Abstract
Background
The frequency of antibodies in autoimmune encephalitis (AIE) may vary in different populations, however, data from developing countries are lacking. To describe the clinical profile of AIE in Brazil, and to evaluate seasonality and predictors of AIE in adult and pediatric patients.
Methods
We evaluated patients with possible AIE from 17 centers of the Brazilian Autoimmune Encephalitis Network (BrAIN) between 2018 and 2022. CSF and serum were tested with TBAs and CBAs. Data on clinical presentation, complementary investigation, and treatment were compiled. Seasonality and predictors of AIE in adult and pediatric populations were analyzed.
Results
Of the 564 patients, 145 (25.7%) were confirmed as seropositive, 69 (12.23%) were seronegative according to Graus, and 58% received immunotherapy. The median delay to diagnosis confirmation was 5.97 ± 10.3 months. No seasonality variation was observed after 55 months of enrolment. The following antibodies were found: anti-NMDAR (n=79, 54%), anti-MOG (n=14, 9%), anti-LGI1(n=12, 8%), anti-GAD (n=11, 7%), anti-GlyR (n=7, 4%), anti-Caspr2 (n=6, 4%), anti-AMPAR (n=4, 2%), anti-GABA-BR (n=4, 2%), anti-GABA-AR (n=2, 1%), anti-IgLON5 (n=1, 1%), and others (n=5, 3%). Predictors of seropositive AIE in the pediatric population (n=42) were decreased level of consciousness (p=0.04), and chorea (p=0.002). Among adults (n=103), predictors of seropositive AIE were movement disorders (p=0.0001), seizures (p=0.0001), autonomic instability (p=0.026), and memory impairment (p=0.001).
Conclusion
Most common antibodies in Brazilian patients are anti-NMDAR, followed by anti-MOG and anti-LGI1. Only 26% of the possible AIE patients harbor antibodies, and 12% were seronegative AIE. Patients had a 6-month delay in diagnosis and no seasonality was found. Findings highlight the barriers to treating AIE in developing countries and indicate an opportunity for cost-effect analysis. In this scenario, some clinical manifestations help predict seropositive AIE such as decreased level of consciousness, chorea, and dystonia among children, and movement disorders and memory impairment among adults.
Keywords: autoimmune encephalitis, Anti-NMDA-receptor encephalitis, anti-glycine receptor antibody, encephalitis, antineuronal antibodies, anti-MOG antibodies
Introduction
Autoimmune encephalitis (AIE) is a group of inflammatory diseases characterized by prominent neuropsychiatric symptoms associated with antineuronal and antiglial antibodies, usually directed against ion channel molecules or proteins associated with neurotransmitter receptors (1). The most common type of AIE is an anti-N-methyl-D-aspartate receptor (anti-NMDAR) encephalitis (2, 3). Patients with this condition are usually children or young adults, that present with subacute psychosis, memory complaints and/or movement disorders. A substantial proportion of patients become severely ill, presenting with a decreased level of consciousness, refractory status epilepticus, dysautonomia, or central hypoventilation (4). Diagnosis is based on clinical manifestations, complementary investigation, and antibody testing (3), according to the criteria of Graus. First-line treatment involves steroids, intravenous immunoglobulin (IVIg), and/or plasmapheresis (5–7), and variables associated with poor prognosis are delay in treatment over 4 weeks, CSF pleocytosis, abnormal brain MRI, and admission to an intensive care unit (8).
Reports from centers across different global regions show varying frequencies of AIE antibodies, such as anti-LGi1, anti-Caspr2, and anti-GABA-BR-associated encephalitis (9–11). For instance, Iran has a higher incidence of anti-GABA-BR-associated encephalitis when compared to other Asian countries and the United States (11). A study of the serum of 22,472 adult patients found that less than 4% of the samples harbor antineuronal antibodies, most commonly anti-NMDAR antibodies (24.6%), anti-GAD (21,5%) and anti-LGI1 antibodies (20,5%) (12). Among children (n=251), the most common antibodies detected were anti-NMDAR followed by anti-MOG (12). Interestingly, encephalitis associated with anti-MOG has been observed in both adult and pediatric populations.
AIE is not a rare cause of encephalitis (6). In developed countries, AIE prevalence was estimated in 8-13 cases/100.000 inhabitants, affecting people of all ages (13). Prior data from northern Europe showed that 20% of all encephalitis are immune-mediated (14) and in the California Encephalitis Project, 47% of encephalitis in patients under 30 years of age were identified as AIE (15). Moreover, reports from some centers or small geographic regions of non-tropical countries suggested that AIE might be seasonal, with higher frequency in warmer months (16, 17).
Information on AIE from developing countries is scarce. A review of all reported cases of AIE in Latin America published in 2020 included only 383 patients, probably due to underdiagnosis (18). Barriers to AIE diagnosis include limited access to testing. Over the past four years, we have established the Brazilian Autoimmune Encephalitis Network, which involves 17 sites in partnership with the Medical University of Vienna. We aimed to describe the clinical manifestations of seropositive Brazilian patients, evaluate AIE seasonality from a tropical country, and identify clinical variables as predictors of AIE in adult and pediatric patients.
Material and methods
Brazilian Autoimmune Encephalitis Network (BrAIN) comprises 17 sites from all geographic Brazilian regions (including the states of Ceará, Alagoas, Pernambuco, Bahia, Maranhão, Rio Grande do Norte, Distrito Federal, Rio de Janeiro, São Paulo, Paraná, and Santa Catarina). Principal investigators from each Neurology Department’s site included patients from June 2018 to November 2022 with the following inclusion criteria: (1) possible AIE according to Graus (3) and (2) agreement to informed consent. This study was approved by the local Ethical Committee and was supported by the Medical University of Vienna, Fleury Group, and FAPESP.
Clinical and epidemiological information was compiled using REDCap. Data on gender, age at onset, clinical presentation, behavioral, cognitive, and motor symptoms, and initial treatment were collected. Additionally, data from complementary investigations such as CSF analysis, EEG, and brain MRI were recorded. The coordinator center further reviewed all information for a final decision on eligibility for antibody testing. Upon decision from the coordinating team, CSF and serum samples were frozen to -20°C and shipped to the coordinating center in São Paulo and then sent to the Division of Neuropathology and Neurochemistry, Department of Neurology, Medical University of Vienna.
In the laboratory in Vienna, serum and CSF samples of all patients included were screened for antineuronal autoantibodies (ANeA) using in-house tissue-based assays (TBA) for surface and intracellular antibodies. Samples showing a specific tissue staining in the TBA were sequentially tested using in-house or commercial cell-based assays (CBA) for surface antibodies (anti-NMDAR, anti-AMPAR, anti-GABA-BR, anti-GABA-AR, anti-LGI1, anti-Caspr2, anti-DPPX, anti- IgLON5, anti-neurexin3alpha, anti-mGluR1, and anti-mGluR5) and immunoblot (Ravo PNS 14 Line Assay), according to previously described protocols (19). Under the disclosure of the coordinator center, anti-MOG and anti-GlyR CBA were performed as previously described using in-house CBAs (20, 21). Anti-GAD was detected using TBA and immunoblot (20). Anti-MOG antibodies were screened in serum and if available CSF with an in-house CBA using full-length human MOG. Serum samples were scored according to a high-titer cut-off as MOG reactivity below cut-off (titer 1:40-1:80), moderately positive (titer 1:160-1:320), and strongly positive (titer 1:640 and higher).
