Abstract
Background
While venoarterial extracorporeal membrane oxygenation (V-A ECMO) provides lifesaving support for cardiopulmonary failure, complications may increase mortality, with few studies focusing on ischemic/hemorrhagic stroke. We aimed to determine the trends and associations of stroke incidence and mortality, and their risk factors, including the effects of annual case volumes of ECMO centers.
Methods
Retrospective analysis was performed on the Extracorporeal Life Support Organization (ELSO) registry, including adult V-A ECMO patients from 534 international centers between 2012 and 2021, excluding extracorporeal cardiopulmonary resuscitation. Temporal trend analyses were performed for stroke incidence and mortality. Univariate testing, multivariable regression, and survival analysis were used to evaluate the associations of stroke, 90-day mortality, and impact of annual center volume.
Results
Of 33,041 patients, 20,297 had mortality data, and 12,327 were included in the logistic regression. Between 2012 and 2021, ischemic stroke incidence increased (p < 0.0001), hemorrhagic stroke incidence remained stable, and overall 90-day mortality declined (p < 0.0001). Higher 24-h PaO2 and greater decrease between pre-ECMO PaCO2 and post-cannulation 24-h PaCO2 were associated with greater ischemic stroke incidence, while annual case volume was not. Ischemic/hemorrhagic strokes were associated with increased 90-day mortality (both p < 0.0001), while higher annual case volume was associated with lower 90-day mortality (p = 0.001). Hazard of death was highest in the first several days of V-A ECMO.
Conclusion
In V-A ECMO patients between 2012 and 2021, 90-day mortality decreased, while ischemic stroke incidence increased. ELSO centers with higher annual case volumes had lower mortality, but were not associated with ischemic/hemorrhagic stroke incidence. Both ischemic/hemorrhagic strokes were associated with increased mortality.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13054-023-04707-z.
Keywords: Venoarterial ECMO, Stroke, Mortality, Trend
Background
Venoarterial (V-A) extracorporeal membrane oxygenation (ECMO) is a form of temporary life support for patients with refractory cardio-circulatory or cardiopulmonary failure. It operates by extracting de-oxygenated blood from the patients’ venous system, and reinfusing oxygenated blood into the patients’ arterial system with adequate pressure. However, V-A ECMO support is not without risk, as an increasing number of studies throughout the years have reported on various neurological complications, which in turn are associated with higher mortality [1, 2]. Very few studies focusing specifically on the incidence of ischemic and/or hemorrhagic stroke as a complication of V-A ECMO, excluding extracorporeal cardiopulmonary resuscitation (ECPR) [3, 4]. Additionally, prior ECMO studies in the pediatric population revealed that ECMO centers with lower case volumes had higher mortality, though such studies in the adult ECMO patient population are more limited [5, 6]. Therefore, a robust, large-scale epidemiological study is needed to explore the incidence and outcomes related to ischemic and hemorrhagic stroke in adult patients supported with V-A ECMO.
We sought to characterize the trends regarding ischemic and hemorrhagic strokes across time and ECMO center volume, as well as the effects of stroke on mortality adjusting for known risk factors, with the aim to (1) determine the incidence and trend of ischemic strokes, hemorrhagic strokes, and mortality over the past 10 years; (2) determine the association between the case volume per year of ECMO centers and incidence of ischemic stroke, hemorrhagic stroke, or mortality; and 3) determine the association between mortality and ischemic or hemorrhage stroke.
Methods
Study design and population
The Extracorporeal Life Support Organization (ELSO) registry is an international voluntary database that collects information on usage, indications, complications, and outcomes of ECMO support in adults and children from 534 centers worldwide currently. The registry collects data related to patient demographics, clinical characteristics, pre-ECMO conditions, hemodynamic and laboratory values before and during ECMO support, complications that occur during ECMO support, and outcomes such as survival at the time of hospital discharge. Diagnosis and medical history are reported according to the International Classification of Diseases, 9th Revision (ICD-9) and 10th Revision (ICD-10) codes.
This study was a retrospective analysis of the ELSO registry database from 2012 to 2021. Inclusion criteria consisted of adult patients (≥ 18 years) who underwent V-A ECMO support for either cardiac or respiratory failure, and whose ischemic/hemorrhagic stroke data were available. Exclusion criteria consisted of patients whose ECMO was later converted to different modes. The period of 2012–2021 was chosen to assess the current, modern practices of ECMO support over the past decade. Pediatric patients were excluded, as their pathophysiology of conditions requiring ECMO often differs considerably from those in adults. ECPR and venovenous ECMO were also excluded as their risk factors and mechanisms of acute brain injury differ from those of V-A ECMO. This study was approved by the local institutional review board.
Data collection and definitions
For all included patients, the following data were collected from the ELSO registry: patient demographics, ECMO characteristics, pre- and post-ECMO cannulation laboratory values and hemodynamics, on-ECMO complications and their reported timings, including ischemic stroke, hemorrhagic stroke, and status at hospital discharge. For the variable of ischemic stroke, the ELSO registry terms “CNS diffuse ischemia,” defined as computed tomography (CT) or magnetic resonance imaging (MRI) demonstrating diffuse ischemic changes, and “CNS infarction,” defined as CT or ultrasound or MRI demonstrating localized ischemic change, were combined. For the variable of hemorrhagic stroke, three ELSO registry terms were combined: “CNS hemorrhage,” which was discontinued in 2018, as well as “intra/extra parenchymal CNS hemorrhage” and “intraventricular CNS hemorrhage,” which were newly introduced in 2018.
Outcomes
Primary outcome was defined as 90-day mortality, while secondary outcome was defined as 30-day mortality.
Statistical analysis
Continuous variables were reported as medians with interquartile range (IQR). Categorical variables were reported as frequencies with percentages. For the patients’ ages, the ELSO registry records the data as a continuous variable with the exception of the age group “80 or older.” In this setting, the ages of patients “80 or older” were changed to 80, so that age could still be analyzed as a continuous variable. To assess the differences in the demographic information and ECMO-related variables between patients with and without strokes, t test was used to compare the means of continuous variables, while χ2 test was used to compare proportions with each subgroup sample size greater or equal to 5, or Fisher’s exact test in cases of subgroup sample size less than 5.
The Cochrane-Armitage test and Poisson regression were used to evaluate the trends over time (Aim 1). Logistic regression models were created to identify risk factors associated with on-ECMO complications of ischemic and hemorrhagic strokes, with independent variables including ELSO center volume per year (Aim 2). Kaplan–Meier curves and hazard function curves were generated, and log-rank tests were performed to evaluate the risk factors associated with 90-day and 30-day mortality (Aim 3). Cox-regression analysis was also considered initially, however, ultimately unable to be performed, as the test for the proportional hazard assumption based on the Schoenfeld residuals revealed that this requirement was not met. Instead, multivariable logistic regression models were generated with the dependent variables of 90-day (primary outcome) or 30-day mortality (secondary outcome).
