Abstract
Background:
Heightened risks of cognitive impairment, disability, and barriers to care among sexual and gender minority (SGM) older adults are well documented. To date, culturally responsive evidence-based dementia interventions for this population do not exist.
Objective:
This study describes the design of the first randomized controlled trial (RCT) testing a culturally responsive cognitive behavioral and empowerment intervention, Innovations in Dementia Empowerment and Action (IDEA), developed to address the unique needs of SGM older adults living with dementia and care partners.
Methods:
IDEA is a culturally enhanced version of Reducing Disability in Alzheimer’s Disease (RDAD), an efficacious, non-pharmaceutical intervention for people with dementia and care partners. We utilized a staggered multiple baseline design with the goal to enroll 150 dyads randomized into two arms of 75 dyads each, enhanced IDEA and standard RDAD.
Results:
IDEA was adapted using findings from the longitudinal National Health, Aging, and Sexuality/Gender study, which identified modifiable factors for SGM older adults, including SGM-specific discrimination and stigma, health behaviors, and support networks. The adapted intervention employed the original RDAD strategies and enhanced them with culturally responsive empowerment practices designed to cultivate engagement, efficacy, and support mobilization. Outcomes include adherence to physical activity, reduction in perceived stress and stigma, and increased physical functioning, efficacy, social support, engagement, and resource use.
Conclusion:
IDEA addresses contemporary issues for underserved populations living with dementia and their care partners. Our findings will have important implications for marginalized communities by integrating and evaluating the importance of cultural responsiveness in dementia and caregiving interventions.
Keywords: Alzheimer’s disease, Underserved populations, LGBT, RDAD, IDEA, Cultural diversity
1. Background
By 2050, Alzheimer’s disease and related dementias will affect an estimated 13.8 million Americans, with associated annual costs estimated at $355 billion [1]. Sexual and gender minorities1 (SGM) comprise 2.4% of the U.S. population aged 50 and older [2,3], and by 2050 the total number of SGM individuals is predicted to double in size to approximately 7 million [2]. Within the SGM older adult population, it is likely 400,000 SGM older adults currently experience dementia, and by 2050 this is expected to increase to more than 735,000 SGM older adults, with associated annual care costs of $17 billion [4]. In the general population, cost (70%) of lifetime care is generally borne by more than 16 million family and other unpaid care partners in the form of unpaid caregiving and out-of-pocket expenses [5], with recent estimates valuing this care at $244 billion annually [6].
Nearly one-third (31%) of SGM older adults provide informal care to a partner, friend, or family member, with an estimated 840,000 SGM care partners, including about 125,000 care partners assisting community members living with dementia [7], many of whom are older adults themselves. Compared to heterosexuals, SGM care partners are more often age cohort peers, and they are more likely to be ‘families of choice’ or friends with whom they have no biological or legal relationship [7–10]. Research from Aging with Pride: National Health, Aging, and Sexuality/Gender Study (NHAS), identified 62.5% of SGM care partners were providing care to someone other than a partner or spouse, including 29% to friends and 7% to an ex-partner or spouse [7,10]. These care partners experience both psychological and physical health-related quality of life (QoL) declines over time, especially those who are older and physically inactive [4,10]. Among SGM care partners, micro-aggressions are associated with poorer quality of life and microaggressions and day-to-day discrimination with higher levels of depressive symptoms [11]; lifetime victimization is associated with higher perceived stress [7]; and SGM community engagement and social support with lower perceived stress [7]. There are also differences among SGM care partner sub-groups, with bisexual, queer, African American/Black, and other racial minorities reporting more adverse psychosocial outcomes and transgender care partners more positive outcomes [11]. SGM care partners also report barriers to receiving support, including a lack of representation in services, negative attitudes of care staff, and a reluctance to seek support [12].
Compared to their heterosexual age peers, SGM older adults evidence poorer physical and mental health outcomes [2,13]; higher rates of disability and functional limitations [14]; and more risk factors associated with dementia, including HIV/AIDS, smoking, depression, and social isolation [2,13,15]. SGM older adults are significantly more likely to report subjective cognitive impairment (24.5%) than heterosexuals (19.1%) [16]; increased risk for cognitive impairment and higher incidence of subjective cognitive decline [17,18], and to report their cognitive impairment as severe and frequent [16].
Despite the disparities in cognitive health among SGM populations [16], they are rarely included in dementia research, interventions, or services [19,20]. Yet, SGM older adults living with dementia or cognitive decline and their care partners face substantial barriers in accessing culturally relevant dementia care and services. They are less likely to benefit from formal services because of providers’ explicit and implicit bias [19,20]. Fear of accessing or utilizing services due to stigma among SGM older adults also creates difficulty in securing services and support [20]. Experiences of discrimination and stigma across the lifespan often require ongoing identity management strategies, such as not seeking services and/or hiding SGM identities and relationships in contexts they perceive as unsafe to disclose, potentially blocking access to needed resources. Cognitive decline itself may increase SGM older adults’ stress and reluctance to utilize care services. As such, the centrality of informal caregiving for this population may be even greater than in the general population.