Patients under 13 years of age were allocated to the pediatric cohort. After receiving the antibody results, the coordinator site classified adult and pediatric participants into 3 groups: seropositive (SP) AIE, seronegative (SN) AIE, and non-AIE. SP and SN AIE were diagnosed according to Graus criteria (3, 21). Because we wanted to evaluate SN patients according to Graus criteria, patients fulfilling the criteria of seronegative limbic encephalitis were not included in the SN group. All charts were reviewed for clinical phenotype characterization. We only included in the SN group patients fulfilling criteria for probable negative AIE criteria according to Graus.
Clinical, epidemiological, laboratory, and imaging characteristics were compared according to seropositivity using Mann-Whitney, chi-square, or Fisher’s exact test. AIE seasonality was based on the date of symptoms onset and was evaluated over the 55 months of the study, using the time series analysis of Ljung-Box Figure 1 . Variables associated with SP AIE in adult and pediatric cohorts were evaluated with univariate analysis followed by logistic regression models. We used SPSS, R, and seatest for the statistical analysis. P-value < 0.05 was considered significant.
Figure 1.
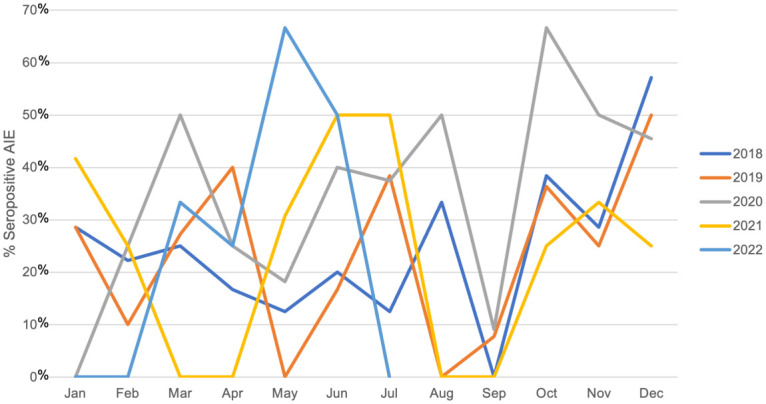
Seasonality of seropositive patients during 2018 and 2022 months using time series analysis of Ljung-Box.
Results
The general profile of Brazilian seropositive patients
We tested 564 patients with possible AIE, 145 (26%) were confirmed as SP AIE, 69 (12%) were classified as SN AIE, 16 (3%) were classified as seronegative limbic encephalitis, and 334 (59%) had another diagnosis. Twenty-seven SP patients presented limbic encephalitis, including two anti-GABA-BR, one anti-GABA-AR, four anti-GAD, two anti-Caspr2, and four anti-LGI1. All SN patients presented with antibody-negative but probable AIE (ANPRA) phenotype.
Forty-two (29%) SP patients were children. The median delay to diagnosis confirmation was 5.97 ± 10.3 months. Sixty-eight patients were from southeast Brazil, 48 from the Northeast region, 14 from the South, 12 from the Midwest, and 3 from the North region. No seasonal variation for SP AIE diagnosis was observed within 55 months of patient enrolment (p= 0.245) ( Figure 1 ).
Antibodies found in this cohort were 79 (54%) anti-NMDAR, 14 (10%) anti-MOG, 12 (8%) anti-LGI1, 11 (8%) anti-GAD, 7 (5%) anti-GlyR, 6 (4%) anti-Caspr2, 4 (3%) anti-AMPAR, 4 (3%) anti-GABA-BR, 2 (1%) anti-GABA-AR, 1 (1%) anti-IgLON5, and 5 others (1 anti-mGluR1, 1 atypical neuropil staining, 1 anti-Neurexin-3-alpha, 1 GFAP, and 1 anti-mGluR5) ( Supplemental Figure ).
Among pediatric SP patients, 55% were female with a mean age of 5.87 ± 2.9 years. Thirty children (71%) had anti-NMDAR, 11 (26%) had anti-MOG, and 1 (2%) had anti-GlyR. Of the 103 SP adult patients, 64% were female, with a mean age of 34.33 ± 20.33 years. Among adults, we found 49 anti-NMDAR patients (47%), 12 anti-LGI1 (11%), 11 anti-GAD (11%), 6 anti-GlyR (6%), 5 anti-Caspr2 (5%), and all the other antibodies described in this cohort.
Five patients presented a co-occurrence of ANeA. Two had anti-NMDAR and anti-MOG, 1 had anti-LGI1 and anti-Caspr2 antibodies, 1 had anti-GFAP and anti-AMPA, and 1 had anti-GlyR and anti-MOG. Ninety-nine patients (68%) had ANeA in both CSF and serum and 20 (14%) had only in serum (1 anti-GABA-BR, 11 anti-MOG, 1 anti-LGI1, and 7 anti-GlyR). Additionally, we found 9 patients with ANeA exclusively in the CSF (8 anti-NMDAR, and 1 anti-MOG).
We found four patients with possible AIE with high-risk antibodies (two with anti-Hu antibodies and two with anti-Yo). We excluded them from this analysis because of their distinct pathophysiology.
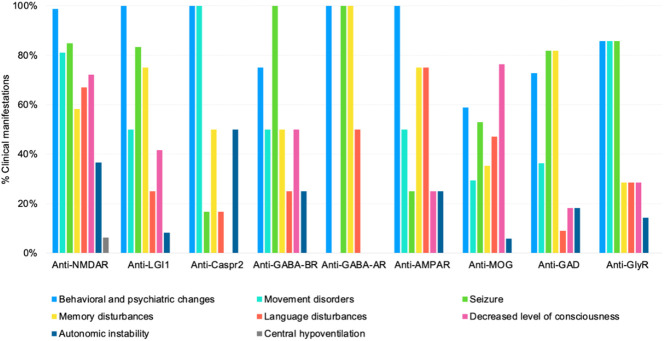
Clinical characterization and complementary investigation
Among anti-NMDAR patients, 67% (n=53) were female and 38% (n=30) were children. All patients had the typical clinical picture, with behavioral symptoms, seizures, and/or movement disorders mostly orofacial dyskinesia (n=34), and dystonia (n=31). EEG showed diffuse slowing or disruption of base activity in 42 patients. All patients had anti-NMDAR antibodies in CSF. Brain MRI was normal in 57% of patients and 14% of patients had uni or bilateral mesial temporal FLAIR/T2 abnormalities. Figure 2 , illustrates the distribution of symptoms by antibody and Table 1 provides an overview of all clinical presentations and complementary investigation.
Figure 2.
Clinical manifestations by the antineuronal antibody. NMDAR, N-methyl-D-Aspartate receptor; LGI1, Leucine-rich glioma inactivated 1; CASPR2, Contactin-associated protein 2; GABA-BR, Gamma-aminobutyric acid-B receptor; GABA-AR, Gamma-aminobutyric acid-A receptor; AMPAR, a-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid receptor; MOG, Myelin oligodendrocyte glycoprotein; GAD, Glutamic acid decarboxylase; GlyR, Glycine receptor.
Table 1.