Independent covariates chosen a priori consisted of patient demographics including age and sex; center case volume per year; central cannulation site; pre-ECMO blood gas values of arterial oxygen pressure (PaO2), arterial carbon dioxide pressure (PaCO2), and pH; post-cannulation 24-h blood gas values of PaO2 and PaCO2; post-cannulation 24-h blood pump flow rate; ECMO duration; and on-ECMO complications, including ischemic and/or hemorrhagic stroke, brain death, gastrointestinal hemorrhage, cardiac arrhythmia, pump failure, moderate-to-severe hemolysis (peak plasma hemoglobin > 50 mg/dL or at least one occurrence of > 500 mg/L during ECMO, sustained for ≥ 2 days), the requirement of neurosurgical intervention, renal replacement therapy, and/or cardiopulmonary bypass. These specific variables were chosen based on their medical relevance and the clinically hypothesized significance of their associations with mortality. Additionally, the ELSO definitions of blood gas-related variables were updated in 2017 and 2018, such that pre-ECMO PaO2 and PaCO2 were changed from “worst” values to “closest to” ECMO start time, while 24-h PaO2, 24-h PaCO2, and 24-h blood pump flow rate were changed from “best” values to “closest to 24-h” of ECMO. As a result, ΔPaCO2 was calculated only for patients who underwent ECMO in 2018 or later. Similarly, in 2018, the on-ECMO complication of brain death was more clearly defined, and the variable of neurosurgical interventions was added to the ELSO registry. As a result, the logistic regression models, which included PaO2, PaCO2, brain death, and neurosurgical interventions as independent variables, were generated only with patient data reported from 2018 or later. Bonferroni correction was used to account for the 58 univariate statistical tests performed, resulting in the change of threshold significance from p < 0.05 to p < 0.00086 for the univariate tests. Finally, the Pearson correlation coefficient was calculated to evaluate the association between 24-h PaO2 and 24-h blood pump flow rate. None of these variables had missing that exceeded 40%. All statistical analyses were performed using R Studio (Version 2023.06.2, www.r-project.org).
Results
Overall, 34,734 V-A ECMO patients were queried from the 2012 to 2021 ELSO database. Of those, 1693 patients were later converted to different modes of ECMO, and thus excluded from analysis, resulting in 33,041 patients. 20,297 had complete mortality data, of which 12,327 were from 2018 to 2021 (Additional file 1). Table 1 summarizes the variables related to patient demographics, ECMO, and mortality. Among the patients with complete mortality data, 96% (n = 19,389) had neither ischemic nor hemorrhagic stroke, 3% (n = 659) developed ischemic strokes, 1% (n = 287) developed hemorrhagic strokes, and 0.2% (n = 38) developed both ischemic and hemorrhagic strokes during ECMO support. The median detection timing was 3.04 days for ischemic strokes and 3.79 days for hemorrhagic strokes since ECMO cannulation. The 90-day mortality was higher for patients with ischemic strokes than those without (65% vs 36%, respectively, p < 0.0001, χ2 test). Similarly, the 90-day mortality was higher for patients with hemorrhagic strokes than those without (72% vs 37%, respectively, p < 0.0001, χ2 test). Many ECMO-related variables were found to be significantly different between patients who developed ischemic or hemorrhagic stroke and those who did not (Table 1). Notably, patients who developed ischemic stroke also experienced other on-ECMO complications more often than those who did not develop ischemic stroke, including longer duration of ECMO support (p < 0.0001, t test), as well as more neurosurgical interventions (p < 0.0001, χ2 test), brain death (p < 0.0001, χ2 test), cardiac arrhythmias (p < 0.0001, χ2 test), gastrointestinal hemorrhage (p < 0.0001, χ2 test), moderate-to-severe hemolysis (p < 0.0001, χ2 test), and renal replacement therapy (p < 0.0001, χ2 test). This was similar to the cases of patients who developed hemorrhagic strokes compared to those who did not, including longer duration of ECMO support (p < 0.0001, t-test), as well as more neurosurgical interventions (p < 0.0001, χ2 test), brain death (p < 0.0001, χ2 test), cardiac arrhythmias (p = 0.0002, χ2 test), gastrointestinal hemorrhage (p < 0.0001, χ2 test), and renal replacement therapy (p = 0.0002, χ2 test).
