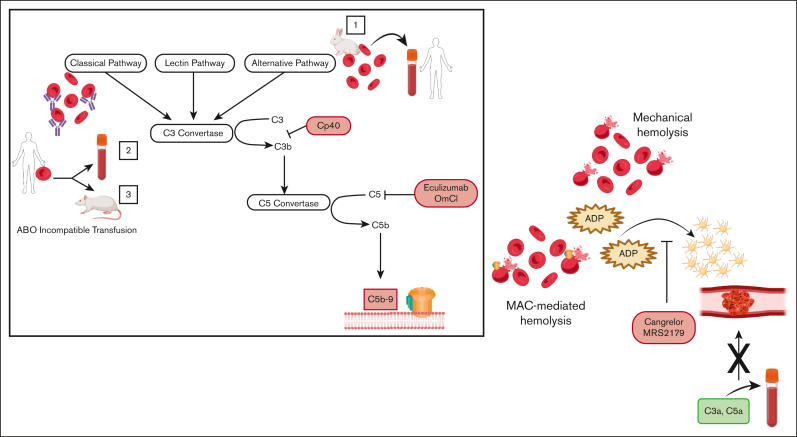
Hemolysis caused by either MAC formation or mechanical shearing of erythrocytes leads to prothrombotic platelet activation, through the release of ADP, which is blocked by the ADP-receptor antagonists, Cangrelor and MRS2179. Addition of isolated complement anaphylatoxins (C3a, C5a) to blood does not lead to platelet activation in the absence of hemolysis. Box: activation of (1) the alternative pathway of complement on rabbit erythrocytes or (2,3) the classical pathway on human erythrocytes through ABO incompatible transfusion was used to induce MAC-mediated lysis. ABO incompatible transfusion was stimulated (2) ex vivo by addition of human type AB erythrocytes into type O blood and (3) in vivo through transfusion of human type AB erythrocytes into rats possessing antihuman AB antibodies. Proximal (CP40) and terminal (eculizumab, OmCl) complement inhibitors block MAC-mediated hemolysis and downstream platelet activation.

An official website of the United States government
Here's how you know
Official websites use .gov
A
.gov website belongs to an official
government organization in the United States.
Secure .gov websites use HTTPS
A lock (
) or https:// means you've safely
connected to the .gov website. Share sensitive
information only on official, secure websites.