Abstract
Objective
This study aimed to assess whether workplace exposures as estimated via a COVID-19 job exposure matrix (JEM) are associated with SARS-CoV-2 in the UK.
Methods
Data on 244 470 participants were available from the Office for National Statistics Coronavirus Infection Survey (CIS) and 16 801 participants from the Virus Watch Cohort, restricted to workers aged 20–64 years. Analysis used logistic regression models with SARS-CoV-2 as the dependent variable for eight individual JEM domains (number of workers, nature of contacts, contact via surfaces, indoor or outdoor location, ability to social distance, use of face covering, job insecurity, and migrant workers) with adjustment for age, sex, ethnicity, index of multiple deprivation (IMD), region, household size, urban versus rural area, and health conditions. Analyses were repeated for three time periods (i) February 2020 (Virus Watch)/April 2020 (CIS) to May 2021), (ii) June 2021 to November 2021, and (iii) December 2021 to January 2022.
Results
Overall, higher risk classifications for the first six domains tended to be associated with an increased risk of infection, with little evidence of a relationship for domains relating to proportion of workers with job insecurity or migrant workers. By time there was a clear exposure–response relationship for these domains in the first period only. Results were largely consistent across the two UK cohorts.
Conclusions
An exposure–response relationship exists in the early phase of the COVID-19 pandemic for number of contacts, nature of contacts, contacts via surfaces, indoor or outdoor location, ability to social distance and use of face coverings. These associations appear to have diminished over time.
Keywords: cohort, coronavirus, epidemiology, JEM, occupation, virus, workplace
COVID-19 has been responsible for millions of deaths globally (1). Risk of infection with SARS-CoV-2 has been found to vary with occupation (2, 3), and differences in workplace exposure is likely to explain some of this variation (4, 5). Accordingly, there is interest in identifying the occupations at increased risk and workplace features and mitigation strategies that modulate this risk. Workplace factors associated with exposure include number and type of daily contacts, ability to socially distance, and workplace ventilation (4). Studies of social contact patterns (6, 7) suggest that workers in retail, hospitality, healthcare, education and transportation have the highest number of workplace contacts. Baker et al (8) identified healthcare, protective service, office and administrative support, education, community and social services and construction and extraction occupations as all having a high level of exposure to infection. Evidence varies on whether this perceived exposure translates to increased COVID-19 disease and mortality (3, 9–11). In addition, differences in occupational risk have varied over time, coinciding with changes in the nature of work, the mitigations in place, and differing levels immunity from prior infection (12–15).
The COVID-19 job exposure matrix (COVID-19-JEM) has been developed to categorize occupations according to workplace factors believed to be associated with SARS-CoV-2 infection (4). This JEM was based on assessments from occupational exposure experts from three countries (Denmark, The Netherlands, United Kingdom) regarding eight distinct risk domains related to the risk of transmission [(i) number of contacts (ii), nature of contacts (iii), contaminated workspaces (iv), location of the worksite]; the presence of mitigation measures [(v) social distance and (vi) the use of face covering]; and the level of precarity of the occupation involved [(vii) proportion of workers with income insecurity and (viii) proportion of migrant workers]. The risk levels are described in table 1. Distinct JEM scores for each country were established to account for the presence of different guidelines and mitigation measures at a time following the first lockdown. A validation exercise using 6794 participants has already been performed in The Netherlands involving comparison of the risk scores assigned by the COVID-19-JEM against self-reported data from surveys performed for this purpose (16). Results suggested good agreement between the JEM scores and the self-reported data for most dimensions except face covering. Validation of the separate JEM domains against self-reported COVID-19 illness was also performed. Higher COVID-19-JEM assigned risk scores were associated with higher odds ratios (OR 1.28–1.80) of COVID-19 for all except the precarious dimensions (16) Here we extend the validation exercise to two large UK cohorts and conduct a time-stratified analysis to explore whether the utility of the JEM extends to time periods later in the pandemic.
Table 1.
Description of 8 domains of the job exposure matrix (JEM).
| Dimension | Description | Abbreviation used in tables and figures | Levels |
|---|---|---|---|
| 1 | The number of workers at worksite | Number | Homeworking/lone working (No risk) |
| <10 workers/day (Low risk) | |||
| 10–30 workers/day (Elevated risk) | |||
| >30 workers/day (High risk) | |||
| 2 | The nature of contacts with co-workers, general public or patients with COVID-19 | Nature | Homeworking/lone working (No risk) |
| Co-workers only (Low risk) | |||
| General public (Elevated risk) | |||
| Patients, including with C19 (High risk) | |||
| 3 | The risk through contaminated work surfaces and materials | Surfaces | Homeworking/lone working (No risk) |
| Frequently sharing contact surfaces with co-workers (Low risk) | |||
| Occasionally sharing contact surfaces with general public (Elevated risk) | |||
| Frequently sharing contact surfaces with general public (High risk) | |||
| 4 | Location of work: indoors or outdoors | Location | Homeworking/lone working (No risk) |
| Mostly outdoors (Low risk) | |||
| Partly indoor (Elevated risk) | |||
| Mostly indoor (High risk) | |||
| 5 | The possibility to keep at least 1m of social distance | Distancing | Homeworking/lone working (No risk) |
| Always maintained (Low risk) | |||
| Cannot always be maintained (Elevated risk) | |||
| can never be maintained (High risk) | |||
| 6 | The need and usage of face covering | Face covering | Homeworking/lone working (No risk) |
| Always (Low risk) | |||
| Not always while in proximity to others (Elevated risk) | |||
| Face covering not feasible (High risk) | |||
| 7 | Job insecurity: proportion of flexible labour contracts | Insecurity | 0 (None) 1–10% (Low) |
| 11–25% (Elevated) | |||
| >25% (High) | |||
| 8 | Migrant workers: proportion of migrant workers | Migrants | 0 (None) |
| 1–10% (Low) | |||
| 11–25% (Elevated) | |||
| >25% (High) |
In the present study, we implemented the UK specific risk scores/assignment of the COVID-19-JEM on two separate large UK studies containing information on occupation and SARS-CoV-2 infections with the aim of (i) evaluating the performance of the UK edition of the COVID-19 JEM as a tool for assessing occupational exposure to SARS-CoV-2 and (ii) assessing the relationship between the exposure affecting factors included in the JEM and SARS-CoV-2 infection risk; and (iii) assessing whether this relationship is consistent over time.