The lack of efficacious, research-based interventions for vulnerable and underserved older adults living with dementia and their care partners, including SGM populations, is a significant public health problem. It is critically urgent to translate evidence-based interventions [21,22] that address unique characteristics and experiences of SGM older adults living with dementia and their care partners. In this paper we describe the design and development of the first innovative RCT developed to address the distinct risks and barriers facing SGM older adults living with dementia and their care partners, the Innovations in Dementia Empowerment and Action (IDEA) intervention.
1.1. Innovation
To better serve SGM older adults living with dementia and their care partners, we developed a culturally specialized approach based on findings from the first of its kind longitudinal study, NHAS [3]. Results suggested that for SGM older adults living with cognitive impairment, modifiable health promoting pathways include SGM-specific discrimination, identity stigma, health behaviors (e.g. physical activity, outdoor leisure activity, optimal sleep, and food intake), and support networks [23]. Incorporating these modifiable factors, we built upon an efficacious dementia intervention, Reducing Disability in Alzheimer’s Disease (RDAD) [24–26], designed to increase physical activity and problem-solving by engaging persons living with dementia and their caregivers. Evaluated in an RCT, RDAD findings have been peer-reviewed and published in highly-regarded scientific journals [27,28], and it is included as a model program in the Administration on Aging Evidence-Based Intervention Grants Program [29]. The RDAD program contains many of the characteristics identified in the literature as essential to translation [30,31], including a well-developed assessment and training protocol with a trainer manual, structured session-by-session outlines, and participant materials.
1.2. Conceptual framework
The IDEA intervention is informed by the Health Equity Promotion Model (HEPM) [32] guiding the NHAS study. The HEPM explicates SGM health and well-being by conceptualizing the: “a) heterogeneity and intersectionality within… [SGM] communities; (b) the influence of structural and environmental context; and (c) both health-promoting and adverse pathways that encompass behavioral, social, psychological, and biological processes…. by integrating a life course development perspective within the health-promotion model” (p. 653). We employ this framework to understand specific risk and protective factors in underserved populations that may be associated with both dementia and caregiving, as they may hamper or enhance intervention engagement, delivery, and retention. The HEPM also informs how healthcare access in underserved populations is shaped by multidimensional processes, including the components outlined above [33]. We combined HEPM principles with the theories and strategies underlying RDAD. Social-learning [34] and cognitive behavioral strategies [26] within RDAD include modeling and observation, as well as goal-setting, self-monitoring, problem solving, and reinforcement. This theoretical grounding was not originally tailored for SGM populations; therefore, we enhanced the intervention through the integration of the HEPM and the application of motivational interviewing (MI) to explicitly include goal-setting and problem-solving around SGM-specific health care access and unique concerns such as barriers due to exposure to implicit and explicit bias [26,35] and histories of trauma [36,37] to reduce stress for the person living with dementia and their care partner.
2. Methods
2.1. Study aims and design
The purpose of this RCT is to design and develop a culturally responsive multidimensional intervention designed specifically for SGM persons living with dementia and their care partners to enhance their physical functioning, social engagement, and QoL. The primary aims of the RTC are threefold: to 1) test short- and long-term effects of enhanced IDEA, comparing it to the standard intervention RDAD on primary and secondary outcomes for SGM older adults and their care partners; 2) evaluate intervention adherence; and 3) test whether the effects of enhanced IDEA and the standard RDAD differ by subgroups. The current study is a 2-arm (enhanced IDEA & standard RDAD), single-blind, RCT using a staggered multiple baseline design [38], approved by the University’s Institutional Review Board.
2.2. Sample size estimation
Based on a previous study [28], we ran a series of power analyses (2-sided) aimed at detecting differences in outcome variables and taking into consideration interaction terms to determine the size of our smallest sub-sample. For the equal subgroup size by intervention condition, we based power calculations on mixed-effects models with individual random intercepts and slopes that accounted for heterogeneity in baseline outcome variables, and changes in outcome variables among individuals, adjusting for key covariates and applying the Bonferroni correction to control for error rates associated with multiple tests. To detect a small effect (d = 0.25), which is greater than a minimal clinically important difference level [39], assuming statistical power of 0.8 and significance level of 0.05, the estimated sample size was 52 dyads in each group (104 dyads total). Adjusting the sample size up to account for the projected 25% attrition over two years indicated a total sample to recruit of 150 dyads.
2.3. Participants and recruitment procedures
In this RCT study, participants are recruited from multiple sources using a multifaceted approach, including direct referrals from community agencies providing aging and health services using presentations, flyers, newsletters, and social media. Study staff facilitate meetings for community agencies that serve older adults as well as those that serve SGM individuals, making all recruitment materials available to them. Emails with the study website, flyer, and ready-made social media posts are also sent to community agencies.
2.4. Eligibility requirements (Table 1)
Table 1.
