Summary
Neurodegenerative protein conformational diseases (PCDs), such as Alzheimer’s, Parkinson’s, and Huntington’s, are a leading cause of death and disability worldwide and have no known cures or effective treatments. Emerging evidence suggests a role for the gut microbiota in the pathogenesis of neurodegenerative PCDs; however, the influence of specific bacteria on the culprit proteins associated with each of these diseases remains elusive, primarily due to the complexity of the microbiota. In the present study, we employed a single-strain screening approach to identify human bacterial isolates that enhance or suppress the aggregation of culprit proteins and the associated toxicity in Caenorhabditis elegans expressing Aβ1–42, α-synuclein, and polyglutamine tracts. Here, we reveal the first comprehensive analysis of the human microbiome for its effect on proteins associated with neurodegenerative diseases. Our results suggest that bacteria affect the aggregation of metastable proteins by modulating host proteostasis rather than selectively targeting specific disease-associated proteins. These results reveal bacteria that potentially influence the pathogenesis of PCDs and open new promising prevention and treatment opportunities by altering the abundance of beneficial and detrimental microbes.
Introduction
Neurodegenerative protein conformational diseases (PCDs) are characterized by disturbances in proteostasis that result in the aggregation of disease-associated proteins, ultimately leading to tissue death.1 Alzheimer’s disease (AD), Parkinson’s disease (PD), Huntington’s disease (HD), and amyotrophic lateral sclerosis (ALS) are among the most prevalent neurodegenerative diseases, with AD recognized by the World Health Organization (WHO) as one of the leading causes of death worldwide.2 However, despite their increasing prevalence, the etiology and potential therapeutic targets remain obscure. The sporadic onset and variable severity of neurodegenerative diseases, along with their idiopathic nature, suggest the possibility of a triggering factor for their onset and progression. Multiple factors have been associated with the pathogenicity of PCDs, including an expanding body of evidence that suggests the involvement of microbes, but primarily those within the human gut microbiota (HGM). The HGM is considered an “organ” due to its production of essential proteins and metabolites, including vitamins, hormones, and neurotransmitters.3,4 Hence, dysbiosis of the gut microbiota has been linked to various ailments, including neurodegenerative diseases.5
The complexity of the microbiome has made it challenging to determine the precise role of bacteria in the pathogenesis of neurodegenerative diseases. In addition, most of the evidence that associates bacteria with the occurrence of neurodegenerative diseases is based on correlation.6 Interestingly, correlational evidence does not demonstrate any selectivity between different neurodegenerative diseases, despite each disease featuring a unique, specific culprit protein species. For example, a lower abundance of Prevotella spp. has been observed in patients with different PCDs, including PD, and ALS.7–15 Due to this lack of specificity, we hypothesized that bacteria could be affecting these diseases through the host proteostasis network— upstream of protein aggregate formation. This hypothesis is further supported by our previous study in which we identified gram-negative enteropathogens that significantly disrupt proteostasis across tissues in C. elegans.16 The utility of C. elegans as a model to study host-microbe interaction is strengthened by its unique ability to be colonized by a single bacterial strain. Such a feature simplifies the complexity of the microbiome, allowing us to study the effect of individual species on host proteostasis.
Here, we characterized the effect of 229 unique bacterial isolates from the Human Microbiome Project on the aggregation of disease-associated proteins in C. elegans, using transgenic nematodes expressing Aβ1–42, α-synuclein, and polyglutamine (PolyQ). Surprisingly, our results suggest that bacteria-mediated enhancement or suppression of host protein aggregation is not specific to any particular culprit protein species. Instead, our results demonstrate that bacteria broadly affect the aggregation of metastable proteins present within the host proteome. Furthermore, we also observed that the proteostasis-modulating effects of intestinal bacteria reach distal tissues. Thus, our results indicate that bacteria influence host proteostasis, ultimately affecting the ability of both proximal and distal tissues to buffer protein folding. To date, our results provide the most comprehensive characterization of the effect of individual constituents of the human microbiome on host proteostasis. These results reveal the bacterial contribution to the pathogenesis of AD, PD, HD, ALS, and possibly other PCDs. Collectively, our results provide a framework for the development of microbiome-based risk factor assessments and disease management strategies.
Results
Characterization of the human microbiome on host proteostasis
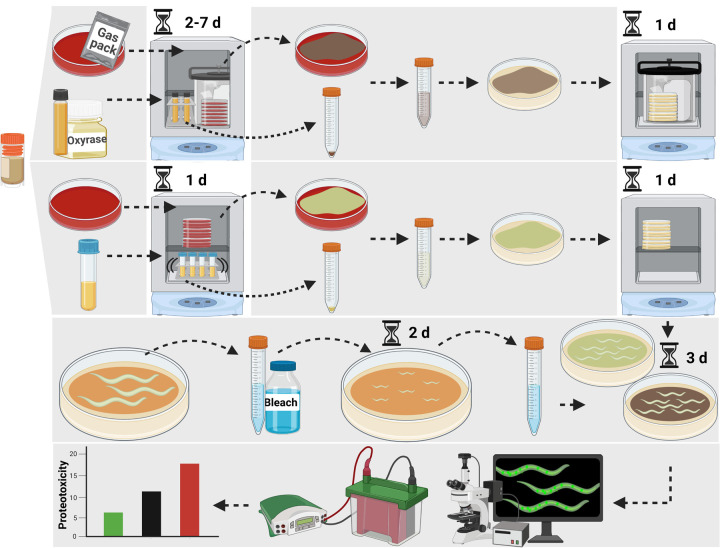
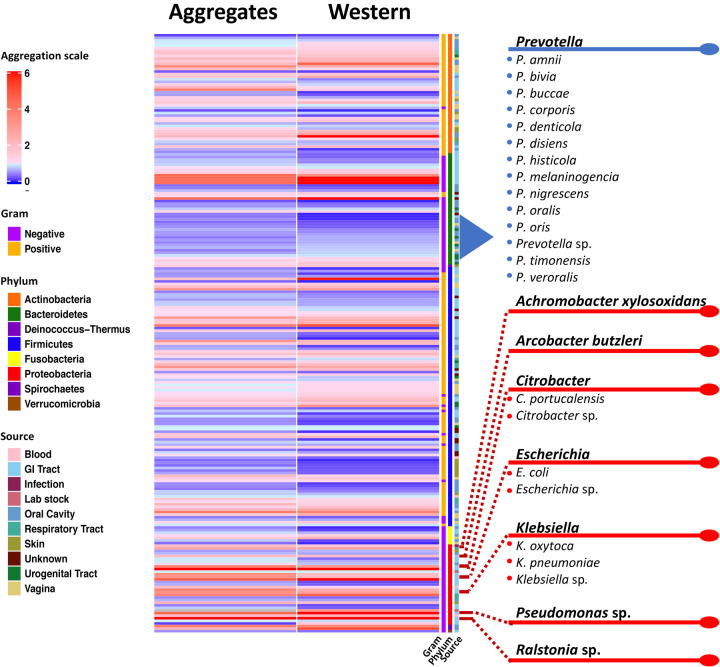
We obtained a comprehensive Human Microbiome Project collection of 229 unique bacterial isolates from BEI Resources and assessed their effect on C. elegans proteostasis. The method used to conduct this experiment is illustrated in Figure 1. The collection encompasses isolates from a range of diverse phyla and a variety of anatomical sites (Figure 2). In our previous study, we used aggregation-prone polyQ tracts as a sensor of the protein folding environment to demonstrate that gram-negative pathogens disrupt host proteostasis.16 Among animals carrying intestine-, muscle-, and neuron-specific polyQ∷YFP, we previously found that proteostasis in the intestine was most robustly affected by the colonizing bacteria.16 As such, we performed our initial screen using the intestinal polyQ model (Figure 2). To eliminate the possibility that bacteria will affect C. elegans development, worms were grown to adulthood prior to being transferred to the bacterial strains of interest. polyQ aggregation was assessed by fluorescent microscopy. To ensure the validity of our results, we also assessed polyQ aggregation by western blotting. Validating our approach, both quantitative methods yielded similar results.
Figure 1. Schematic illustrating the method used to assess the effect of bacterial isolates on C. elegans proteostasis.
Details can be found in Star Methods.
Figure 2. Heat map showing the extent of the screen that identified the effect of human bacterial isolates on C. elegans intestinal polyQ aggregation.
Aggregation data are normalized to worms fed control E. coli OP50.
Bacteria from the isolate collection exhibited a differential effect on C. elegans proteostasis as indicated by increases and decreases in polyQ aggregation compared to worms fed control E. coli OP50 (Figure 2). Figure 2 summarizes the screen revealing bacteria that most robustly affected host proteostasis. For example, Prevotella was the only genus that consistently resulted in low polyQ aggregation across all 229 strains tested (Figure 2). Conversely, significant host proteotoxicity was observed in nematodes that were fed Achromobacter xylosoxidans and Arcobacter butzleri, as well as Citrobacter, Escherichia, Klebsiella, Pseudomonas, and Ralstonia spp. (Figure 2). A detailed list of all bacterial strains and their effect on polyQ aggregation is summarized in Table S1. Intriguingly, our data align with previous research linking the depletion or enrichment of these bacteria in patients with PCDs, which is further described in the discussion section of the present study. To our knowledge, this is the first-ever comprehensive screen that assessed the effect of human bacterial isolates on host proteostasis.
Prevotella spp. mitigate the proteotoxic aggregation of diverse culprit proteins
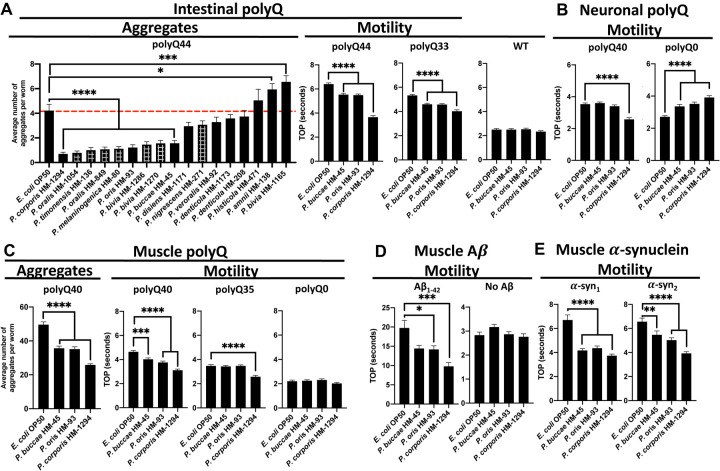
Out of the 229 strains tested, the Prevotella genus had the highest number of members that suppressed polyQ aggregation. We further retested 17 Prevotella spp. using the intestinal polyQ44 model. To increase the robustness of the response, we started feeding animals test bacteria immediately after hatching. Although we observed an enhanced suppression of aggregation for most retested strains, there were few isolates that did not significantly inhibit polyQ aggregation, likely due to the timing of feeding. Furthermore, as expected, feeding worms test bacteria beginning at the L1 larval stage affected development (Figure 3A, “Aggregates”). Out of all strains, P. buccae, P. oris, and P. corporis significantly suppressed polyQ aggregation without causing any detectable developmental delay (Figure 3A, “Aggregates”). Therefore, we followed up with these three strains. Motility defects are associated with neurodegenerative PCDs. As such, we assessed whether the three Prevotella spp. alleviate aggregate-dependent motility defects caused by culprit proteins expressed in the intestine and distal tissues. We used our well-established and validated time-off-pick (TOP) assay that relies on C. elegans motility as a readout of proteotoxicity.16,17 Consistent with their suppression of polyQ aggregation, all three strains alleviated aggregate-dependent motility defects with P. corporis having the strongest effect (Figure 3A, “Motility”). To determine whether the observed suppression is dependent on polyQ, we used N2 wild-type worms and a model expressing a shorter polyglutamine tract, polyQ33. The results revealed no effect on the N2 worms and a less robust suppression of the motility defect for polyQ33, indicating that Prevotella suppressed proteotoxicity.