Description of the job exposure matrix
The COVID-19-JEM was established using expert judgement and consensus (4). The JEM was developed with reference to the conditions present during the period following the easing of the first strict lockdown measures. It was anticipated that workers were encouraged to work from home, where possible, but those who needed to attend the workplace were allowed to work. It was also assumed that hand washing, use of personal protective equipment (PPE) and face coverings and social distancing in the workplace were advised, and vaccination programmes had not yet started. The JEM contained eight domains representing factors that were judged to affect occupational exposure to SARS-CoV-2, classified by 4 risk levels (table 1). The COVID-19-JEM was coded according to the International Standard Classification of Occupations 2008 (ISCO-08) coding system (17) and includes specific scores for The Netherlands, Denmark and the UK.
For the UK component, the JEM was translated from the ISCO-08 coding system to the UK Standard Occupational Classification (SOC) 2010 version coding system (18). Translation was facilitated by a crosswalk developed by the UK Office for National Statistics (ONS) (19). Evaluation of occupation descriptions between the two coding systems revealed that there was no direct correspondence, with 46 ISCO codes not represented in the SOC system and 42 SOC codes not represented in the ISCO system. The same three UK experts involved in the development of the main JEM scored those the domains of the JEM related to risk for transmission and mitigation measures using the same consensus procedure. Domains related to income insecurity and migrant workers used UK data extracted from the Great Britain and Scottish components of the Annual Population Survey (APS) April 2019 to March 2020 (20) and the UK broad Labour Force Survey (LFS) from August to October 2010 (21), respectively (as utilized in the original JEM). To minimize bias due to changes in perception of experts by time, the translation to SOC 2010 occurred simultaneously with the original JEM.
Datasets
Virus Watch is a prospective household cohort study based in England and Wales (58 560 participants from 28 449 households). Participants provide demographic and health-related information at enrolment; they then complete weekly surveys reporting any symptoms, test results of lateral flow or polymerase chain reaction (PCR) tests taken under national testing scheme, and vaccinations, as well as monthly surveys concerning sociobehavioral and clinical factors. Subsets of participants received in-clinic serological testing and/or performed monthly at-home finger-prick serological tests. All participants’ records were linked to national databases of SARS-CoV-2 PCR and lateral flow test results. SARS-CoV-2 infection status relates to any evidence of infection via self-reported, national database or serological test. Upon study enrolment, participants are asked about their employment status and, if employed or self-employed, prompted to enter free text for their job title; four-digit SOC codes were derived from free-text job titles using semi-automatic processing using Cascot Version 5.6.3 (warwick.ac.uk/fac/soc/ier/software/cascot/) – the ONS-recommended methodology for assigning SOC codes to free-text data. The survey began in June 2020 but retrospectively looked at infection status from Feb 2020 onwards. Data used relates to Feb 2020 to Jan 2022. Further details on the Virus Watch cohort and methodology can be found on its study protocol available at bmjopen.bmj.com/content/11/6/e048042, and details of response rates at ucl-virus-watch.net. Approximately 50% of the cohort continued to provide responses to the weekly follow-up survey across the study period; however, infection status was also ascertained based on linkage to national databases.
The ONS COVID-19 Infection Survey (CIS) is a repeated cross-sectional household survey designed to be representative of the UK population for calculation of monthly UK prevalence estimates of SARS-CoV-2 virus. Participation starts with five weeks of weekly visits for each household, followed by monthly visits. Each visit includes a survey and a COVID-19 PCR test for each household member regardless of symptoms. At each visit, participants are asked about their work status and job title; ONS used free text job titles to derive four-digit SOC codes via a combination of automatic methods and manual coding. We used the data from April 2020 to January 2022, which was accessed via the Secure Research Server (SRS) using Stata 17 (22). A detailed description of the CIS methodology is provided within its study protocol available at www.ndm.ox.ac.uk/covid-19/covid-19-infection-survey/protocol-and-information-sheetsand detail of response and retention rates can be found at www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/datasets/COVID19infectionsurveytechnicaldata.
Occupation data for both cohorts is published elsewhere (12, 13)
Statistical methods
All analyses were restricted to working age adults (20–64 years) who reported being employed or self-employed at enrolment into the studies. Missing covariate data were known to be sparse across adjustment covariates (0–1.3%), so we restricted data to complete cases on these variables. Relationships between the individual JEM risk domains and SARS-CoV-2 infection status (ever/never within the time period of interest) were evaluated using logistic regression. In Virus Watch, the infection status was derived based on any serological or virological evidence of infection (positive lateral flow (LFT), PCR, anti-nucleocapsid antibody serological test, or anti-spike antibody serological test in absence of vaccination). For the CIS and the Virus Watch serological sub-cohort, only tests conducted as part of the survey (approximately monthly) were included and, therefore, infection status is independent of national testing strategies. Infection rates for these two cohorts will not include positive infections between surveys and therefore are not estimates of period prevalence. The proportion of participants having at least one infection for CIS and the Virus Watch serological sub-cohort will be substantially lower than the proportion for the full Virus Watch cohort, which includes all self-reported test results.
Four digit SOC codes were used to derive covariates relating to perceived occupational exposure on the 8 JEM domains. These related to the first available SOC within each time period for CIS and baseline occupation for Virus Watch. ‘No risk’ was set as the reference category for all JEM exposures, with the exception of the migrant workers domain for Virus Watch where it was set at ‘low risk’ due to small cell sizes in the ‘no risk’ category. A ‘missing’ category was included for working participants for whom a four digit SOC code was not available, and this was used in summary tables and regression (for comparison). The coefficients relating to the missing category are not presented in the coefficient plots. A correlation matrix of Spearman’s rank correlation between derived JEM domain scores was produced.