Table 1.
Patient Demographics and ECMO Variables for ECMO-associated Ischemic or Hemorrhagic Stroke
| Variable | Ischemic stroke (n = 659) | No ischemic stroke (n = 19,638) | p value | Hemorrhagic stroke (n = 287) | No Hemorrhagic stroke (n = 20,010) | p value |
|---|---|---|---|---|---|---|
| Age (years) | 58.1 (46.4–65.4) | 57.5 (45.3–66.2) | 0.61 | 57.9 (46.1–65.6) | 57.5 (45.3–66.2) | 0.82 |
| Female | 234 (36%)f | 6,310 (32%)g | 0.09 | 114 (40%)h | 6430 (32%)i | 0.01 |
| Center volume per year | 19 (8–32) | 18 (9–31) | 0.50 | 20 (9–32) | 18 (9–31) | 0.50 |
| Aortic cannulation | 129 (20%) | 3696 (19%) | 0.66 | 49 (17%) | 3776 (19%) | 0.49 |
| Year of ECMO | ||||||
| 2012 | 20 (3%) | 581 (3%) | 0.35 | 10 (3%) | 591 (3%) | 0.17 |
| 2013 | 25 (4%) | 718 (4%) | 16 (6%) | 727 (4%) | ||
| 2014 | 27 (4%) | 1001 (5%) | 12 (4%) | 1016 (5%) | ||
| 2015 | 51 (8%) | 1352 (7%) | 15 (5%) | 1388 (7%) | ||
| 2016 | 55 (8%) | 1716 (9%) | 21 (7%) | 1750 (9%) | ||
| 2017 | 59 (9%) | 2365 (12%) | 24 (8%) | 2400 (12%) | ||
| 2018 | 100 (15%) | 2726 (14%) | 34 (12%) | 2792 (14%) | ||
| 2019 | 123 (19%) | 3249 (17%) | 55 (19%) | 3317 (17%) | ||
| 2020 | 96 (15%) | 2975 (15%) | 51 (18%) | 3020 (15%) | ||
| 2021 | 103 (16%) | 2955 (15%) | 49 (17%) | 3009 (15%) | ||
| Pre-ECMO ABG | ||||||
| pH (2012–2016)a | 7.25 (7.12–7.35)f | 7.30 (7.19–7.39)g | 0.002 | 7.25 (7.13–7.32)h | 7.30 (7.19–7.39)i | 0.004 |
| pH (2017–2021)b | 7.28 (7.17–7.37)f | 7.30 (7.21–7.39)g | 0.0002 | 7.29 (7.20–7.36)h | 7.30 (7.21–7.39)i | 0.04 |
| PaO2 (2012–2016)a | 95 (59–216)f | 96 (64–197)g | 0.35 | 97 (68–159)h | 96 (64–197)i | 0.32 |
| PaO2 (2017–2021)b | 100 (68–254)f | 116 (74–232)g | 0.63 | 107 (76–218)h | 116 (74–233)i | 0.25 |
| PaCO2 (2012–2016)a | 41 (31–53)f | 40 (32.5–49.1)g | 0.79 | 38 (30–45)h | 40 (32.4–49.5)i | 0.01 |
| PaCO2 (2017–2021)b | 41 (35–50.8)f | 40 (33.8–48.7)g | 0.04 | 39 (32–48)h | 40 (33.9–48.8)i | 0.60 |
| ABG at 24-h post-cannulation | ||||||
| pH (2012–2017)c | 7.42 (7.38–7.45)f | 7.42 (7.38–7.47)g | 0.50 | 7.41 (7.36–7.45)h | 7.42 (7.38–7.47)i | 0.18 |
| pH (2018–2021)d | 7.43 (7.37–7.47)f | 7.43 (7.38–7.47)g | 0.29 | 7.43 (7.39–7.48)h | 7.43 (7.38–7.47)i | 0.09 |
| PaO2 (2012–2017)c | 149 (92–254)f | 143 (94–238)g | 0.62 | 157 (91–299)h | 143 (94–238)i | 0.15 |
| PaO2 (2018–2021)d | 132 (88–270)f | 134 (91–222)g | 0.08 | 129 (86–207)h | 134 (91–224)i | 0.81 |
| PaCO2 (2012–2017)c | 38 (33–41.4)f | 38 (31–41)g | 0.03 | 38.5 (33–42.8)h | 38 (33–42)i | 0.96 |
| PaCO2 (2018–2021)d | 38 (33.8–42)f | 38 (33.8–42)g | 0.66 | 38 (34–43)h | 38 (33.8–42)i | 0.84 |
| Blood pump flow rate (2018–2021)d | 3.84 (3.28–4.47)f | 3.88 (3.20–4.41)g | 0.51 | 3.92 (3.20–4.45)h | 3.88 (3.20–4.41)i | 0.49 |
| Days on ECMO support | 6.17 (3.71–10.04) | 4.75 (2.71–7.67) | < 0.0001 | 6.33 (3.71–10.81) | 4.79 (2.71–7.71) | < 0.0001 |
| Timing of stroke (days) (2018–2021) | 3.04 (1.29–6.29)f | N/A | N/A | 3.79 (1.25–6.88) | N/A | N/A |
| Mortality | ||||||
| 90-Day mortality | 427 (65%) | 7123 (36%) | < 0.0001 | 206 (72%) | 7344 (37%) | < 0.0001 |
| 30-Day mortality | 411 (62%) | 6339 (32%) | < 0.0001 | 195 (68%) | 6555 (33%) | < 0.0001 |
| ECMO complications | ||||||
| Cardiac arrhythmia | 129 (20%) | 2112 (11%) | < 0.0001 | 52 (18%) | 2189 (11%) | 0.0002 |
| CPB | 166 (25%) | 4172 (21%) | 0.02 | 54 (19%) | 4284 (21%) | 0.32 |
| Brain death (2018–2021)e | 9 (2%) | 42 (0.4%) | < 0.0001 | 7 (4%) | 44 (0.4%) | < 0.0001 |
| Gastrointestinal hemorrhage | 48 (7%) | 601 (3%) | < 0.0001 | 27 (9%) | 622 (3%) | < 0.0001 |
| Hemolysis (Moderate-Severe) | 22 (3%) | 261 (1%) | < 0.0001 | 7 (2%) | 276 (1%) | 0.21 |
| Neurosurgical Intervention (2018–2021)e | 5 (1%) | 8 (0.07%) | < 0.0001 | 8 (4%) | 5 (0.04%) | < 0.0001 |
| Pump failure | 7 (1%) | 100 (0.5%) | 0.10 | 4 (1%) | 103 (0.5%) | 0.10 |