Eligibility criteria.
| Criteria | Care Recipient | Care Partner | |
|---|---|---|---|
| Inclusion Criteria | • Either the person living with dementia, or the care partner must self-identify as SGM or sexual or gender diverse, OR have had a romantic relationship with, or attraction to someone of the same sex or gender, or engaged in same-sex behavior. | Either care partner OR care recipient | |
| • 50 years of age or older at enrollment | √ | ||
| • Has Alzheimer’s disease or other dementia. Or meets the definition of dementia suggested by scientific literature, which is determined 1) by asking care partner the current diagnostic status of care recipient or 2) by asking whether care recipient has any difficulties in the domains of dementia AND needs any help in daily activities | √ | ||
| • Living in the community (not in a long-term care facility receiving nursing home skilled level of care) | √ | √ | |
| • Willing to spend at least 30 min per day for study activities or willing to coordinate others to assist | √ | ||
| • Providing care or assistance to the care recipient | √ | ||
| Exclusion Criteria | • Plans to move to a long-term care setting for skilled nursing care within 6 months of enrollment | √ | √ |
| • Known terminal illness (with death anticipated within the next 12 months) | √ | √ | |
| • Psychiatric disorder in the 12 months prior to baseline | √ | √ | |
| • Currently suicidal | √ | √ | |
| • Major hallucinations or delusions | √ | √ | |
| • Physical limitations/chronic conditions preventing participation in a low impact exercise program and the exercise program can’t be modified for the person to participate | √ | √ | |
| • Currently engaged in more than 150 min a week of moderate physical activity or regularly participates in a formal exercise program | √ | √ | |
| • Is not a paid care partner or a volunteer affiliated with a service organization | √ | ||
As a dyadic study, both the person living with dementia and their care partner participate. The care partner is the person designated by the person living with dementia as the informal helper who assists most with daily needs, is not paid, and is not a volunteer affiliated with a service organization. Either the person living with dementia, or the care partner must self-identify as SGM or sexual or gender diverse, OR have had a romantic relationship with, or attraction to someone of the same sex or gender, or engaged in same-sex behavior. The person living with dementia must be at least 50 years of age and have dementia, based on the definition suggested by scientific literature [40,41], determined 1) by asking the care partner the current diagnostic status of the person living with dementia, or 2) by asking the care partner whether the person living with dementia has any difficulties in dementia domains AND needs help in everyday activities. This method has two key aspects: (1) it precludes considerable increased costs that would be necessitated by obtaining a physical exam and (2) avoids unnecessary delays (and potential the loss of participants) needed to schedule an exam or wait for receipt of patient charts. The care partner must be willing to spend at least 30 min per day for study activities or be willing to coordinate with others to assist the person living with dementia.
Exclusion criteria for the person living with dementia or the care partner include a) residing in a nursing home or long-term care facility or having plans to move to one within six months of enrollment; b) known terminal illness; c) hospitalization due to a psychiatric disorder in the 12 months preceding enrollment; d) currently suicidal; e) having major hallucinations or delusions; and, f) having physical limitations or chronic conditions that prevent participation in the low-impact exercises program.
2.5. Consenting
After a dyad is screened eligible, consent forms are emailed prior to a scheduled consent interview. Research staff are trained to review consent forms, including addressing any questions or concerns raised by participants, as well as to ask a series of questions to assess comprehension and competence to consent. For example, if the care recipient is unable to provide consent, research staff will contact the care partner or, if applicable, the care recipient’s legally authorized representative, to obtain consent. If any issues arise during the consent process, a trained and licensed psychologist with expertise in dementia and informed consent is consulted by the research staff. Following consent, the care recipient is administered the MMSE cognitive screening.
2.6. Randomization
Eligible and consented dyads are randomized into enhanced IDEA or standard RDAD through a clustered randomization procedure [42]. Using a computer algorithm, dyads are randomly assigned to the two experimental conditions in blocks of six, reducing the chance that group assignments would be unbalanced.
2.7. Intervention
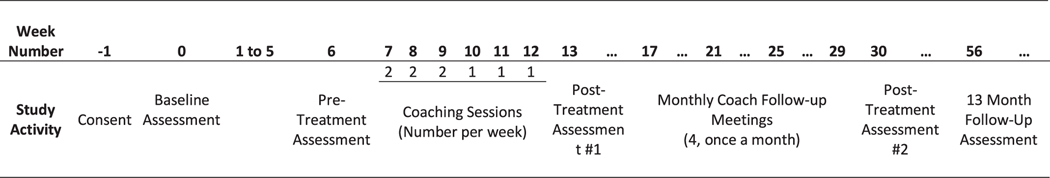
Fig. 1 details the study sequencing. The care partner of the randomized dyads completes the initial baseline assessment at 0 weeks, which assesses a variety of demographic characteristics, as well as primary and secondary physical, psychological, and social outcomes. Primary and secondary outcomes replicated those utilized in standard RDAD [28] with the inclusion of SGM-specific outcomes based upon the findings of NHAS [3]. All measures are completed by the care partner, including self-report and for the person living with dementia. See Table 2 for a description of all measures. Following the initial baseline assessment, participants have a 6-week waiting period and complete another baseline (pretreatment) assessment six weeks after the Time 0 baseline assessment. The staggered pre-treatment assessments provide a within-subjects control period. Then, after the 6-week treatment period, follow-up assessments are conducted at 13, 30, and 56 weeks. The six-week enhanced IDEA and standard RDAD are delivered by coaches randomly assigned to intervention arms. Coaches have a variety of educational and professional backgrounds, with the majority having some experience working within SGM communities and trained in either health, human, or behavioral services. Both programs consist of nine, 1-h sessions, conducted in the participants’ homes over six weeks. The sessions are conducted twice a week for the first three weeks; once a week for the next three weeks. After the treatment phase is concluded, the participants enter a 12-week maintenance phase. During this time, all participants receive four, 30-min follow-up phone meetings once a month for the next four months from their assigned coach. Table 3 details enhanced IDEA and standard RDAD curricular intervention components.