Potential confounders were selected and included on the models based on a directed acylic graphs (DAG) an interactive version, of which is available at dagitty.net/dags.html?id=mGNoZU. We adjusted all estimates for age (4/5 ordered categories), sex, minority ethnicity (White British versus other), geographic region (ONS national region), deprivation based on indices of multiple deprivation (IMD) derived from postcode (23), household size, urban versus rural area, and health status. For Virus Watch, clinically vulnerable (yes/no) was defined as any condition on the UK NHS/government list of clinically vulnerable conditions, obesity, and/or having received an NHS shielding letter (24). For the CIS, health conditions was a yes response to the question “Do you have any physical or mental health conditions or illnesses lasting or expected to last 12 months or more (excluding any long-lasting COVID-19 symptoms)?”
To investigate whether the association between JEM domains and risk of infection varied across different pandemic phases, we then repeated the analysis stratified by time period. The first time period corresponded to the first and second waves of the pandemic (up to May 2021), the second to the third pandemic wave (June 2021 to November 2021), and the third to the Omicron-dominated fourth wave (December 2021–January 2022). For Virus Watch, period 1 comprised a large amalgamated time period as serological testing began during the second wave, and thus infections could be attributed to either the first or second wave; mass population testing also only became available post-first-wave in England and Wales. Infections that were derived from serological testing without a prior negative result could not be attributed to a particular date. JEM domains relating to job insecurity and migrant workers were excluded from the time-stratified analyses due to low cells sizes for some risk levels.
For Virus Watch, to address differences in access and virological/antigen testing protocols across occupations, as well as address asymptomatic infection, we also performed a sensitivity analysis limited to participants who had undergone serological testing (N=6712). As above, JEM domains relating to job insecurity and migrant workers were excluded from this analysis due to low cells sizes for some risk levels. Data regarding vaccination status were available for Virus Watch but not CIS (for this project), and we performed a sensitivity analysis adjusting for vaccination status overall (0, 1, 2, or 3 doses following recommendations for all adults in the UK by the end of the study period), and stratified by time period.
Results
Demographic features of included Virus Watch and CIS participants are reported in table 2. There were 244 470 participants from the CIS cohort and 16 479 from Virus Watch who met our inclusion criteria and were included in the analyses. Overall, the two studies shared comparable demographic distributions regarding gender and ethnicity. Virus Watch contained a higher proportion of participants aged 60–64 years and in 1–2 person households with a greater proportion of participants residing in East England. Scotland was geographically represented only in the CIS study. Table 3 reports SARS-CoV-2 infection status by each risk category for all JEM domains for the full cohorts (CIS and Virus Watch) and serological sub-cohort (Virus Watch). In the supplementary material (www.sjweh.fi/article/4076), table S2 shows there was strong correlation between some domains of the JEM, with the strongest correlations observed between the domains related to nature and surfaces (0.90) and number and nature (0.84).
Table 2.
Demographic characteristics of workers participating in the COVID-19 Infection survey (CIS) and Virus Watch. [IMD= index of multiple deprivation.]
| Characteristic | CIS N=244 470 | Virus Watch N=16 479 |
|---|---|---|
|
|
|
|
| N (%) | N (%) | |
| Age (years) | ||
| 20–29 | 34 744 (14) | 1560 (9.5) |
| 40–49 | 55 436 (23) | 3010 (18) |
| 30–39 | 63 688 (26) | 3661 (22) |
| 50–59 | 67 803 (28) | 4534 (28) |
| 60–64 | 22 799 (9.3) | 3714 (23) |
| Sex | ||
| Female | 128 359 (52) | 9090 (55) |
| Male | 116 111 (47) | 7389 (45) |
| Ethnic group | ||
| White | 233 306 (91) | 14 687 (89) |
| Black | 2827 (1.2) | 208 (1.3) |
| Mixed | 3748 (1.5) | 308 (1.9) |
| Asian | 11 837 (4.8) | 1165 (7.1) |
| Other ethnicity | 2605 (1.0) | 111 (0.67) |
| Health conditions | 37 907 (16) | |
| Clinically vulnerable | 8606 (52) | |
| IMD quartile (CIS)/quintile (VW) | ||
| 1 | 36 376 (15) | 1799 (11) |
| 2 | 58 459 (24) | 2945 (18) |
| 3 | 70 300 (29) | 3395 (21) |
| 4 | 79 335 (32) | 4057 (25) |
| 5 | 4283 (26) | |
| Household size | ||
| 1 person | 31 977 (13) | 3153 (19) |
| 2 people | 89 782 (37) | 7084 (43) |
| 3 people | 51 003 (21) | 2772 (17) |
| 4 people | 51 521 (21) | 2584 (16) |
| 5 or more people | 20 187 (8.3) | 886 (5.4) |
| Region | ||
| East Midlands | 15 239 (6.2) | 1433 (8.7) |
| East of England | 22 259 (9.1) | 3311 (20) |
| London | 51 554 (21) | 3304 (20) |
| North East | 8092 (3.3) | 757 (4.6) |
| North West | 26 830 (11) | 1641 (10.0) |
| South East | 30 117 (12) | 3125 (19) |
| South West | 18 252 (7.5) | 1043 (6.3) |
| Wales | 11 229 (4.6) | 340 (2.1) |
| West Midlands | 17 312 (7.1) | 750 (4.6) |
| Yorkshire and The Humber | 18 667 (7.6) | 775 (4.7) |
| Scotland | 18 550 (7.6) | NA |
Table 3.