| Renal replacement therapy | 237 (36%) | 4509 (23%) | < 0.0001 | 94 (33%) | 4652 (23%) | 0.0002 |
All data are presented as n (%) for categorical variables, and median (interquartile range) for continuous variables
Bolded text: Statistically significant with p < 0.05
aWorst” values
bClosest” value to ECMO start time
cBest” values
dClosest” value to post-cannulation 24-h of ECMO
eUsed sample size of patients in years 2018–2021 as denominator
fMissing values for variables in the “Ischemic Stroke” group: Sex (n = 3), pre-ECMO pH (n = 175), pre-ECMO PaO2 (n = 188), pre-ECMO PaCO2 (n = 182), 24-h pH (n = 43), 24-h PaO2 (n = 53), 24-h PaCO2 (n = 52), 24-h blood pump flow rate (n = 36), timing of stroke (n = 9)
gMissing values for variables in the “No Ischemic Stroke” group: Sex (n = 176), pre-ECMO pH (n = 4995), pre-ECMO PaO2 (n = 5584), pre-ECMO PaCO2 (n = 5503), 24-h pH (n = 2644), 24-h PaO2 (n = 3247), 24-hr PaCO2 (n = 3207), 24-h blood pump flow rate (n = 1786)
hMissing values for variables in the “Hemorrhagic Stroke” group: pre-ECMO pH (n = 65), pre-ECMO PaO2 (n = 70), pre-ECMO PaCO2 (n = 68), 24-h-pH (n = 30), 24-h PaO2 (n = 34), 24-h PaCO2 (n = 35), 24-h blood pump flow rate (n = 23)
iMissing values for variables in the “No Hemorrhagic Stroke” group: Sex (n = 179), pre-ECMO pH (n = 5105), pre-ECMO PaO2 (n = 5702), pre-ECMO PaCO2 (n = 5617), 24-h pH (n = 2657), 24-h PaO2 (n = 3266), 24-h PaCO2 (n = 3224), 24-h blood pump flow rate (n = 1999); ABG: arterial blood gas; CPB: cardiopulmonary bypass; ECMO: extracorporeal membrane oxygenation; N/A: not applicable
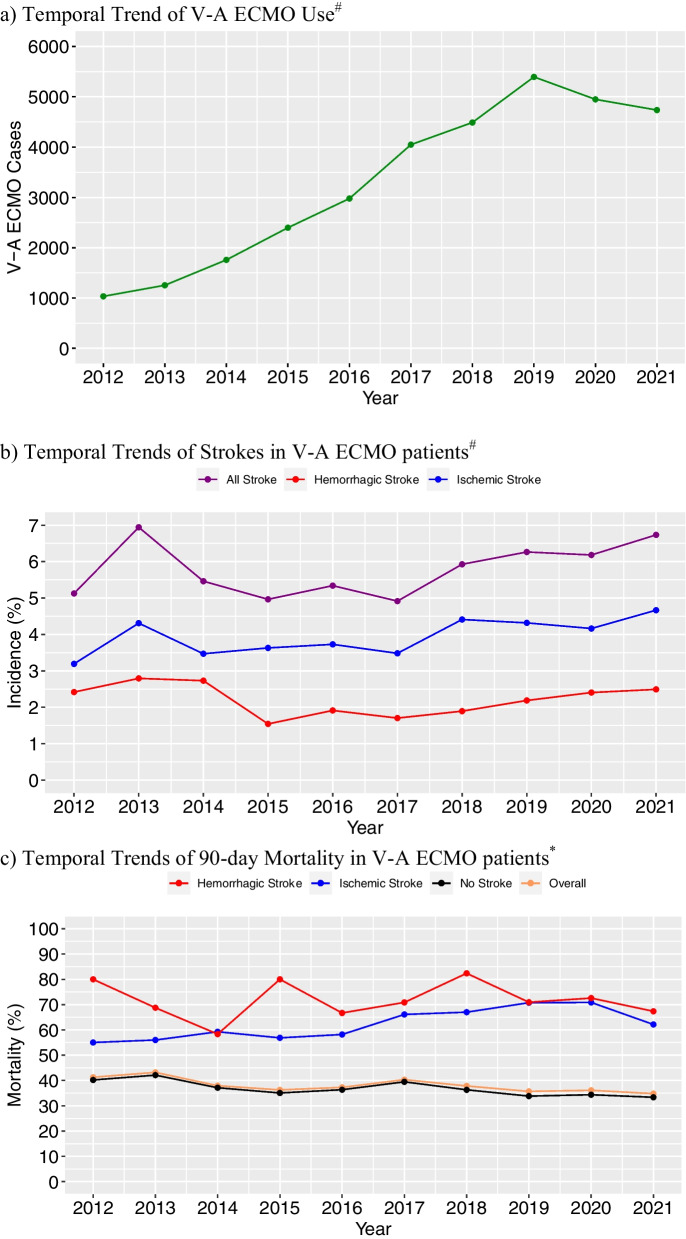
Trend of V-A ECMO associated ischemic stroke, hemorrhagic stroke, and mortality
Figure 1a shows the trend of V-A ECMO cases submitted to the ELSO registry database. The number of cases has generally increased during the past decade, from 1034 cases in 2012 to 4737 cases in 2021, corresponding to a roughly 1.18 times increase per year (p < 0.0001, Poisson regression). Figure 1b depicts the temporal trends of the incidence of ischemic and hemorrhagic strokes. The incidence of hemorrhagic stroke did not change overall between 2012 and 2021 (p = 0.41, Cochran-Armitage). However, the incidence of ischemic stroke increased (p = 0.002, Cochran-Armitage), with the number of cases increasing roughly 1.21 times per year (p < 0.0001, Poisson regression). Figure 1c and Additional file 2 illustrate the temporal trends of 90-day and 30-day mortality, respectively. The overall 90-day mortality declined (p < 0.0001, Cochran-Armitage) by 1.78% per year between 2012 and 2021 (p = 0.0003, Poisson regression). Similarly, 90-day mortality of patients without strokes also declined (p < 0.0001, Cochran-Armitage) by 2.02% per year (p < 0.0001, Poisson regression). In contrast, 90-day mortality of patients with hemorrhagic stroke did not significantly change over time (p = 0.85). While the 90-day mortality of patients with ischemic stroke showed a potential trend toward increased mortality over time, this did not reach statistical significance (p = 0.053).
Fig. 1.
Temporal Trends of V-A ECMO, Strokes, and 90-day Mortality. a Temporal Trend of V-A ECMO Use#. b Temporal Trends of Strokes in V-A ECMO patients#. c Temporal Trends of 90-day Mortality in V-A ECMO patients*. #: All 33,041 cases; *: 20,297 cases with complete mortality data; V-A ECMO: venoarterial extracorporeal membrane oxygenation
Association between ELSO center volume and incidence of ischemic and hemorrhagic stroke
The center volume per year for ELSO centers ranged from 1 to 84 (median 18, IQR 9–31). Multivariable logistic regression revealed that the center volume per year was not a significant factor for the incidence of ischemic or hemorrhagic stroke (Table 2). On the other hand, 24-h PaO2 and ΔPaCO2 were significantly associated with ischemic stroke incidence—for each increase of 10 mmHg in PaO2, the odds of ischemic stroke increased by 1.6% (p = 0.0006); and for each decrease of 10 mmHg in ΔPaCO2, the odds of ischemic stroke increased by 10.7% (p = 0.0009).
Table 2.