Figure 3. The effect of Prevotella spp. on proteins associated with neurodegenerative diseases.
A) The effect of Prevotella spp. on C. elegans intestinal polyQ aggregation (“Aggregates”) and the associated toxicity (“Motility”). Checkered bars represent bacteria-associated developmental delay. The three strongest suppressors of polyQ aggregation that did not affect development were tested using intestinal polyQ, B) neuronal polyQ, C) muscle polyQ, D) muscle Aβ1–42, and E) muscle α-synuclein. Data are represented as the average number of aggregates or TOP (seconds) per worm obtained from at least two independent experiments for a total of 30–60 worms. Error bars represent standard error of the mean (SEM). Statistical significance was calculated using one-way ANOVA followed by multiple comparison Dunnett’s post-hoc test (*p<0.05, **p<0.01, ***p<0.001, ****p<0.0001).
To determine whether Prevotella also affects polyQ in distal tissues, we employed the neuronal and muscle models. Because worms expressing the neuronal polyQ do not exhibit quantifiable aggregates, we used the TOP assay as a motility readout. Our results show that of the three strains, only P. corporis showed significant suppression of the motility defect in worms expressing neuronal polyQ40 (Figure 3B). Unexpectedly, P. buccae, P. oris, and P. corporis increased motility defects in the neuronal empty vector control (polyQ0); the reason for this is unknown, but importantly does not diminish the observed beneficial effects of Prevotella on neuronal polyQ. In a manner similar to the intestinal polyQ, we observed Prevotella-mediated suppression of aggregation and proteotoxicity in worms expressing muscle-specific polyQ (Figure 3C).
The association between the low abundance of gut Prevotella and diverse neurodegenerative PCDs suggests that the bacterial influence on these diseases is independent of the culprit protein species.8–14. As such, we hypothesized that bacteria might affect protein aggregation by modulating host proteostasis, and if this is the case, Prevotella spp. should enhance proteostasis in worms expressing various aggregation-prone proteins. To test the effect of Prevotella on other disease-associated proteins, we chose three muscle-specific models: one expressing Aβ1–42, and two expressing α-synuclein.18–20 These culprit proteins model Alzheimer’s and Parkinson’s diseases, respectively. Additionally, these models exhibit age-dependent proteotoxicity, which is consistent with the age-dependent progression of neurodegenerative diseases.16,21,22 To investigate progressive proteotoxicity in the Aβ1–42 and α-synuclein models,18–20 we assessed their motility between days three to five post-hatching (Figure S2). Nematodes expressing Aβ1–42 and α-synuclein had age-dependent motility defects that were markedly greater than those of the controls (Figure S2). We examined the effect of P. buccae, P. oris, and P. corporis on proteotoxicity associated with each of these three models. In a manner similar to the polyQ models, P. buccae, P. oris, and P. corporis reduced aggregate-dependent toxicity compared to wild-type control (Figure 3A), particularly with P. corporis having the strongest effect (Figure 3D, Figure 3E). Bacteria that strongly enhance or suppress host proteostasis induce notable differences in the aggregation of Aβ1–42, which parallels the extent of the motility defect (Figure S1). Both Aβ1–42 aggregation and the associated toxicity were suppressed by P. corporis and enhanced by Pseudomonas aeruginosa (Figure S1), a bacterium that strongly disrupted host proteostasis in our previous studies.16,23 All of our transgenic worms express exogenous proteins. To determine whether Prevotella can also provide protection against misfolding of endogenous proteins, we used a strain that carries a temperature-sensitive mutation in myosin heavy chain (UNC-54) that leads to its misfolding and paralysis at the restrictive temperature (25°C).24,25 In agreement with the proteoprotective effect against misfolding and aggregation of exogenous proteins, Prevotella suppressed the temperature-dependent motility defect at the restrictive temperature, further supporting its beneficial role (Figure S3). Collectively, our findings suggest the broader potential of Prevotella in mitigating the pathogenesis of neurodegenerative diseases.
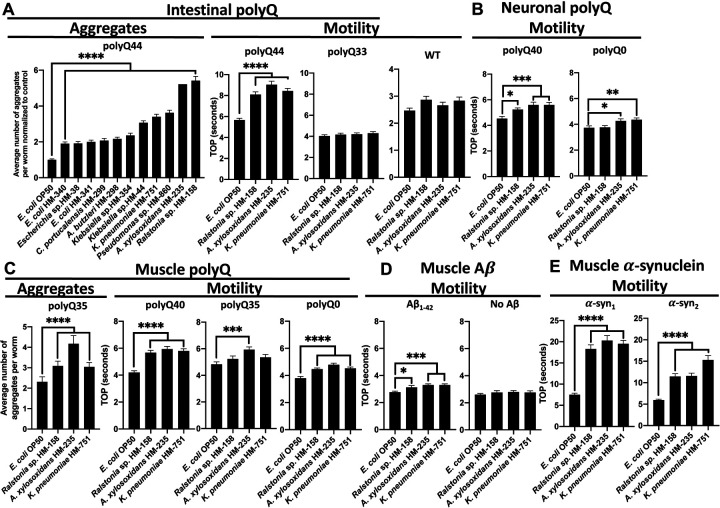
Proteotoxic bacteria enhance the aggregation and toxicity of PCD-associated proteins
To confirm the effect of the most robust proteotoxic strains identified in our original screen (Figure 2, Table S1), we assessed polyQ44 aggregation in animals fed gram-negative aerobes (Figure 4A, “Aggregates”). We concentrated on these specific bacteria because they did not affect worm development, which is known to influence proteostasis.26 We found that Ralstonia sp., Achromobacter xylosoxidans, Pseudomonas sp., and K. pneumoniae were the strongest inducers of polyQ aggregation (Figure 4A). As we have already demonstrated the proteotoxic potential of P. aeruginosa in our previous work,16,23 we focused on the three remaining species in follow-up experiments. To assess the proteotoxic effect of these bacteria, we employed the TOP assay to measure the motility of worms expressing aggregating polyQ44 and non-178 aggregating polyQ33. While we detected a significant enhancement in the motility defect in animals expressing polyQ44, no significant changes were observed in wild-type or in animals expressing polyQ33 (Figure 4A). These results indicate that the impairment of motility induced by bacteria is contingent on polyQ aggregation rather than general bacterial pathogenicity. The aggregate-dependent motility defects were also observed in worms expressing neuronal and muscle-specific polyQ; although, the phenotype was less robust as we did detect some decrease in motility in control animals (Figures 4B and 4C). K. pneumoniae, Ralstonia sp., and A. xylosoxidans also elevated muscle-specific polyQ aggregation (Figure 4C). To test the microbial influence on other disease-associated proteins, we employed worms expressing muscle-specific Aβ1–42 and α-synuclein. In agreement with the intestinal polyQ model, all of these bacterial isolates also induced proteotoxicity associated with these additional culprit proteins (Figures 4D and E). These results demonstrate that bacteria can enhance the proteotoxicity of diverse disease-associated proteins, supporting their role in the pathogenesis of neurodegenerative PCDs.
Figure 4. The effect of proteotoxic bacteria on proteins associated with neurodegenerative diseases.
A) The effect of gram-negative, aerobic bacteria on C. elegans intestinal polyQ aggregation (“Aggregates”) and the associated toxicity (“Motility”). Three robust enhancers of polyQ aggregation were tested using intestinal polyQ, B) neuronal polyQ, C) muscle polyQ, D) muscle Aβ1–42, and E) muscle α-synuclein. Data are represented as the average number of aggregates or TOP (seconds) per worm obtained from at least two independent experiments for a total of 30–60 worms. Error bars represent SEM. Statistical significance was calculated using one-way ANOVA followed by multiple comparison Dunnett’s post-hoc test (*p<0.05, **p<0.01, ***p<0.001, ****p<0.0001).
Discussion
In the present study, we screened a comprehensive collection of 229 unique bacterial isolates from the Human Microbiome Project for their ability to affect host proteostasis from within the intestinal milieu. Our follow-up experiments on the most robust beneficial and detrimental bacteria confirmed their influence on proteostasis across host tissues, affecting the stability of proteins associated with Alzheimer’s, Parkinson’s, and Huntington’s diseases. The phylogenetic analysis revealed clustering of select proteotoxic and proteoprotective bacteria, indicating that genetically related bacteria affect host proteostasis in a similar manner, but with a different magnitude (Figure S4). To our knowledge, this is the first comprehensive characterization of bacteria from human microbiomes on host proteostasis. Surprisingly, our data suggest that bacteria do not selectively target any specific host proteins associated with PCDs, but rather affect proteostasis in general, leading to the aggregation and proteotoxicity of any destabilized proteins present within the proteome, such as exogenous polyQ, Aβ1–42, and α-synuclein, tested in our experiments. While this is a generalized mechanism, there could be microbes that exclusively affect a specific disease.
Numerous studies that employed genomic analyses of microbial compositions in affected patients revealed a connection between comparable gut dysbioses and diverse neurodegenerative PCDs.6 These correlational studies from human subjects support our conclusion that bacteria impact protein stability by modulating host proteostasis. This mechanism is likely mediated by the interplay between host proteostasis and immune responses to bacteria.27,28
Many of the studies aiming to identify neurodegenerative PCD etiology or treat the disease have centered on host-targeted therapeutics, primarily focused on targeting the aggregating proteins or the affected cell types. However, this approach has not been successful in pre-clinical or clinical trials.29,30 Perhaps the focal point of the host-targeted approach occurs too late in the aggregation cascade given that the changes in the gut microbiota can happen prior to any clinical manifestation.31,32 Indeed, individuals with neurodegenerative PCDs have insufficient proteostatic capacity.33 While some studies have attempted to treat neurodegenerative PCDs by enhancing components of the host proteostasis network, these have not been successful.29 In support of our results indicating that bacteria affect host proteostasis, a shift towards microbial-centered therapeutic approaches has shown more promise in lessening disease symptoms. For example, eradication of H. pylori in AD patients was associated with improved disease presentation in a clinical trial and a population-based study.34,35 Interestingly, the beneficial effect of antibiotics on the progression of PCDs, when administered post-onset, is absent when antibiotics were used prior to disease onset; notably, general antibiotic use has been associated with increased risk for PCDs as well as gut dysbiosis.36–38 While H. pylori is a good clinical example of microbial contribution to neurodegenerative diseases, we did not expect to detect proteotoxicity associated with this bacterium in our C. elegans model due to a limitation of our approach that includes transferring and incubating bacteria at sub-optimal temperature – a factor that facilitates H. pylori virulence.39 Additional reports suggest that H. pylori can indirectly affect the composition of the human gut microbiota.40 Microbe-targeted therapeutic approaches hold promise and are further bolstered by a recent study that demonstrated that gut microbiota and serum derived from AD patients accelerate disease symptoms and affect neurogenesis in healthy rats and tissue culture, respectively.41
In our screen (Figure 2), Prevotella stood out as the only genus devoid of any species that exhibit proteotoxicity towards the host. Furthermore, our findings indicate that Prevotella spp. have a broad and suppressive effect on host protein aggregation, regardless of the specific disease-associated protein (Figure 3). Sequencing data suggest that a low abundance of Prevotella in the guts of patients with PCDs enhances disease pathogenesis.7–14 However, despite the fact that the Prevotella genus contains over 50 species, many studies report their results at the genus level.42 Our data indicate that various Prevotella species exhibit a differential effect on host proteostasis (Figure 3A). Such various effects of individual species could be explained by large variability in their genomes.42 The species, P. intermedia, P. nigrescense, and P. melanigencia have been consistently associated with infection,43–45 inflammation,46–49 and have also been linked to AD and associated mortality.50 Conversely, it has been shown that P. buccae and P. corporis, two strains of Prevotella that exhibited strong suppression of protein aggregation and the associated toxicity, were found not to induce inflammation.51 Instead, P. buccae and P. corporis were shown to induce the expression of mucin-associated membrane proteins MUC3 and MUC4.51 Interestingly, induction of MUC3 expression by a probiotic cocktail prevented adherence of enteropathogenic E. coli.52 MUC4 has been shown to be essential for maintaining mucus barrier function and intestinal homeostasis in mice, as its absence resulted in severe large intestinal bleeding and significant down regulation of antimicrobial peptides.53 Though preliminary, the evidence suggesting the protective role of Prevotella in maintaining intestinal integrity is interesting, as intestinal integrity is often compromised in people with neurodegenerative PCDs.54 Damage to the intestinal epithelium can lead to translocation of bacteria and bacterial products, resulting in systemic inflammation and the breakdown of the blood-brain barrier, contributing to a variety of diseases, including PCDs.55,56 The contrasting associations of different Prevotella species in host health and disease, highlight the importance of studying bacteria at the species level, as demonstrated in the present study, to unravel the precise roles of bacteria in disease pathogenesis.