Clinical and complementary investigation findings by each AIE phenotype.
| Antibody (n) |
Anti-NMDAR (79) |
Anti-LGI1 (12) |
Anti-Caspr2 (6) |
Anti- GABA-BR (4) |
Anti- GABA-AR (2) |
Anti-AMPAR (4) |
Anti-MOG (14) |
Anti-IgLON5 (1) |
Anti-GAD (11) |
Anti-GlyR (7) |
|---|---|---|---|---|---|---|---|---|---|---|
| Age (mean ± SD) | 26.17 ± 21.52 | 58.56 ± 16.73 | 39.54 ± 16.54 | 60.3 ± 16.64 | 59.29 ± 14.89 | 24.56 ± 8.75 | 15.78 ± 21.46 | 62 | 41.04 ± 15.36 | 23.25 ± 13.73 |
| Complementary investigation n (%) | ||||||||||
| Normal EEG | 10 (13) | 3 (25) | 4 (67) | 0 (0) | 0 (0) | 0 (0) | 3 (21) | 0 (0) | 2 (18) | 0 (0) |
| Normal Brain MRI | 45 (57) | 3 (25) | 3 (50) | 2 (50) | 0 (0) | 2 (50) | 3 (21) | 0 (0) | 5 (45) | 3 (43) |
| MTH | 12 (15) | 7 (58) | 2 (33) | 2 (50) | 1 (50) | 0 (0) | 0 (0) | 0 (0) | 5 (45) | 1 (14) |
| CH | 14 (18) | 0 (0) | 0 (0) | 0 (0) | 1 (50) | 1 (25) | 8 (57) | 0 (0) | 0 (0) | 2 (28) |
| WMH | 9 (11) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 5 (36) | 0 (0) | 1 (9) | 1 (14) |
| Encephalic atrophy | 5 (6) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 2 (50) | 0 (0) | 0 (0) | 1 (9) | 0 (0) |
| CSF pleocytosis n (%) | 48 (60) | 2 (17) | 2 (33) | 1 (25) | 0 (0) | 1 (25) | 7 (50) | 1 (100) | 1 (1) | 4 (57) |
NMDAR, N-methyl-D-Aspartate receptor; LGI1, Leucine-rich glioma inactivated 1; CASPR2, Contactin-associated protein 2; GABA-BR, Gamma-aminobutyric acid-B receptor; GABA-AR, Gamma-aminobutyric acid-A receptor; AMPAR, a-amino-3 hydroxy-5-methyl-4-isoxazole propionic acid receptor; MOG, Myelin oligodendrocyte glycoprotein; IgLON5, Immunoglobulin-like cell adhesion molecule 5; GAD, Glutamic acid decarboxylase; GlyR, Glycine receptor; BPC, Behavioral and psychiatric changes; DLC, Decreased level of consciousness; MTH, Mesial temporal hyperintensities; CH, Cortical hyperintensities; WMH, White matter hyperintensities.
Anti-LGI1 patients mostly presented behavioral and psychiatric changes, seizures, and memory disturbances. Most patients with anti-Caspr2 were male and one was female. All of them presented behavioral and psychiatric symptoms, as well as abnormal movements such as dyskinesia, dystonia, or myoclonus, and half of them showed autonomic instability.
All anti-GABA-BR patients presented seizures as the main clinical manifestation and half of them fulfilled the criteria for limbic encephalitis with bilateral mesial temporal hyperintensities in brain MRI. Anti-GABA-AR patients presented behavioral changes, seizures, and brain MRI with mesial temporal or cortical hyperintensities. Half of them had limbic encephalitis and 50% had normal MRI. Anti-AMPAR encephalitis patients presented behavioral complaints, memory, and language disturbance. Half of our patients presented with normal brain MRI, which is an interesting finding.
Of the 14 patients with anti-MOG, 11 were children and 3 were adults. Of note, anti-MOG represented 3% of all SP AIE adult patients and 26% of the children with AIE. Common manifestations were decreased level of consciousness, behavioral and psychiatric changes, and seizures. All patients had serum anti-MOG antibodies at a title higher than 1:80 (in-house CBA). One adult patient met both acute disseminated encephalomyelitis (ADEM) and AIE criteria, and the other two only met the criteria for AIE. Three patients (two adults and one child) had normal brain MRIs, including an 80-year-old female, who presented with memory complaints, hallucinations, and weight loss with a serum antibody titer of 1:160. Additionally, two adult patients were retrospectively diagnosed with anti-MOG encephalitis, with prior negative ANeA testing.
Concerning anti-GAD patients (n=11), four patients presented bilateral mesial temporal hyperintensities, compatible with limbic encephalitis, five had normal brain MRI, one patient with white matter hyperintensities, and another with unilateral mesial temporal hyperintensities.
Anti-GlyR patients (n=7) were mostly adults, and only one was a six-year-old child, who presented acute epilepsy and psychosis, that evolved with abnormal inferior limb posture and ataxia. Only three were male. All patients met AIE criteria and had only anti-GlyR antibodies detected. All developed variable abnormal movements such as ataxia, dyskinesia, tremor, and myokymia. One adult patient had a prior diagnosis of temporal lobe epilepsy with hippocampal atrophy and developed cephalic tremor, ataxia, and dystonia after two years. All of them had epilepsy. EEG findings were abnormal in all cases, mostly focal or diffuse slowing.
Evaluation of prodromal symptoms amongst patients with AIE
Table 2 shows the frequency of prodromal symptoms associated with each antibody. Anti-NMDAR, anti-MOG, and anti-GlyR patients showed the highest frequency of prodromal symptoms.
Table 2.
Frequency of prodromal symptoms by antibody.
| Antibody (n) (%) | Anti-NMDAR (79) |
Anti-LGI1 (12) |
Anti-Caspr2 (6) |
Anti-GABA-BR (4) |
Anti-GABA-AR (2) |
Anti-AMPAR (4) | Anti-MOG (14) |
Anti-IgLON5 (1) |
Anti-GAD (11) |
Anti-GlyR (7) |
|---|---|---|---|---|---|---|---|---|---|---|
| Fever n (%) | 18 (23) | 0 (0) | 0 (0) | 1 (25) | 0 (0) | 1 (25) | 6 (35) | 0/0 | 0 (0) | 2 (28) |
| Nausea n (%) | 10 (13) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (25) | 3 (21) | 0/0 | 1 (9) | 1 (14) |
| Coryza n (%) | 5 (6) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (25) | 1 (7) | 0/0 | 0 (0) | 0 (0) |
| Cough n (%) | 3 (4) | 0 (0) | 0 (0) | 1 (25) | 0 (0) | 1 (25) | 1 (7) | 0/0 | 0 (0) | 1 (14) |
| Headache n (%) | 18 (23) | 1 (8) | 1 (17) | 0 (0) | 0 (0) | 1 (25) | 3 (21) | 0/0 | 0 (0) | 2 (28) |
| Malaise n (%) | 7 (9) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (7) | 0/0 | 1 (9) | 0 (0) |
| Myalgia n (%) | 1 (1) | 1 (8) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (7) | 0/0 | 0 (0) | 1 (14) |
NMDAR, N-methyl-D-Aspartate receptor; LGI1, Leucine-rich glioma inactivated 1; CASPR2, Contactin-associated protein 2; GABA-BR, Gamma-aminobutyric acid-B receptor; GABA-AR, Gamma-aminobutyric acid-A receptor; AMPAR, a-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid receptor; MOG, Myelin oligodendrocyte glycoprotein; IgLON5, Immunoglobulin-like cell adhesion molecule 5; GAD, Glutamic acid decarboxylase; GlyR, Glycine receptor.
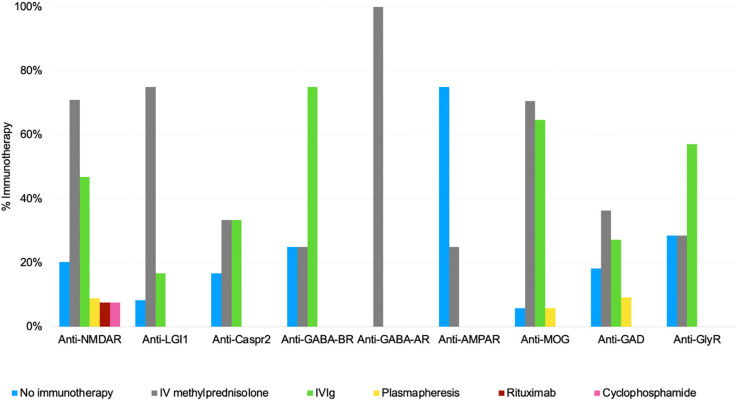
Tumor screening and treatment data
Of the 529 possible AIE patients, 384 (72%) received immunotherapy by the time of enrollment. Intravenous methylprednisolone was the most prescribed treatment (n=339; 64%), followed by IVIg (n=208; 39%), plasmapheresis (n=31; 6%), rituximab (n=21; 4%), and cyclophosphamide (n=21; 4%).
