22 23 A systematic review has also shown that school interventions with a family element can be more effective at increasing physical activity than just focusing on the school setting alone24; however, few studies have determined the efficacy of strategies to reduce prolonged sitting both at school and home among children.25 The initial TransformUs programme26 was one of the earliest programmes (developed in 2009) to incorporate many of these elements with a particular focus on reducing and breaking up children’s sitting throughout the school day.
The efficacy of the initial TransformUs programme was demonstrated in a four-arm two-by-two factorial design cluster-randomised controlled trial (RCT) involving 20 primary (elementary) schools, 226 teachers and over 1600 children in Melbourne, Australia (2010–2013).26 The three intervention arms targeted either increases in physical activity (PA-I), reductions in sedentary behaviour (SB-I) or a combination of both (PA+SB-I), compared with a usual practice control. The results of this RCT are described and interpreted in detail elsewhere.26 However, in brief, at 18 months (n=348), compared with usual practice, children who received the physical activity intervention (groups PA-I and PA+SB-I) had significantly less weekday sedentary time (−27 min/day). Compared with usual practice, children who received the sedentary behaviour intervention (SB-I and PA+SB-I) spent more time in daily physical activity (5.5 min/day) at 18 months, and at 30 months spent 33 min less in daily sedentary time, and specifically, 63 min less in sedentary time on weekdays, with no differences in physical activity at 30 months.26 Thus, strategies to promote both children’s physical activity and reduce sedentary behaviour were important. Results also showed beneficial effects on children’s adiposity markers (body mass index (BMI) and waist circumference (n=564)). However, there were mixed effects on children’s blood pressure (BP), positive effects on systolic BP and negative effects on diastolic BP (n=537) and in a subsample of children (n=206), on blood parameters (eg, negative effects on some inflammatory markers such as C reactive protein, interleukin (IL)-6, IL-2 and tumour necrosis factor-α, beneficial effects on vitamin D, brain-derived neurotrophic factor and plasminogen activator inhibitor-1).26
Teachers, parents and children reported that the programme was positively received, and teachers involved in the intervention arms also reported perceptions of better classroom management and improved ‘on-task’ behaviour during lessons.20 Although barriers to implementation were experienced (including a lack of school leadership to support implementation long term, promotion and awareness raising, teacher time constraints and challenges with sustained integration into existing practices), overall, the programme was effectively integrated into the school curriculum.20 Existing teaching practices, children’s enjoyment and teacher awareness of programme values and benefits were the main facilitators of delivery and sustainability.20 Following the success of TransformUs, and exploration of adaptations for scaling (described in the Methods section), the Victorian Department of Education committed to partnering with the research team to support the dissemination and implementation of the programme to all primary (elementary) schools in Victoria, Australia. Given the small number of school-based interventions that are studied at scale27 and that use implementation theories to guide this process,28 29 scaling up of TransformUs presented a unique opportunity to investigate real-world implementation at scale. Assessment of intervention implementation among school-based interventions is greatly needed in the field.19
This paper describes the study protocol for a 5-year trial (launched September 2018–final data collection December 2023), which aims to evaluate the real-world effectiveness and implementation of TransformUs at scale. To note, the paper outlines the intended protocol for the trial (including planned dates and timelines for data collection), but also describes where and how this changed due to the impacts of the COVID-19 global pandemic. In line with the RE-AIM (Reach, Effectiveness, Adoption, Implementation and Maintenance) framework criteria,30 we will evaluate the following five aims: the programme’s aim 1: Reach (proportion and representativeness of principals and teachers, parents and children participating in TransformUs); aim 2: Effectiveness (change in children’s daily physical activity and sedentary time 12 and 24 months post-baseline); aim 3: Adoption (proportion and representativeness of schools choosing to implement TransformUs); aim 4: Implementation (dissemination by education and health partners, uptake of intervention components, frequency, dose and adaptation to TransformUs delivery, and barriers and enablers to implementation); and aim 5: Individual-level Maintenance (change in children’s physical activity and sedentary time 24 months post-baseline) and Organisational-level Maintenance (institutionalisation and sustainability of the programme within the education and health systems, school settings and by teachers as part of routine practice).
Methods and analysis
Overview of the TransformUs programme
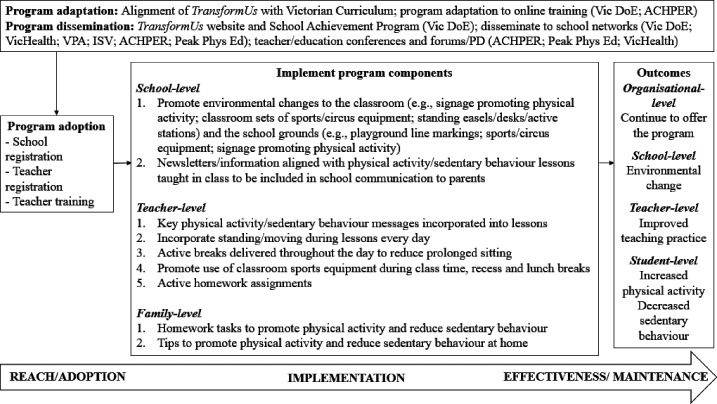
TransformUs is a behavioural and environmental intervention delivered in the classroom, broader school environment and family setting to increase children’s physical activity levels and reduce sedentary behaviour.31 The programme includes: (1) health lessons incorporating key physical activity/sedentary behaviour messages; (2) active academic lessons; (3) active breaks; (4) changes to the school environment; (5) active homework; and (6) parent newsletters promoting physical activity/reducing sitting time (for more detail, see figure 1). The programme was based on the Social Cognitive Theory,32 Behavioural Choice Theory33 and Ecological Systems Theory.34 The health lessons, active academic lessons and active breaks are all aligned with the Victorian35 and Australian curriculum and standards.36 All TransformUs components are contained in the members’ area of the website (https://transformus.com.au). To access these resources, Victorian primary school teachers need to register (at no cost) using their work email address. A detailed description of the programme strategies31 and programme logic model has been published elsewhere.20 Adaptations to the TransformUs programme for scale-up are described later in the Methods section, and online supplemental file 1 presents the evolution of TransformUs since the original RCT (2009) to date.
Figure 1.
TransformUs programme components for scale-up. ACHPER, Australian Council for Health, Physical Education and Recreation; ISV, Independent Schools Victoria; PD, Professional Development; Vic DoE, Victorian Department of Education; VPA, Victorian Principals Association.
bmjopen-2023-078410supp001.pdf (265.4KB, pdf)
Study design
This study uses a type II hybrid effectiveness–implementation trial design,37 38 to concurrently examine both effectiveness outcomes and implementation and scale-up processes. Mixed-methods data will be collected at the systems (state government, partner organisations), organisational (school) and individual (teacher, parent and child) levels. Online supplemental file 2 contains the Standard Protocol Items: Recommendations for Interventional Trials checklist, relevant to this manuscript.