The physiological relevance of our findings is supported by studies that focus on pathogenic bacteria and subsequently establish a connection with PCDs. For example, the robust induction of proteotoxicity by K. pneumoniae across all C. elegans models expressing different aggregation-prone protein species (Figure 4), is in agreement with a previous study that identified an overabundance of K. pneumoniae in the gut microbiota of individuals with AD.57 Furthermore, a positive correlation has been demonstrated between the presence of K. pneumoniae in the gut and elevated levels of the AD biomarker, C-reactive protein, in blood samples of AD patients.58 Another study found an elevated abundance of Ralstonia in mucosal samples from individuals with PD,59 which is another bacterium that was robustly proteotoxic to our C. elegans models (Figure 4). Interestingly, this bacterium was also found to be more prevalent in individuals with autism,60 which is another disease that has been associated with the presence of misfolded proteins.61–64 Autism has also been associated with both Achromobacter and Pseudomonas genera.65,66 Both Achromobacter and Pseudomonas are linked to cystic fibrosis, which is another PCD that does not feature neurodegeneration;67,68 Achromobacter was reported to exacerbate the disease,69 and P. aeruginosa is a predominant pathogenic species that colonizes the lungs of CF patients.70 A. xylosoxidans induced proteotoxicity in all our disease models (Figure 4), along with Pseudomonas, which displayed a notable increase in polyQ aggregation (Figure 4A, “Aggregates”). Furthermore, we previously demonstrated that P. aeruginosa exert robust proteotoxic effects on C. elegans.16,23 The presence of Pseudomonas, in conjunction with another bacterial genus, was successfully used to differentiate individuals with AD from control subjects.71 Collectively, the aforementioned studies are in agreement with our results and further support the wide-ranging impact of bacteria on protein folding diseases. It is remarkable that the abovementioned bacteria induce proteotoxicity consistently across all our C. elegans models expressing distinct disease proteins. The convergence of our results with existing literature linking these bacteria to PCDs strongly reinforces the notion that bacteria affect the host proteostasis network, broadly affecting protein stability.
While our results support a wider-reaching impact of bacteria on the stability of host proteins, it is worth noting that bacteria can selectively target components of the host proteostasis network. For example, P. aeruginosa produces toxins that target the mitochondrial unfolded protein response (UPRMT),72 a transcriptional pathway that ensures proper protein folding and clearance.73 As such, when the UPRMT is overwhelmed or disrupted, proteotoxicity can occur, leading to accelerated protein aggregation.74 Our previous work demonstrated that P. aeruginosa and E. coli can also disrupt host proteostasis through the production of bacteria-derived protein aggregates.16,23 Additionally, P. aeruginosa FapC amyloids were shown to cross-seed with Aβ1–42.75 Interestingly, the fap operon is also present in the genomes of Burkholderiales, which include Ralstonia and Achromobacter.76,77 The E. coli amyloid, curli, enhanced the aggregation of α-synuclein in vivo.78 K. pneumoniae is also capable of producing amyloids,79 and was proteotoxic to all C. elegans lines (Figure 4). The underlying mechanisms of the bacteria-induced proteotoxicity remain elusive; however, it is likely that metastable proteins of bacterial origin sequester host chaperones. Such sequestration would diminish the capacity of the proteostasis network to buffer folding of endogenous proteins. A similar mechanism is supported by the organismal ability to buffer protein polymorphisms present within the host proteome, which is hindered by the introduction of misfolded proteins.80
A comprehensive understanding of individual bacterial residents of the human microbiota in the pathogenesis of neurodegenerative PCDs is crucial in developing effective interventions. Our study challenges the traditional approach of solely focusing on host-targeted therapeutics for neurodegenerative PCDs. Instead, modulating the gut microbiota may offer an effective strategy for preventing and managing these devastating diseases. Gut-targeted interventions will likely have to be implemented early in the disease or even prior to its onset. While our results indicate that bacteria generally affect host proteostasis, ultimately influencing the stability of host proteins, further studies are needed to decipher the role of proteoprotective and proteotoxic species in humans and devise approaches to control their levels.
STAR Methods
Key resources table
C. elegans and bacterial strains that are not from the BEI repository can be found in Table 1.
C. elegans maintenance and strains
C. elegans were maintained as previously described.16 For experiments that generated the data represented in the heat-map (Figure 2), nematodes were kept on E. coli OP50 for two days at 20°C, washed three times and transferred to indicated bacteria, where they were kept at 22.5°C for three days. For all other experiments, nematodes were plated on indicated bacteria as L1s at 22.5°C, where they remained until the time of assay, except for the experiment in Figure S3, in which worms were cultured in temperatures indicated in the figure. All C. elegans strains used in this study can be found in Table 1.
Bacterial culture conditions
All bacteria were cultured at 37°C. Parenthesized numbers (1–5) in ST1 reflect the remaining conditions in which bacteria were grown in the heat-map (Figure 2): 1) anaerobically in reinforced clostridial broth (RCB) with Oxyrase, 2) facultative conditions (no shaking, tube filled to top) in brain heart infusion broth (BHI), 3) aerobic conditions, shaking at 220 revolutions per minute (RPM) in BHI, 4) anaerobic conditions on tryptic soy agar (TSA) supplemented with 5% defibrinated sheep’s blood, 5) aerobic conditions on TSA supplemented with 5% defibrinated sheep’s blood. E. coli OP50 controls were grown in a manner consistent with which experiment was performed. Bacteria were washed and resuspended in M9 before being seeded on NGM. All follow-up experiments were performed with bacteria grown on TSA supplemented with 5% defibrinated sheep’s blood at 37°C except for the intestinal confirmation experiment of the proteotoxic bacteria (Figure 4A, “Aggregates”). Except for Prevotella spp. which were grown under anaerobic conditions, bacteria were grown aerobically in follow-up experiments.
Aggregate quantification
Fluorescent aggregates were quantified using Leica MZ10F Modular Stereo Microscope equipped with CoolLED pE300lite 365 dir mount STEREO with filter set ET GFP-MZ10F. Fluorescent aggregates in worms used to generate data for the heat-map (Figure 2, Table S1) were manually quantified after having been cultured as indicated in “C. elegans maintenance and strains”. For all other experiments, worms were plated on indicated bacteria as L1s and fluorescent aggregates were manually quantified after four days (intestinal polyQ44) or three days (muscle polyQ35, 40) of life as previously described.
Motility assays
All motility assays were performed at room temperature as previously described.16 Time-off-pick (seconds) of transgenic nematodes harboring tissue-specific aggregating protein species was assessed as previously described,16,17 on three days (muscle polyQ, muscle Aβ1–42, TS and respective controls) or four days (intestine polyQ, neuron polyQ, muscle α-synuclein and control) after having been plated on indicated bacteria as L1s.
Live imaging
Nematodes expressing muscle-specific Aβ1–42 were plated as L1s on NGM containing E. coli OP50, P. corporis HM-1294, and P. aeruginosa PAO1 for three days were mounted, frozen to reduce background fluorescence, and imaged. Fluorescent and Nomarski images were taken using Zeiss Axio Observer 7, equipped as described previously.16 Images were processed as previously described.16
Gel electrophoresis and western blotting
Worms were prepared for gel electrophoresis and western blotting which were performed as previously described with a few modifications.16 In brief, M9 was used to lift worms from NGM which were washed until superficial bacteria was removed. Worms were plated on unseeded NGM, were allowed to dry briefly and 50 worms were picked into 10 μL M9 with 1mM phenylmethylsulfonyl fluoride (PMSF) in non-skirted screw-cap microcentrifuge tubes and frozen overnight or longer at −80°C. Tubes were pulse-centrifuged and three, 1.5mm zirconium beads were added to each tube. The following two steps were repeated a minimum of two times; if large worm particulates were observed, these steps were repeated again with the entire sample set until no tubes contained worm pieces that were visible under a dissecting microscope: Samples were homogenized by placing tubes in a Bead Bug homogenizer at 280×10 rates per minute (RPM) for 90 seconds. Tubes were cooled on ice and centrifuged for 1–2 minutes on a low speed to re-settle worms and worm particulates. Samples were prepped for gel electrophoresis as previously described,16 and entire samples were loaded on 4–12% gradient sodium dodecylsulfate-polyacrylamide gels (SDS-PAGE) to separate proteins through electrophoresis. Proteins were transferred onto polyvinyl difluoride (PDVF) membrane, blocked with 5% nonfat milk powder in PBS-Tween-20 (PBST) and probed with Living Colors JL-8 monoclonal primary antibody (1:1000) for 48 hours at 4C on orbital shaker and underwent three, five-minute washes with 0.1% PBST followed by incubation 1:10,000 with goat-anti-mouse horse-radish peroxidase (HRP) conjugated secondary antibody for at least two hours followed by three, ten-minute washes with 0.1% PBST. Chemiluminescence was achieved by incubation with Clarity Western ECL substrate. Image J (v1.52) was used to analyze insoluble fractions.