Participants with at least one infection by JEM domain by risk level for the COVID-19 Infection survey (CIS) and two Virus Watch cohorts (full cohort and serological sub-cohort). See table 1 for domain descriptions. [NA2=suppressed for statistical disclosure control due to small cell size; SOC= Standard Occupational Classification]
| CIS N=25 4851 | Virus Watch N=39 951 | Virus Watch serological sub-cohort N=6851 | |
|---|---|---|---|
|
|
|
|
|
| N (%) | N (%) | N (%) | |
| Number at worksite | |||
| Homeworking/lone working | 5549 (9.4) | 1165 (23) | 195 (8.6) |
| <10 workers/day | 2684 (10) | 585 (22) | 103 (9.0) |
| 10–30 workers/day | 4862 (10) | 1108 (26) | 208 (12) |
| >30 workers/day | 4843 (11) | 1026 (26) | 172 (11) |
| Nature of contacts | |||
| Homeworking/lone working | 5639 (9.4) | 1175 (23) | 197 (8.6) |
| Co-workers only | 3574 (10) | 844 (24) | 165 (11) |
| General public | 7652 (11) | 1582 (25) | 265 (10) |
| Patients including with C-19 | 1073 (9.0) | 283 (29) | 51 (13) |
| Surfaces | |||
| Homeworking/lone working | 6607 (9.5) | 1386 (22) | 239 (8.7) |
| Frequently sharing contact surfaces with co-workers | 2900 (11) | 697 (25) | 138 (12) |
| Occasionally sharing contact surfaces with general public | 2270 (10) | 566 (25) | 92 (9.6) |
| Frequently sharing contact surfaces with general public | 6161 (11) | 1235 (26) | 209 (11) |
| Indoor or outdoor | |||
| Homeworking/lone working | 5549 (9.4) | 1165 (23) | 195 (8.6) |
| Mostly outdoors | 578 (11) | 92 (23) | 12 (7.6) |
| Partly indoor | 10 332 (10) | 209 (22) | 43 (11) |
| Mostly indoor | 10 332 (10) | 2418 (25) | 428 (11) |
| Social sistancing | |||
| Homeworking/lone working | 5549 (9.4) | 1165 (23) | 195 (8.6) |
| Always maintained | 5602 (9.8) | 1293 (23) | 241 (10) |
| Cannot always be maintained | 4145 (11) | 902 (26) | 148 (11) |
| Can never be maintained | 2642 (12) | 524 (30) | 94 (14) |
| Protective face mask | |||
| Homeworking/lone working | 5549 (9.4) | 1165 (23) | 195 (8.6) |
| Always | 3120 (9.9) | 733 (27) | 135 (12) |
| Not always while in proximity to others | 9091 (11) | 1908 (24) | 329 (10) |
| Face covering not feasible | 178 (11) | 78 (29) | 19 (18) |
| Job Insecurity | |||
| <1% | 9023 (10) | 1865 (24) | 311 (9.6) |
| 1–10% | 8175 (10) | 1886 (24) | 344 (10) |
| 11–25% | 586 (11) | 116 (32) | NA2 |
| >25% | 154 (14) | 17 (26) | NA2 |
| Migrant workers | |||
| <1% | 26 (12) | 5 (25) | NA2 |
| 1–10% | 10315 (10) | 2077 (24) | 382 (10) |
| 11–25% | 7494 (10) | 1785 (25) | 290 (10.0) |
| >25% | 103 (12) | 17 (29) | NA2 |
| Missing SOC | 7547 (11) | 111 (23) | 7 (10) |
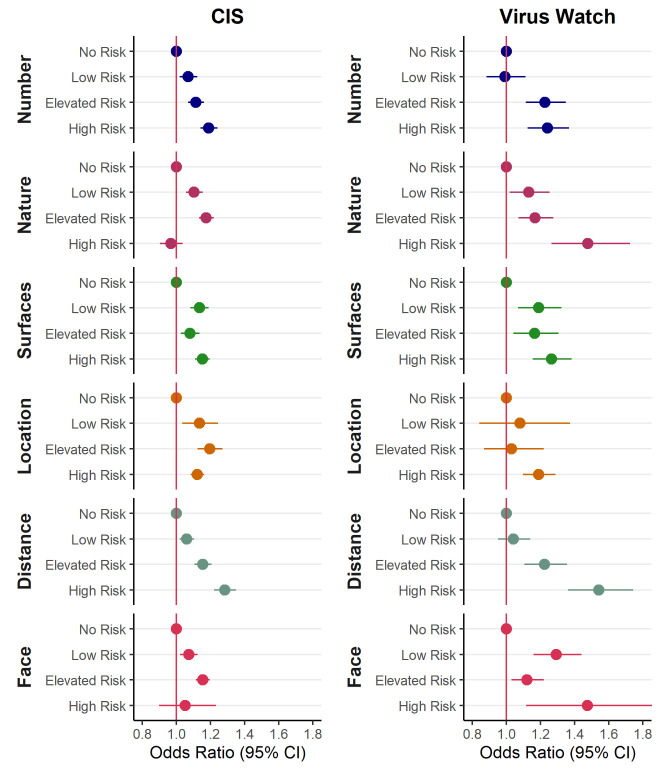
Figure 1 shows the relationship between the first six JEM domains and COVID-19 infection. Estimates for all eight domains are shown in supplementary table S1, showing consistency across the two cohorts. Higher risk classifications were generally associated with increased risk of infection for the first six domains, although not always displaying an exposure–response relationship across all four categories. For domains relating to insecurity and migration, the association was less clear, such that classification as ‘no risk’ was not consistently lower than other risk categories.
Figure 1.
Odds ratios by level of exposure for 6 domains of the job exposure matrix (compared to the no risk group) from [Virus Watch (N=16 801) and COVID-19 Infection survey (CIS) (N=244 470)] participants in work and aged 20-64. Models adjusted for age quintile, sex, ethnicity, index of multiple deprivation (IMD)/health conditions, region, household size, urban versus rural area, and presence of health conditions. Domains relating to insecurity and migrant workers not displayed here due to imprecision. See table 1 for explanation of abbreviations. [CI=confidence intervals.]