bmjopen-2023-078410supp002.pdf (176.6KB, pdf)
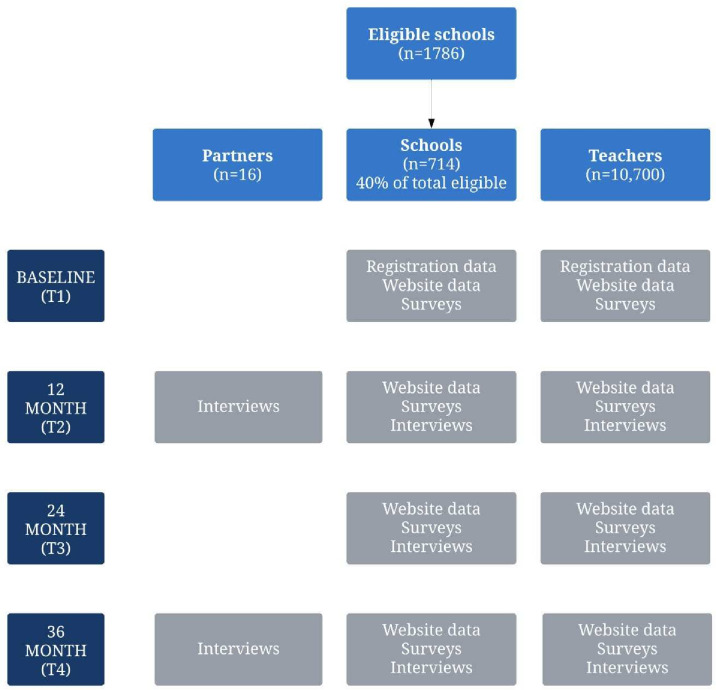
Implementation trial
Every primary school in Victoria (government, independent and Catholic) will be offered TransformUs and will be eligible for inclusion in the state-wide implementation trial. Our objective is for the programme to be adopted by at least 715 primary schools (40% of a total of 1786 primary schools in Victoria39) by the end of the trial. The adoption estimates are based on school uptake of state-wide initiatives offered by the Victorian Department of Education and previous implementation trials in schools.40 As TransformUs dissemination will be ongoing over 5 years, schools can register anytime between September 2018 and December 2022. Data are planned to be collected from schools and teachers who agree to participate in the evaluation at baseline (T1), 12 months (T2), 24 months (T3) and 36 months (T4) post-registration—within the funding time period (September 2018–December 2022). These data will contribute to assessing Reach, Adoption, Implementation and Organisational-level Maintenance (aims 1, 3, 4 and 5).
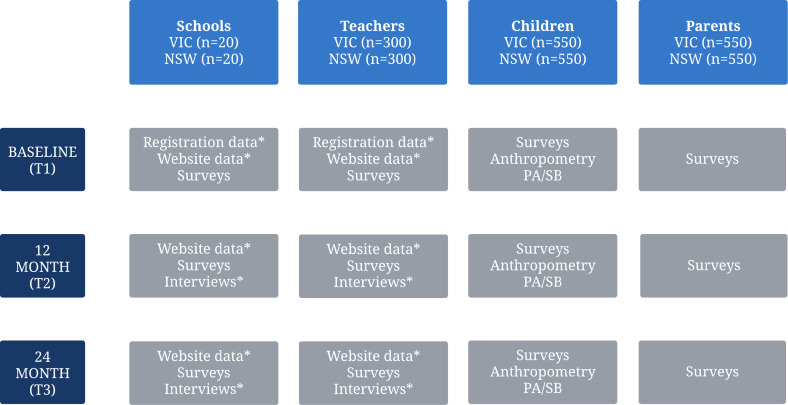
Effectiveness trial
To determine short-term and long-term changes in children’s levels of physical activity and sedentary time under ‘real-world’ conditions (based on adaptations from the original TransformUs programme described below), an embedded effectiveness trial is planned with 20 intervention schools in Victoria and 20 control schools in the state of New South Wales (NSW). A quasi-experimental pre/post non-equivalent group design41 with follow-up will be adopted. As this is a real-world roll-out in Victoria, a non-randomised two-group parallel arm approach was adopted. Data collected at baseline (T1), 12 months (T2) and 24 months (T3) will contribute to assessing programme effectiveness and maintenance at the student level (aims 2 and 5). Schools in NSW were considered suitable controls as NSW has a similar population size and geographical spread to Victoria compared with other states and territories, and the TransformUs programme was not available in NSW.
Programme adaptation and piloting
The TransformUs RCT showed that strategies to promote children’s physical activity and reduce sedentary behaviour were both important,42 and therefore the combined (PA+SB-I) approach was the focus for wider scale-up. During the RCT, teacher professional development was delivered face-to-face by the research team, and schools received ongoing support from the team over the 2.5 years of the study. This approach was not considered feasible for scale-up. To facilitate scale-up, professional development, support and all programme materials and resources were converted into an online format to maximise potential reach at a lower cost. Formative evaluation with partners responsible for implementing interventions at scale can also be useful to inform adaptations to the intended dissemination strategy and refine the programme materials to enhance scalability.43 Therefore, in close partnership with local councils (from Local Government Areas) and teachers, the TransformUs online materials were tested in two pilot dissemination trials and formative evaluation was conducted with key partner organisations involved in scale-up, detailed in the following section.
TransformUs pilot dissemination trials (2015–2017)
Two 12-month pilot dissemination trials were conducted during July 2015–2016 (pilot trial 1; n=4 schools, n=41 teachers) and 2017 (pilot trial 2; n=5 schools, 22 teachers), to assess the feasibility of TransformUs dissemination and the online teacher professional development. In both pilots, the programme was advertised to schools via two councils (representing two different Local Government Areas) in Victoria. The costs of programme equipment (eg, standing easels, sports equipment) and installation of playground line markings (eg, hopscotch) were subsidised by the councils to support uptake. Schools located in a lower-income area were offered a greater subsidy than schools in a higher-income area (determined using the Schools in a Socio-Economic Indexes for Areas (SEIFA), methods consistent with the original RCT).44 All teachers within participating pilot schools were asked to, preferably, complete the online professional development (lasting 30–45 min) during a session on their school site that was facilitated by a representative from the relevant council. As this was to inform the real-world dissemination trial and to help understand the feasibility of online professional development, schools could also send a nominated teacher and adopt a train-the-trainer approach.
Teachers completed online surveys before and after the professional development session, 2 months and 12 months post-baseline (max n=51 teachers; pilot trial 1), and at 4 months post-baseline (n=22 teachers; pilot trial 2). Most teachers reported that they: (1) gained new knowledge of ways to increase children’s physical activity (88%) and reduce sedentary behaviour (90%) at school; (2) learnt new teaching methods (78%); (3) perceived the online training to be an appropriate delivery method (82%); and (4) gained the required knowledge (90%) and confidence (80%) to implement the programme. Teachers requested visual examples of programme implementation (ie, digital video clips), which they felt would strengthen teacher engagement and sustain delivery of the programme. Although the RCT focused on children in grades 3–5 (ages 8–11 years), in both pilot trials, participating schools planned a whole-of-school approach to implementation across all school year levels, foundation to grade 6 (ages 5–12 years). For scale-up, programme materials were modified to accommodate delivery across all year levels, covering a range of learning areas (eg, mathematics, English, science and humanities), and digital video clips were developed to demonstrate appropriate implementation.