Quantification and statistical analysis
Quantification of aggregate counts per worm in Figure 2 were performed on a cohort of ten worms to corroborate the findings from the western blot analysis. In the rest of the figures, data are represented as the average number of aggregates or TOP (seconds) per worm obtained from two independent experiments for a total of 45–60 worms (Figure 3A “Aggregates”), 60 worms (Figure 4A “Aggregates”); three independent experiments for a total of 45 worms (Figure 3A “Motility”, Figure 3B, Figure 3C, Figure 4A “Motility”, Figure 4C “Aggregates”) or 30 worms (Figure 3D, Figure 3E, Figure 4B, Figure 4C “Motility”, Figure 4D, Figure 4E, Figure S1B, Figure S3); two independent experiments for a total of 20 worms (Figure S2). Data are described as statistically significant when p<0.05 as determined by Student’s t-test or one-way ANOVA followed by multiple comparison Dunnett’s post-hoc test performed using Graphpad Prism 8.4.3 or later. Degrees of significance are denoted by the use of asterisks such that *p<0.05, **p<0.01, ***p<0.001, ****p<0.0001. The heat map (Figure 1) is represented as data normalized to the control E. coli OP50. Error bars represent standard error of the mean.
Heat map generation
Heatmap was constructed in R-studio using the ComplexHeatmap package from the Bioconductor project. The experimental data were fed into R-studio as an organized .CSV file. The heatmap is the graphical representation of this data, clustering the bacteria by phylum.
Phylogenetic tree generation
Whole genome sequences were assembled using the Bacterial and Viral Bioinformatics Resources Center (BV-BCR) via Unicycler. All genomes were annotated in BV-BRC using Prokka. Phylogenetic analysis was conducted in BV-BRC based on concatenated alignments of 100 single-copy genes using mafft, and the results were assessed for maximum likelihood using RAxML. Sequences that did not have 100 complete single-copy genes due to poor sequencing quality were excluded.
Supplementary Material
Table S1. Data used to generate Figure 2. “Western” indicates the band intensity of the polyQ insoluble fraction of worms fed indicated bacteria normalized to those fed E. coli OP50 control. “Count” indicates the average number of aggregates per worm of worms fed indicated bacteria normalized to those fed E. coli OP50 control. Parenthesized numbers (1–5) reflect the remaining conditions in which bacteria were grown:1) anaerobically in reinforced clostridial broth (RCB) with Oxyrase, 2) facultative conditions (no shaking, tube filled to top) in brain heart infusion broth (BHI), 3) aerobic conditions, shaking at 220 revolutions per minute (RPM) in BHI, 4) anaerobic conditions on tryptic soy agar (TSA) supplemented with 5% defibrinated sheep’s blood, 5) aerobic conditions on TSA supplemented with 5% defibrinated sheep’s blood.
Fig. S1. The robust effect of bacteria on the aggregation of Aβ1–42 correlates with aggregate-dependent changes in motility. (A) Nomarski and fluorescent images (mScarlet) and the corresponding (B) TOP motility measurements of transgenic worms expressing muscle-specific Aβ1–42 fed a proteoprotective strain (P. corporis) and a proteotoxic strain (P. aeruginosa). Each TOP data point is representative of the average of three independent experiments for a total of 30 worms. Error bars represent SEM. Statistical significance was calculated using one-way analysis of variants (ANOVA) followed by multiple comparison Dunnett’s post-hoc test (*p<0.05, **p<0.01, ***p<0.001). Scale bar is 100 μm.
Fig. S2. Aggregate-dependent toxicity in transgenic animals harboring Aβ1–42 and α-synuclein is age-dependent. Age-dependent changes in the motility of animals expressing muscle-specific (A) Aβ1–42 and (B) α-synuclein and corresponding control animals: empty vector (No Aβ) and wild-type N2 (WT). Data are represented as the average TOP (seconds) per worm. Each data point is representative of two independent experiments for a total of 20 worms. Error bars represent SEM. Statistical significance was calculated using one-way analysis of variants (ANOVA) followed by multiple comparison Dunnett’s post-hoc test (***p<0.001, ****p<0.0001).
Figure S3. P. corporis prevents temperature-dependent motility defect. Temperature-dependent changes in the motility of animals expressing a muscle-specific mutation in the myosin heavy-chain gene (e1301). Data are represented as the average TOP (seconds) per worm. Each data point is representative of three independent experiments for a total of 30 worms. Error bars represent SEM. Statistical significance was calculated using one-way analysis of variants (ANOVA) followed by multiple comparison Dunnett’s post-hoc test (****p<0.0001).
Figure S4. Phylogenetic grouping reflects the effect of bacteria on host proteostasis. Phylogenetic tree shows that proteotoxic bacteria predominantly cluster together, separate from proteoprotective bacteria which also form their own distinct cluster. The size of the bacterial identifiers is proportional to the magnitude of their respective proteotoxic or proteoprotective effects. Proteoprotective bacteria are indicated in blue, and proteotoxic bacteria in red. Tree analysis was performed on a large collection of human microbiome isolates in BV-BRC using maximum likelihood based on concatenated alignments of 100 single-copy genes.
Key resources table
| REAGENT or RESOURCE | SOURCE | IDENTIFIER |
|---|---|---|
| Antibodies | ||
| Living Colors JL-8 primary monoclonal antibody | Takara Bio | Cat#632381 |
| Goat anti-mouse HRP secondary antibody | Thermo Scientific | Prod#31430 |
| Bacterial and virus strains | ||
| Escherichia coli OP50 | Caenorhabditis Genetics Center | WB OP50: RRID: WB-STRAIN: OP50; NCBITaxlD: 637912; DC199 |
| Pseudomonas aeruginosa PAOl | Shuman Lab (University of Chicago, USA) | PAOl; DC3 |
| Acetobacteraceae sp. | BEI Resources | HM-648 |
| Achromobacter xylosoxidans | BEI Resources | HM-235 |
| Acidaminococcus sp. | BEI Resources | HM-81 |
| Acidaminococcus sp. | BEI Resources | HM-853 |
| Acinetobacter radioresistens | BEI Resources | HM-107 |
| Actinomyces cardiffensis | BEI Resources | HM-147 |
| Actinomyces gerencseriae | BEI Resources | HM-97 |
| Actinomyces graevenitzii | BEI Resources | HM-236 |
| Actinomyces israelii | BEI Resources | HM-98 |
| Actinomyces johnsonii | BEI Resources | HM-1070 |
| Actinomyces massiliensis | BEI Resources | HM-814 |
| Actinomyces neuii | BEI Resources | HM-1266 |
| Actinomyces odontolyticus | BEI Resources | HM-94 |
| Actinomyces sp. | BEI Resources | HM-1090 |
| Actinomyces sp. | BEI Resources | HM-146 |
| Actinomyces urogenitalis | BEI Resources | HM-1089 |
| Actinomyces viscosus | BEI Resources | HM-238 |
| Aggregatibacter aphrophilus | BEI Resources | HM-206 |
| Akkermansia sp. | BEI Resources | HM-844 |
| Alloscardovia omnicolens | BEI Resources | HM-1282 |
| Anaerococcus hydrogenalis | BEI Resources | HM-1292 |
| Anaerococcus lactolyticus | BEI Resources | HM-1034 |
| Anaerostipes sp. | BEI Resources | HM-220 |
| Arcobacter butzleri | BEI Resources | HM-298 |
| Arthrobacter albus | BEI Resources | HM-1152 |
| Atopobium parvulum | BEI Resources | HM-1035 |
| Atopobium parvulum | BEI Resources | HM-1084 |
| Atopobium sp. | BEI Resources | HM-839 |
| Bacteroides caccae | BEI Resources | HM-728 |
| Bacteroides cellulosilyticus | BEI Resources | HM-726 |
| Bacteroides dorei | BEI Resources | HM-717 |
| Bacteroides eggerthii | BEI Resources | HM-210 |
| Bacteroides finegoldii | BEI Resources | HM-727 |
| Bacteroides fragilis | BEI Resources | HM-20 |
| Bacteroides fragilis | BEI Resources | HM-709 |
| Bacteroides ovatus | BEI Resources | HM-222 |
| Bacteroides salyersiae | BEI Resources | HM-725 |
| Bacteroides sp. | BEI Resources | HM-18 |
| Bacteroides stercoris | BEI Resources | HM-1036 |
| Bacteroides vulgatus | BEI Resources | HM-720 |
| Bacteroidetes | BEI Resources | HM-4 |
| Bifidobacterium adolescentis | BEI Resources | HM-633 |
| Bifidobacterium angulatum | BEI Resources | HM-1189 |
| Bifidobacterium breve | BEI Resources | HM-856 |
| Bifidobacterium longum | BEI Resources | HM-846 |
| Bifidobacterium sp. | BEI Resources | HM-30 |
| Campylobacter coli | BEI Resources | HM-296 |
| Campylobacter upsaliensis | BEI Resources | HM-297 |
| Capnocytophaga ochracea | BEI Resources | HM-15 |
| Capnocytophaga sp. | BEI Resources | HM-840 |
| Capnocytophaga sputigena | BEI Resources | HM-1037 |
| Cardiobacterium valvarum | BEI Resources | HM-477 |
| Catabacter hongkongensis | BEI Resources | HM-1192 |
| Citrobacter portucalensis | BEI Resources | HM-299 |
| Citrobacter sp. | BEI Resources | HM-34 |
| Clostridiales bacterium | BEI Resources | HM-1098 |
| Clostridiales bacterium | BEI Resources | HM-793 |
| Clostridiales sp. | BEI Resources | HM-1182 |
| Clostridium bolteae | BEI Resources | HM-318 |
| Clostridium cadaveris | BEI Resources | HM-1039 |
| Clostridium cadaveris | BEI Resources | HM-1041 |
| Clostridium citroniae | BEI Resources | HM-315 |
| Clostridium clostridioforme | BEI Resources | HM-306 |
| Clostridium difficile | BEI Resources | HM-745 |
| Clostridium difficile | BEI Resources | HM-746 |
| Clostridium difficile | BEI Resources | HM-88 |
| Clostridium innocuum | BEI Resources | HM-173 |
| Clostridium orbiscindens | BEI Resources | HM-1044 |
| Clostridium orbiscindens | BEI Resources | HM-303 |
| Clostridium sp. | BEI Resources | HM-287 |
| Clostridium sp. | BEI Resources | HM-36 |
| Clostridium symbiosum | BEI Resources | HM-309 |
| Collinsella sp. | BEI Resources | HM-304 |
| Coprobacillus sp. | BEI Resources | HM-85 |
| Coprococcus sp. | BEI Resources | HM-794 |
| Corynebacterium amycolatum | BEI Resources | HM-109 |
| Corynebacterium sp. | BEI Resources | HM-1295 |
| Cory ne bacterium sp. | BEI Resources | HM-784 |
| Cory ne bacterium tuscaniense | BEI Resources | HM-1153 |
| Deinococcus grandis | BEI Resources | HM-111 |
| Dermabacter sp. | BEI Resources | HM-857 |
| Dorea formicigenerans | BEI Resources | HM-300 |
| Eggerthella sp. | BEI Resources | HM-1099 |
| Enterococcus faecalis | BEI Resources | HM-432 |
| Enterococcus faecium | BEI Resources | HM-968 |
| Erysipelotrichaceae sp. | BEI Resources | HM-180 |
| Escherichia coli | BEI Resources | HM-340 |
| Escherichia coli | BEI Resources | HM-341 |
| Escherichia sp. | BEI Resources | HM-38 |
| Eubacterium infirmum | BEI Resources | HM-369 |
| Eubacterium sp. | BEI Resources | HM-766 |
| Facklamia sp. | BEI Resources | HM-289 |
| Faecalibacterium prausnitzii | BEI Resources | HM-473 |
| Finegoldia magna | BEI Resources | HM-1285 |