Fig. 1.
Study sequencing.
Table 2.
Measures.
| Variable(s) | Measure(s) | Person Assessed | Response Range |
|---|---|---|---|
| Health related quality of life | |||
| Physical activity | Number of days of aerobic activity of at least 30 min per week | CR & CP | 0–7 |
| Chronic conditions/diseases | 15-item measure of different health conditions. | CR & CP | Yes/no |
| Memory, depression, and behavior disturbances | 24-item Revised Memory and Behavior Problem Checklist (RMBPC) [25] | CR | 4-point scale: none to daily or more often |
| Depressive symptomology | 10-item (mean score), Center for Epidemiological Studies-Depression scale (CESD-10) [44] | CP | 5-point scale: less than once a week or never to everyday |
| Activity limitations | 10-item (mean score), physical functioning subscale of the Medical Outcomes Study 36-Item Short Form (SF-36) [45] | CR & CP | Yes/no |
| Quality of life | 13-item Quality of Life in Alzheimer’s Disease (QOL – AD) [46] | CR | 4-point scale: poor to excellent |
| Social connectedness | |||
| Relationship status | Single item | CR & CP | Partnered, married, divorced, widowed, separated, never married, or never partnered |
| Social Support | 4-item (mean score), brief MOS-Social Support Scale [47] | CR & CP | 5-point scale: never to very often |
| SGM community engagement | 3-item questionnaire regarding SGM community knowledge and resources | CP | 4-point scale: strongly disagree to agree |
| Social Isolation | 3-item (mean score) UCLA Loneliness Scale [48] | CP | 4-point scale: never to often |
| Caregiving | |||
| Relationship between CR/CP | Single item question about relationship between CR/CP | CP | Partner/spouse, friend, parent or parent-in-law, child, grandchild, other relative, other relationship |
| Caregiving efficiency | 3-items, assessing competency in problem solving and support seeking | CP | 4-point scale: strongly disagree to agree |
| Minority stress | |||
| Perceived stress | 4-item (mean score) Brief Perceived Stress Scale [49] | CP | 5-point scale: never to very often |
| Adverse experiences | 6-item (mean score), SGM Microaggressions assessing frequency of external stigma based on perceived SGM identity | CP | 5-point scale: never to very often. |
| Background characteristics at baseline | |||
| Age | Single item | CR & CP | Month, day, year Female, male, not listed |
| Sex assigned at birth | Single item | CR & CP | Woman, man, not |
| Gender identity | Single item question about gender identity | CR & CP | Woman, man, not listed (gender diverse) |
| Transgender identity | Single item question about transgender identity | CR & CP | Yes/no |
| Sexual orientation | Single item question about sexual orientation | CR & CP | Gay or lesbian, bisexual, straight, not listed (sexually diverse) |
| Race | Single item question about race | CR & CP | White, Black or African American, Asian, Native Hawaiian or Other Pacific Islander, American Indian, Alaska Native, Other |
| Ethnicity | Single item question about ethnicity | CR & CP | Yes/no |
| Language(s) spoken | Single item | CR & CP | Yes/no |
| Educational level | Single item question | CR & CP | No high school, some high school, high school graduate or equivalent, some college, college degree, some graduate, graduate degree, vocational/technical certificate |
| Employment status | Single item question about employment | CR & CP | Yes/no |
| Military/veteran status | Single item question about military status | CR & CP | Yes/no |
| Cognitive functioning | Mini-Mental State Exam (MMSE) [43] | CR | Open ended responses |
Table 3.
Intervention curriculum.