Logistic regression of risk factors for ischemic or hemorrhagic stroke incidence^
| Odds ratio | 95% CI | p value | |
|---|---|---|---|
| Ischemic stroke incidence | |||
| Age (years) | 1.006 | 0.998–1.013 | 0.18 |
| Center volume per year | 1.005 | 0.998–1.012 | 0.17 |
| Year of ECMO support | |||
| 2019a | 0.990 | 0.707–1.390 | 0.95 |
| 2020a | 1.042 | 0.741–1.467 | 0.81 |
| 2021a | 1.113 | 0.795–1.564 | 0.53 |
| Aortic cannulation | 0.887 | 0.645–1.199 | 0.45 |
| ABG related factors | |||
| 24-h PaO2 (mmHg) | 1.002 | 1.001–1.002 | 0.0006 |
| ΔPaCO2 (mmHg) | 0.990 | 0.984–0.996 | 0.0009 |
| 24-h Blood Pump Flow Rate (L/minute) | 1.071 | 0.941–1.219 | 0.30 |
| Hemorrhagic Stroke Incidence | |||
| Age (years) | 0.998 | 0.987–1.010 | 0.80 |
| Center volume per year | 1.009 | 0.998–1.019 | 0.09 |
| Year of ECMO Support | |||
| 2019a | 1.385 | 0.828–2.366 | 0.22 |
| 2020a | 1.304 | 0.766–2.257 | 0.33 |
| 2021a | 1.384 | 0.816–2.389 | 0.23 |
| Aortic cannulation | 0.825 | 0.485–1.329 | 0.45 |
| ABG related factors | |||
| 24-h PaO2 (mmHg) | 0.999 | 0.997–1.000 | 0.21 |
| ΔPaCO2 (mmHg) | 1.000 | 0.990–1.011 | 0.98 |
| 24-h blood pump flow rate (L/minute) | 0.986 | 0.812–1.197 | 0.89 |
Bolded text: Statistically significant with p < 0.05
Abbreviations: ^:12,327 patients from 2018 to 2021 with complete mortality data; aYear 2018 was used as the dummy variable, as the year of ECMO support was used as a categorical variable; ΔPaCO2: change in arterial carbon dioxide pressure between pre-ECMO and 24-h post-cannulation; 24-h PaO2: 24-h post-cannulation arterial oxygen pressure; ABG: arterial blood gas; CI: confidence interval; ECMO: extracorporeal membrane oxygenation
Association between ELSO center volume and mortality
Multivariable logistic regression revealed that lower center volume per year was significantly associated with increased 90-day mortality (p < 0.0001). Additionally, the complications of ischemic stroke and hemorrhagic stroke significantly increased mortality (p < 0.0001 for both). Other significantly associated variables included older age, higher 24-h PaO2, higher 24-h blood pump flow rate, longer duration of ECMO, and complications of gastrointestinal hemorrhage and renal replacement therapy (Table 3, Additional file 3). Brain death occurred in 51 patients (0.4%), however, could not be included in the logistic regression model, given that no patients with brain death (n = 0) had the outcome of survival. Given that both the 24-h PaO2 and the 24-h blood pump flow rate were significantly associated with mortality, a Pearson’s correlation coefficient was calculated, which did not reveal a strong linear correlation (R2 = 0.0016) (Additional file 4).
Table 3.
Logistic regression of risk factors for 90-day mortality^
| Odds ratio | 95% CI | p value | |
|---|---|---|---|
| Age (years) | 1.036 | 1.032–1.039 | < 0.0001 |
| Center volume per year | 0.990 | 0.987–0.993 | < 0.0001 |
| Year of ECMO support | |||
| 2019a | 0.872 | 0.760–1.002 | 0.05 |
| 2020a | 0.929 | 0.807–1.068 | 0.30 |
| 2021a | 0.862 | 0.748–0.903 | 0.04 |
| Aortic cannulation | 0.911 | 0.804–1.052 | 0.18 |
| ABG related factors | |||
| 24-h PaO2 (mmHg) | 1.001 | 1.001–1.002 | < 0.0001 |
| ΔPaCO2 (mmHg) | 1.000 | 0.997–1.003 | 0.79 |
| 24-h blood pump flow rate (L/minute) | 1.077 | 1.020–1.138 | 0.008 |
| ECMO duration (days) | 1.019 | 1.011–1.027 | < 0.0001 |
| Neurological complications | |||
| Cardiac arrhythmia | 1.075 | 0.925–1.249 | 0.34 |
| Cardiopulmonary bypass | 1.006 | 0.890–1.136 | 0.93 |
| Gastrointestinal hemorrhage | 1.722 | 1.328–2.239 | < 0.0001 |
| Hemolysis (moderate-to-severe) | 1.315 | 0.966–1.785 | 0.08 |
| Hemorrhagic stroke | 2.918 | 1.961–4.396 | < 0.0001 |
| Ischemic stroke | 2.987 | 2.299–43.902 | < 0.0001 |
| Neurosurgical intervention | 1.846 | 0.459–8.014 | 0.39 |
| Pump failure | 1.154 | 0.569–2.308 | 0.69 |
| Renal replacement therapy | 2.105 | 1.885–2.350 | < 0.0001 |
Bolded text: Statistically significant with p < 0.05
Abbreviations: ^:12,327 patients from 2018 to 2021 with complete mortality data; a: Year 2018 was used as the dummy variable, as the year of ECMO support was used as a categorical variable; ΔPaCO2: change in arterial carbon dioxide pressure between pre-ECMO and 24-h post-cannulation; 24-h PaO2: 24-h post-cannulation arterial oxygen pressure; ABG: arterial blood gas; CI: confidence interval; ECMO: extracorporeal membrane oxygenation
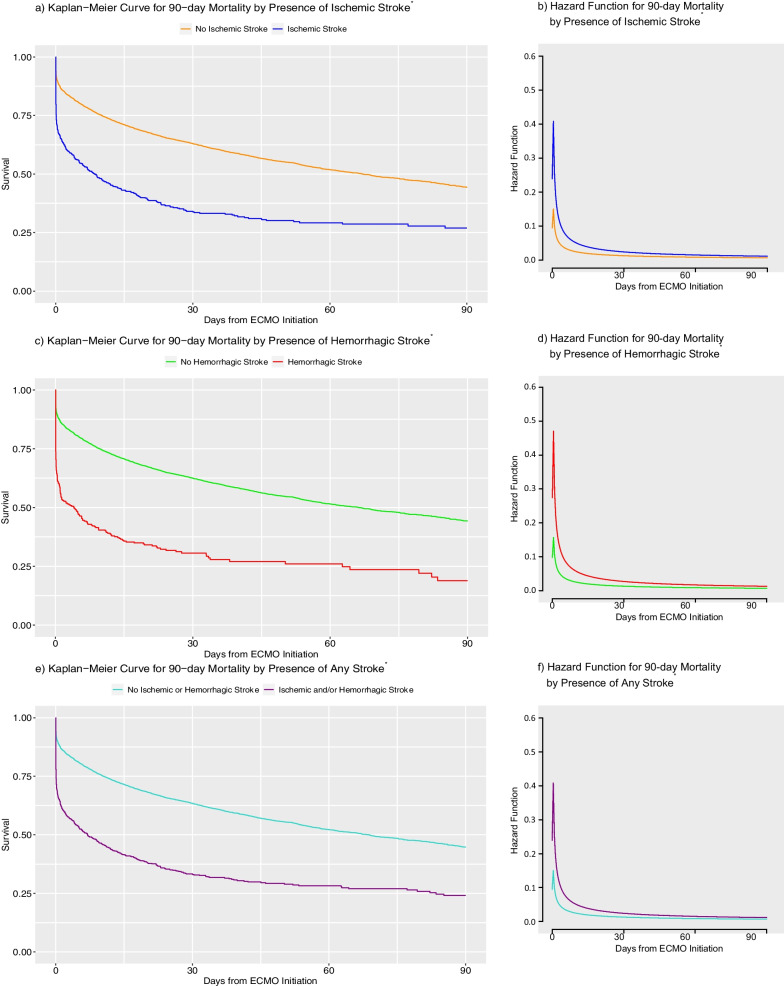
Ischemic and hemorrhage stroke as risk factors for mortality
Figure 2 and Additional file 5 show the overall survival curves and hazard functions of V-A ECMO patients with or without strokes. Median 90-day survival times were significantly different between patients who developed strokes and those who did not: 8.54 vs 67.17 days in the presence or absence of ischemic stroke, respectively (p < 0.0001, log-rank test); 4.00 vs 66.20 days in the presence or absence of hemorrhagic stroke, respectively (p < 0.0001, log-rank test); and 7.00 vs 68.80 days in the presence or absence of any stroke, respectively (p < 0.0001, log-rank test).