| Fusobacterium gonidiaformans | BEI Resources | HM-1274 |
| Fusobacterium nucleatum | BEI Resources | HM-75 |
| Fusobacterium nucleatum | BEI Resources | HM-260 |
| Fusobacterium sp. | BEI Resources | HM-871 |
| Fusobacterium ulcerans | BEI Resources | HM-57 |
| Gardnerella vaginalis | BEI Resources | HM-1105 |
| Gemella asaccharolytica | BEI Resources | HM-1242 |
| Gemella haemolysans | BEI Resources | HM-239 |
| Gemella morbillorum | BEI Resources | HM-240 |
| Gemella sanguinis | BEI Resources | HM-241 |
| Granulicatella adiacens | BEI Resources | HM-1047 |
| Helicobacter pullorum | BEI Resources | HM-124 |
| Helicobacter pylori | BEI Resources | HM-273 |
| Hungatella hathewayi | BEI Resources | HM-308 |
| Klebsiella oxytoca | BEI Resources | HM-624 |
| Klebsiella pneumoniae | BEI Resources | HM-751 |
| Klebsiella sp. | BEI Resources | HM-354 |
| Klebsiella sp. | BEI Resources | HM-44 |
| Lachnoanaerobaculum sp. | BEI Resources | HM-780 |
| Lactobacillis oris | BEI Resources | HM-560 |
| Lactobacillus crispatus | BEI Resources | HM-375 |
| Lactobacillus gasseri | BEI Resources | HM-399 |
| Lactobacillus gasseri | BEI Resources | HM-647 |
| Lactobacillus iners | BEI Resources | HM-702 |
| Lactobacillus jensenii | BEI Resources | HM-646 |
| Lactobacillus johnsonii | BEI Resources | HM-643 |
| Lactobacillus parafarraginis | BEI Resources | HM-478 |
| Lactobacillus rhamnosus | BEI Resources | HM-106 |
| Leptotrichia goodfellowii | BEI Resources | HM-12 |
| Listeria monocytogenes | BEI Resources | HM-1048 |
| Mageeibacillus indolicus | BEI Resources | HM-1095 |
| Megasphaera micronuciformis | BEI Resources | HM-1172 |
| Microbacterium sp. | BEI Resources | HM-841 |
| Micrococcus luteus | BEI Resources | HM-114 |
| Mobiluncus mulieris | BEI Resources | HM-125 |
| Neisseria flavescens | BEI Resources | HM-115 |
| Neisseria mucosa | BEI Resources | HM-242 |
| Neisseria sp. | BEI Resources | HM-91 |
| Olsenella sp. | BEI Resources | HM-1239 |
| Olsenella uli | BEI Resources | HM-877 |
| Oribacterium sinus | BEI Resources | HM-13 |
| Oscillibacter sp. | BEI Resources | HM-1030 |
| Oxalobacter formigenes | BEI Resources | HM-1 |
| Paenibacillus barengoltzii | BEI Resources | HM-1049 |
| Paenisporosarcina sp. | BEI Resources | HM-788 |
| Parabacteroides goldsteinii | BEI Resources | HM-1050 |
| Parabacteroides merdae | BEI Resources | HM-729 |
| Parvimonas micra | BEI Resources | HM-1052 |
| Parvimonas sp. | BEI Resources | HM-1253 |
| Parvimonas sp. | BEI Resources | HM-207 |
| Peptoniphilus lacrimalis | BEI Resources | HM-1161 |
| Peptoniphilus sp. | BEI Resources | HM-825 |
| Peptoniphilus sp. | BEI Resources | HM-263 |
| Peptostreptococcaceae bacterium | BEI Resources | HM-483 |
| Peptostreptococcus sp. | BEI Resources | HM-1051 |
| Phascolarctobacterium sp. | BEI Resources | HM-179 |
| Plesiomonas sp. | BEI Resources | HM-791 |
| Porphyromonas gingivalis | BEI Resources | HM-1071 |
| Porphyromonas gingivalis | BEI Resources | HM-1073 |
| Porphyromonas sp. | BEI Resources | HM-1064 |
| Porphyromonas sp. | BEI Resources | HM-781 |
| Porphyromonas uenonis | BEI Resources | HM-130 |
| Prevotella amnii | BEI Resources | HM-138 |
| Prevotella bivia | BEI Resources | HM-1165 |
| Prevotella bivia | BEI Resources | HM-1270 |
| Prevotella bivia | BEI Resources | HM-1286 |
| Prevotella buccae | BEI Resources | HM-45 |
| Prevotella corporis | BEI Resources | HM-1294 |
| Prevotella denticola | BEI Resources | HM-1173 |
| Prevotella denticola | BEI Resources | HM-208 |
| Prevotella disiens | BEI Resources | HM-1171 |
| Prevotella histicola | BEI Resources | HM-471 |
| Prevotella melaninogenica | BEI Resources | HM-80 |
| Prevotella nigrescens | BEI Resources | HM-271 |
| Prevotella oralis | BEI Resources | HM-1054 |
| Prevotella oralis | BEI Resources | HM-849 |
| Prevotella oris | BEI Resources | HM-93 |
| Prevotella sp. | BEI Resources | HM-1103 |
| Prevotella sp. | BEI Resources | HM-16 |
| Prevotella sp. | BEI Resources | HM-5 |
| Prevotella timonensis | BEI Resources | HM-136 |
| Prevotella veroralis | BEI Resources | HM-92 |
| Propionibacterium acidifaciens | BEI Resources | HM-8 |
| Propionibacterium acnes | BEI Resources | HM-491 |
| Propionibacterium propionicum | BEI Resources | HM-209 |
| Propionibacterium sp. | BEI Resources | HM-843 |
| Pseudomonas sp. | BEI Resources | HM-860 |
| Psychrobacter sp. | BEI Resources | HM-332 |
| Ralstonia sp. | BEI Resources | HM-158 |
| Rhodococcus erythropolis | BEI Resources | HM-116 |
| Rothia aeria | BEI Resources | HM-818 |
| Rothia dentocariosa | BEI Resources | HM-245 |
| Rothia mucilaginosa | BEI Resources | HM-1055 |
| Ruminococcaceae sp. | BEI Resources | HM-79 |
| Ruminococcus gnavus | BEI Resources | HM-1056 |
| Ruminococcus lactaris | BEI Resources | HM-1057 |
| Scardovia wiggsiae | BEI Resources | HM-470 |
| Selenomonas noxia | BEI Resources | HM-270 |
| Selenomonas sp. | BEI Resources | HM-564 |
| Shigella sp. | BEI Resources | HM-87 |
| Shuttleworthia sp. | BEI Resources | HM-882 |
| Sneathia amnii | BEI Resources | NR-50515 |
| Solobacterium moorei | BEI Resources | HM-1058 |
| Solobacterium moorei | BEI Resources | HM-1059 |
| Sporosarcina sp. | BEI Resources | HM-331 |
| Staphylococcus aureus | BEI Resources | HM-466 |
| Staphylococcus capitis | BEI Resources | HM-117 |
| Staphylococcus caprae | BEI Resources | HM-143 |
| Staphylococcus epidermidis | BEI Resources | HM-140 |
| Staphylococcus haemolyticus | BEI Resources | HM-1164 |
| Staphylococcus hominis | BEI Resources | HM-119 |
| Staphylococcus lugdunensis | BEI Resources | HM-141 |
| Staphylococcus warneri | BEI Resources | HM-120 |
| Stomatobaculum longum | BEI Resources | HM-480 |
| Streptococcus anginosus | BEI Resources | HM-282 |
| Streptococcus cristatus | BEI Resources | HM-163 |
| Streptococcus downei | BEI Resources | HM-475 |
| Streptococcus gallolyticus | BEI Resources | HM-272 |
| Streptococcus intermedius | BEI Resources | HM-368 |
| Streptococcus mitis | BEI Resources | HM-262 |
| Streptococcus parasanguinis | BEI Resources | HM-1060 |
| Streptococcus pneumoniae | BEI Resources | HM-145 |
| Streptococcus salivarius | BEI Resources | HM-121 |
| Streptococcus sobrinus | BEI Resources | HM-1063 |
| Streptococcus sp. | BEI Resources | HM-885 |
| Streptococcus vestibularis | BEI Resources | HM-561 |
| Sutterella wadsworthensis | BEI Resources | HM-852 |
| Tissierellia bacterium | BEI Resources | HM-1096 |
| Treponema denticola | BEI Resources | HM-569 |
| Treponema denticola | BEI Resources | HM-575 |
| Varibaculum cambriense | BEI Resources | HM-1190 |
| Veillonella atypica | BEI Resources | HM-1301 |
| Veillonella montpellierensis | BEI Resources | HM-1157 |
| Veillonella sp. | BEI Resources | HM-778 |
| Weissella cibaria | BEI Resources | HM-1200 |
| Biological samples | ||
| Chemicals, peptides, and recombinant proteins | ||
| Levamisole | Fisher Scientific | Cat#ICN15522805 |
| Cholesterol | MP Biomedicals | Cat#101382 |
| Powdered nonfat milk | Research Products International | M17200–1000 |
| Tween-20 | Fisher BioReagents | Cat#BP337–100 |
| Trans-Blot Turbo Midi-size Transfer Stacks | BioRad | Cat#1704273 |
| Trans-Blot Turbo Midi-size PDVF membrane | BioRad | Cat#10026933 |
| Trans-Blot Turbo 5x transfer buffer | BioRad | Cat#10026938 |
| Criterion XT Precast Gel | BioRad | Cat#3450124 |
| XT 4x Sample Buffer | BioRad | Cat#1610791 |
| 20X Reducing Agent | BioRad | Cat#1610792 |
| XT MOPS | BioRad | Cat#1610788 |
| Clarity Western ECL | BioRad | Cat#1705061 |
| Oxyrase | OXYRASE | Cat#OB-0100 |
| Critical commercial assays | ||
| Deposited data | ||
| Experimental models: Cell lines | ||
| Experimental models: Organisms/strains | ||
| rmls297[vha-6p::q44::yfp; rol-6(su1006)] | Morimoto Lab (Northwestern University, USA) | AM738; intestinal polyQ44 |
| rmls281[vha-6p::q33::yfp; rol-6(su1006 | Morimoto Lab (Northwestern University, USA) | AM712; intestinal polyQ33 |
| rmls133[unc-54p::q40::yfp] | Morimoto Lab (Northwestern University, USA) | AM141; muscle polyQ40 |
| rmls132[unc-54p::q35::yfp] | Morimoto Lab (Northwestern University, USA) | AM140; muscle polyQ35 |
| rmls126[unc-54p::q0::yfp] | Morimoto Lab (Northwestern University, USA) | AM134; muscle polyQO |
| rmls110[F25B3.3p::q40::yfp] | Morimoto Lab (Northwestern University, USA) | AM101; neuronal polyQ40 |
| rmls182[F25B3.3p::q0::yfp] | Morimoto Lab (Northwestern University, USA) | AM52; neuronal polyQO |
| ls[myo-3p::Signalpeptide-Abeta(1-42)::hsp-3(IRES)::wrmScarlet-Abeta(1-42)::unc-54(3’UTR)+rps-Opr.HygroR] | Morimoto Lab (Northwestern University, USA) | JKM7; muscle Aβ1-42 |
| Ex[myo-3p::wrmScarlet-Abeta::unc-54(3’UTR)+rps-Opr.HygroR] | Kirstein Lab (Leibniz Institute on Aging - Fritz Lipmann Institute, Germany) | JKM8, no Aβ1-42 |
| uonEx1[unc-54::alpha-synuclein::CFP+unc-54::alpha-synuclein::YFP(Venus)] | Caenorhabditis Genetics Center | DDP1; α-syn1 |
| pkls2386[unc-54p::alphasynuclein::YFP+unc-119(+)] | Caenorhabditis Genetics Center | NL5901; α-syn2 |
| N2, Bristol | Caenorhabditis Genetics Center | N2, WT |
| unc-54(e1301)l | Caenorhabditis Genetics Center | CB1301; TSΔ |
| Oligonucleotides | ||
| Recombinant DNA | ||
| Software and algorithms | ||
| GraphPad Prism v8.4.0 | GraphPad Software, Inc | http://www.graphpad.com |
| BioRender | BioRender | www.biorender.com |
| RStudio | RStudio Integrated Development for R | http://www.rstudio.com/ |
| BV-BCR | Bacterial and Viral Bioinformatics Resources Center | https://www.bv-brc.org/ |
| Other | ||
| Thermo Scientific- Anaeropack | Fisher Scientific | Cat#23-246-376 |
| ProSignal Blotting Film | Prometheus | Cat#30–810L |
Acknowledgments
We thank Dr. Richard Morimoto and Sue Fox for providing C. elegans polyQ strains (Northwestern University), and Dr. Janine Kirstein (Leibniz Institute on Aging- Fritz Lipmann Institute) for providing C. elegans Aβ1-42 strain and the control. The other C. elegans strains were provided by the Caenorhabditis Genetics Center, which is funded by the NIH Office of Research Infrastructure Programs (P40 OD010440). Human bacterial isolates (listed in Table S1) were obtained through BEI Resources, NIAID, and NIH as part of the Human Microbiome Project. We thank Mark Gorelik for training RB and for assistance with computational analysis. We would like to thank the funders who have supported our work on the bacterial contribution to protein conformational diseases, namely the National Institute on Aging (R03AG070580), and the Infectious Diseases Society of America. Furthermore, we would like to thank the Department of Microbiology and Cell Science for start-up funding. Figure 1 was created using BioRender.com.