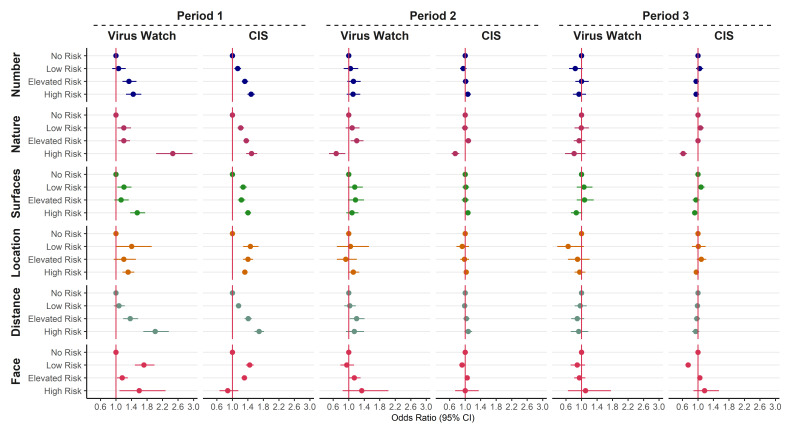
Figure 2 and table 3 show the relationship between the domains of the JEM and COVID-19 infection during three time periods. Generally, patterns across both cohorts and the Virus Watch serological sub-cohort are consistent. During time period 1, there is a clear exposure–response relationship in both cohorts between the level of risk attributed by the JEM and the risk of SARS-CoV-2 infection for the domains relating to the number of contacts, the nature of contacts and social distancing; with increasing OR comparing low, elevated and high risk groups to the no risk group. Other domains (relating to surfaces, location and distancing) have OR in the expected direction, showing increased risks for those in the low, elevated and high-risk groups when compared to no risk, but the dose–response relationship is not evident. During time periods 2 and 3, there is little evidence of a relationship between the JEM domains and the risk of infection, most confidence intervals (CI) straddle the line of no difference and overlap. One exception is the domain relating to the nature of contacts; the ‘high risk’ group (contact with patients, including those suspected with COVID-19) in this domain is observed to have a reduced risk of infection in time periods 2 and 3 for both cohorts. Another exception is the domain relating to use of face coverings, where the low risk group appears to have a reduced risk of infection compared to no risk in time period 3 for the CIS data.
Figure 2.
Odds ratios for COVID-19 by level of exposure for 6 domains of the job exposure matrix (compared to the no risk group) from [Virus Watch (N=16 801) and COVID-19 Infection survey (CIS) (N=244 470)] participants in work and aged 20-64. Data split into 3 time periods and models adjusted for age, sex, ethnicity, index of multiple deprivation (IMD), region, household size, urban versus rural area, and presence of health conditions. See table 1 for explanation of abbreviations. Domains relating to insecurity and migrant workers not displayed here due to imprecision. Domain descriptions can be found in table 1.
Sensitivity analyses with alternative assumptions about missing or time-varying occupation data did not alter conclusions. Adjustment for vaccination status also did not alter conclusions (supplementary figure S1).
Discussion
The present study evaluated the performance of a COVID-19 JEM by examining the relationships between its domains comprising occupational factors thought to be related to the risk of SARS-CoV-2 infection in two independent UK cohorts. Over the entire study period, a higher JEM score was associated with a higher risk of SARS-CoV-2 infection for the four domains of transmission risk (number of contacts, nature of contacts, contaminated work spaces, location) and the two domains of mitigation measures (social distancing, use of face covering) across both cohorts. We cannot interpret these associations as causal; the four domains relating to transmission risk are also highly correlated with each other so we cannot know from this data which of these exposures, if any, is driving the observed differences in infection. After stratification by time, this trend was evident only during the first period across both cohorts.
Three domains (number, nature, and distancing) showed an exposure–response relationship between the risk level of the JEM and the risk of SARS-CoV-2 infection in the overall analysis. The absence of a clear relationships for the other domains could, at least partly, reflect the low number of participants working (mostly) outside (low risk), never using face covering (high risk) or having contact with the public (elevated risk), which can also explain the very broad confidence intervals estimated for those categories.
When stratified by time, the same associations were not observed in period 2 or 3 in either cohort, which could be due to several reasons. Firstly the JEM was not updated to reflect different mitigation strategies in each time period; there is likely to be misclassification of exposure in those periods, especially with regards to the “home working / lone working” (no risk) category where large changes took place for a number of occupations following the implementation of a “return to work” policy in June 2021. Considering this group is the reference category this would likely result in bringing relationships towards the null. This was observed, particularly within the CIS, where the increasing trends between the low, medium and high-risk categories remain for some dimensions, but not relative to the reference category (Figure 2). The JEM was developed on the knowledge from the first wave, when the theory of contaminated work surfaces was very prominent, however, with later evidence it has become clear that airborne transmission and ventilation were far more important (25), which we suggest should be reflected in updates of the JEM.
Secondly, a substantial part of the population had been vaccinated with at least one dose during the second and third time period. Nafilyan et al (26) found differences between occupation in vaccine coverage with rates ranging from 84.7% amongst health professionals to 57.6% in elementary trades and related occupations (26). Higher rates of vaccination amongst the workers with the highest expected rates of exposure may have attenuated differences between occupational groups to some extent although our sensitivity analysis suggests that any mediation effect is small.
Thirdly, changes in societal / social behaviors may mean that contribution from occupational exposures on risk of infection is reduced when compared to exposures outside the workplace. The Omicron wave was more likely to lead to infections within the household (27). In addition, the fact that fewer people went to their workplaces during time period 1 meant people were less likely to attend social activities outside of work (28), therefore relative contribution of occupation to the risk of contracting COVID-19 was greater, which made the JEM perform better during this time period. Further developments of the COVID-19 JEM should include different periods reflecting different levels of ‘working from home’.
The reduced risk of infection in time periods 2 and 3 observed for the high-risk group for the domain relating to the likelihood of contact with COVID-19 could be explained by the fact that this group mainly consists of health- and social care workers. Previous surveys on the UK health sector suggested logistical issues with PPE in the UK health sector including a lack of means, inadequate training and inconsistent guidance during the first period of the pandemic (29). In addition, analysis amongst these occupational groups have shown lower risks in later stages of the pandemic, possibly related to better access to PPE, being a priority group for vaccination, or previous infection (12–14). Another exception is the domain relating to use of face coverings, where the low risk group appears to have a reduced risk of infection in time periods 2 and 3 when compared to the ‘no risk/work from home’ group; perhaps due to an increased risk in the homeworker group as restrictions changed.
In The Netherlands, the eight dimensions of the Dutch version of this JEM were validated against self-reported data relating to the transmission risks and mitigation measures as well as COVID-19 infections within the past 12 months from The Netherlands Working Conditions Survey COVID-19 (NWCS-COVID-19) cohort study (16). Results showed good comparability between risk scores derived from the self-reported measures and the risks derived from the JEM. Self-reported infection data were collected during March 2021 and thereby the 12-month period that those cover is roughly comparable to our data covered by time period 1. The results of the Dutch study were very similar to the results of our study for the same period with higher JEM scores for the first six dimensions associated with a higher risk of having had COVID-19 compared with the reference score of “no risk”. In concordance with our findings, they also observed less strong associations for the dimensions “work location” and “face covering” and no evidence of association with the precarious work dimensions. Previous studies have suggested that migrant workers are at increased risk of SARS-CoV-2 infection at work due to their status as essential worker with often inequitable working and living conditions (30–32). Our results were imprecise due to small numbers in the higher risk categories so we cannot make conclusions. We did not find an association between a precarious occupation and SARS-CoV-2, but again there was a lot of uncertainty; earlier findings (5) suggested links between insecure employment and increased risk of COVID-19. The strict definition employed for precarious employment in the JEM was based on the proportion of workers with zero hours contracts. Precarity in employment is a complex issue characterized by employment insecurity, income inadequacy, and the lack of rights and protection and perhaps the JEM definition should be revised to capture precarity more broadly (33).