Fig. 2.
Kaplan–Meier Curves and Hazard Functions for 90-day Survival by the Presence of Strokes. Abbreviations: *: 20,297 cases with complete mortality data; ECMO: extracorporeal membrane oxygenation
The multivariable logistic regression models for 90-day and 30-day mortality revealed numerous, significantly associated variables (Table 3, Additional file 3). In particular, the odds of 90-day mortality were higher for patients with ischemic stroke than those without (odds ratio = 2.987, p < 0.0001, logistic regression). This was also similar to the case of 90-day mortality of patients with hemorrhagic stroke compared to those without (odds ratio = 2.918, p < 0.0001, logistic regression).
Discussion
This study is the largest to date that assesses the associations of mortality and strokes in the context of other ECMO-related variables, as well as the trends of stroke incidence over 10 years in V-A ECMO. The ELSO registry database has grown markedly, with the number of reported cases increasing nearly fivefold over the past decade, continuing the trend identified in the ELSO study of V-A ECMO from 1992 to 2013 [2]. Encouragingly, the overall 90-day and 30-day mortality rate of V-A ECMO patients have steadily down-trended over time (Fig. 1, Additional file 2). This is also consistent with the survival trends of ECMO patients in the ELSO database since its inception in 1989, which has steadily risen over time from < 1% survival rate [7]. However, the survival for patients who developed ischemic and/or hemorrhagic strokes has not improved. While the incidence of ischemic stroke appears to have mildly increased over time, this may be in the setting of more recognition and vigilance regarding ECMO-related complications, leading to more detection of ischemic strokes, rather than worsening ECMO management. For example, a study conducted at Johns Hopkins Hospital demonstrated that a standardized neuromonitoring protocol for ECMO patients led to higher detection of acute brain injury, yet improved patient outcomes [1]. Alternatively, the increasing incidence of strokes as a complication of V-A ECMO over time may be due to V-A ECMO being offered to a progressively wider patient population, including those who may be more critically ill than in prior years, as ECMO use and practice have evolved over time with more experience and standardized ECMO care. Overall, the incidences of ischemic and hemorrhagic strokes as complications of V-A ECMO were 3.2% and 1.4%, respectively. For comparison, a prior study of V-V ECMO patients in the ELSO registry revealed that the incidences of ischemic and hemorrhagic strokes were 1.4% and 3.1%, respectively [3]. As expected, the incidence of ischemic stroke was higher in V-A ECMO than in V-V ECMO. The fact that the incidence of hemorrhagic stroke was higher in V-V ECMO may be attributed to the fact that cannulation of the internal jugular vein (especially double-lumen cannulation) is more commonly performed, which may lead to complications of cerebral venous sinus thrombosis and/or venous hypertension that can further progress into hemorrhagic strokes [8]. Another potential factor is that the duration of ECMO is longer in V-V EMCO compared to V-A ECMO, thereby increasing the exposure time.
Risk factors associated with on-ECMO complications of ischemic stroke in the logistic regression model included 24-h PaO2 and ΔPaCO2 (Table 2). These findings are consistent with a prior ELSO study of V-A ECMO from a slightly older timeframe, which identified that large reductions in PaCO2 over 24-h were associated with increased neurological complications [9]. Another recent ELSO study, albeit regarding the ECPR patient population, also showed that early severe hyperoxia during ECMO is a significant risk factor for complications of acute brain injury [10]. However, center volume per year was not associated with incidence of ischemic or hemorrhagic stroke. This may be related to the fact that there is no standardized protocol for monitoring patients for on-ECMO complications of strokes, which is made especially difficult due to limitations in performing reliable physical exams in the setting of sedating medications. Further studies are needed to identify the optimal timing of neuro-imaging to detect strokes during ECMO.
In contrast, ELSO centers with higher annual case volumes generally had lower mortality, such that for each 10 additional cases per year performed at a given ELSO center, the 90-day mortality reduced by 9.7%. This finding is similar to other ECMO studies of different patient populations (ECPR, ECMO for respiratory failure, and ECMO for cardiogenic shock), which also identified that mortality was lower at centers with higher annual case volumes [11–13]. This association is likely, at least in part, due to ECMO centers with higher annual case volumes having more established infrastructure, experience, and knowledge of ECMO therapy, thereby achieving greater success rates.
Additionally, the presence of ischemic and/or hemorrhagic stroke was significantly associated with increased 90-day and 30-day mortality (Fig. 2, Additional file 5). The hazard of death was highest in the first week of ECMO support, by which time 82% of all ischemic strokes and 78% of all hemorrhagic strokes had occurred, then plateaued in the subsequent weeks. Hazards were even higher for patients who developed strokes early on as a complication of ECMO compared to those who did not. Prior literature evaluating the associations between mortality and strokes are limited, both in quantity and the mostly single-center nature of the studies. Overall, these studies have shown mixed results, with some reporting hemorrhagic stroke, but not ischemic stroke, as a risk factor for increased mortality during ECMO support [14, 15], while others also reporting ischemic stroke to be a risk factor [16–19]. In this context, our multi-center study contributes further evidence that both ischemic and hemorrhagic strokes are associated with increased 90-day and 30-day mortality.