Formative evaluation with key partner organisations (2016)
Through an integrated research–practice partnership approach, collaboration began with one government (Victorian State government Department of Education) and five non-governmental organisations (the Victorian Health Promotion Foundation (VicHealth), the Victorian Principals Association, Independent Schools Victoria, the Australian Council for Health, Physical Education and Recreation Victoria (ACHPER), and Peak Phys Ed). These partners play various roles in the education and health systems including, for example, responsibility for delivery of education to children and young people in Victorian government and independent schools (eg, Department of Education), and coordinating and delivering teacher education professional development (eg, ACHPER and Peak Phys Ed). In collaboration, these partners will provide ongoing input into the state-wide dissemination strategy, ensuring that the programme aligns with other existing school-based health promotion initiatives in the state (eg, the Victorian Achievement Program, which aims to create healthier early childhood services, schools and workplaces; http://www.achievementprogram.health.vic.gov.au/), and that all resources (eg, health lessons) are linked to the Victorian curriculum and each resource identifies the specific strand, substrand, content description and achievement standard. For example, TransformUs supports the development of student capabilities (eg, critical and creative thinking, personal and social capabilities), which are taught explicitly in and through the learning area resources. TransformUs also provides cross-curriculum opportunities for students to strengthen their literacy and numeracy general capabilities.
Implementation and scale-up of TransformUs
Theoretical underpinnings
Our approach to scale-up is ‘horizontal’, defined as extending the reach of an intervention by replicating it in other localities, cities or states.45 Our implementation approach is derived from evidence-based recommendations for the successful scalability of population-level health interventions,43 46 47 and concepts within the translation, support and delivery systems of the Interactive Systems Framework.48 We draw on ways to improve implementation and sustainability as outlined in the Quality Implementation Framework,49 PRACTIS Guide43 and from literature on ways to increase public health programme sustainability.50 To identify underlying barriers and facilitators to individual-level implementation, qualitative data collection will be informed by the Theoretical Domains Framework,51 which is a systematic and theoretically based approach to behaviour change that identifies barriers to practice change and potential strategies to intervene. The RE-AIM framework30 informs the overarching evaluation outcomes following implementation and scale-up.
Implementation and scale-up strategies
In addition to findings from the TransformUs pilot adaptation studies described above, scale-up strategies were also guided by literature on strategies for effective implementation and scale-up planning43 45 and attributes of successful scale-up (ie, compatibility of the programme with the values and facilities of intended users, and perceived need for the innovation within the organisation).52 Online supplemental file 3 presents the 14 TransformUs implementation and scale-up strategies, reported in line with recommendations and definitions for specifying implementation strategies.53
bmjopen-2023-078410supp003.pdf (206.3KB, pdf)
Our focus is on implementation quality as opposed to controlling rigorous programme fidelity that is essential in efficacy trials. In school-based intervention implementation, ‘quality’ can include: (1) sufficient exposure (dose); (2) fidelity to the programme protocol; (3) implementation (engaging students through active participation); (4) adaptation (modifying the intervention to meet developmental and cultural needs); and (5) teachers’ attitudes, understanding of the concepts/issues and prior experience.54 In TransformUs, schools were encouraged to choose contextually relevant strategies for implementation at their school, rather than a prescriptive programme, to enhance quality and ensure programme adoption occurs in the most contextually relevant way to achieve health benefits. This approach is associated with increased effectiveness of real-world interventions and those more likely to produce sustainable results.49
In the context of TransformUs, we will be creating an implementation infrastructure for schools via Department of Education endorsement, provision of sustainability resources (ie, template policy statements for schools to embed the programme), and active engagement with state education decision-makers and other non-government partner organisations. Implementation resources will also be provided to support and encourage school-level leadership to implement the programme, and provide recommendations to promote integration and sustainability (ie, TransformUs champion roles and responsibilities, a template policy document).
TransformUs programme for scale-up
Figure 1 presents the TransformUs programme components for scale-up. Based on outcomes from the two pilot trials and formative work with our partner organisations and to maximise programme reach, all supporting programme materials, implementation and training resources are available online via a programme website. The website (https://transformus.com.au/) is managed by the research team at Deakin University. Teachers are required to complete the mandatory online professional development via the TransformUs website. The professional development provides strategies to integrate and sustain implementation of the programme in schools, and thus is essential to ensure minimum standards and knowledge are established prior to programme delivery. Based on evidence for the determinants of effective implementation by adopting individuals (users, ie, teachers),55 56 the content of the professional development programme has been designed to address the following seven key areas: (1) support for implementation (teacher and school level); (2) skills required for implementation; (3) knowledge required for implementation; (4) self-efficacy to implement; (5) fit of the programme into existing practices; (6) relative advantage of the intervention over existing practices; and (7) perceived ownership of the programme (allowing for adaptation). For example, the professional development includes ways of embedding the programme in practice, such as development of a tailored implementation plan (ie, a checklist of activities teachers wish to undertake and how they plan to sustain delivery) and knowledge reflection (quizzes) to test learning.
Multiple dissemination routes will be used to maximise programme uptake and sustainability (eg, via our partners, through sharing the web link, email lists, social media, teacher professional learning networks, and teacher professional development conferences and workshops). Interactions with stakeholders will include face-to-face or online meetings (eg, approximately two group meetings per year in addition to regular one-on-one meetings), and the provision of dissemination materials and communication packs to stakeholders, to enable them to promote TransformUs via their existing social media platforms and newsletters.
Recruitment
Implementation trial: partners (state level)
One representative from each of our partner organisations (six organisations were formal partners prior to the project being funded) who has experience in disseminating and/or supporting the TransformUs roll-out will be invited to participate in interviews to capture system-level impact (eg, organisational-level maintenance, which relates to aim 5 of the study). We expect to recruit one representative from each of our partner organisations. As depth of qualitative data is more important than sample size,57 we aim to recruit a purposeful sample of representatives from our partner organisations. Recruited participants will be asked to provide signed consent prior to taking part.
Implementation trial: principals (school level) and teachers
Schools and teachers will be made aware of TransformUs via multiple dissemination routes (as described in the TransformUs programme for scale-up section). All schools and teachers who wish to adopt TransformUs register free of charge via the TransformUs website, and teachers can register to access the TransformUs programme regardless of whether their school (ie, principal) has registered. This is to allow for both top-down and bottom-up programme adoption. To access the professional development, registration is mandatory. Upon registration, a unique login username for each teacher/school will be generated, which they can use to revisit the website and access the professional development and online resources. During registration, schools/teachers will be invited to participate in the survey component of the implementation trial, where they will receive a plain language statement and online consent form.
The registration process collects information about where they heard about the programme, general physical activity policy and practice information for their school (eg, information on participation in additional physical activity programmes will also be collected), and which elements of the TransformUs programme their school plans to implement. There are no costs to access the online resources. Implementation schools wishing to install new playground line markings or purchase physical activity equipment will not receive funding from the research project to do so. To help minimise the financial investment required, information on how to best use existing playground line markings and physical activity equipment is provided online.
We plan to reach 714 schools (based on an estimate of 40% of the total number of schools in Victoria39; n=1786). As part of the implementation trial, we aim to recruit ~15 school leaders who registered for the survey evaluation component of TransformUs to participate in a qualitative interview about their experiences of adopting and implementing the programme. This sample size provides sufficient ‘information power’.58 While schools/teachers will provide online consent to participate in the survey component of the implementation trial at the point of TransformUs registration, the subsample of participants invited to complete an interview will be required to provide additional consent prior to the interview commencing.
Effectiveness trial: schools and teachers
Twenty schools in Victoria will be recruited using stratified non-random sampling to maximise area-level socioeconomic position and geographical location. Targeted recruitment of 20 control schools in NSW will be matched as much as possible (based on school size, type (eg, government, Catholic and independent), SEIFA index (a measure of socioeconomic advantage and disadvantage by area in Australia), geographical area (eg, rural, remote), single sex/mixed students), with schools enrolled in the effectiveness trial in Victoria. Schools will represent different socioeconomic urban and rural areas, including different types, based on a minimum of two grade 3 classes or four composite classes (ie, grade 3 and 4 classes combined).