Several other studies assessed the association between various transmission and mitigation factors at work and the risk of COVID-19 (9, 34–37). Voko et al (37) evaluated the effect of social distancing on COVID-19 prevention in 28 European countries using incidence data from the European Centre for Disease Prevention and Control and index of social distancing developed from Google COVID-19 Community Mobility Reports. An increased social distance index was associated with fewer cases of infection on a daily basis (15). In regression analysis of data from the O*NET database, exposure to disease/infection in the workplace and a requirement of close physical proximity to other people during work singlehandedly explained >47% of disease prevalence variance (11). Another study examined the effect of ventilation, frequency of workplace contact and of the indoor/outdoor working environment contrast against serological SARS-CoV-2 status data from 3761 UK adult workers (12). Seropositivity was higher among workers with daily close contact, compared to those with intermediate-frequency contact and/or no work-related close contact. The risk of positive infection status was also generally elevated among workers in indoor trades, health care and in poor ventilated workplaces. The importance of ventilation by natural airflows was found in a study involving an outpatient building in Shenzen, China (14). Although surface contamination is not the main pathway for exposure to SARS-CoV-2, it may still be important and is most prevalent in frequently used, uncleaned, surfaces (35, 38, 39). Regarding the JEM, the observed association between surface contamination and infection may also be a result of correlation with other domains.
These findings further support the applicability and relevance of a COVID-19 JEM for the assessment of infection/disease risk when individual data are unavailable, insufficient, or unfeasible to obtain. Several domains are highly correlated and some appear more relevant than others; focus on social distancing and indoor/outdoor working may capture the majority of variation while minimizing collinearity.
Strengths of this study include the use of infection data from two independent cohorts, with a large number of participants including multiple time periods with different rates of infection as well as different restrictions and public health measures. One cohort (CIS) used repeated testing for all participants, hence frequency of testing was not related to occupation; in the other cohort (Virus Watch) testing on a subsample was used to check the reliability of the results relating to self-reported tests.
A JEM has limitations; differences exist within job codes that can dilute the results. We were unable to discriminate between infections acquired at work and those acquired outside work. The level of non-occupational exposure to SARS-CoV-2 was not included in analyses and will have changed substantially over time. In addition, it is possible that participants changed job (code) or lost their job during the study period, although for the stratified analyses by time period, occupation at the start of the time period was used for CIS data. Occupational data were only available at registration for Virus Watch, though misclassification is likely to be minimal due to the relatively short study period. Finally, it is possible that infections between visits or prior to starting the study were missed. Missing data could be related to occupation, for example shift workers being unavailable at the time of the CIS study visits or too busy to respond to the Virus Watch questionnaire.
Overall, findings suggest that the COVID-19 JEM is a useful tool to assess occupational exposure to SARS-CoV-2 during the first time period, especially when more precise and/or individual level data are lacking. In order to extend this to later time periods, the addition of a dimension on vaccination and a job specific variable to indicate the likelihood of attending work during a certain time period should be considered. These adjustments could improve performance, resulting in a more accurate research instrument.
Concluding remarks
We evaluated whether domains of a COVID-19 JEM were associated with the risk of SARS-CoV-2 infection. We observed clear exposure–response relationships in the early phase of the COVID-19 pandemic between the scores of the JEM relating to the number of contacts, the nature of contacts and social distancing, and the risk of SARS-CoV-2 infection. These relationships were accordant across the two cohorts involved and consistent with earlier results from a validation exercise of the JEM using Dutch data (35). However, these observed relationships were not persistent over time. At the latter phases of the pandemic there was little evidence of a relationship between the domains of the JEM and SARS-CoV-2. Explanations could include (i) a reduced role of workplace for infection risk as society opened, (ii) changes in risk factors and effectiveness of control measures due to different variants and vaccinations introduction, and (iii) an increased potential for JEM misclassification amid changes in policy measures and restrictions. These findings suggest that the COVID-19-JEM is a useful tool for assessing risk of exposure to SARS-CoV-2 in the workplace during the period up to the end of the second wave of the pandemic. Modifications of the JEM may improve the performance of the JEM in the latter periods of the pandemic.
Declaration
This work was produced using statistical data from ONS. The use of the ONS statistical data in this work does not imply the endorsement of the ONS in relation to the interpretation or analysis of the statistical data. This work uses research datasets that may not exactly reproduce National Statistics aggregates.
Ethics
CIS received ethical approval from the South Central Berkshire B Research Ethics Committee (20/SC/0195). All participants provided informed consent. For use of this data for this project statistics authority self-assessment classified the study as low risk. The ONS Research Accreditation Panel approved this assessment.
The Hampstead NHS Health Research Authority Ethics Committee approved the Virus Watch study (20/HRA/2320), which and conformed to the ethical standards set out in the Declaration of Helsinki. All participants provided informed consent for all aspects of the study.
Data availability
ONS CIS data can be accessed only by ONS-accredited researchers, who can apply for accreditation through the Research Accreditation Service. Access is through the Secure Research Service (SRS) and approved on a project basis. For further details see www.ons.gov.uk/aboutus/whatwedo/statistics/requestingstatistics/approvedresearcherscheme.
Virus Watch aim to share aggregate data from this project on our website and via a “Findings so far” section on the website ucl-virus-watch.net. We also share some individual record level data on the ONS Secure Research Service. In sharing the data, we will work within the principles set out in the UKRI Guidance on best practice in the management of research data. Access to use of the data whilst research is being conducted will be managed by the Chief Investigators (ACH and RWA) in accordance with the principles set out in the UKRI guidance on best practice in the management of research data. We will put analysis code on publicly available repositories to enable their reuse.