All SP patients were screened for tumors at diagnosis; only 6% had neoplasia (n=9). The most common tumors were thymomas (33%), and ovarian teratomas (22%). Four patients received oncological treatment (tumor resection, chemotherapy, and/or radiation therapy). Notably, in 4 patients neurological symptoms occurred before tumor diagnosis. Among the 79 anti-NMDA encephalitis patients, only one had ovarian teratoma, which was a striking finding. Figure 3 illustrates the treatment prescribed for each SP AIE phenotype. We observed that SP patients rarely received second-line therapy such as rituximab and cyclophosphamide, especially in anti-NMDAR cases.
Figure 3.
The treatment protocol used by each AIE phenotype. NMDAR, N-methyl-D-Aspartate receptor; LGI1, Leucine-rich glioma inactivated 1; CASPR2, Contactin-associated protein 2; GABA-BR, Gamma-aminobutyric acid-B receptor; GABA-AR, Gamma-aminobutyric acid-A receptor; AMPAR, a-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid receptor; MOG, Myelin oligodendrocyte glycoprotein; IgLON5, Immunoglobulin-like cell adhesion molecule 5; GAD, Glutamic acid decarboxylase; GlyR, Glycine receptor; IVIg, Intravenous immunoglobulin; IV, intravenous.
Among SN patients with available treatment data (56/69), 38 patients received methylprednisolone, 26 IVIg, 5 plasmapheresis, 5 rituximab, 4 cyclophosphamide, and 14 received no treatment at enrollment.
Although in this study we did not systematically evaluate the final diagnosis of non-AIE patients, some patient information was available. Alternative diagnoses reported were epilepsy (n=8), rapidly progressive dementia (n=5), Creutzfeldt-Jakob disease (n=5), psychiatric disorder (n=4), systemic lupus erythematosus (n=3), immune-mediated ataxia (n=3), parkinsonism (n=2), Alzheimer’s disease (n=2), frontotemporal dementia (n=2), Behçet’s disease (n=1), normal pressure hydrocephalus (n=1), amyotrophic lateral sclerosis (n=1), HaNDL syndrome (Headache with neurological deficits and CSF lymphocytosis) (n=1), thyrotoxic crisis (n=1), ADEM (n=1), neuromyelitis optica spectrum disorder (n=1), multiple sclerosis (n=1), and unknown (n=20).
Comparison of seropositive and seronegative AIE patients
Patients with SN AIE have inflammation detected in brain MRI (66/67, 98%), CSF cells (54/63, 86%), and OBC (4/14, 28%). Detailed information on SN AIE is available in Table 3 .
Table 3.
Comparison between seropositive and seronegative AIE patients in a Brazilian cohort.
| Pediatric patients (n) |
AIE | p-value | |
|---|---|---|---|
| Seronegative (15) |
Seropositive (42) |
||
| Age (mean ± SD) | 7.27 ± 3.32 | 6.26 ± 2.7 | 0.24 |
| Clinical manifestations n (%) | |||
| BPC | 7 (47) | 34 (81) | 0.01* |
| Memory disturbances | 1 (7) | 16 (38) | 0.02* |
| Seizures | 7 (47) | 31 (74) | 0.06 |
| Movement disorders | 4 (27) | 30 (71) | 0.003* |
| Dystonia | 1 (7) | 17 (40) | 0.02* |
| Dyskinesia | 1 (7) | 14 (33) | 0.05* |
| Chorea | 0 (0) | 11 (26) | 0.03* |
| Language disturbances | 4 (27) | 29 (69) | 0.005* |
| DLC | 7 (47) | 34 (81) | 0.01* |
| MRI findings n (%) | |||
| MTH | 3 (20) | 5 (12) | 0.45 |
| WMH | 7 (47) | 6 (14) | 0.009* |
| CH | 4 (27) | 13 (31) | 0.77 |
| BH | 2 (13) | 4 (9) | 0.66 |
| EEG findings n (%) | |||
| FD | 3 (20) | 11 (26) | 0.64 |
| ES | 3 (20) | 2 (5) | 0.08 |
| EDB | 0 (0) | 5 (12) | 0.16 |
| GD | 2 (13) | 0 (0) | 0.36 |
| Pleocytosis (%) | |||
| CSF cell account (mean ± SD) | 98.1 ± 219.24 | 20.35 ± 38.8 | 0.03* |
| Abnormal CSF n (%) | 12/13 (92) | 22/39 (56) | 0.01* |
| Adult patients (n) |
AIE | p-value | |
|---|---|---|---|
| Seronegative (54) |
Seropositive (103) |
||
| Age (mean ± SD) | 45.17 ± 18.12 | 34.33 ± 20.33 | 0.001* |
| Clinical manifestations n (%) | |||
| BPC | 45 (83) | 97 (94) | 0.02* |
| Memory disturbances | 28 (52) | 69 (67) | 0.07 |
| Seizures | 24 (44) | 79 (77) | <0.0001* |
| Movement disorders | 13 (24) | 69 (67) | <0.0001* |
| Orofacial dyskinesia | 3 (5) | 26 (25) | 0.002* |
| Dystonia | 2 (4) | 22 (21) | 0.005* |
| Dyskinesia | 2 (4) | 18 (17) | 0.02* |
| Abnormal posture | 2 (4) | 16 (15) | 0.04* |
| Chorea | 1 (2) | 8 (8) | 0.13 |
| Language disturbances | 21 (39) | 46 (45) | 0.5 |
| DLC | 28 (52) | 48 (46) | 0.5 |
| Brain MRI findings n (%) | |||
| MTH | 25 (46) | 26 (25) | 0.007* |
| WMH | 15 (28) | 12 (13) | 0.02 |
| CH | 19 (35) | 14 (10) | 0.0001* |
| BH | 11 (20) | 0 (0) | 0.0006* |
| EEG findings n (%) | |||
| FD | 10 (18) | 22 (18) | 1 |
| ES | 4 (7) | 5 (6) | 0.8 |
| EDB | 0 (0) | 10 (9) | 0.02* |
| GD | 1 (2) | 2 (2) | 1 |
| CSF n (%) | |||
| CSF cell account (mean ± SD) | 43.24 ± 89.14 | 19.26 ± 31.45 | 0.01* |
| Abnormal CSF n (%) | 42/50 (84) | 42/101 (41) | <0.0001* |
*p < 0.05.
BPC, Behavioral and psychiatric changes; DLC, Decreased level of consciousness; MTH, Mesial temporal hyperintensities; CH, Cortical hyperintensities; WMH, White matter hyperintensities; BH, Brainstem hyperintensities; FD, Focal discharges; ES, Electrographic seizures; EDB, Extreme Delta-Brush; GD, Generalized discharges.
The comparison of pediatric SN and SP AIE showed that SP pediatric patients had more frequent behavioral and psychiatric changes, memory disturbances, movement disorders (such as chorea, dystonia, dyskinesia), language disturbances, and decreased level of consciousness. SN AIE patients presented more frequent white matter hyperintensities and higher pleocytosis than SP AIE children. We did not find differences between groups in other clinical variables and EEG findings ( Table 1 ).