Effectiveness trial: children and parents
Grades 3 and 4 children attending schools enrolled in the effectiveness schools (and their parents) will be invited to help assess the effectiveness of the programme. Children will be in grade 3 or 4 at baseline to enable a planned follow-up at 12 months and 24 months, and this is consistent with the target age group evaluated in the original TransformUs RCT.31 Parents will receive information about the study via the schools’ regular methods of communication (eg, school intranet system, email, text) and an information brochure sent home with the students. There will be a plain language statement and consent form for parents to provide consent for themselves and/or their child to participate in the assessments (eg, parent online survey, child MVPA, BMI and waist circumference). As part of the consent process, parents/guardians will provide contact details (email and mobile telephone), which will be used to email a unique link to an online parent survey at each time point and to communicate with parents about the wearing and return of data collection devices from their child. Three emails or texts will be sent over 6 weeks to remind parents to complete the survey.
Figures 2 and 3 present flow diagrams of participant recruitment into the effectiveness and implementation trials, respectively.
Figure 2.
Effectiveness trial participant flow diagram. ∗VIC only. NSW, New South Wales; PA, physical activity; SB, sedentary behaviour; VIC, Victoria.
Figure 3.
Implementation trial participant flow diagram.
Sample size and power
Twenty Victorian schools will be recruited to ensure we have a diverse sample from a range of school types (government, Catholic and independent), socioeconomic status (SES) tertiles (based on SEIFA data) and geographical areas. The target recruitment of children for the effectiveness study is based on statistical power calculations of the minimum number of participants required to detect differences in mean average daily sedentary behaviour (primary outcome) at 12 months (primary time point) between children in control and intervention schools. In the efficacy trial, average daily sedentary time was 347 min (SD=60) for the PA+SB intervention group and 371 min (SD=80) for the control group at time 3 (18 months post-baseline). Sample size calculations were conducted assuming a pre/post-design, adjusting for baseline, in accordance with a published formula.59 Based on estimates from the original cluster-RCT, to account for the design effect, an intraclass correlation coefficient of 0.03 for children within school clusters was used, with a conservative correlation of 0.015 assumed between two different pupils within a cluster at different time points and a correlation of 0.22 between the same pupils at different time points. Assuming α=0.05, 80% power will be available to detect a 16-minute difference in sedentary time (two-thirds of that observed in the efficacy trial as effects may diminish at scale)60 at 12 months between intervention and control with recruitment of 1094 children (547 from intervention and control schools, assuming approximately 28 students/school sampled). This number is sufficient to detect as small an effect as a 6-minute difference in physical activity between the control and intervention schools, based on estimated SDs of 9 min for the PA+SB group and 7 min for the control group from the cluster-RCT.
Inclusion and exclusion criteria: implementation trial
All government, independent and Catholic primary schools in Victoria (n=1786)39 will be eligible to adopt the programme and thus participate in this research. In the implementation trial, registered schools can include those previously involved in the original RCT and adaptation pilot trials. Schools or teachers located outside of Victoria are not able to register for the programme or gain access to the professional development and online resources.
Inclusion and exclusion criteria: effectiveness trial
Schools that participated in the 2010–2013 TransformUs RCT and 2015–2017 pilot trials will be excluded from the sample frame for the effectiveness trial. Special schools for children with a disability (defined by the school) and schools with less than 30 students across both grades 3 and 4 will also be excluded to ensure that there is sufficient power to test the effectiveness of the programme among students (n=20 schools, 550 students from Victoria vs n=20 schools and 550 students from NSW) and parents. A matrix containing the names and types of all Victorian primary schools will be used for sampling, to ensure a range of government, independent and Catholic schools from inner city, outer suburban and regional areas are approached for recruitment. To be eligible as a control school in NSW, the school should not be implementing a similar health or physical activity-related programme at baseline data collection. Any uptake of similar programmes was monitored at each time point. For pragmatic and cost-related reasons, schools need to be located within a 4-hour drive from Deakin University (Burwood, Victoria) or Australian Catholic University (North Sydney, NSW).
Programme dissemination and implementation timeline
Online supplemental file 4 shows the timing of the implementation activities over 5 years and how data collection maps to the RE-AIM framework. Programme refinement and online training took place in the first 6 months (2017). Programme dissemination and implementation began in September 2018 and is ongoing. It will be monitored until December 2023. Final data collection (interviews with partners) will occur in December 2023.
bmjopen-2023-078410supp004.pdf (91.6KB, pdf)
Patient and public involvement
At what stage in the research process were patients/the public first involved in the research and how?
Six organisations were formal partners prior to the project being funded. This included a state government Department of Education and independent schools’ peak body, teacher professional development organisations, a principals’ association and a health promotion foundation. As this is an implementation/effectiveness trial designed to scale up a previously efficacious school-based intervention, we engaged closely with these partners in the adaptation of the programme for scale-up. After funding was secured, these partnerships will continue to be integral to the dissemination and evaluation of this project.
How were the research question(s) and outcome measures developed and informed by their priorities, experience and preferences?
The research question related to the effectiveness of implementing and scaling up an evidence-based school intervention on children’s physical activity and sedentary behaviour is directly aligned with the policy priorities of the Victorian Department of Education. The Department of Education has Education State targets which aim to increase the percentage of children in Victoria meeting physical activity guidelines by 20% by 2025. This alignment was critical in securing partnership with the Department of Education in Victoria.
How were patients/the public involved in the design of this study?
As previously noted, from study inception and through the adaptation process for scale-up, we have had input from teachers, teacher professional development organisations (eg, ACHPER and Peak Phys Ed), as well as key stakeholders such as local councils.
How were they involved in the recruitment to and conduct of the study?
Stakeholder partners have actively disseminated the programme and assisted with the recruitment of schools and teachers for this study, and some partners have also assisted with implementation of the intervention.
Were they asked to assess the burden of the intervention and time required to participate in the research?
An economic evaluation was conducted in the previous RCT which assessed the burden and time required for teachers to implement the programme. Interviews with teachers during a pilot phase prior to the RCT also informed the number of standing lessons and active breaks per day was feasible for teachers to implement in terms of time requirements. We also pilot tested the feasibility of the programme in terms of fitting it into the curriculum with teachers. This evidence was critical for informing the design and adaptations for the current project. Formal partners on the trial were also asked to consider the time required for their involvement in the trial (including any potential burden), as part of the in-kind contributions they provided as a partner organisation.
How were (or will) they be involved in your plans to disseminate the study results to the participants and relevant wider patient communities (eg, by choosing what information/results to share, when and in what format)?
All stakeholder partners will play a role in dissemination of findings to teachers, schools and broader audience (eg, health promotion officers, sport and recreation industry, etc) via a range of communication platforms (eg, social media, websites, newsletters, email distribution lists) and teacher education professional learning events and opportunities (eg, seminars, professional learning sessions and conference presentations, keynote addresses, etc).
Data collection
Online supplemental file 4 presents the mixed-methods data to be collected at the partner (state), principal (school), teacher, parent and child levels, in accordance with the RE-AIM framework. Recruitment and baseline data collection from schools in the effectiveness trial commenced in 2018.