Funding
This work was supported by funding from the PROTECT COVID-19 National Core Study on transmission and environment, managed by the Health and Safety Executive on behalf of HM Government. The Virus Watch study is supported by the MRC Grant Ref: MC_PC 19070 awarded to UCL on 30 March 2020 and MRC Grant Ref: MR/V028375/1 awarded on 17 August 2020. The study also received $15 000 of Facebook advertising credit to support a pilot social media recruitment campaign on 18 August 2020. The Wellcome Trust supported the study through a Wellcome Clinical Research Career Development Fellowship to RA [206602]. The funders had no role in study design, data collection, analysis and interpretation, in the writing of this report, or in the decision to submit the paper for publication.
Conflict of interests
SR, JW, KvV, IB, WM, NP, AH and MvT report funding from the UK Health and Safety Executive paid to their institution. SB reports funding to her institution from the Medical Research Council MR/N013867/1. AB, SP, ZS, VS, HK, AP declare no conflict of interests.
Supplementary material
References
- 1.Taylor L. COVID-19:true global death toll from pandemic is almost 15 million, says WHO. BMJ. 2022 May;377:o1144. doi: 10.1136/bmj.o1144. [DOI] [PubMed] [Google Scholar]
- 2.Mutambudzi M, Niedwiedz C, Macdonald EB, Leyland A, Mair F, Anderson J, et al. Occupation and risk of severe COVID-19:prospective cohort study of 120 075 UK Biobank participants. Occup Environ Med. 2020 Dec;78(5):307–14. doi: 10.1136/oemed-2020-106731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nafilyan V, Pawelek P, Ayoubkhani D, Rhodes S, Pembrey L, Matz M, et al. Occupation and COVID-19 mortality in England:a national linked data study of 14.3 million adults. Occup Environ Med. 2022 Jul;79(7):433–41. doi: 10.1136/oemed-2021-107818. [DOI] [PubMed] [Google Scholar]
- 4.Oude Hengel KM, Burdorf A, Pronk A, Schlünssen V, Stokholm ZA, Kolstad HA, et al. Exposure to a SARS-CoV-2 infection at work:development of an international job exposure matrix (COVID-19-JEM) Scand J Work Environ Health. 2022 Jan;48(1):61–70. doi: 10.5271/sjweh.3998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burdorf A, Porru F, Rugulies R. The COVID-19 pandemic:one year later - an occupational perspective. Scand J Work Environ Health. 2021 May;47(4):245–7. doi: 10.5271/sjweh.3956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nelson KN, Siegler AJ, Sullivan PS, Bradley H, Hall E, Luisi N, et al. Nationally Representative Social Contact Patterns among U. S. adults, August 2020-April 2021. medRxiv. 2022 Mar 30;:2021. doi: 10.1101/2021.09.22.21263904. 09.22.21263904. Preprint. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beale S, Hoskins S, Byrne T, Fong WLE, Fragaszy E, Geismar C, et al. Workplace contact patterns in England during the COVID-19 pandemic:Analysis of the Virus Watch prospective cohort study. Lancet Reg Health Eur. 2022 May;16:100352. doi: 10.1016/j.lanepe.2022.100352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baker MG, Peckham TK, Seixas NS. Estimating the burden of United States workers exposed to infection or disease:A key factor in containing risk of COVID-19 infection. PLoS One. 2020 Apr;15(4):e0232452. doi: 10.1371/journal.pone.0232452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beale S, Patel P, Rodger A, Braithwaite I, Byrne T, Fong WL, et al. Virus Watch Collaborative. Occupation, work-related contact and SARS-CoV-2 anti-nucleocapsid serological status:findings from the Virus Watch prospective cohort study. Occup Environ Med. 2022 Apr;79(11):729–35. doi: 10.1136/oemed-2021-107920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen YH, Glymour M, Riley A, Balmes J, Duchowny K, Harrison R, et al. Excess mortality associated with the COVID-19 pandemic among Californians 18-65 years of age, by occupational sector and occupation:march through November 2020. PLoS One. 2021 Jun;16(6):e0252454. doi: 10.1371/journal.pone.0252454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Billingsley S, Brandén M, Aradhya S, Drefahl S, Andersson G, Mussino E. COVID-19 mortality across occupations and secondary risks for elderly individuals in the household:A population register-based study. Scand J Work Environ Health. 2022 Jan;48(1):52–60. doi: 10.5271/sjweh.3992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beale S, Hoskins S, Byrne T, Erica Fong WL, Fragaszy E, Geismar C, et al. Differential Risk of SARS-CoV-2 Infection by Occupation:Evidence from the Virus Watch prospective cohort study in England and Wales. medRxiv. 2022 doi: 10.1186/s12995-023-00371-9. 2021.12.14.21267460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rhodes S, Wilkinson J, Pearce N, Mueller W, Cherrie M, Stocking K, et al. Occupational differences in SARS-CoV-2 infection:analysis of the UK ONS COVID-19 infection survey. J Epidemiol Community Health. 2022 Jul;76(10):841–6. doi: 10.1136/jech-2022-219101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bonde JP, Sell L, Johan Høy JH, Begtrup LM, Flachs EM, Jakobsson K, et al. Occupational risk of COVID-19 across pandemic waves:a two-year national follow-up study of hospital admissions. Scand J Work Environ Health. 2022 Nov;48(8):672–7. doi: 10.5271/sjweh.4056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cherrie M, Rhodes S, Wilkinson J, Mueller W, Nafilyan V, Van Tongeren M, et al. Longitudinal changes in proportionate mortality due to COVID-19 by occupation in England and Wales. Scand J Work Environ Health. 2022 Nov;48(8):611–20. doi: 10.5271/sjweh.4048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van der Feltz S, Peters S, Pronk A, Schlünssen V, Stokholm ZA, Kolstad HA, et al. Validation of a COVID-19 Job Exposure Matrix (COVID-19-JEM) for Occupational Risk of a SARS-CoV-2 Infection at Work:Using Data of Dutch Workers. Ann Work Expo Health. 2022 doi: 10.1093/annweh/wxac032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Office IL. International Standard Classification of Occupations Geneva2008. Available from: https://www.ilo.org/public/english/bureau/stat/isco/docs/publication08.pdf .