| Session # | RDAD Standard Components | IDEA Enhanced Components Enhancement: Application of EES Check-in in the beginning of each session |
|---|---|---|
| 1 | • Introduction/logistics • Overview and rationale of exercise program • Overview of behavior changes in ADRD |
• Introduction/logistics • Overview and rationale of exercise program • Overview of behavior changes in ADRD ∘ Enhancement: Discuss current social and community supports ∘ Enhancement: Discuss relationship between the person with dementia and the care partner and their living arrangement and identify potential obstacles ∘ Enhancement: Respond to SGM identity, bias, and trauma; discussed as part of memory loss experience |
| 2 | • Exercise program: Warm-up/cool down exercises • Behavior program: Realistic expectations and learning to observe problematic behaviors |
• Exercise program: Warm-up/cool down exercises • Behavior program: Realistic expectations and learning to observe problematic behaviors ∘ Enhancement: Respond to issues of personal histories and identity management ∘ Enhancement: Explore support from family, family of choice, friends, and community resources |
| 3 | • Exercise program: Strengthening exercises • Behavior program: Introduction to the ABCs |
• Exercise program: Strengthening exercises • Behavior program: Introduction to pleasant events ∘ Enhancement: Consideration of unique life histories and experiences both adverse and positive, including bias, trauma, and personal engagement. ∘ Enhancement: Discuss social connections (SGM identities effect on social interaction; SGM-related and general community resources) |
| 4 | • Exercise program: Endurance exercise • Behavior Program: Communication and applying the ABCs |
• Exercise program: Endurance exercise • Behavior Program: Communication & identifying pleasant events ∘ Enhancement: Communication with focus on SGM culture and communities ∘ Enhancement: Involving the person with dementia in identifying pleasant events if possible ∘ Enhancement: Discuss support needed to complete pleasant events |
| 5 | • Exercise program: Overview and practice • Behavior program: Developing a problem-solving plan with the ABCs |
• Exercise program: Overview and practice • Behavior program: Introduction to the EES-ABCs ∘ Enhancement: EES-ABCs enhanced from RDAD ABCs to include MI components and promote efficacy, engagement, and support mobilization in problem solving |
| 6 | • Exercise program: Monitoring and creating safe environment • Behavior program: Introduction to pleasant events |
• Exercise program: Monitoring and creating safe environment ∘ Enhancement: Discuss SGM identity and bias-related safety concerns • Behavior program: Applying the EES-ABCs |
| 7 | • Exercise program: Monitoring • Behavior program: Discussing nutrition management • Behavior program: Identifying pleasant events |
• Exercise program: Monitoring • Behavior program: Discussing nutrition management • Behavior program: Developing problem-solving plan with the EES-ABCs ∘ Enhancement: Taking into consideration SGM distinct issues. |
| 8 | • Exercise program: Monitoring • Behavior program: Coping with caregiving |
• Exercise program: Monitoring • Behavior program: Coping and thriving with caregiving ∘ Enhancement: Encouraging care partner to use the EES-ABC strategies and develop a plan to cope with stress, identify positive aspects of care, and strengthen confidence and support mobilization |
| 9 | • Exercise program: Review • Behavior program: Maintaining skills |
• Exercise program: Review • Behavior program: Maintaining skills ∘ Enhancement: Revisit SGM-specific issues that have been raised ∘ Enhancement: Discuss skills and ways to increase community engagement and support |
| 10–13 | • Follow-up phone meetings | • Follow-up phone meetings ∘ Enhancement: Revisit SGM specific issues raised throughout intervention ∘ Enhancement: Discuss social support needed for program maintenance |
The elements of standard RDAD include exercise with aerobic/endurance activities, strength training, and improving balance and flexibility. Exercises are introduced incrementally and individualized to meet the needs of each person, with the goal for both the person living with dementia and care partner to engage in a minimum of 30 min of moderate-intensity exercise daily. In the cognitive-behavioral component of standard RDAD, the antecedent-behavior-consequence (ABC) technique is applied. Care partners are taught to identify A) activating events leading to B) behavioral issues, and C) the consequences of the behavior. Care partners are taught to identify and modify behavioral dementia-related-challenges that can impair day-to-day functioning, and adversely affect interactions and exercise. Care partners are also instructed on how to create a secure, safe environment, ensure good nutrition, and identify pleasant activities that can be incorporated into daily life for both members of the dyad. Finally, issues with dementia and/or caregiving, such as depression, burden, and stress, are assessed and sources of support are identified. During the follow-up monthly phone meetings, the intervention participants review treatment skills with their coach, including how well exercise, problem-solving, and pleasant events have been maintained. They also discuss with their coach any new issues that may have arisen during the intervening month and assist the care partner to develop plans for dealing with them.
3. IDEA enhancements
In addition to the standard RDAD program components, enhanced IDEA employs culturally responsive empowerment practices based on findings from NHAS [3]. Empowerment is a process designed to cultivate engagement, efficacy, and support mobilization (EES) among the person living with dementia and their care partners. Enhanced IDEA coaches are taught and utilize the principles of EES and MI, to address barriers to engagement commonly faced by this and other underserved populations and to take full advantage of their psychological and social resources, with the expectation of improvement in program adherence and compliance. The EES key principles include:
Engagement:
The enhanced IDEA program is designed to increase the engagement of participants. The coach engages with participants, integrates SGM cultural content, remains open to feedback from participants about what is relevant to them, elicits participants’ personal motivation for engagement, and guides them to articulate their own values and goals.
Efficacy:
The development of the participants’ sense of efficacy is key to empowerment. When participants feel that they can achieve their goals, they are better equipped to work toward doing so. Therefore, enhanced IDEA coaches support participants in their abilities, emphasize their strengths, guide them in planning to meet their personal goals, encourage them to provide feedback on the program, and utilize feedback in the follow-up sessions.
Support mobilization:
Due to the social isolation of many SGM older adults and their unique and varied care partner relationships, mobilizing support resources is crucial in establishing sustainable change. The enhanced IDEA coach helps both the person living with dementia and the care partner identify existing national and local resources addressing the needs of SGM older adults such as the Goldsen Institute older adult resources and programs (https://goldseninstitute.org), the National Resource Center on LGBTQ+ Aging (https://www.lgbtagingcenter.org), and SGM related Alzheimer’s and dementia information and support. Such community resources provide valuable information, materials, and support and can help mitigate the effect of stigma on loneliness, depression, and overall quality of life. Enhanced IDEA coaches provide information about potential additional resources and guide the dyad in concrete planning steps for accessing and utilizing support.