Measures
Reach
Estimation of reach (online supplemental files 4 and 5) consists of all teachers and children in registered schools (based on Victorian Department of Education records) who will be classified as potentially exposed to the programme. The total number of programme recipients (teachers and children) compared with the total number eligible will represent one measure of potential reach. However, teachers could register and complete the professional development without a school being registered or be included within a participating school but chose not to complete the professional development. Therefore, we will also compare the number of teachers completing the professional development (actual recipients) versus the total number of teachers in Victorian schools (potentially eligible for the professional development) as an additional measure of programme reach. The TransformUs website will be used to capture the number of teachers registered and if teachers complete the professional development. Unique tracking codes (Google Analytics) associated with different promotional campaigns will contribute to assessing TransformUs dissemination.
bmjopen-2023-078410supp005.pdf (64KB, pdf)
Effectiveness and individual-level maintenance
The effectiveness trial outcome variables will be assessed at T1 (baseline) and T2 (12 months) using accelerometers (online supplemental files 4 and 5). Primary outcomes include children’s average minutes/day of MVPA and sedentary time. Secondary outcomes include children’s average weekday MVPA and sedentary time (minutes/day), average minutes/day of MVPA and sedentary during school hours, BMI z-scores (zBMI) and waist circumference. Individual-level maintenance will be assessed at T3 (24 months). Individual-level maintenance is defined as continued benefits among recipients (ie, sustained increases in MVPA or decreases in sedentary time).
Grades 3 and 4 children’s MVPA and sedentary time will be assessed using hip-mounted ActiGraph GT3X+ accelerometers (Pensacola, Florida, USA) during waking hours for 8 consecutive days (excluding water-based activities). To capture the sporadic nature of children’s physical activity, data will be collected in 5-second epochs, and will be processed using Evenson cut-off points.61 Non-wear time is defined as ≥20 min of consecutive zeros62 and a cut-off point of 100 counts/min will be used to indicate sedentary time in children. Primary and secondary outcomes will be computed using only data from days on which a minimum of 8 hours of wear time on weekdays and 7 hours of wear time on weekend days were recorded (valid days). A minimum of 4 valid days (either weekday or weekend) will be required for inclusion in analysis. Inclusion criteria for school days will be accelerometer data for at least 50% of school hours.63 64
Children’s height (cm) and waist circumference (cm), and weight (kg) will be assessed twice (to the nearest 0.1 cm and 0.1 kg, respectively) in school at each time point by trained research assistants. If the difference between the two measurements is greater than the following thresholds (height=0.5 cm; waist=1 cm; weight=0.2 kg), a third measurement will be taken. An average of the two closest measurements will then be calculated for analyses. Height will be assessed using a portable stadiometer (SECA 220, Los Angeles, California, USA). Weight will be assessed using digital scales (Wedderburn Tanita, Melbourne, Victoria, Australia), and a flexible steel tape will assess waist circumference at the narrowest point between the bottom rib and the iliac crest, in the midaxillary plane. BMI (kg/m2) z-scores will be calculated by subtracting the sex–age population median BMI scores from children’s raw BMI scores.65
Additional exploratory outcomes will include children’s awareness of the programme and self-reported quality of life,66 assessed via an online survey at T1 (baseline), T2 (12 months) and T3 (24 months). The EQ-5D-Y-3L questionnaire67 for children and adolescents aged 8–16 years is an internationally validated English–Australian version of the EQ-5D questionnaire developed by the EuroQol Research Foundation. The health-related quality of life (HRQoL) section contains five items that capture (on a 3-point scale) mobility, independence, usual activity, pain and feelings, and a sixth item that captures the child’s perceived overall health rating (sliding scale 0–100) on the day of survey completion. Following EQ-5D-Y-3L scoring protocols, an overall HRQoL score will be created.
Parents will provide via an online survey a proxy report of their child’s physical activity using a validated single-item measure assessing compliance with Australian physical activity guidelines.68
Adaptations to data collection due to COVID-19 restrictions
The COVID-19 pandemic had a significant impact on data collection resulting in a need to change our protocol (online supplemental files 4 and 5). Due to extended COVID-19 lockdowns and government restrictions in Australia, on-site data collection in schools was prohibited in Victoria during 2020 and 2021 and in NSW during 2021. During periods when children were able to attend school over that time, accelerometers were sent directly to families or directly to schools for distributing to students (NSW only), and the child and parent surveys were completed online. Height, weight and waist circumference data were not collected. Teacher and principal data (survey and interview) were also not collected to reduce burden on school staff during the challenges of teaching remotely. These adaptations impacted 6 schools at T2, and 20 schools at T3 in Victoria and 2 schools at T3 in NSW. Due to differences in lockdown restrictions between the states in 2020, the timing of data collection in NSW was adjusted to match Victoria. As a result, principal/teachers’ interviews were only conducted at 12 months.
As primary schools in Victoria were unable to operate as normal and ran learning from home for a total of 267 days across 2020 and 2021, additional teacher support was provided so they could apply the pedagogical elements of TransformUs to online teaching and learning. This included a remote learning sample pack with active English and Math lesson ideas that could be delivered online. An online family pack was also provided for parents to help support their child’s physical activity at home.
Adoption
All schools in Victoria are eligible to participate in TransformUs and therefore the total number of schools in the state (potentially eligible) and the total number who register (actual schools who adopt TransformUs) will be used to estimate the adoption rate (online supplemental files 4 and 5). The TransformUs website will be used to capture the number of schools registered and if the teacher completes the professional development. Partner interviews were due to occur at 12 months, 24 months and 36 months post-baseline; however, due to COVID-19 restrictions outlined previously, interviews were conducted at 12 months (September–October 2019) and a final interview will occur at 5 years post-baseline (2023).
Implementation
To capture implementation at the school level (online supplemental files 4 and 5), survey and interview data will capture organisational infrastructure and resource availability, organisational readiness and capacity to implement TransformUs, planned implementation, strategies for implementation and perceived impact of the programme on children’s physical activity, sedentary behaviour and classroom behaviour outcomes, and outcomes at the school level (eg, change in teaching behaviours). Existing survey measures will be sourced from previous studies of children’s physical activity31 69 70 and school-based implementation.71 Organisational readiness will be assessed using the Organisational Readiness for Implementation Change Scale,72 adapted for the TransformUs context.
Interviews with partners (12 months and 5 years post-baseline) and principals/teachers (12 months) will be based on the 14 domains of the Theoretical Domains Framework51 to identify barriers and targeted strategies to enhance teacher and school implementation of the programme. In addition, we will use Google Analytics to capture how schools and teachers use the TransformUs website, which programme components are downloaded, and which aspects of the website are most and least accessed. For parents and children, survey data will capture dose received and perceptions of the programme.
Organisational-level maintenance
For the implementation trial, organisational-level maintenance is defined as continued activities by implementers (eg, adaptation over time, changes in implementation dose, institutionalisation within the school setting and change to policies and practices) and continued capacity within the community (eg, stakeholder engagement and support for the intervention, and activities over time). Organisational-level maintenance will be assessed via partner self-report and interviews, principal and teacher online surveys/interviews, and parent/child survey data on dose received and perceptions of the programme (online supplemental files 4 and 5). Google Analytics data will inform on continued use of the TransformUs website.