Footnotes
Declaration of interests
The authors declare no competing interest.
References
- (1).Soto C. Unfolding the Role of Protein Misfolding in Neurodegenerative Diseases. Nat. Rev. Neurosci. 2003, 4 (1), 49–60. 10.1038/nrn1007. [DOI] [PubMed] [Google Scholar]
- (2).2022 Alzheimer’s Disease Facts and Figures. Alzheimers Dement. J. Alzheimers Assoc. 2022, 18 (4), 700–789. 10.1002/alz.12638. [DOI] [PubMed] [Google Scholar]
- (3).Oliphant K.; Allen-Vercoe E. Macronutrient Metabolism by the Human Gut Microbiome: Major Fermentation by-Products and Their Impact on Host Health. Microbiome 2019, 7 (1), 91. 10.1186/s40168-019-0704-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (4).Clarke G.; Stilling R. M.; Kennedy P. J.; Stanton C.; Cryan J. F.; Dinan T. G. Minireview: Gut Microbiota: The Neglected Endocrine Organ. Mol. Endocrinol. 2014, 28 (8), 1221–1238. 10.1210/me.2014-1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (5).Intili G.; Paladino L.; Rappa F.; Alberti G.; Plicato A.; Calabrò F.; Fucarino A.; Cappello F.; Bucchieri F.; Tomasello G.; Carini F.; Pitruzzella A. From Dysbiosis to Neurodegenerative Diseases through Different Communication Pathways: An Overview. Biology 2023, 12 (2), 195. 10.3390/biology12020195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (6).Fang P.; Kazmi S. A.; Jameson K. G.; Hsiao E. Y. The Microbiome as a Modifier of Neurodegenerative Disease Risk. Cell Host Microbe 2020, 28 (2), 201–222. 10.1016/j.chom.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (7).Jin M.; Li J.; Liu F.; Lyu N.; Wang K.; Wang L.; Liang S.; Tao H.; Zhu B.; Alkasir R. Analysis of the Gut Microflora in Patients With Parkinson’s Disease. Front. Neurosci. 2019, 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (8).Scheperjans F.; Aho V.; Pereira P. A. B.; Koskinen K.; Paulin L.; Pekkonen E.; Haapaniemi E.; Kaakkola S.; Eerola-Rautio J.; Pohja M.; Kinnunen E.; Murros K.; Auvinen P. Gut Microbiota Are Related to Parkinson’s Disease and Clinical Phenotype. Mov. Disord. Off. J. Mov. Disord. Soc. 2015, 30 (3), 350–358. 10.1002/mds.26069. [DOI] [PubMed] [Google Scholar]
- (9).Hertzberg V. S.; Singh H.; Fournier C. N.; Moustafa A.; Polak M.; Kuelbs C. A.; Torralba M. G.; Tansey M. G.; Nelson K. E.; Glass J. D. Gut Microbiome Differences between Amyotrophic Lateral Sclerosis Patients and Spouse Controls. Amyotroph. Lateral Scler. Front. Degener. 2022, 23 (1–2), 91–99. 10.1080/21678421.2021.1904994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (10).Vidal-Martinez G.; Chin B.; Camarillo C.; Herrera G. V.; Yang B.; Sarosiek I.; Perez R. G. A Pilot Microbiota Study in Parkinson’s Disease Patients versus Control Subjects, and Effects of FTY720 and FTY720-Mitoxy Therapies in Parkinsonian and Multiple System Atrophy Mouse Models. J. Park. Dis. 2020, 10 (1), 185–192. 10.3233/JPD-191693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (11).Unger M. M.; Spiegel J.; Dillmann K.-U.; Grundmann D.; Philippeit H.; Bürmann J.; Faßbender K.; Schwiertz A.; Schäfer K.-H. Short Chain Fatty Acids and Gut Microbiota Differ between Patients with Parkinson’s Disease and Age-Matched Controls. Parkinsonism Relat. Disord. 2016, 32, 66–72. 10.1016/j.parkreldis.2016.08.019. [DOI] [PubMed] [Google Scholar]
- (12).Li F.; Wang P.; Chen Z.; Sui X.; Xie X.; Zhang J. Alteration of the Fecal Microbiota in North-Eastern Han Chinese Population with Sporadic Parkinson’s Disease. Neurosci. Lett. 2019, 707, 134297. 10.1016/j.neulet.2019.134297. [DOI] [PubMed] [Google Scholar]
- (13).Bedarf J. R.; Hildebrand F.; Coelho L. P.; Sunagawa S.; Bahram M.; Goeser F.; Bork P.; Wüllner U. Functional Implications of Microbial and Viral Gut Metagenome Changes in Early Stage L-DOPA-Naïve Parkinson’s Disease Patients. Genome Med. 2017, 9 (1), 39. 10.1186/s13073-017-0428-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (14).Aho V. T. E.; Pereira P. A. B.; Voutilainen S.; Paulin L.; Pekkonen E.; Auvinen P.; Scheperjans F. Gut Microbiota in Parkinson’s Disease: Temporal Stability and Relations to Disease Progression. EBioMedicine 2019, 44, 691–707. 10.1016/j.ebiom.2019.05.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (15).Wallen Z. D.; Demirkan A.; Twa G.; Cohen G.; Dean M. N.; Standaert D. G.; Sampson T. R.; Payami H. Metagenomics of Parkinson’s Disease Implicates the Gut Microbiome in Multiple Disease Mechanisms. Nat. Commun. 2022, 13 (1), 6958. 10.1038/s41467-022-34667-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (16).Walker A. C.; Bhargava R.; Vaziriyan-Sani A. S.; Pourciau C.; Donahue E. T.; Dove A. S.; Gebhardt M. J.; Ellward G. L.; Romeo T.; Czyż D. M. Colonization of the Caenorhabditis Elegans Gut with Human Enteric Bacterial Pathogens Leads to Proteostasis Disruption That Is Rescued by Butyrate. PLOS Pathog. 2021, 17 (5), e1009510. 10.1371/journal.ppat.1009510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (17).Walker A. C.; Bhargava R.; Brust A. S.; Owji A. A.; Czyż D. M. Time-off-Pick Assay to Measure Caenorhabditis Elegans Motility. Bio-Protoc. 2022, 12 (12), e4436. 10.21769/BioProtoc.4436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (18).Bodhicharla R.; Nagarajan A.; Winter J.; Adenle A.; Nazir A.; Brady D.; Vere K.; Richens J.; O’Shea P.; Bell D. R.; de Pomerai D. Effects of α-Synuclein Overexpression in Transgenic Caenorhabditis Elegans Strains. CNS Neurol. Disord. Drug Targets 2012, 11 (8), 965–975. 10.2174/1871527311211080005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (19).Ham T. J. van; Thijssen K. L.; Breitling R.; Hofstra R. M. W.; Plasterk R. H. A.; Nollen E. A. A. C. Elegans Model Identifies Genetic Modifiers of α-Synuclein Inclusion Formation During Aging. PLOS Genet. 2008, 4 (3), e1000027. 10.1371/journal.pgen.1000027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (20).Gallrein C.; Iburg M.; Michelberger T.; Koçak A.; Puchkov D.; Liu F.; Ayala Mariscal S. M.; Nayak T.; Kaminski Schierle G. S.; Kirstein J. Novel Amyloid-Beta Pathology C. Elegans Model Reveals Distinct Neurons as Seeds of Pathogenicity. Prog. Neurobiol. 2021, 198, 101907. 10.1016/j.pneurobio.2020.101907. [DOI] [PubMed] [Google Scholar]
- (21).Morley J. F.; Brignull H. R.; Weyers J. J.; Morimoto R. I. The Threshold for Polyglutamine-Expansion Protein Aggregation and Cellular Toxicity Is Dynamic and Influenced by Aging in Caenorhabditis Elegans. Proc. Natl. Acad. Sci. U. S. A. 2002, 99 (16), 10417–10422. 10.1073/pnas.152161099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (22).Taylor R. C.; Dillin A. Aging as an Event of Proteostasis Collapse. Cold Spring Harb. Perspect. Biol. 2011, 3 (5), a004440. 10.1101/cshperspect.a004440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (23).Walker A. C.; Bhargava R.; Dove A. S.; Brust A. S.; Owji A. A.; Czyż D. M.. Bacteria-Derived Protein Aggregates Contribute to the Disruption of Host Proteostasis. Int. J. Mol. Sci. 2022, 23 (9), 4807. 10.3390/ijms23094807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (24).Ben-Zvi A.; Miller E. A.; Morimoto R. I. Collapse of Proteostasis Represents an Early Molecular Event in Caenorhabditis Elegans Aging. Proc. Natl. Acad. Sci. U. S. A. 2009, 106 (35), 14914–14919. 10.1073/pnas.0902882106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (25).Macleod A. R.; Waterston R. H.; Fishpool R. M.; Brenner S. Identification of the Structural Gene for a Myosin Heavy-Chain in Caenorhabditis Elegans. J. Mol. Biol. 1977, 114 (1), 133–140. 10.1016/0022-2836(77)90287-X. [DOI] [PubMed] [Google Scholar]
- (26).Labbadia J.; Morimoto R. I. Proteostasis and Longevity: When Does Aging Really Begin? F1000Prime Rep. 2014, 6, 7. 10.12703/P6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (27).Tansey M. G.; Wallings R. L.; Houser M. C.; Herrick M. K.; Keating C. E.; Joers V. Inflammation and Immune Dysfunction in Parkinson Disease. Nat. Rev. Immunol. 2022, 22 (11), 657–673. 10.1038/s41577-022-00684-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (28).Walker A.; Czyz D. M. Oh My Gut! Is the Microbial Origin of Neurodegenerative Diseases Real? Infect. Immun. 2023, e0043722. 10.1128/iai.00437-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (29).Sweeney P.; Park H.; Baumann M.; Dunlop J.; Frydman J.; Kopito R.; McCampbell A.; Leblanc G.; Venkateswaran A.; Nurmi A.; Hodgson R. Protein Misfolding in Neurodegenerative Diseases: Implications and Strategies. Transl. Neurodegener. 2017, 6. 10.1186/s40035-017-0077-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (30).Mullane K.; Williams M. Preclinical Models of Alzheimer’s Disease: Relevance and Translational Validity. Curr. Protoc. Pharmacol. 2019, 84 (1), e57. 10.1002/cpph.57. [DOI] [PubMed] [Google Scholar]