A lack of empowerment due to stigma, non-disclosure of stigmatized identities, historical and contemporary trauma, and social isolation related to sexual and gender minority statuses among SGM older adults living with dementia and their care partners may be major barriers to engagement and intervention implementation. The empowerment practice integrated in enhanced IDEA is designed to amplify the person-centered approach of the intervention by adapting MI and increasing the cultural relevance of the intervention. For example, an EES Check-In is used to help coaches identify obstacles participants may be facing as well as their strengths and to initiate MI communication strategies to enhance EES.
3.1. Motivational interviewing
Although rarely used with older adults or in dementia intervention research, enhanced IDEA coaches are taught MI as a change mechanism, to promote empowerment among the person living with dementia and their care partner to support intervention goals, retention, and adherence to care plans. MI guides coaches in four fundamental processes: 1) establish a mutually trusting and respectful helping relationship; 2) clarify goals or directions for change; 3) elicit the participants’ own motivation for change; and 4) develop specific change plans that the participants are interested in implementing [50]. MI is an evidence-based, collaborative communication style that promotes motivation for change [50]. Aspects of MI have been shown to affect treatment retention and adherence, predict better outcomes, and achieve results for clients in less time [51–53]. MI can be particularly salient with groups who have experienced social rejection, stigma, and societal pressure because of its humanistic style and emphasis on self-determination [53]. It has been shown to have a more significant effect on outcomes when implemented with clients from marginalized populations [52,53]. MI is employed to facilitate positive change in exercise and behavior change and other outcomes via building trust with participants and guiding them to enhance engagement, self-efficacy, and support mobilization.
3.2. Cultural responsiveness
Enhanced IDEA is designed to respond to SGM specific needs and barriers, including stigma, identity management, disclosure and concealment, bias and trauma, and social isolation, as well as to address other potential barriers and to identity strengths and resources. Enhanced IDEA coaches are trained in these specific areas of cultural relevance and the application of trauma informed care [36].
Stigma:
SGM older adults living with memory loss and their care partners face sexual, gender, age, culture, and dementia related stigma, which involves the devaluing of the person based on their identities within the social context. Stigma exists when there is a characteristic that society views as discrediting [54] creating a situation where they are seen as “other” than mainstream society. Such stigma manifests at multiple levels, including intrapersonal (internalized), interpersonal (including familial), institutional and community (including health and social services), and structural (including public policies) [55,56]. Social stigma has been found to be significantly associated with SGM older adults’ adverse mental and physical health outcomes, increased substance use, internal and external conflict, and social exclusion [57,58]. Among SGM populations, sexual and gender-related stigma is compounded by differing types of stigma and other intersectional identities, including age, culture and race/ethnicity, dementia [4], and HIV related stigma [55]. The World Alzheimer’s Report [59], for example, found that in the U.S., 26.4% of the general public would hide their dementia diagnosis if possible. Both sexual, gender, age, culture and race/ethnicity, and dementia-related stigma are factors that can impact not obtaining a timely dementia diagnosis but also limit access to appropriate services and supports [4]. As part of enhanced IDEA, coaches are trained on specific ways to assist those living with dementia and their care partners to both recognize and effectively respond to sexual, gender, age, culture and race/ethnicity, and dementia-related stigma.
Identity management:
The process of identity management – when, where, how, in what particular contexts identities are concealed/hidden or disclosed are complicated by declining cognitive ability, as persons living with dementia may have difficulty safely navigating disclosure [60]. Enhanced IDEA coaches focus on teaching both the person living with dementia and the care partner how to assess and respond to identity management challenges. The coaches are trained to assist participants on how to navigate identity management as well as potential feelings of discomfort or embarrassment they may experience when faced with difficulty with disclosure of their identifies.
Bias:
Bias can be explicit, such as discrimination, victimization and the failure to provide services, or implicit, such as an automatic prejudice activated independently of an individual’s current attitudes or beliefs and can produce systematic discrimination in subtle, indirect ways that are difficult to monitor and control [61,62]. The adverse influence of both explicit and implicit bias on treatment decisions and adherence, patient-provider interactions, and perceptions of care and accessing care [63–65] make interrupting bias an important consideration for enhanced IDEA. During training and throughout intervention delivery, enhanced IDEA coaches are encouraged to critically analyze their own experiences and potential biases toward participants. Coaches also help participants identify and respond to experiences of explicit and implicit bias and connect them with resources specific to SGM older adults, potentially attenuating bias and resulting in more positive perceptions of care.
Trauma informed care:
Research indicates that most SGM older adults have experienced trauma multiple times over their lifetime [57,58]. The trauma informed care model utilized in this intervention is responsive to issues of culture, sexuality, and gender, with the goal to ensure safety and promote trust, collaboration, autonomy, and empowerment among intervention participants [36]. Enhanced IDEA coaches are trained to assist care partners and participants, if appropriate, to learn to identify potential triggers for them in terms of remembering traumatic life events, and how to limit exposure to triggers when possible. For example, if stimuli are identified as antecedents to traumatic agitation, the person living with dementia and the care partner are coached to structure activities or redirect in ways that minimize contact and adverse impact.