- 18.ONS. SOC2010 volume 2: the structure and coding index 2010. Available from: https://www.ons.gov.uk/methodology/classificationsandstandards/standardoccupationalclassificationsoc/soc2010/soc2010volume2thestructureandcodingindex .
- 19.Statistics OoN. Classifying the Standard Occupational Classification 2020 (SOC 2020) to the International Standard Classification of Occupations (ISCO-08). UK2020 [Google Scholar]
- 20.ONS. Annual population survey (APS) QMI. 2012. Available from: https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/employmentandemployeetypes/methodologies/annualpopulationsurveyapsqmi .
- 21.ONS. Labour Force Survey (LFS) QMI. 2015. Available from: https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/employmentandemployeetypes/methodologies/labourforcesurveylfsqmi .
- 22.StataCorp. Stata Statistical Software:Release 17. College Station, TX: StataCorp LLC; 2021. [Google Scholar]
- 23.Government U. National statistics English indices of deprivation 2019. Available from: https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019 .
- 24.NHS. Who is at high risk from coronavirus (COVID-19) 2022. Available from: https://www.nhs.uk/conditions/coronavirus-COVID-19/people-at-higher-risk/who-is-at-high-risk-from-coronavirus/
- 25.Greenhalgh T, Jimenez JL, Prather KA, Tufekci Z, Fisman D, Schooley R. Ten scientific reasons in support of airborne transmission of SARS-CoV-2. Lancet. 2021 May;397(10285):1603–5. doi: 10.1016/S0140-6736(21)00869-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nafilyan V, Dolby T, Finning K, Pawelek P, Edge R, Morgan J, et al. Differences in COVID-19 vaccination coverage by occupation in England:a national linked data study. Occup Environ Med. 2022;79(11):758. doi: 10.1136/oemed-2021-108140. [DOI] [PubMed] [Google Scholar]
- 27.Jalali N, Brustad HK, Frigessi A, MacDonald E, Meijerink H, Feruglio S, et al. Increased household transmission and immune escape of the SARS-CoV-2 Omicron variant compared to the Delta variant:evidence from Norwegian contact tracing and vaccination data. medRxiv. 2022 doi: 10.1038/s41467-022-33233-9. 2022.02.07.22270437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.J P. Homeworking and spending during the coronavirus (COVID-19) pandemic, Great Britain:April 2020 to January 2022. In:Statistics OoN. 2022 [Google Scholar]
- 29.Mantelakis A, Spiers HV, Lee CW, Chambers A, Joshi A. Availability of Personal Protective Equipment in NHS Hospitals During COVID-19:A National Survey. Ann Work Expo Health. 2021 Jan;65(1):136–40. doi: 10.1093/annweh/wxaa087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reid A, Rhonda-Perez E, Schenker MB. Migrant workers, essential work, and COVID-19. Am J Ind Med. 2021 Feb;64(2):73–7. doi: 10.1002/ajim.23209. [DOI] [PubMed] [Google Scholar]
- 31.Burton-Jeangros C, Duvoisin A, Lachat S, Consoli L, Fakhoury J, Jackson Y. The Impact of the COVID-19 Pandemic and the Lockdown on the Health and Living Conditions of Undocumented Migrants and Migrants Undergoing Legal Status Regularization. Front Public Health 2020 Dec. 8:596887. doi: 10.3389/fpubh.2020.596887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liem A, Wang C, Wariyanti Y, Latkin CA, Hall BJ. The neglected health of international migrant workers in the COVID-19 epidemic. Lancet Psychiatry. 2020 Apr;7(4):e20. doi: 10.1016/S2215-0366(20)30076-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kreshpaj B, Orellana C, Burström B, Davis L, Hemmingsson T, Johansson G, et al. What is precarious employment?A systematic review of definitions and operationalizations from quantitative and qualitative studies. Scand J Work Environ Health. 2020 May 1;46(3):235–47. doi: 10.5271/sjweh.3875. [DOI] [PubMed] [Google Scholar]
- 34.Zhang M. Estimation of differential occupational risk of COVID-19 by comparing risk factors with case data by occupational group. Am J Ind Med. 2021 Jan;64(1):39–47. doi: 10.1002/ajim.23199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020 Mar;104(3):246–51. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li C, Tang H. Study on ventilation rates and assessment of infection risks of COVID-19 in an outpatient building. J Build Eng. 2021;42:103090. doi: 10.1016/j.jobe.2021.103090. [DOI] [Google Scholar]
- 37.Vokó Z, Pitter JG. The effect of social distance measures on COVID-19 epidemics in Europe:an interrupted time series analysis. Geroscience. 2020 Aug;42(4):1075–82. doi: 10.1007/s11357-020-00205-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hennessy NT, Toomey S, Gautier V, O'Reilly S, de Barra E, Hanrahan EO, et al. COVID-19 contamination of high-touch surfaces in the public domain. Ir J Med Sci. 2022 Dec;191(6):2839–40. doi: 10.1007/s11845-021-02881-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Silva PG, Gonçalves J, Lopes AI, Esteves NA, Bamba GE, Nascimento MS, et al. Evidence of Air and Surface Contamination with SARS-CoV-2 in a Major Hospital in Portugal. Int J Environ Res Public Health. 2022 Jan;19(1):525. doi: 10.3390/ijerph19010525. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
ONS CIS data can be accessed only by ONS-accredited researchers, who can apply for accreditation through the Research Accreditation Service. Access is through the Secure Research Service (SRS) and approved on a project basis. For further details see www.ons.gov.uk/aboutus/whatwedo/statistics/requestingstatistics/approvedresearcherscheme.
Virus Watch aim to share aggregate data from this project on our website and via a “Findings so far” section on the website ucl-virus-watch.net. We also share some individual record level data on the ONS Secure Research Service. In sharing the data, we will work within the principles set out in the UKRI Guidance on best practice in the management of research data. Access to use of the data whilst research is being conducted will be managed by the Chief Investigators (ACH and RWA) in accordance with the principles set out in the UKRI guidance on best practice in the management of research data. We will put analysis code on publicly available repositories to enable their reuse.