Data analysis
Qualitative data
Qualitative data in this study contribute to assessing all five dimensions of the RE-AIM framework. Qualitative interview data will be transcribed and analysed thematically via NVivo V.12. Coding and theme development will be first deductive, guided by the study aims and RE-AIM domains,73 followed by an inductive approach that will be directed by content of the data.74 Themes will be grouped against the 14 domains of the Theoretical Domains Framework.51 Data will be coded by two independent researchers.
Quantitative data
Survey data for programme Reach, Adoption, Implementation and Organisational-level Maintenance will be reported descriptively. Methods for calculating level of implementation will be based on a previous implementation evaluation of the TransformUs efficacy trial.20 In brief, teachers will be grouped by level of implementation based on the proportion of the entire intervention delivered (dose delivered and fidelity). Implementation levels will correspond to: (1) ‘low’ (<33% of the entire intervention delivered); (2) ‘moderate’ (33–67% delivered) and (3) ‘high’ (>67% delivered).20
Quantitative data: effectiveness trial
The effectiveness component of the study will compare primary, secondary and exploratory outcomes among children, between intervention and control schools. Linear mixed models will be fitted to compare mean average daily sedentary time and MVPA at T1 (baseline), T2 (12 months) and T3 (24 months) (primary outcomes), average sedentary time and MVPA on weekdays and during school hours, zBMI, waist circumference (secondary outcomes) and quality of life (exploratory outcomes) at 12 months and 24 months between children in intervention and control schools. Linear mixed models will include fixed effects for group (intervention/control), time (months since baseline (time 1)) and a group by time interaction, and random effects for clustering of time nested within children, class and school. In the absence of random assignment, propensity scores will be developed to determine the probability of a child receiving the intervention based on observed baseline covariates (eg, age, sex, area-level SES of residence). Inverse probability of treatment weighting using the propensity score will be adopted to assist in obtaining unbiased estimates of average treatment effects, although it is acknowledged that this will not control for the difference in location (Victoria or NSW) between intervention and control schools.75 Due to the impact of COVID-19 interruptions on this study, sensitivity analysis will consider only children who participated in baseline and 12-month follow-up in intervention and control schools to examine the effectiveness prior to home schooling and other COVID-19 impacts.
Descriptive statistics will be calculated for the additional exploratory outcomes: children’s perceptions and awareness of the programme, at 12 months and 24 months for children in the intervention group, and parent-proxy report of their child’s physical activity at baseline, 12 months and 24 months in both the control and intervention groups. All statistical analyses will be performed using Stata SE V.17.
Ethics and dissemination
The trial was approved by the Deakin University Human Research Ethics Committee (HEAG-H 28_2017), Victorian Department of Education and Training, the NSW Department of Education, Australian Catholic University (2017-145R) and the relevant Catholic Education Offices. Partners, schools/teachers and parents will provide informed signed consent prior to taking part in surveys or interviews. Parents will provide consent for their child to participate in assessments as part of the effectiveness trial.
Findings from this trial will be disseminated via peer-reviewed publications, scientific conferences, summary reports to schools and our partner organisations. This trial builds on the successful cluster RCT of TransformUs.26 Completion of the TransformUs RCT was timely, as in 2016, the Victorian Department of Education released the Education State policy, with a 10-year target to increase the number of children meeting physical activity guidelines on weekdays by 20%.76 TransformUs directly aligns with the policy priorities of the Department of Education, and this alignment was critical in securing partnership with the Department of Education in Victoria. Establishing how best to scale up this efficacious programme will generate important learning that will inform future research studies in terms of implementation, assessment and monitoring of policy uptake, and provide key information for relevant stakeholders wishing to expand similar initiatives.
Supplementary Material
Footnotes
Twitter: @Harriet_Koorts
Contributors: JS, HK, AT, CL, NDR, DRL, JDG, AB, AT, LB, KEL, LA and HB contributed to the study design. HK led the writing of the manuscript with JS, and KEL led the development of the analysis plan for the effectiveness component. JS, HK, AT, CL, NDR, DRL, JDG, AB, AT, LB, KEL, LA, NL, SKL, TS, HB and KW revised the manuscript for intellectual content and read and approved the final draft.
Funding: This work is funded by an Australian National Health and Medical Research Council (NHMRC) Partnership Grant (APP1115708) and VicHealth. JS is supported by an NHMRC Leadership Level 2 Fellowship (APP1176885). DRL is supported by an NHMRC Senior Research Fellowship (APP1154507). NDR was supported by a Future Leader Fellowship from the National Heart Foundation of Australia (ID 101895). LA is supported by an Australian Research Council Discovery Early Career Researcher Award (DE220100847).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Tambalis KD, Sidossis LS. Physical activity and Cardiometabolic health benefits in children. In: Kokkinos P, Narayan P, eds. Cardiorespiratory Fitness in Cardiometabolic Diseases: Prevention and Management in Clinical Practice. Cham: Springer International Publishing, 2019: 405–23. 10.1007/978-3-030-04816-7 [DOI] [Google Scholar]
- 2.Biddle SJH, Ciaccioni S, Thomas G, et al. Physical activity and mental health in children and adolescents: an updated review of reviews and an analysis of causality. Psychol Sport Exerc 2019;42:146–55. 10.1016/j.psychsport.2018.08.011 [DOI] [Google Scholar]
- 3.Singh AS, Saliasi E, van den Berg V, et al. Effects of physical activity interventions on cognitive and academic performance in children and adolescents: a novel combination of a systematic review and recommendations from an expert panel. Br J Sports Med 2019;53:640–7. 10.1136/bjsports-2017-098136 [DOI] [PubMed] [Google Scholar]
- 4.Watson A, Timperio A, Brown H, et al. Effect of classroom-based physical activity interventions on academic and physical activity outcomes: a systematic review and meta-analysis. Int J Behav Nutr Phys Act 2017;14:114. 10.1186/s12966-017-0569-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schmidt M, Benzing V, Kamer M. Classroom-based physical activity breaks and children's attention: cognitive engagement works! Front Psychol 2016;7:1474. 10.3389/fpsyg.2016.01474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Minges KE, Chao AM, Irwin ML, et al. Classroom standing desks and sedentary behavior: a systematic review. Pediatrics 2016;137:e20153087. 10.1542/peds.2015-3087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tremblay MS, Aubert S, Barnes JD, et al. Sedentary behavior research network (SBRN) – terminology consensus project process and outcome. Int J Behav Nutr Phys Act 2017;14:75. 10.1186/s12966-017-0525-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chaput J-P, Willumsen J, Bull F, et al. WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5–17 years: summary of the evidence. Int J Behav Nutr Phys Act 2020;17:141. 10.1186/s12966-020-01037-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dornhecker M, Blake J, Benden M, et al. The effect of stand-biased desks on academic engagement: an exploratory study. Int J Health Promot Educ 2015;53:271–80. 10.1080/14635240.2015.1029641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Australian Institute of Health and Welfare . Australia’s Health 2022. Canberra: AIHW, 2022. [Google Scholar]