The logistic regression model identified numerous other risk factors that are associated with higher mortality (Table 3, Additional file 3). Patients who require longer ECMO support are likely more critically ill and more prone to developing on-ECMO complications, which can lead to poorer prognosis. The positive associations between mortality and the risk factors of older age, longer ECMO duration, higher PaO2, and renal replacement therapy are also consistent with prior studies [4, 9, 20]. Additionally, the fact that gastrointestinal hemorrhage, renal replacement therapy, and brain death are associated with both incidence of ischemic stroke and mortality suggests that these on-ECMO complications likely represent a diffuse, systemic process that collectively contributes to increased mortality (Table 1). Finally, in contrast to the incidence of ischemic stroke, mortality was associated with higher 24-h blood pump flow rate. However, there was no significant linear correlation between higher 24-h blood pump flow rate and 24-h PaO2 (Additional file 4). This suggests that while hyperoxia can be detrimental during ECMO by increasing the risk of both ischemic strokes and mortality, these relations cannot be attributed to the blood pump flow rates alone. The strong association between higher 24-h blood pump flow rate and mortality may be representative of patients who lack native cardiac output and thus are more critically ill.
Limitations
This study has several limitations. First, there were missing and/or unavailable data in the ELSO database, including the size and severity of strokes during ECMO support, which could not be accounted for in the analyses. Nevertheless, the major advantage of the ELSO registry data is its large sample size that allows for higher statistical power, hundreds of available variables, and the multi-institutional nature that allows for generalizability of the study. Second, while the center volume analysis focused on annual case volume, this does not account for the number of years that the centers have been performing ECMO support. However, total center volume registered in the ELSO registry was not chosen as the variable, as the ECMO centers may have operating ECMO programs prior to joining ELSO, thereby not reflecting the true total center experience. Third, the ECMO protocols of the numerous ELSO centers are not necessarily standardized, which may lead to some differences in diagnoses of complications, such as how and when strokes were diagnosed and/or management decisions, such as when neurosurgical interventions were performed. Given that these medical decisions were made based on best clinical judgment and necessity, these differences were considered to be relatively minor overall. Finally, withdrawal of life sustaining therapies was not accounted for in the database or analysis, which often limits the outcomes studies of critically ill patient populations.
Conclusions
Over the past decade, while the incidence of ischemic stroke in V-A ECMO patients has progressively increased, 90-day mortality has decreased, possibly explained by the increased awareness, detection, and management of on-ECMO complications. Higher 24-h PaO2 and greater decrease in PaCO2 from pre-ECMO to 24-h values were associated with greater ischemic stroke incidence, while higher annual center volume was not. On-ECMO complications of ischemic/hemorrhagic strokes, gastrointestinal hemorrhage, and renal replacement, as well as higher 24-h PaO2 and longer ECMO duration, were associated with increased 90-day mortality. In contrast, higher annual center volume was significantly associated with lower 90-day mortality. Hazard of death was highest in the first several days of V-A ECMO.
Supplementary Information
Additional file 1. Flowchart of patient selection.
Additional file 2. Temporal trends of 30-day mortality in V-A ECMO patients.
Additional file 3. Logistic regression of risk factors for 30-day mortality.
Additional file 4. Correlation between 24-hour PaO2 and 24-hour blood pump flow rate.
Additional file 5. Kaplan–Meier curves and hazard functions for 30-day survival by the presence of strokes.
Abbreviations
- ΔPaCO2
Change in PaCO2 between pre-ECMO and post-cannulation 24-h values
- CT
Computed tomography
- ECMO
Extracorporeal membrane oxygenation
- ECPR
Extracorporeal cardiopulmonary resuscitation
- ELSO
Extracorporeal Life Support Organization
- ICD-9
International Classification of Diseases, 9th Revision
- ICD-10
International Classification of Diseases, 10th Revision
- IQR
Interquartile range
- MRI
Magnetic resonance imaging
- PaO2
Arterial oxygen pressure
- PaCO2
Arterial carbon dioxide pressure
- V-A
Venoarterial
Author contributions
JH is the First author, who contributed to data collection and conceptualization of statistical analyses, performed statistical analyses, and drafted and revised the manuscript. AK contributed to data collection, performed statistical analyses, and revised the manuscript. BLS contributed to data collection, performed statistical analyses, and revised the manuscript. GW contributed to conceptualization and critical revision. CW, AMZ, RL and DB were involved in critical revision. KU contributed to statistical plan and critical revision. SMC is the Senior author who formed the hypotheses, conceptualized the study design and statistical analyses, supervised the entire study, and revised the manuscript.
Funding
This study was supported by Dr. Sung-Min Cho’s NHLBI grant (1K23HL157610).
Availability of data and materials
The data that support the findings of this study are available from the Extracorporeal Life Support Organization (ELSO), but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of ELSO.
Declarations
Ethics approval and consent to participate
This study was approved by the local institutional review board (IRB00257651).
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ong CS, Etchill E, Dong J, Shou BL, Shelley L, Giuliano K, Al-Kawaz M, Ritzl EK, Geocadin RG, Kim BS, Bush EL, Choi CW, Whitman GJR, Cho SM. Neuromonitoring detects brain injury in patients receiving extracorporeal membrane oxygenation support. J Thorac Cardiovasc Surg. 2023;165:2104–2110.e1. doi: 10.1016/j.jtcvs.2021.09.063. [DOI] [PubMed] [Google Scholar]
- 2.Lorusso R, Barili F, Mauro MD, Gelsomino S, Parise O, Rycus PT, Maessen J, Mueller T, Muellenbach R, Belohlavek J, Peek G, Combes A, Frenckner B, Pesenti A, Thiagarajan RR. In-hospital neurologic complications in adult patients undergoing venoarterial extracorporeal membrane oxygenation: results from the extracorporeal life support organization registry. Crit Care Med. 2016;44:e964–972. doi: 10.1097/CCM.0000000000001865. [DOI] [PubMed] [Google Scholar]