- (31).Savica R.; Carlin J. M.; Grossardt B. R.; Bower J. H.; Ahlskog J. E.; Maraganore D. M.; Bharucha A. E.; Rocca W. A. Medical Records Documentation of Constipation Preceding Parkinson Disease. Neurology 2009, 73 (21), 1752–1758. 10.1212/WNL.0b013e3181c34af5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (32).Ferreiro A. L.; Choi J.; Ryou J.; Newcomer E. P.; Thompson R.; Bollinger R. M.; Hall-Moore C.; Ndao I. M.; Sax L.; Benzinger T. L. S.; Stark S. L.; Holtzman D. M.; Fagan A. M.; Schindler S. E.; Cruchaga C.; Butt O. H.; Morris J. C.; Tarr P. I.; Ances B. M.; Dantas G. Gut Microbiome Composition May Be an Indicator of Preclinical Alzheimer’s Disease. Sci. Transl. Med. 2023, 15 (700), eabo2984. 10.1126/scitranslmed.abo2984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (33).Tseng C.-S.; Chao Y.-W.; Liu Y.-H.; Huang Y.-S.; Chao H.-W. Dysregulated Proteostasis Network in Neuronal Diseases. Front. Cell Dev. Biol. 2023, 11, 1075215. 10.3389/fcell.2023.1075215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (34).Chang Y.-P.; Chiu G.-F.; Kuo F.-C.; Lai C.-L.; Yang Y.-H.; Hu H.-M.; Chang P.-Y.; Chen C.-Y.; Wu D.-C.; Yu F.-J. Eradication of Helicobacter pylori Is Associated with the Progression of Dementia: A Population-Based Study. Gastroenterology Research and Practice. 10.1155/2013/175729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (35).Kountouras J.; Boziki M.; Gavalas E.; Zavos C.; Grigoriadis N.; Deretzi G.; Tzilves D.; Katsinelos P.; Tsolaki M.; Chatzopoulos D.; Venizelos I. Eradication of Helicobacter Pylori May Be Beneficial in the Management of Alzheimer’s Disease. J. Neurol. 2009, 256 (5), 758–767. 10.1007/s00415-009-5011-z. [DOI] [PubMed] [Google Scholar]
- (36).Elvers K. T.; Wilson V. J.; Hammond A.; Duncan L.; Huntley A. L.; Hay A. D.; Werf E. T. van der. Antibiotic-Induced Changes in the Human Gut Microbiota for the Most Commonly Prescribed Antibiotics in Primary Care in the UK: A Systematic Review. BMJ Open 2020, 10 (9), e035677. 10.1136/bmjopen-2019-035677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (37).Sun J.; Zhan Y.; Mariosa D.; Larsson H.; Almqvist C.; Ingre C.; Zagai U.; Pawitan Y.; Fang F. Antibiotics Use and Risk of Amyotrophic Lateral Sclerosis in Sweden. Eur. J. Neurol. 2019, 26 (11), 1355–1361. 10.1111/ene.13986. [DOI] [PubMed] [Google Scholar]
- (38).Mertsalmi T. H.; Pekkonen E.; Scheperjans F. Antibiotic Exposure and Risk of Parkinson’s Disease in Finland: A Nationwide Case-Control Study. Mov. Disord. 2020, 35 (3), 431–442. 10.1002/mds.27924. [DOI] [PubMed] [Google Scholar]
- (39).Goodwin C. S.; Armstrong J. A. Microbiological Aspects ofHelicobacter Pylori (Campylobacter Pylori). Eur. J. Clin. Microbiol. Infect. Dis. 1990, 9 (1), 1–13. 10.1007/BF01969526. [DOI] [PubMed] [Google Scholar]
- (40).Iino C.; Shimoyama T. Impact of Helicobacter Pylori Infection on Gut Microbiota. World J. Gastroenterol. 2021, 27 (37), 6224–6230. 10.3748/wjg.v27.i37.6224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (41).Grabrucker S.; Marizzoni M.; Silajdži E.; Lopizzo N.; Mombelli E.; Nicolas S.; Dohm-Hansen S.; Scassellati C.; Moretti D. V.; Rosa M.; Hoffmann K.; Cryan J. F.; O’Leary O. F.; English J. A.; Lavelle A.; O’Neill C.; Thuret S.; Cattaneo A.; Nolan Y. M. Microbiota from Alzheimer’s Patients Induce Deficits in Cognition and Hippocampal Neurogenesis. Brain 2023, awad303. 10.1093/brain/awad303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (42).Tett A.; Pasolli E.; Masetti G.; Ercolini D.; Segata N. Prevotella Diversity, Niches and Interactions with the Human Host. Nat. Rev. Microbiol. 2021, 19 (9), 585–599. 10.1038/s41579-021-00559-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (43).Summanen P. H.; Talan D. A.; Strong C.; McTeague M.; Bennion R.; Thompson J. E. Jr.; Väisänen M.-L.; Moran G.; Winer M.; Finegold S. M. Bacteriology of Skin and Soft-Tissue Infections: Comparison of Infections in Intravenous Drug Users and Individuals with No History of Intravenous Drug Use. Clin. Infect. Dis. 1995, 20 (Supplement_2), S279–S282. 10.1093/clinids/20.Supplement_2.S279. [DOI] [PubMed] [Google Scholar]
- (44).Civen R.; Jousimies-Somer H.; Marina M.; Borenstein L.; Shah H.; Finegold S. M. A Retrospective Review of Cases of Anaerobic Empyema and Update of Bacteriology. Clin. Infect. Dis. 1995, 20, S224–S229. [DOI] [PubMed] [Google Scholar]
- (45).Socransky S. s.; Haffajee A. d.; Cugini M. a.; Smith C.; Kent R. L. Jr. Microbial Complexes in Subgingival Plaque. J. Clin. Periodontol. 1998, 25 (2), 134–144. 10.1111/j.1600-051X.1998.tb02419.x. [DOI] [PubMed] [Google Scholar]
- (46).Kim S.-J.; Choi E.-Y.; Kim E. G.; Shin S.-H.; Lee J.-Y.; Choi J.-I.; Choi I.-S. Prevotella Intermedia Lipopolysaccharide Stimulates Release of Tumor Necrosis Factor-α through Mitogen-Activated Protein Kinase Signaling Pathways in Monocyte-Derived Macrophages. FEMS Immunol. Med. Microbiol. 2007, 51 (2), 407–413. 10.1111/j.1574-695X.2007.00318.x. [DOI] [PubMed] [Google Scholar]
- (47).Xu P.; Shao R.; Zhang S.; Tan Z.; Guo Y.; He Y. The Mechanism on Prevotella Melaninogenica Promoting the Inflammatory Progression of Oral Lichen Planus. Clin. Exp. Immunol. 2022, 209 (2), 215. 10.1093/cei/uxac054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (48).Marietta E. V.; Murray J. A.; Luckey D. H.; Jeraldo P. R.; Lamba A.; Patel R.; Luthra H. S.; Mangalam A.; Taneja V. Human Gut-Derived Prevotella Histicola Suppresses Inflammatory Arthritis in Humanized Mice. Arthritis Rheumatol. Hoboken NJ 2016, 68 (12), 2878. 10.1002/art.39785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (49).Larsen J. M. The Immune Response to Prevotella Bacteria in Chronic Inflammatory Disease. Immunology 2017, 151 (4), 363. 10.1111/imm.12760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (50).Beydoun M. A.; Beydoun H. A.; Hossain S.; El-Hajj Z. W.; Weiss J.; Zonderman A. B. Clinical and Bacterial Markers of Periodontitis and Their Association with Incident All-Cause and Alzheimer’s Disease Dementia in a Large National Survey. J. Alzheimers Dis. 2020, 75 (1), 157–172. 10.3233/JAD-200064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (51).Ilhan Z. E.; Łaniewski P.; Tonachio A.; Herbst-Kralovetz M. M. Members of Prevotella Genus Distinctively Modulate Innate Immune and Barrier Functions in a Human Three-Dimensional Endometrial Epithelial Cell Model. J. Infect. Dis. 2020, 222 (12), 2082–2092. 10.1093/infdis/jiaa324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (52).Mack D. R.; Michail S.; Wei S.; McDougall L.; Hollingsworth M. A. Probiotics Inhibit Enteropathogenic E. Coli Adherence in Vitro by Inducing Intestinal Mucin Gene Expression. Am. J. Physiol. 1999, 276 (4), G941–950. 10.1152/ajpgi.1999.276.4.G941. [DOI] [PubMed] [Google Scholar]
- (53).Pothuraju R.; Pai P.; Chaudhary S.; Siddiqui J. A.; Cox J. L.; Kaur S.; Rachagani S.; Roy H. K.; Bouvet M.; Batra S. K. Depletion of Transmembrane Mucin 4 (Muc4) Alters Intestinal Homeostasis in a Genetically Engineered Mouse Model of Colorectal Cancer. Aging 2022, 14 (5), 2025–2046. 10.18632/aging.203935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (54).Seguella L.; Sarnelli G.; Esposito G. Leaky Gut, Dysbiosis, and Enteric Glia Activation: The Trilogy behind the Intestinal Origin of Parkinson’s Disease. Neural Regen. Res. 2019, 15 (6), 1037–1038. 10.4103/1673-5374.270308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (55).Obrenovich M. E. M. Leaky Gut, Leaky Brain? Microorganisms 2018, 6 (4). 10.3390/microorganisms6040107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (56).Mu Q.; Kirby J.; Reilly C. M.; Luo X. M. Leaky Gut As a Danger Signal for Autoimmune Diseases. Front. Immunol. 2017, 8, 598. 10.3389/fimmu.2017.00598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (57).Haran J. P.; Bhattarai S. K.; Foley S. E.; Dutta P.; Ward D. V.; Bucci V.; McCormick B. A. Alzheimer’s Disease Microbiome Is Associated with Dysregulation of the Anti-Inflammatory P-Glycoprotein Pathway. mBio 2019, 10 (3). 10.1128/mBio.00632-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (58).Kaiyrlykyzy A.; Kozhakhmetov S.; Babenko D.; Zholdasbekova G.; Alzhanova D.; Olzhayev F.; Baibulatova A.; Kushugulova A. R.; Askarova S. Study of Gut Microbiota Alterations in Alzheimer’s Dementia Patients from Kazakhstan. Sci. Rep. 2022, 12, 15115. 10.1038/s41598-022-19393-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (59).Keshavarzian A.; Green S. J.; Engen P. A.; Voigt R. M.; Naqib A.; Forsyth C. B.; Mutlu E.; Shannon K. M. Colonic Bacterial Composition in Parkinson’s Disease. Mov. Disord. Off. J. Mov. Disord. Soc. 2015, 30 (10), 1351–1360. 10.1002/mds.26307. [DOI] [PubMed] [Google Scholar]
- (60).Ragusa M.; Santagati M.; Mirabella F.; Lauretta G.; Cirnigliaro M.; Brex D.; Barbagallo C.; Domini C. N.; Gulisano M.; Barone R.; Trovato L.; Oliveri S.; Mongelli G.; Spitale A.; Barbagallo D.; Di Pietro C.; Stefani S.; Rizzo R.; Purrello M. Potential Associations Among Alteration of Salivary miRNAs, Saliva Microbiome Structure, and Cognitive Impairments in Autistic Children. Int. J. Mol. Sci. 2020, 21 (17), 6203. 10.3390/ijms21176203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (61).Atkin T. A.; Brandon N. J.; Kittler J. T. Disrupted in Schizophrenia 1 Forms Pathological Aggresomes That Disrupt Its Function in Intracellular Transport. Hum. Mol. Genet. 2012, 21 (9), 2017–2028. 10.1093/hmg/dds018. [DOI] [PubMed] [Google Scholar]