- 11.Department of Health . Physical Activity and Exercise Guidelines for All Australians. Canberra: Australian Government, 2021. [Google Scholar]
- 12.Ridgers ND, Salmon J, Ridley K, et al. Agreement between activPAL and actigraph for assessing children's sedentary time. Int J Behav Nutr Phys Act 2012;9:15. 10.1186/1479-5868-9-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ridgers ND, Timperio A, Crawford D, et al. Five-year changes in school recess and lunchtime and the contribution to children's daily physical activity. Br J Sports Med 2012;46:741–6. 10.1136/bjsm.2011.084921 [DOI] [PubMed] [Google Scholar]
- 14.Victoria State Government . Active schools toolkit. Victoria: Australia: Department of Education and Training, Available: https://www.education.vic.gov.au/school/teachers/teachingresources/discipline/physed/Pages/activeschoolstoolkit.aspx [Google Scholar]
- 15.Centers for Disease Control and Prevention . Comprehensive School Physical Activity Programs: A Guide for Schools. Atlanta, GA: U.S: Department of Health and Human Services, 2013. [Google Scholar]
- 16.World Health Organization . Global action plan on physical activity 2018-2030: more active people for a healthier world. World Health Organization, 2018. [Google Scholar]
- 17.Lai SK, Costigan SA, Morgan PJ, et al. Do school-based interventions focusing on physical activity, fitness, or fundamental movement skill competency produce a sustained impact in these outcomes in children and adolescents? A systematic review of follow-up studies. Sports Med 2014;44:67–79. 10.1007/s40279-013-0099-9 [DOI] [PubMed] [Google Scholar]
- 18.Hegarty LM, Mair JL, Kirby K, et al. School-based interventions to reduce sedentary behaviour in children: a systematic review. AIMS Public Health 2016;3:520–41. 10.3934/publichealth.2016.3.520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Love R, Adams J, van Sluijs EMF. Are school-based physical activity interventions effective and equitable? A meta-analysis of cluster randomized controlled trials with accelerometer-assessed activity. Obes Rev 2019;20:859–70. 10.1111/obr.12823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koorts H, Timperio A, Abbott G, et al. Is level of implementation linked with intervention outcomes? process evaluation of the TransformUs intervention to increase children's physical activity and reduce sedentary behaviour. Int J Behav Nutr Phys Act 2022;19:122. 10.1186/s12966-022-01354-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lonsdale C, Rosenkranz RR, Peralta LR, et al. A systematic review and meta-analysis of interventions designed to increase moderate-to-vigorous physical activity in school physical education lessons. Prev Med 2013;56:152–61. 10.1016/j.ypmed.2012.12.004 [DOI] [PubMed] [Google Scholar]
- 22.Parrish A-M, Chong KH, Moriarty AL, et al. Interventions to change school recess activity levels in children and adolescents: a systematic review and meta-analysis. Sports Med 2020;50:2145–73. 10.1007/s40279-020-01347-z [DOI] [PubMed] [Google Scholar]
- 23.Escalante Y, García-Hermoso A, Backx K, et al. Playground designs to increase physical activity levels during school recess: a systematic review. Health Educ Behav 2014;41:138–44. 10.1177/1090198113490725 [DOI] [PubMed] [Google Scholar]
- 24.Santos F, Sousa H, Gouveia ÉR, et al. School-based family-oriented health interventions to promote physical activity in children and adolescents: a systematic review. Am J Health Promot 2023;37:243–62. 10.1177/08901171221113836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hinckson E, Salmon J, Benden M, et al. Standing classrooms: research and lessons learned from around the world. Sports Med 2016;46:977–87. 10.1007/s40279-015-0436-2 [DOI] [PubMed] [Google Scholar]
- 26.Salmon J, Arundell L, Cerin E, et al. Transform-us! cluster RCT: 18-month and 30-month effects on children’s physical activity, sedentary time and Cardiometabolic risk markers. Br J Sports Med 2023;57:311–9. 10.1136/bjsports-2022-105825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lonsdale C, Sanders T, Cohen KE, et al. 'Erratum to: Scaling-up an efficacious school-based physical activity intervention: study protocol for the 'Internet-based professional learning to help teachers support activity in youth' (iPLAY) cluster randomized controlled trial and scale-up implementation evaluation'. BMC Public Health 2016;16:1026. 10.1186/s12889-016-3724-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cassar S, Salmon J, Timperio A, et al. Adoption, implementation and sustainability of school-based physical activity and sedentary behaviour interventions in real-world settings: a systematic review. Int J Behav Nutr Phys Act 2019;16:120. 10.1186/s12966-019-0876-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Koorts H, Bauman A, Edwards N, et al. Tensions and paradoxes of scaling up: a critical reflection on physical activity promotion. Int J Environ Res Public Health 2022;19:14284. 10.3390/ijerph192114284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 1999;89:1322–7. 10.2105/ajph.89.9.1322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Salmon J, Arundell L, Hume C, et al. A cluster-randomized controlled trial to reduce sedentary behavior and promote physical activity and health of 8-9 year olds: the transform-us! study. BMC Public Health 2011;11:759. 10.1186/1471-2458-11-759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall, 1986. [Google Scholar]
- 33.Rachlin H. Judgement, Decision, and Choice: A Cognitive/Behavioral Synthesis. New York: WH Freeman, 1989. [Google Scholar]
- 34.Bronfenbrenner U. Six theories of child development: revised formulations and current issues. In: Vasta R, ed. Ecological Systems Theory. London: Jessica Kingsley Publishers, 1992: 187–249. [Google Scholar]
- 35.Available: https://victoriancurriculum.vcaa.vic.edu.au/ [Accessed 10 Jun 2018].
- 36.Available: https://www.australiancurriculum.edu.au/ [Accessed 18 May 2018].
- 37.Curran GM, Bauer M, Mittman B, et al. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care 2012;50:217–26. 10.1097/MLR.0b013e3182408812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Peters DH, Tran NT, Adam T. Implementation Research in Health: A Practical Guide. Alliance for Health Policy and Systems Research, 2013. [Google Scholar]
- 39.Available: www.education.vic.gov.au/Documents/about/department/brochureJuly.docx [Accessed 10 Aug 2016].
- 40.Dunton GF, Liao Y, Grana R, et al. State-wide dissemination of a school-based nutrition education programme: a RE-AIM (reach, efficacy,adoption, implementation, maintenance) analysis. Public Health Nutr 2014;17:422–30. 10.1017/S1368980012005186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shadish WR, Cook TD, Campbell DT. Experimental and quasi-experimental designs for generalized causal inference. Boston: Houghton Miffler Company, 2002. [Google Scholar]
- 42.Salmon J, Arundell L, Cerin E, et al. The transform-us! cluster RCT: 18- and 30-month effects on children’s physical activity, sedentary time and Cardiometabolic risk markers. Br J Sports Med 2023;57:311–9. 10.1136/bjsports-2022-105825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Koorts H, Eakin E, Estabrooks P, et al. Implementation and scale up of population physical activity interventions for clinical and community settings: the PRACTIS guide. Int J Behav Nutr Phys Act 2018;15:51. 10.1186/s12966-018-0678-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Australian Bureau of Statistics . Information paper: an introduction to socio-economic indexes for areas (SEIFA); 2006.