3.3. Fidelity
To ensure treatment fidelity and maintain high quality control throughout the intervention and evaluation, Lead Interventionists closely monitor coaches’ training and skill acquisition, treatment intensity, consistency, treatment receipt, and enactment. The intervention goal is to ensure equivalency in coach skill and ability through a well-developed training program. All coaches are randomly assigned to either the enhanced IDEA or standard RDAD arms, and they attend a two-day training, one covering standard RDAD only by the RDAD research team [66] and one for enhanced IDEA coaches [67] designed to address the needs of SGM older adults. Both trainings introduce coaches to study curriculum, best practices for coaching dyad sessions, and guided practice through intervention components. Coaches record their sessions with dyads, and complete progress notes after each session. Each coach has a training case, with each session reviewed and rated by the Lead Interventionists for fidelity to the treatment protocol.
Lead Interventionists provide feedback to coaches after each session in the training case on adherence to protocol content, competence delivering behavior management, exercise instructions to participants, intervention components, use of problem-solving strategies, general therapeutic communication skills, and relationship building skills. To move beyond their training case (3 allowed), coaches are required to have a total rating of 80% or higher. Following successful completion of the training case, coaches receive feedback from Lead Interventionists on two randomly selected sessions on their second case. On an on-going basis, Lead Interventionists follow-up as needed with specific coaches via phone calls. To support, advise, and provide feedback to coaches implementing the intervention, regular weekly coach group consultation meetings take place to facilitate problem-solving and enhance skill development. The PIs hold regular consultation meetings with Lead Interventionists and monitor maintenance of treatment fidelity throughout the implementation phase.
3.4. Adverse events monitoring
Coaches are trained to identify, obtain additional information on, and report any adverse events experienced by participants. The research coordinator records all adverse event information from the start of enrollment to the last phone assessment. The research coordinator is trained to identify potential serious adverse events and reports them immediately to the PIs, who ensures the proper action and categorization are taken.
4. Discussion and conclusion
This study is designed to develop IDEA, the first ever culturally enhanced intervention for SGM older adults experiencing dementia and their care partners, based on, and compared to, standard RDAD, an efficacious intervention [28]. Our goal is to increase the physical functioning, social engagement, and QoL of SGM older adults living with dementia, and promote intervention adherence. To minimize bias, data on treatment effects are collected with no knowledge about participants’ randomization status. To assess whether randomization of participants is successful, the two treatment groups will be compared on baseline demographics and clinical characteristics. Once all intervention data is collected, the efficacy of the intervention will be evaluated and we will assess both recruitment and retention of enhanced IDEA participants, compared to standard RDAD and all study aims and outcomes.
To promote efficacy, engagement, and successful implementation, interventions must be responsive to cultural context [68]. Enhanced IDEA is the first culturally informed evidence-based dementia intervention designed for SGM older adults living with dementia and their care partners. It joins the small body of research focused on adapting dementia interventions for marginalized and underserved populations. Culturally adapted cognitive interventions for Hispanic and Latino dementia care partners have been described and tested [69,70]. Emerging evidence with African Americans with mild cognitive impairment has also found support for a culturally adapted intervention [71] that, like IDEA, is grounded in cognitive behavioral and MI strategies. In each of these adapted interventions, evidenced-based models are combined with a cultural framework specific to the population of interests’ strengths, challenges, and cultural history.
SGM populations have been identified as a health disparate population [72], with unique health and social disparities placing them at heightened risk of dementia, and distinctive care giving vulnerabilities and strengths. Given these factors, interventions designed for SGM individuals with dementia and their care partners are needed in the context of a diverse, aging population. By supporting change via empowerment practice, promoting physical activity, and addressing stigma, we move the knowledge base forward by evaluating the importance of population and cultural-specific content within a historically marginalized and stigmatized population. The enhanced IDEA intervention is poised to respond to the growing diverse population and the existing disparities in dementia care.
Funding
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number R01AG055488 (Fredriksen-Goldsen and Teri, MPI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This study is registered with ClinicalTrials.gov (Identifier: NCT03666624).
Footnotes
Sexual and gender minorities are defined in this research as individuals who self-identify as lesbian, gay, bisexual, or transgender, or sexually or gender diverse, or ever engaged in same-sex sexual behavior, or had a romantic relationship with, or attraction to, someone of the same sex or gender.
Declaration of Competing Interest
The authors report no conflict of interest.
Data availability
No data was used for the research described in the article.
