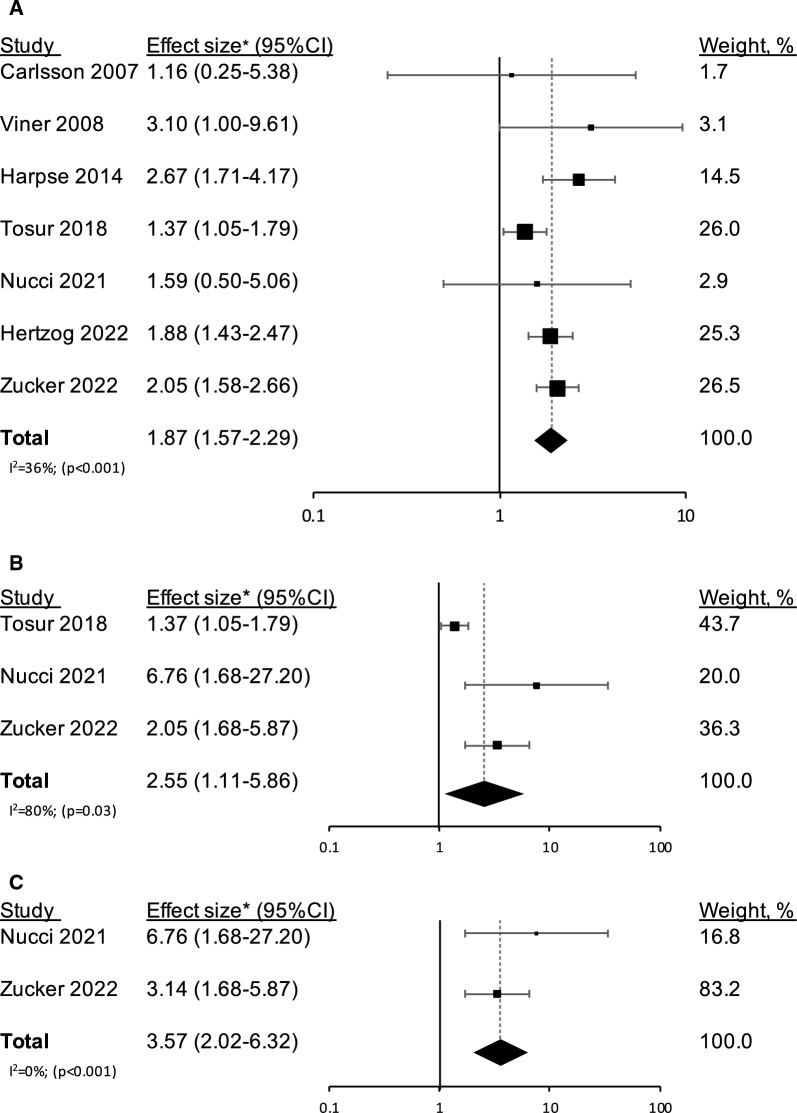
Fig. 2.
Confounder-adjusted effect sizes (95% CI) for incident type 1 diabetes among individuals with obesity or overweight/obesity compared to those without, are shown for individual studies and for pooled risk ratio results from the meta-analysis. The effect sizes are shown across all the studies (a) and across the studies that were limited to autoantibody-proven type 1 diabetes (b). Panel c shows the confounder-adjusted effect size (95% CI) for incident type 1 diabetes, limited to autoantibody-proven type 1 diabetes, in individuals with obesity. The sizes of the boxes correspond to the weights of the study in the meta-analysis. The diamond depicts the point estimate (95% CI). The vertical line is centered at the null. Overweight and obesity were defined as follows: Carlsson et al. and Harpsøe et al. [25, 24] —BMI ≥ 25 kg/m2 and BMI ≥ 30 kg/m2, Viner et al. and Nucci et al.[19, 21], —according to the International Obesity Task Force cut-off points by sex and age (corresponding BMI ≥ 25 kg/m2 and BMI ≥ 30 kg/m2 in adults), Zucker et al. [15], —85th ≤ BMI ≤ 94th percentiles and BMI ≥ 95th percentile. Tosur et al. [20] and Herzog et al. [23] merged overweight and obesity into a single category that was defined as BMI ≥ 25 kg/m2. Of note, Carlsson et al. [25] considered either anti-GAD presence or C-peptide levels < 150 pmol/L as confirmation of type 1 diabetes. Yet, as this was done in only 76% of self-reported type 1 diabetes cases, the study was excluded from the subgroup analysis in panels b and c. *All the studies reported hazard ratios, except Carlsson et al. [25] who reported risk ratios.