The comparison of adult SN and SP AIE showed that SP patients were younger, and had more behavioral and psychiatric changes, seizures, movement disorders (such as orofacial dyskinesia, dystonia, dyskinesia), and abnormal posture. Brain MRI abnormalities were more frequent in SN patients. CSF WBCs were lower in SP adults, and we found a higher frequency of extreme delta-brush among SP adult AIE patients. We did not find any differences between groups in other clinical variables ( Table 1 ).
Predictors of AIE among adult and pediatric patients
Clinical variables associated with SP AIE in the pediatric population were decreased level of consciousness and chorea ( Table 2 ). In the adult population, variables associated with SP AIE were movement disorders, seizures, autonomic instability, and memory impairment ( Table 4 ).
Table 4.
Predictors of AIE in pediatric and adult patients.
| Pediatric patients | p-value | Exp(B) | 95% CI | |
|---|---|---|---|---|
| BPC | 0.875 | 0.896 | 0.229 | 3.513 |
| DLC | 0.040* | 3.005 | 1.051 | 8.595 |
| Memory disturbances | 0.879 | 1.127 | 0.243 | 5.219 |
| Language disturbances | 0.167 | 1.930 | 0.759 | 4.907 |
| Movement disorders | 0.288 | 1.692 | 0.641 | 4.464 |
| Chorea | 0.002* | 8.985 | 2.227 | 36.246 |
| Dyskinesia | 0.654 | 1.306 | 0.407 | 4.191 |
| Orofacial dyskinesia | 0.952 | 0.958 | 0.235 | 3.897 |
| Adult patients | p-value | Exp(B) | 95% CI | |
| BPC | 0.997 | 1.002 | 0.341 | 2.947 |
| Memory disturbances | 0.001* | 2.747 | 1.543 | 4.890 |
| Seizures | 0.000* | 4.524 | 2.537 | 8.067 |
| Language disturbances | 0.579 | 0.849 | 0.477 | 1.511 |
| Autonomic instability | 0.026* | 2.128 | 1.096 | 4.131 |
| Movement disorders | 0.000* | 4.130 | 2.359 | 7.228 |
| Chorea | 0.850 | 0.889 | 0.261 | 3.024 |
| Dyskinesia | 0.700 | 1.230 | 0.430 | 3.512 |
| Orofacial dyskinesia | 0.643 | 0.800 | 0.312 | 2.054 |
BPC, Behavioral and psychiatric changes; DLC, Decreased level of consciousness. * p-value < 0.05.
Discussion
In Brazil, the most common antibodies associated with AIE among adults are anti-NMDAR, followed by anti-LGI1, anti-GAD, anti-GlyR, anti-Caspr-2, and anti-AMPAR. These findings align with a large report of 41,217 adults in the United States that reported anti-NMDAR, anti-GAD65, and anti-LGI1 as the most frequent antibodies in serum and CSF (12). However, our results differ from small reports in Hungary (22), China (10, 23), and Iran (11). This might be attributed to the smaller samples in those studies, techniques used for ANeA detection, and potential genetic susceptibilities in different populations, such as the Brazilian admixed population. Some AIE subtypes have specific HLA susceptibility genes (24–26) that have been reported in some populations but not in others, findings which were also reported in neuromyelitis optica and multiple sclerosis (27, 28).
Our results from pediatric patients are in line with prior data from the Spanish, Danish, and Chinese populations, who identified anti-NMDAR and anti-MOG as the most common antibodies among children with possible AIE (29–33). We found only one child with anti-GlyR antibodies that presented with psychosis, abnormal posture, and ataxia. Other antibodies such as anti-AMPAR, anti-LGI1, anti-Caspr2, and anti-GABA-AR were rarely reported in the pediatric population (29–36). Therefore, our findings together with the prior data might indicate that cost-effective panels prioritizing anti-NMDAR and anti-MOG antibodies in children might be a reasonable approach to diagnosis, especially in low-income countries, and to early refer samples to research labs if the child has negative anti-MOG and anti-NMDAR results and fulfill the clinical criteria for pediatric AIE.
In this study, we found anti-GlyR antibodies in 7% of the SP AIE cases without co-occurrence with other antibodies. Anti-GlyR antibodies were initially described in progressive encephalomyelitis with rigidity and myoclonus (PERM) (37). Nonetheless, since 2018 anti-GlyR has been also reported in the serum and/or CSF of patients with epilepsy, cerebellar ataxia, parkinsonism, optic neuritis, multiple sclerosis, ADEM, and Bickerstaff, which may indicate that the antibody is unspecific and not associated with a detailed clinical phenotype (38–42). Additionally, a cohort from Australia reported anti-GlyR in over 20% of patients with possible AIE (38, 43). In our study, all anti-GlyR patients were carefully selected using the AIE criteria, all developed abnormal movements and were screened for other antibodies, including moderate and high-risk antibodies in CSF and serum. Although anti-GlyR antibodies were positive only in serum, and one should interpret these results with caution, such finding has been described in other series (38, 43). We believe our results may help foster the discussion on the relevance of anti-GlyR in AIE and how to interpret positive results. Despite anti-GlyR being also described in other diseases, we believe that in the context of AIE with brainstem involvement and movement disorder, its detection might indicate an immune-mediated pathophysiology. Whether the antibody is truly pathogenic remains unclear. Because anti-GlyR antibodies are not detected in TBA, commercial kits might underestimate their prevalence. Future studies should evaluate whether systematic testing for anti-GlyR is a reasonable strategy when investigating patients with possible AIE.
Another important result from this study is the incidence of anti-MOG in adult patients with AIE. We found that 3% of the adult patients with AIE harbor anti-MOG antibodies which is higher than other antibodies such as anti-GABA-AR and anti-GABA-BR. Anti-MOG encephalitis in adults typically presents with cortical encephalitis, characterized by fever, headache, seizures, and brain MRI FLAIR-hyperintensities (FLAMES) (44, 45), while others report a clinical presentation very similar to ADEM, with a decreased level of consciousness and movement disorders (46–49). We report three cases, with clinical presentation not suggestive of demyelinating symptoms, including a later presentation. Further studies should investigate and confirm the occurrence of anti-MOG encephalitis in adults, especially because treatment and prognosis of anti-MOG may differ from AIE.
Our study confirms that in some populations the proportion of males with anti-NMDAR may reach 30% and association with teratoma and malignancy may vary. Anti-NMDAR encephalitis was mainly seen in young females with a high percentage of cases with an ovarian teratoma (50–53) around 50%, especially in the Caucasian population. We found similar results to the Australian and Chinese cohorts that reported 25% of males and only 10% association with tumors (10, 43). Future genetic analysis of a multiethnic population will clarify this pending question.
We provide consistent information from ANPRA, as all cases classified as seronegative were reviewed and tested with TBA and CBA in both serum and CSF, avoiding misdiagnosis (21). We observed that of the 564 patients with possible AIE, 12% met the criteria for ANPRA phenotype. This specific group of patients was rarely submitted to brain biopsy. We observed that pediatric SN AIE patients were more frequently male and had fewer movement disorders than SP AIE patients (54). Among adults, we found that SN patients were older, and had less cognitive involvement and abnormal movements. Because of those variable clinical manifestations future prospective studies should evaluate the final diagnosis of these patients. We also provide evidence that patients who fulfill the possible AIE criteria may have another disease such as CJD, SLE and other inflammatory diseases, AD, and other degenerative diseases, highlighting the importance of adequate testing to exclude AIE and further look for alternate diagnosis.