- 45.World Health Organization . Practical Guidance for Scaling Up Health Service Innovations. Geneva, Switzerland: World Health Organization, 2009. [Google Scholar]
- 46.Milat AJ, Newson R, King L. Increasing the Scale of Population Health Interventions: A Guide. Sydney: NSW Ministry of Health: Centre for Epidemiology and Evidence, 2014. [Google Scholar]
- 47.O’Hara BJ, Phongsavan P, King L, et al. ''Translational formative evaluation': critical in up-Scaling public health programmes'. Health Promot Int 2014;29:38–46. 10.1093/heapro/dat025 [DOI] [PubMed] [Google Scholar]
- 48.Wandersman A, Duffy J, Flaspohler P, et al. Bridging the gap between prevention research and practice: the interactive systems framework for dissemination and implementation. Am J Community Psychol 2008;41:171–81. 10.1007/s10464-008-9174-z [DOI] [PubMed] [Google Scholar]
- 49.Meyers DC, Durlak JA, Wandersman A. The quality implementation framework: a synthesis of critical steps in the implementation process. Am J Community Psychol 2012;50:462–80. 10.1007/s10464-012-9522-x [DOI] [PubMed] [Google Scholar]
- 50.Wiltsey Stirman S, Kimberly J, Cook N, et al. The Sustainability of new programs and innovations: a review of the empirical literature and recommendations for future research. Implement Sci 2012;7:17. 10.1186/1748-5908-7-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Michie S, Johnston M, Francis J, et al. From theory to intervention: mapping theoretically derived behavioural determinants to behaviour change techniques. Applied Psychology 2008;57:660–80. 10.1111/j.1464-0597.2008.00341.x Available: https://iaap-journals.onlinelibrary.wiley.com/toc/14640597/57/4 [DOI] [Google Scholar]
- 52.Simmons R, Shiffman J. Scaling up health service innovations: a framework for action. In: Simmons R, Fajans P, Ghiron L, eds. Scaling Up Health Service Delivery. Geneva: World Health Organization, 2007: 1–30. [Google Scholar]
- 53.Proctor EK, Powell BJ, McMillen JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci 2013;8:139. 10.1186/1748-5908-8-139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dusenbury L, Brannigan R, Hansen WB, et al. Quality of implementation: developing measures crucial to understanding the diffusion of preventive interventions. Health Educ Res 2005;20:308–13. 10.1093/her/cyg134 [DOI] [PubMed] [Google Scholar]
- 55.Fleuren M, Wiefferink K, Paulussen T. Determinants of innovation within health care organizations: literature review and Delphi study. Int J Qual Health Care 2004;16:107–23. 10.1093/intqhc/mzh030 [DOI] [PubMed] [Google Scholar]
- 56.Chaudoir SR, Dugan AG, Barr CHI. Measuring factors affecting implementation of health innovations: a systematic review of structural, organizational, provider, patient, and innovation level measures. Implement Sci 2013;8:22. 10.1186/1748-5908-8-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Braun V, Clarke V. To saturate or not to saturate? Questioning data saturation as a useful concept for thematic analysis and sample-size Rationales. Qualitative Research in Sport, Exercise and Health 2021;13:201–16. 10.1080/2159676X.2019.1704846 [DOI] [Google Scholar]
- 58.Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res 2016;26:1753–60. 10.1177/1049732315617444 [DOI] [PubMed] [Google Scholar]
- 59.Rutterford C, Copas A, Eldridge S. Methods for sample size determination in cluster randomized trials. Int J Epidemiol 2015;44:1051–67. 10.1093/ije/dyv113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nettlefold L, Naylor PJ, Macdonald HM, et al. Scaling up action schools! BC: how does voltage drop at scale affect student level outcomes? A cluster randomized controlled trial. Int J Environ Res Public Health 2021;18:10. 10.3390/ijerph18105182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Evenson KR, Catellier DJ, Gill K, et al. Calibration of two objective measures of physical activity for children. J Sports Sci 2008;26:1557–65. 10.1080/02640410802334196 [DOI] [PubMed] [Google Scholar]
- 62.Gabel L, Ridgers ND, Della Gatta PA, et al. Associations of sedentary time patterns and TV viewing time with inflammatory and endothelial function biomarkers in children. Pediatr Obes 2016;11:194–201. 10.1111/ijpo.12045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ridgers ND, Timperio A, Crawford D, et al. Five-year changes in school recess and lunchtime and the contribution to children’s daily physical activity. Br J Sports Med 2012;46:741–6. 10.1136/bjsm.2011.084921 [DOI] [PubMed] [Google Scholar]
- 64.Arundell L, Ridgers ND, Veitch J, et al. 5-year changes in Afterschool physical activity and sedentary behavior. Am J Prev Med 2013;44:605–11. 10.1016/j.amepre.2013.01.029 [DOI] [PubMed] [Google Scholar]
- 65.Kuczmarski RJ, Ogdon CL, Guo SS. Vital health Statistics. In: CDC Growth Charts for the United States: Methods and Development 11. Washington: Statistics NCfH, 2000: 2002. [PubMed] [Google Scholar]
- 66.Wille N, Badia X, Bonsel G, et al. Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. quality of life research: an international Journal of quality of life aspects of treatment, care and rehabilitation. 2010;19:875–86. 10.1007/s11136-010-9648-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dalziel K, Catchpool M, García-Lorenzo B, et al. Feasibility, validity and differences in adolescent and adult EQ-5D-Y health state valuation in Australia and Spain: an application of best-worst Scaling. Pharmacoeconomics 2020;38:499–513. 10.1007/s40273-020-00884-9 [DOI] [PubMed] [Google Scholar]
- 68.Ridgers ND, Timperio A, Crawford D, et al. Validity of a brief self-report instrument for assessing compliance with physical activity guidelines amongst adolescents. J Sci Med Sport 2012;15:136–41. 10.1016/j.jsams.2011.09.003 [DOI] [PubMed] [Google Scholar]
- 69.Telford A, Salmon J, Jolley D, et al. Reliability and validity of physical activity questionnaires for children. The Children’s Leisure Activities Study Survey (CLASS) 2004;16:64. 10.1123/pes.16.1.64 [DOI] [Google Scholar]
- 70.Salmon J, Timperio A, Telford A, et al. Association of family environment with children's television viewing and with low level of physical activity. Obes Res 2005;13:1939–51. 10.1038/oby.2005.239 [DOI] [PubMed] [Google Scholar]
- 71.Naylor P-J, Macdonald HM, Reed KE, et al. Action schools! BC: a Socioecological approach to modifying chronic disease risk factors in elementary school children. Prev Chronic Dis 2006;3:A60. [PMC free article] [PubMed] [Google Scholar]
- 72.Shea CM, Jacobs SR, Esserman DA, et al. Organizational readiness for implementing change: a Psychometric assessment of a new measure. Implement Sci 2014;9:7. 10.1186/1748-5908-9-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Holtrop JS, Rabin BA, Glasgow RE. Qualitative approaches to use of the RE-AIM framework: rationale and methods. BMC Health Serv Res 2018;18:177. 10.1186/s12913-018-2938-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Joffe H, Yardley L. Content and thematic analysis. In: Marks D, Yardley L, eds. Research Methods for Clinical and Health Psychology. Sage Publications, 2004: 56–66. [Google Scholar]
- 75.Wasserstein RL, Schirm AL, Lazar NA. 'Moving to a world beyond 'P < 0.05'' Am Stat 2019;73:1–19. 10.1080/00031305.2019.1583913 [DOI] [Google Scholar]
- 76.Department of Education and Training . The education state: schools. State of Victoria, Department of Education and Training [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-078410supp001.pdf (265.4KB, pdf)
bmjopen-2023-078410supp002.pdf (176.6KB, pdf)
bmjopen-2023-078410supp003.pdf (206.3KB, pdf)
bmjopen-2023-078410supp004.pdf (91.6KB, pdf)
bmjopen-2023-078410supp005.pdf (64KB, pdf)