- (62).Fujita E.; Dai H.; Tanabe Y.; Zhiling Y.; Yamagata T.; Miyakawa T.; Tanokura M.; Momoi M. Y.; Momoi T. Autism Spectrum Disorder Is Related to Endoplasmic Reticulum Stress Induced by Mutations in the Synaptic Cell Adhesion Molecule, CADM1. Cell Death Dis. 2010, 1 (6), e47–e47. 10.1038/cddis.2010.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (63).Jaco A. D.; Lin M. Z.; Dubi N.; Comoletti D.; Miller M. T.; Camp S.; Ellisman M.; Butko M. T.; Tsien R. Y.; Taylor P. Neuroligin Trafficking Deficiencies Arising from Mutations in theα/β-Hydrolase Fold Protein Family *. J. Biol. Chem. 2010, 285 (37), 28674–28682. 10.1074/jbc.M110.139519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (64).J ko H.; Cie lik M.; Gromadzka G.; Adamczyk A. Dysfunctional Proteins in Neuropsychiatric Disorders: From Neurodegeneration to Autism Spectrum Disorders. Neurochem. Int. 2020, 141, 104853. 10.1016/j.neuint.2020.104853. [DOI] [PubMed] [Google Scholar]
- (65).De Angelis M.; Piccolo M.; Vannini L.; Siragusa S.; De Giacomo A.; Serrazzanetti D. I.; Cristofori F.; Guerzoni M. E.; Gobbetti M.; Francavilla R. Fecal Microbiota and Metabolome of Children with Autism and Pervasive Developmental Disorder Not Otherwise Specified. PLoS ONE 2013, 8 (10), e76993. 10.1371/journal.pone.0076993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (66).Taniya M. A.; Chung H.-J.; Al Mamun A.; Alam S.; Aziz Md. A.; Emon N. U.; Islam Md. M.; Hong S.-T. shool; Podder B. R.; Ara Mimi A.; Aktar Suchi S.; Xiao J. Role of Gut Microbiome in Autism Spectrum Disorder and Its Therapeutic Regulation. Front. Cell. Infect. Microbiol. 2022, 12, 915701. 10.3389/fcimb.2022.915701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (67).Gabrielaite M.; Bartell J. A.; Nørskov-Lauritsen N.; Pressler T.; Nielsen F. C.; Johansen H. K.; Marvig R. L. Transmission and Antibiotic Resistance of Achromobacter in Cystic Fibrosis. J. Clin. Microbiol. 2021, 59 (4), 10.1128/jcm.02911–20. 10.1128/jcm.02911-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (68).Veschetti L.; Boaretti M.; Saitta G. M.; Passarelli Mantovani R.; Lleò M. M.; Sandri A.; Malerba G. Achromobacter Spp. Prevalence and Adaptation in Cystic Fibrosis Lung Infection. Microbiol. Res. 2022, 263, 127140. 10.1016/j.micres.2022.127140. [DOI] [PubMed] [Google Scholar]
- (69).Marsac C.; Berdah L.; Thouvenin G.; Sermet-Gaudelus I.; Corvol H. Achromobacter Xylosoxidans Airway Infection Is Associated with Lung Disease Severity in Children with Cystic Fibrosis. ERJ Open Res. 2021, 7 (2), 00076–02021. 10.1183/23120541.00076-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (70).Bhagirath A. Y.; Li Y.; Somayajula D.; Dadashi M.; Badr S.; Duan K. Cystic Fibrosis Lung Environment and Pseudomonas Aeruginosa Infection. BMC Pulm. Med. 2016, 16, 174. 10.1186/s12890-016-0339-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (71).Xi J.; Ding D.; Zhu H.; Wang R.; Su F.; Wu W.; Xiao Z.; Liang X.; Zhao Q.; Hong Z.; Fu H.; Xiao Q. Disturbed Microbial Ecology in Alzheimer’s Disease: Evidence from the Gut Microbiota and Fecal Metabolome. BMC Microbiol. 2021, 21, 226. 10.1186/s12866-021-02286-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (72).Deng P.; Uma Naresh N.; Du Y.; Lamech L. T.; Yu J.; Zhu L. J.; Pukkila-Worley R.; Haynes C. M. Mitochondrial UPR Repression during Pseudomonas Aeruginosa Infection Requires the bZIP Protein ZIP-3. Proc. Natl. Acad. Sci. U. S. A. 2019, 116 (13), 6146–6151. 10.1073/pnas.1817259116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (73).Haeussler S.; Conradt B. Methods to Study the Mitochondrial Unfolded Protein Response (UPRmt) in Caenorhabditis Elegans. Methods Mol. Biol. Clifton NJ 2022, 2378, 249–259. 10.1007/978-1-0716-1732-8_16. [DOI] [PubMed] [Google Scholar]
- (74).Haynes C. M.; Ron D. The Mitochondrial UPR – Protecting Organelle Protein Homeostasis. J. Cell Sci. 2010, 123 (22), 3849–3855. 10.1242/jcs.075119. [DOI] [PubMed] [Google Scholar]
- (75).Javed I.; Zhang Z.; Adamcik J.; Andrikopoulos N.; Li Y.; Otzen D. E.; Lin S.; Mezzenga R.; Davis T. P.; Ding F.; Ke P. C. Accelerated Amyloid Beta Pathogenesis by Bacterial Amyloid FapC. Adv. Sci. 2020, 7 (18), 2001299. 10.1002/advs.202001299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (76).Dueholm M. S.; Otzen D.; Nielsen P. H. Evolutionary Insight into the Functional Amyloids of the Pseudomonads. PLOS ONE 2013, 8 (10), e76630. 10.1371/journal.pone.0076630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (77).Isler B.; Kidd T. J.; Stewart A. G.; Harris P.; Paterson D. L. Achromobacter Infections and Treatment Options. Antimicrob. Agents Chemother. 2020, 64 (11), e01025–20. 10.1128/AAC.01025-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (78).Chen S. G.; Stribinskis V.; Rane M. J.; Demuth D. R.; Gozal E.; Roberts A. M.; Jagadapillai R.; Liu R.; Choe K.; Shivakumar B.; Son F.; Jin S.; Kerber R.; Adame A.; Masliah E.; Friedland R. P. Exposure to the Functional Bacterial Amyloid Protein Curli Enhances Alpha-Synuclein Aggregation in Aged Fischer 344 Rats and Caenorhabditis Elegans. Sci. Rep. 2016, 6 (1), 34477. 10.1038/srep34477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (79).Bieler S.; Estrada L.; Lagos R.; Baeza M.; Castilla J.; Soto C. Amyloid Formation Modulates the Biological Activity of a Bacterial Protein. J. Biol. Chem. 2005, 280 (29), 26880–26885. 10.1074/jbc.M502031200. [DOI] [PubMed] [Google Scholar]
- (80).Gidalevitz T.; Ben-Zvi A.; Ho K. H.; Brignull H. R.; Morimoto R. I. Progressive Disruption of Cellular Protein Folding in Models of Polyglutamine Diseases. Science 2006, 311 (5766), 1471–1474. 10.1126/science.1124514. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Data used to generate Figure 2. “Western” indicates the band intensity of the polyQ insoluble fraction of worms fed indicated bacteria normalized to those fed E. coli OP50 control. “Count” indicates the average number of aggregates per worm of worms fed indicated bacteria normalized to those fed E. coli OP50 control. Parenthesized numbers (1–5) reflect the remaining conditions in which bacteria were grown:1) anaerobically in reinforced clostridial broth (RCB) with Oxyrase, 2) facultative conditions (no shaking, tube filled to top) in brain heart infusion broth (BHI), 3) aerobic conditions, shaking at 220 revolutions per minute (RPM) in BHI, 4) anaerobic conditions on tryptic soy agar (TSA) supplemented with 5% defibrinated sheep’s blood, 5) aerobic conditions on TSA supplemented with 5% defibrinated sheep’s blood.
Fig. S1. The robust effect of bacteria on the aggregation of Aβ1–42 correlates with aggregate-dependent changes in motility. (A) Nomarski and fluorescent images (mScarlet) and the corresponding (B) TOP motility measurements of transgenic worms expressing muscle-specific Aβ1–42 fed a proteoprotective strain (P. corporis) and a proteotoxic strain (P. aeruginosa). Each TOP data point is representative of the average of three independent experiments for a total of 30 worms. Error bars represent SEM. Statistical significance was calculated using one-way analysis of variants (ANOVA) followed by multiple comparison Dunnett’s post-hoc test (*p<0.05, **p<0.01, ***p<0.001). Scale bar is 100 μm.
Fig. S2. Aggregate-dependent toxicity in transgenic animals harboring Aβ1–42 and α-synuclein is age-dependent. Age-dependent changes in the motility of animals expressing muscle-specific (A) Aβ1–42 and (B) α-synuclein and corresponding control animals: empty vector (No Aβ) and wild-type N2 (WT). Data are represented as the average TOP (seconds) per worm. Each data point is representative of two independent experiments for a total of 20 worms. Error bars represent SEM. Statistical significance was calculated using one-way analysis of variants (ANOVA) followed by multiple comparison Dunnett’s post-hoc test (***p<0.001, ****p<0.0001).
Figure S3. P. corporis prevents temperature-dependent motility defect. Temperature-dependent changes in the motility of animals expressing a muscle-specific mutation in the myosin heavy-chain gene (e1301). Data are represented as the average TOP (seconds) per worm. Each data point is representative of three independent experiments for a total of 30 worms. Error bars represent SEM. Statistical significance was calculated using one-way analysis of variants (ANOVA) followed by multiple comparison Dunnett’s post-hoc test (****p<0.0001).
Figure S4. Phylogenetic grouping reflects the effect of bacteria on host proteostasis. Phylogenetic tree shows that proteotoxic bacteria predominantly cluster together, separate from proteoprotective bacteria which also form their own distinct cluster. The size of the bacterial identifiers is proportional to the magnitude of their respective proteotoxic or proteoprotective effects. Proteoprotective bacteria are indicated in blue, and proteotoxic bacteria in red. Tree analysis was performed on a large collection of human microbiome isolates in BV-BRC using maximum likelihood based on concatenated alignments of 100 single-copy genes.