Seasonal variation in the onset of autoimmune diseases may reflect changes in external environmental factors, some of which hold the potential to modulate pathogenic processes involved in autoimmunity (55). Prior transversal studies from centers of non-tropical countries supported a higher frequency of AIE in warmer months (16, 17). Although we found more cases in summer, statistical analysis for seasonality was not significant after approximately four years of follow-up.
We report a delay in AIE diagnosis in Brazil by several months, which is longer than other cohorts with a median delay of around 1 month (4). Mainly, this reality is due to limited access to testing, the extensive investigation to rule out a differential diagnosis that mimics AIE (18, 56–58), and the lack of knowledge about the disease among clinical and neurology staff. Although we did not perform a prospective study on outcomes, treatment options, and final diagnoses of the whole cohort, our results might indicate that we prescribe less frequently second-line therapy in confirmed AIE, indicating a barrier to treatment with high-cost medications. Since the appropriate use of resources is critical in low-income countries, we suggest not to test patients when possible AIE criteria are not met. Considering that the estimated prevalence of AIE is higher than neuromyelitis optica spectrum disorder (1-10/100.000) (59), future studies should address cost-effective autoantibody testing for AIE.
The strengths of this study are multicentric design and comprehensive testing with TBA and CBA including systematic screening for anti-GlyR and anti-MOG antibodies. The use of additional CBAs for anti-MOG and anti-GlyR, which are antibodies not detected in TBAs, yielded 6,9% of the cases in these series. However, limitations of the study include its cross-section design, lack of follow-up data, and cost-effectiveness analysis. We identified certain clinical variables that may aid in predicting AIE; in children, the presence of decreased level of consciousness, chorea, and dystonia is associated with AIE. Among adults, memory impairment and movement disorders indicate AIE. We believe these findings can assist clinicians in navigating the clinical scenario and making decisions regarding antibody testing and treatment. However, one exception would be when anti-IgLON5-associated encephalitis is suspected, as the clinical course could be protracted.
In summary, our study provides comprehensive clinical data on both adult and pediatric AIE patients and challenges from developing countries. Our results suggest that anti-GlyR and anti-MOG antibodies may be considered alongside other surface and synaptic antibodies in the cases of AIE. Clinical variables such as memory complaints, decreased level of consciousness, and movement disorders may help navigate the clinical decisions and treatment in patients with possible AIE.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Medical Research Council of Hospital Israelita Albert Einstein. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
BF: Investigation, Conceptualization, Data curation, Formal Analysis, Methodology, Project administration, Writing – original draft, Writing – review & editing. FF: Investigation, Conceptualization, Data curation, Formal Analysis, Methodology, Project administration, Writing – original draft, Writing – review & editing. MES: Methodology, Writing – review & editing. RA: Methodology, Writing – review & editing. AD: Methodology, Resources, Writing – review & editing. PK: Methodology, Writing – review & editing. HT: Methodology, Writing – review & editing. MS: Methodology, Writing – review & editing. AF: Methodology, Writing – review & editing. LJ: Methodology, Writing – review & editing. PB-N: Methodology, Writing – review & editing. PR: Methodology, Writing – review & editing. JO-F: Methodology, Writing – review & editing. RM: Methodology, Writing – review & editing. CO: Methodology, Writing – review & editing. FM: Methodology, Writing – review & editing. RB: Methodology, Writing – review & editing. MLS: Writing – review & editing, Methodology. ES: Methodology, Writing – review & editing. AN: Methodology, Writing – review & editing. KL: Methodology, Writing – review & editing. OG: Methodology, Writing – review & editing. VE: Writing – review & editing, Methodology. LC: Conceptualization, Funding acquisition, Methodology, Resources, Writing – review & editing. RH: Resources, Conceptualization, Funding acquisition, Investigation, Methodology, Writing – original draft, Writing – review & editing. LA: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Acknowledgments
We would like to thank Prof. Angela Tavares and Prof. Leandro Luongo for the invaluable support in statistic analysis.
Funding Statement
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. BrAIN stud received funding from the Medical University of Vienna. R.H. was partly supported by grants from the Austrian Science Fund FWF: project I4685-B and I6565-B (SYNABS; R.H.) and the Austrian Society of Neurology (Österreichische Gesellschaft für Neurologie).
Conflict of interest
Authors AD and LA were employed by Fleury Group.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that this study received funding from Fleury Group. The funder had the following role in the study: data acquisition and logistics.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2023.1256480/full#supplementary-material
Antibodies profile of Brazilian patients with AIE. NMDAR, N-methyl-D-Aspartate receptor; LGI1, Leucine-rich glioma inactivated 1; CASPR2, Contactin-associated protein 2; GABA-BR, Gamma-aminobutyric acid-B receptor; GABA-AR, Gamma-aminobutyric acid-A receptor; AMPAR, a-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid receptor; MOG, Myelin oligodendrocyte glycoprotein; IgLON5, Immunoglobulin-like cell adhesion molecule 5; GAD, Glutamic acid decarboxylase; GlyR, Glycine receptor.
References
- 1. Dalmau J, Graus F. Antibody-mediated encephalitis. New Engl J Med (2018) 378(9):840–51. doi: 10.1056/NEJMra1708712 [DOI] [PubMed] [Google Scholar]
- 2. Armangue T, Titulaer MJ, Malaga I, Bataller L, Gabilondo I, Graus F, et al. Pediatric anti-N-methyl-D-aspartate receptor encephalitis-clinical analysis and novel findings in a series of 20 patients. J Pediatr (2013) 162(4):850–856.e2. doi: 10.1016/j.jpeds.2012.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci T, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol (2016) 15(4):391–404. doi: 10.1016/S1474-4422(15)00401-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Titulaer MJ, McCracken L, Gabilondo I, Armangué T, Glaser C, Iizuka T, et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol (2013) 12(2):157–65. doi: 10.1016/S1474-4422(12)70310-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Armangue T, Spatola M, Vlagea A, Mattozzi S, Cárceles-Cordon M, Martinez-Heras E, et al. Frequency, symptoms, risk factors, and outcomes of autoimmune encephalitis after herpes simplex encephalitis: a prospective observational study and retrospective analysis. Lancet Neurol (2018) 17(9):760–72. doi: 10.1016/S1474-4422(18)30244-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Uy CE, Binks S, Irani SR. Autoimmune encephalitis: clinical spectrum and management. Pract Neurol (2021) 21(5):412–23. doi: 10.1136/practneurol-2020-002567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dutra LA, Abrantes F, Toso FF, Pedroso JL, Barsottini OGP, Hoftberger R. Autoimmune encephalitis: a review of diagnosis and treatment. Arq Neuropsiquiatr. (2018) 76(1):41–9. doi: 10.1590/0004-282X20170176 [DOI] [PubMed] [Google Scholar]