- 3.Cho SM, Canner J, Caturegli G, Choi CW, Etchill E, Giuliano K, Chiarini G, Calligy K, Rycus P, Lorusso R, Kim BS, Sussman M, Suarez JI, Geocadin R, Bush EL, Ziai W, Whitman G. Risk factors of ischemic and hemorrhagic strokes during venovenous extracorporeal membrane oxygenation: analysis of data from the extracorporeal life support organization registry. Crit Care Med. 2021;49:91–101. doi: 10.1097/CCM.0000000000004707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cho SM, Canner J, Chiarini G, Calligy K, Caturegli G, Rycus P, Barbaro RP, Tonna J, Lorusso R, Kilic A, Choi CW, Ziai W, Geocadin R, Whitman G. Modifiable risk factors and mortality from ischemic and hemorrhagic strokes in patients receiving venoarterial extracorporeal membrane oxygenation: results from the extracorporeal life support organization registry. Crit Care Med. 2020;48:e897–e905. doi: 10.1097/CCM.0000000000004498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Freeman CL, Bennett TD, Casper TC, Larsen GY, Hubbard A, Wilkes J, Bratton SL. Pediatric and neonatal extracorporeal membrane oxygenation: Does center volume impact mortality? Crit Care Med. 2014;42:512–519. doi: 10.1097/01.ccm.0000435674.83682.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barbaro RP, Odetola FO, Kidwell KM, Paden ML, Bartlett RH, Davis MM, Annich GM. Association of hospital-level volume of extracorporeal membrane oxygenation cases and mortality. Analysis of the extracorporeal life support organization registry. Am J Respir Crit Care Med. 2015;191:894–901. doi: 10.1164/rccm.201409-1634OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thiagarajan RR, Barbaro RP, Rycus PT, Mcmullan DM, Conrad SA, Fortenberry JD, Paden ML. ELSO member centers. Extracorporeal Life Support Organization Registry International Report 2016. ASAIO J. 2017;63:60–67. doi: 10.1097/MAT.0000000000000475. [DOI] [PubMed] [Google Scholar]
- 8.Mazzeffi M, Kon Z, Menaker J, Johnson DM, Parise O, Gelsomino S, Lorusso R, Herr D. Large dual-lumen extracorporeal membrane oxygenation cannulas are associated with more intracranial hemorrhage. ASAIO J. 2019;65:674–677. doi: 10.1097/MAT.0000000000000917. [DOI] [PubMed] [Google Scholar]
- 9.Diehl A, Burrell AJC, Udy AA, Alexander PMA, Rycus PT, Barbaro RP, Pellegrino VA, Pilcher DV. Association between arterial carbon dioxide tension and clinical outcomes in venoarterial extracorporeal membrane oxygenation. Crit Care Med. 2020;48:977–984. doi: 10.1097/CCM.0000000000004347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shou BL, Ong CS, Premraj L, Brown P, Tonna JE, Dalton HJ, Kim BS, Keller SP, Whitman GJR, Cho SM. Arterial oxygen and carbon dioxide tension and acute brain injury in extracorporeal cardiopulmonary resuscitation patients: analysis of the extracorporeal life support organization registry. J Heart Lung Transplant. 2023;42:503–511. doi: 10.1016/j.healun.2022.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tonna JE, Selzman CH, Bartos JA, Presson AP, Ou Z, Jo Y, Becker L, Youngquist ST, Thiagarajan RR, Johnson MA, Rycus P, Keenan HT. The association of modifiable postresuscitation management and annual case volume with survival after extracorporeal cardiopulmonary resuscitation. Crit Care Explor. 2022;4:e0733. doi: 10.1097/CCE.0000000000000733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Muguruma K, Kunisawa S, Fushimi K, Imanaka Y. Epidemiology and volume-outcome relationship of extracorporeal membrane oxygenation for respiratory failure in Japan: a retrospective observational study using a national administrative database. Acute Med Surg. 2020;7:e486. doi: 10.1002/ams2.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Araki T, Kondo T, Imaizumi T, Sumita Y, Nakai M, Tanaka A, Okumura T, Yang M, Butt JH, Petrie MC, Murohara T. Relationship between the volume of cases and in-hospital mortality in patients with cardiogenic shock receiving short-term mechanical circulatory support. Am Heart J. 2023;261:109–123. doi: 10.1016/j.ahj.2023.03.017. [DOI] [PubMed] [Google Scholar]
- 14.Nasr DM, Rabinstein AA. Neurologic complications of extracorporeal membrane oxygenation. J Clin Neurol. 2015;11:383–389. doi: 10.3988/jcn.2015.11.4.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Le Guennec L, Cholet C, Huang F, Schmidt M, Bréchot N, Hékimian G, Besset S, Lebreton G, Nieszkowska A, Leprince P, Combes A, Luyt CE. Ischemic and hemorrhagic brain injury during venoarterial-extracorporeal membrane oxygenation. Ann Intensive Care. 2018;8:129. doi: 10.1186/s13613-018-0475-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lan C, Tsai PR, Chen YS, Ko WJ. Prognostic factors for adult patients receiving extracorporeal membrane oxygenation as mechanical circulatory support–a 14-year experience at a medical center. Artif Organs. 2010;34:E59–64. doi: 10.1111/j.1525-1594.2009.00909.x. [DOI] [PubMed] [Google Scholar]
- 17.Aubin H, Petrov G, Dalyanoglu H, Saeed D, Akhyari P, Paprotny G, Richter M, Westenfeld R, Schelzig H, Kelm M, Kindgen-Milles D, Lichtenberg A, Albert A. A suprainstitutional network for remote extracorporeal life support: a retrospective cohort study. JACC Heart Fail. 2016;4:698–708. doi: 10.1016/j.jchf.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 18.Saeed O, Jakobleff WA, Forest SJ, Chinnadurai T, Mellas N, Rangasamy S, Xia Y, Madan S, Acharya P, Algodi M, Patel SR, Shin J, Vukelic S, Sims DB, Reyes Gil M, Billett HH, Kizer JR, Goldstein DJ, Jorde UP. Hemolysis and nonhemorrhagic stroke during venoarterial extracorporeal membrane oxygenation. Ann Thorac Surg. 2019;108:756–763. doi: 10.1016/j.athoracsur.2019.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim D, Na SJ, Cho YH, Chung CR, Jeon K, Suh GY, Park TK, Lee JM, Song YB, Hahn JY, Choi JH, Choi SH, Gwon HC, Ahn JH, Carriere KC, Yang JH. Predictors of survival to discharge after successful weaning from venoarterial extracorporeal membrane oxygenation in patients with cardiogenic shock. Circ J. 2020;84:2205–2211. doi: 10.1253/circj.CJ-20-0550. [DOI] [PubMed] [Google Scholar]
- 20.Lorusso R, Gelsomino S, Parise O, Mendiratta P, Prodhan P, Rycus P, MacLaren G, Brogan TV, Chen YS, Maessen J, Hou X, Thiagarajan RR. Venoarterial extracorporeal membrane oxygenation for refractory cardiogenic shock in elderly patients: trends in application and outcome from the extracorporeal life support organization (ELSO) registry. Ann Thorac Surg. 2017;104:62–69. doi: 10.1016/j.athoracsur.2016.10.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Flowchart of patient selection.
Additional file 2. Temporal trends of 30-day mortality in V-A ECMO patients.
Additional file 3. Logistic regression of risk factors for 30-day mortality.
Additional file 4. Correlation between 24-hour PaO2 and 24-hour blood pump flow rate.
Additional file 5. Kaplan–Meier curves and hazard functions for 30-day survival by the presence of strokes.
Data Availability Statement
The data that support the findings of this study are available from the Extracorporeal Life Support Organization (ELSO), but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of ELSO.