- 8. Balu R, Mccracken L, Lancaster E, Graus F, Dalmau J, Titulaer MJ. A score that predicts 1-year functional status in patients with anti-NMDA receptor encephalitis. Neurology (2019) 92(3):E244–52. doi: 10.1212/WNL.0000000000006783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ghimire P, Khanal UP, Gajurel BP, Karn R, Rajbhandari R, Paudel S, et al. Anti-LGI1, anti-GABABR, and Anti-CASPR2 encephalitides in Asia: A systematic review. Brain Behav (2020) 10(10):e01793–3. doi: 10.1002/brb3.1793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gu Y, Zhong M, He L, Li W, Huang Y, Liu J, et al. Epidemiology of antibody-positive autoimmune encephalitis in southwest China: A multicenter study. Front Immunol (2019) 10:2611. doi: 10.3389/fimmu.2019.02611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Etemadifar M, Aghababaei A, Nouri H, Kargaran PK, Mohammadi S, Salari M. Autoimmune encephalitis: the first observational study from Iran. Neurological Sci (2022) 43(2):1239–48. doi: 10.1007/s10072-021-05400-1 [DOI] [PubMed] [Google Scholar]
- 12. Kunchok A, McKeon A, Zekeridou A, Flanagan EP, Dubey D, Lennon VA, et al. Autoimmune/paraneoplastic encephalitis antibody biomarkers: frequency, age, and sex associations. Mayo Clin Proc (2022) 97(3):547–59. doi: 10.1016/j.mayocp.2021.07.023 [DOI] [PubMed] [Google Scholar]
- 13. Dubey D, Pittock SJ, Kelly CR, McKeon A, Lopez-Chiriboga AS, Lennon VA, et al. Autoimmune encephalitis epidemiology and a comparison to infectious encephalitis. Ann Neurol (2018) 83(1):166–77. doi: 10.1002/ana.25131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Granerod J, Ambrose HE, Davies NWS, Clewley JP, Walsh AL, Morgan D, et al. Causes of encephalitis and differences in their clinical presentations in England: A multicentre, population-based prospective study. Lancet Infect Dis (2010) 10(12):835–44. doi: 10.1016/S1473-3099(10)70222-X [DOI] [PubMed] [Google Scholar]
- 15. Gable MS, Sheriff H, Dalmau J, Tilley DH, Glaser CA. The frequency of autoimmune N-methyl-D-aspartate receptor encephalitis surpasses that of individual viral etiologies in young individuals enrolled in the california encephalitis project. Clin Infect Diseases. (2012) 54(7):899–904. doi: 10.1093/cid/cir1038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Adang LA, Lynch DR, Panzer JA. Pediatric anti-NMDA receptor encephalitis is seasonal. Ann Clin Transl Neurol (2014) 1(11):921–5. doi: 10.1002/acn3.100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lai QL, Cai MT, Zheng Y, Zhang TY, Fang GL, Shen CH, et al. Seasonal variation in autoimmune encephalitis: A multi-center retrospective study. J Neuroimmunol (2021) 359. doi: 10.1016/j.jneuroim.2021.577673 [DOI] [PubMed] [Google Scholar]
- 18. Vasconcelos G de A, Barreira RM, Antoniollo KENT, Pinheiro AMN, Maia CFR, Alves DMBS, et al. Autoimmune encephalitis in latin america: A critical review. Front Neurol (2021) 11:606350. doi: 10.3389/fneur.2020.606350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ricken G, Schwaiger C, de Simoni D, Pichler V, Lang J, Glatter S, et al. Detection methods for autoantibodies in suspected autoimmune encephalitis. Front Neurol (2018) 9:841. doi: 10.3389/fneur.2018.00841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Graus F, Saiz A, Dalmau J. GAD antibodies in neurological disorders — insights and challenges. Nat Rev Neurol (2020) 16(7):353–65. doi: 10.1038/s41582-020-0359-x [DOI] [PubMed] [Google Scholar]
- 21. Dalmau J, Graus F. Diagnostic criteria for autoimmune encephalitis: utility and pitfalls for antibody-negative disease. Lancet Neurol (2023) 22(6):529–40. doi: 10.1016/S1474-4422(23)00083-2 [DOI] [PubMed] [Google Scholar]
- 22. Hayden Z, Böröcz K, Csizmadia Z, Balogh P, Kellermayer Z, Bodó K, et al. Single-center study of autoimmune encephalitis-related autoantibody testing in Hungary. Brain Behav (2019) 9(12):e01454–4. doi: 10.1002/brb3.1454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Deng S, Qiu K, Liu H, Wu X, Lei Q, Lu W. Clinical characteristics and short-term prognosis of autoimmune encephalitis: A single-center cohort study in changsha, China. Front Neurol (2019) 10:539. doi: 10.3389/fneur.2019.00539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Muñiz-Castrillo S, Vogrig A, Honnorat J. Associations between HLA and autoimmune neurological diseases with autoantibodies. Autoimmun Highlights. (2020) 11(1):2. doi: 10.1186/s13317-019-0124-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chang H, Shin YW, Keam B, Kim M, Im SA, Lee ST. HLA-B27 association of autoimmune encephalitis induced by PD-L1 inhibitor. Ann Clin Transl Neurol (2020) 7(11):2243–50. doi: 10.1002/acn3.51213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jobst BC. A genetic disposition for autoimmune encephalitis: searching for human leukocyte antigen (HLA) complex subtypes. Epilepsy Curr (2017) 17(5):273–4. doi: 10.5698/1535-7597.17.5.273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Amezcua L, McCauley JL. Race and ethnicity on MS presentation and disease course. Mult Scler. (2020) 26(5):561–7. doi: 10.1177/1352458519887328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kister I, Bacon T, Cutter GR. How multiple sclerosis symptoms vary by age, sex, and race/ethnicity. Neurol Clin Pract (2021) 11(4):335. doi: 10.1212/CPJ.0000000000001105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Armangue T, Olivé-Cirera G, Martínez-Hernandez E, Sepulveda M, Ruiz-Garcia R, Muñoz-Batista M, et al. Associations of paediatric demyelinating and encephalitic syndromes with myelin oligodendrocyte glycoprotein antibodies: a multicentre observational study. Lancet Neurol (2020) 19(3):234–46. doi: 10.1016/S1474-4422(19)30488-0 [DOI] [PubMed] [Google Scholar]
- 30. Cellucci T, Van Mater H, Graus F, Muscal E, Gallentine W, Klein-Gitelman MS, et al. Clinical approach to the diagnosis of autoimmune encephalitis in the pediatric patient. Neurology(R) neuroimmunol neuroinflammat (2020) 7(2):e663. doi: 10.1212/NXI.0000000000000663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Han JY, Kim SY, Kim H, Hwang H, Choi J, Chae JH, et al. Clinico-radiological characteristics of anti-myelin oligodendrocyte glycoprotein antibody-associated autoimmune encephalitis in children. Dev Med Child Neurol (2022) 64(8):998–1007. doi: 10.1111/dmcn.15174 [DOI] [PubMed] [Google Scholar]
- 32. Kang Q, Liao H, Yang L, Fang H, Hu W, Wu L. Clinical characteristics and short-term prognosis of children with antibody-mediated autoimmune encephalitis: A single-center cohort study. Front Pediatr (2022) 10:880693. doi: 10.3389/fped.2022.880693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. de Bruijn MAAM, Bruijstens AL, Bastiaansen AEM, van Sonderen A, Schreurs MWJ, Sillevis Smitt PAE, et al. Pediatric autoimmune encephalitis: Recognition and diagnosis. Neurology(R) neuroimmunol neuroinflammat (2020) 7(3):e682. doi: 10.1212/NXI.0000000000000682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Jang S, Kim SY, Kim WJ, Chae JH, Kim KJ, Lim BC. A case of pediatric anti-leucine-rich glioma inactivated 1 encephalitis with faciobrachial dystonic seizure. Brain Dev (2023) 45(6):348–53. doi: 10.1016/j.braindev.2023.02.003 [DOI] [PubMed] [Google Scholar]
- 35. Nosadini M, Toldo I, Tascini B, Bien CG, Parmeggiani L, De Gaspari P, et al. LGI1 and CASPR2 autoimmunity in children: Systematic literature review and report of a young girl with Morvan syndrome. J Neuroimmunol. (2019) 335:577008. doi: 10.1016/j.jneuroim.2019.577008 [DOI] [PubMed] [Google Scholar]
- 36. Stredny CM, Blessing MM, Yi V, Ryan ME, Zhang B, Solomon IH, et al. Mimics of pediatric small vessel primary angiitis of the central nervous system. Ann Neurol (2023) 93(1):109–19. doi: 10.1002/ana.26531 [DOI] [PubMed] [Google Scholar]
- 37. Carvajal-González A, Leite MI, Waters P, Woodhall M, Coutinho E, Balint B, et al. Glycine receptor antibodies in PERM and related syndromes: characteristics, clinical features and outcomes. Brain (2014) 137(8):2178–92. doi: 10.1093/brain/awu142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Swayne A, Tjoa L, Broadley S, Dionisio S, Gillis D, Jacobson L, et al. Antiglycine receptor antibody related disease: a case series and literature review. Eur J Neurol (2018) 25(10):1290–8. doi: 10.1111/ene.13721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Yao Q, Fu M, Ren L, Lin C, Cao L. Inspiratory laryngeal stridor as the main feature of progressive encephalomyelitis with rigidity and myoclonus: a case report and literature review. BMC Neurol (2022) 22(1):42. doi: 10.1186/s12883-022-02555-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Piquet AL, Khan M, Warner JEA, Wicklund MP, Bennett JL, Leehey MA, et al. Novel clinical features of glycine receptor antibody syndrome. Neurol - Neuroimmunol Neuroinflammat (2019) 6(5):e592. doi: 10.1212/NXI.0000000000000592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Symonds JD, Moloney TC, Lang B, McLellan A, O'Regan ME, MacLeod S, et al. Neuronal antibody prevalence in children with seizures under 3 years. Neurology (2020) 95(11):e1590. doi: 10.1212/WNL.0000000000010318 [DOI] [PubMed] [Google Scholar]
- 42. Martinez-Hernandez E, Sepulveda M, Rostásy K, Höftberger R, Graus F, Harvey RJ, et al. Antibodies to aquaporin 4, myelin-oligodendrocyte glycoprotein, and the glycine receptor α1 subunit in patients with isolated optic neuritis. JAMA Neurol (2015) 72(2):187–93. doi: 10.1001/jamaneurol.2014.3602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Swayne A, Warren N, Prain K, Gillis D, O'Gorman C, Tsang BK, et al. An Australian state-based cohort study of autoimmune encephalitis cases detailing clinical presentation, investigation results, and response to therapy. Front Neurol (2021) 12:607773. doi: 10.3389/fneur.2021.607773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Patterson K, Iglesias E, Nasrallah M, González-Álvarez V, Suñol M, Anton J, et al. Anti-MOG encephalitis mimicking small vessel CNS vasculitis. Neurol - Neuroimmunol Neuroinflammat (2019) 6(2):e538. doi: 10.1212/NXI.0000000000000538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Budhram A, Mirian A, Le C, Hosseini-Moghaddam SM, Sharma M, Nicolle MW. Unilateral cortical FLAIR-hyperintense Lesions in Anti-MOG-associated Encephalitis with Seizures (FLAMES): characterization of a distinct clinico-radiographic syndrome. J Neurol (2019) 266(10):2481–7. doi: 10.1007/s00415-019-09440-8 [DOI] [PubMed] [Google Scholar]
- 46. Mariotto S, Monaco S, Peschl P, Coledan I, Mazzi R, Höftberger R, et al. MOG antibody seropositivity in a patient with encephalitis: beyond the classical syndrome. BMC Neurol (2017) 17(1):190. doi: 10.1186/s12883-017-0971-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hoftberger R, Guo Y, Flanagan EP, Lopez-Chiriboga AS, Endmayr V, Hochmeister S, et al. The pathology of central nervous system inflammatory demyelinating disease accompanying myelin oligodendrocyte glycoprotein autoantibody. Acta Neuropathol (2020) 139(5):875–92. doi: 10.1007/s00401-020-02132-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Peschl P, Bradl M, Hoftberger R, Berger T, Reindl M. Myelin oligodendrocyte glycoprotein: deciphering a target in inflammatory demyelinating diseases. Front Immunol (2017) 8:529. doi: 10.3389/fimmu.2017.00529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Banwell B, Bennett JL, Marignier R, Kim HJ, Brilot F, Flanagan EP, et al. Diagnosis of myelin oligodendrocyte glycoprotein antibody-associated disease: International MOGAD Panel proposed criteria. Lancet Neurol (2023) 22(3):268–82. doi: 10.1016/S1474-4422(22)00431-8 [DOI] [PubMed] [Google Scholar]
- 50. Florance NR, Davis RL, Lam C, Szperka C, Zhou L, Ahmad S, et al. Anti–N-methyl-D-aspartate receptor (NMDAR) encephalitis in children and adolescents. Ann Neurol (2009) 66(1):11–8. doi: 10.1002/ana.21756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol (2011) 10(1):63–74. doi: 10.1016/S1474-4422(10)70253-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Okamura H, Oomori N, Uchitomi Y. An acutely confused 15-year-old girl. Lancet (1997) 350(9076):488. doi: 10.1016/S0140-6736(97)06208-9 [DOI] [PubMed] [Google Scholar]
- 53. Nokura K, Yamamoto H, Okawara Y, Koga H, Osawa H, Sakai K. Reversible limbic encephalitis caused by ovarian teratoma. Acta Neurol Scand (1997) 95(6):367–73. doi: 10.1111/j.1600-0404.1997.tb00227.x [DOI] [PubMed] [Google Scholar]
- 54. Lee S, Kim HD, Lee JS, Kang HC, Kim SH. Clinical features and treatment outcomes of seronegative pediatric autoimmune encephalitis. J Clin Neurol (2021) 17(2):300–6. doi: 10.3988/jcn.2021.17.2.300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Watad A, Azrielant S, Bragazzi NL, Sharif K, David P, Katz I, et al. Seasonality and autoimmune diseases: The contribution of the four seasons to the mosaic of autoimmunity. J Autoimmun (2017) 82:13–30. doi: 10.1016/j.jaut.2017.06.001 [DOI] [PubMed] [Google Scholar]
- 56. Flanagan EP, Geschwind MD, Lopez-Chiriboga AS, Blackburn KM, Turaga S, Binks S, et al. Autoimmune encephalitis misdiagnosis in adults. JAMA Neurol (2023) 80(1):30–9. doi: 10.1001/jamaneurol.2022.4251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Bastiaansen AEM, van Steenhoven RW, de Bruijn MAAM, Crijnen YS, van Sonderen A, van Coevorden-Hameete MH, et al. Autoimmune encephalitis resembling dementia syndromes. Neurol - Neuroimmunol Neuroinflammat (2021) 8(5):e1039. doi: 10.1212/NXI.0000000000001039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Dinoto A, Zara P, Mariotto S, Ferrari S, Flanagan EP, Budhram A, et al. Autoimmune encephalitis misdiagnosis and mimics. J Neuroimmunol. (2023) 378:578071. doi: 10.1016/j.jneuroim.2023.578071 [DOI] [PubMed] [Google Scholar]
- 59. Hor JY, Asgari N, Nakashima I, Broadley SA, Leite MI, Kissani N, et al. Epidemiology of neuromyelitis optica spectrum disorder and its prevalence and incidence worldwide. Front Neurol (2020) 11:501(June). doi: 10.3389/fneur.2020.00501 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Antibodies profile of Brazilian patients with AIE. NMDAR, N-methyl-D-Aspartate receptor; LGI1, Leucine-rich glioma inactivated 1; CASPR2, Contactin-associated protein 2; GABA-BR, Gamma-aminobutyric acid-B receptor; GABA-AR, Gamma-aminobutyric acid-A receptor; AMPAR, a-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid receptor; MOG, Myelin oligodendrocyte glycoprotein; IgLON5, Immunoglobulin-like cell adhesion molecule 5; GAD, Glutamic acid decarboxylase; GlyR, Glycine receptor.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.