References
- [1].Hebert LE, Weuve J, Scherr PA, Evans DA, Alzheimer disease in the United States (2010–2050) estimated using the 2010 census, Neurology 80 (19) (2013) 1778–1783, 10.1212/WNL.0b013e31828726f5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Fredriksen-Goldsen KI, Kim H-J, Barkan SE, Muraco A, Hoy-Ellis CP, Health disparities among lesbian, gay, and bisexual older adults: results from a population-based study, Am. J. Public Health 103 (10) (Oct 2013) 1802–1809, 10.2105/AJPH.2012.301110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Fredriksen-Goldsen KI, Kim HJ, The science of conducting research with LGBT older adults-an introduction to aging with pride: National Health, aging, and sexuality/gender study (NHAS), Gerontologist. 57 (Suppl. 1) (Feb 2017) S1–S14, 10.1093/geront/gnw212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Fredriksen-Goldsen KI, Jen S, Bryan AEB, Goldsen J, Cognitive impairment, Alzheimer’s disease, and other dementias in the lives of lesbian, gay, bisexual and transgender (LGBT) older adults and their caregivers: needs and competencies, J. Appl. Gerontol 37 (5) (May 2018) 545–569, 10.1177/0733464816672047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Jutkowitz E, Kane RL, Gaugler JE, MacLehose RF, Dowd B, Kuntz KM, Societal and family lifetime cost of dementia: implications for policy, J. Am. Geriatr. Soc 65 (10) (Oct 2017) 2169–2175, 10.1111/jgs.15043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Alzheimer’s Association, Alzheimer’s disease facts and figures, Alzheimers Dement. 16 (3) (2020). [DOI] [PubMed] [Google Scholar]
- [7].Fredriksen Goldsen K, Shuyman A, Jen S, Jung H, Stress and resilience among sexual and gender diverse caregivers, Res. Aging (2023), 10.1177/01640275231156191. First published online February 11, 2023. [DOI] [PMC free article] [PubMed]
- [8].Croghan CF, Moone RP, Olson AM, Friends, family, and caregiving among midlife and older lesbian, gay, bisexual, and transgender adults, J. Homosex 61 (1) (2014) 79–102, 10.1080/00918369.2013.835238. [DOI] [PubMed] [Google Scholar]
- [9].Anderson JG, Jabson Tree JM, Flatt JD, Gross AL, Williams IC, Rose KM, A comparative analysis of family quality of life between heterosexual and sexual minority caregivers of people with dementia, J. Appl. Gerontol 41 (6) (Jun 2022) 1576–1584, 10.1177/07334648221079496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Fredriksen-Goldsen K, Jen S, Emlet CA, Kim HJ, Jung HH, Key determinants of physical and psychological health-related quality of life over time among midlife and older LGBTQ and sexual and gender diverse caregivers, Gerontologist. (7 Aug 2022), 10.1093/geront/gnac112. [DOI] [PMC free article] [PubMed]
- [11].Anderson JG, Flatt JD, Tree J.M. Jabson, Gross AL, Rose KM, Characteristics of sexual and gender minority caregivers of people with dementia, J. Aging Health 33 (10) (Dec 2021) 838–851, 10.1177/08982643211014767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Di Lorito C, Bosco A, Peel E, et al. , Are dementia services and support organisations meeting the needs of lesbian, gay, bisexual and transgender (LGBT) caregivers of LGBT people living with dementia? A scoping review of the literature, Aging Ment. Health (28 Nov 2021) 1–10, 10.1080/13607863.2021.2008870. [DOI] [PubMed]
- [13].Fredriksen-Goldsen K, Kim H-J, Emlet C, Muraco A, Erosheva E, Hoy-Ellis C, Goldsen J, Petry H, The Aging and Health Report: Disparities and Resilience Among Lesbian, Gay, Bisexual, and Transgender Older Adults, Institute for Multigenerational Health, 2011.
- [14].Fredriksen-Goldsen KI, Kim H-J, Barkan SE, Disability among lesbian, gay, and bisexual adults: disparities in prevalence and risk, Am. J. Public Health 102 (1) (Jan 2012) e16–e21, 10.2105/AJPH.2011.300379. [DOI] [PMC free article] [PubMed]
- [15].Huang J, HIV-associated dementia. Merck Manual Professional Version, Updated February 1,2023 Accessed February 1, 2023, http://www.merckmanuals.com/professional/neurologic-disorders/delirium-and-dementia/hiv-associated-dementia.
- [16].Fredriksen Goldsen KI, Jung HH, Kim H-J, Petros R, Emlet C, Disparities in subjective cognitive impairment by sexual orientation and gender in a national population based study of U.S. adults, 2013–2018, J. Aging Health (14 Oct 2021), 10.1177/08982643211046466. Advance online publication: 8982643211046466. [DOI] [PMC free article] [PubMed]
- [17].Flatt JD, Cicero EC, Lambrou NH, et al. , Subjective cognitive decline higher among sexual and gender minorities in the United States, 2015–2018, Alzheimers Dement (N Y). 7 (1) (2021), e12197, 10.1002/trc2.12197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Hsieh N, Liu H, Lai WH, Elevated risk of cognitive impairment among older sexual minorities: Do health conditions, health behaviors, and social connections matter? Gerontologist 61 (3) (3 Apr 2021) 352–362, 10.1093/geront/gnaa136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Fredriksen-Goldsen KI, Caregiving with Pride, Haworth Press, 2007. [Google Scholar]
- [20].Cantor MH, Brennan M. Caregiving among older lesbian, gay, bisexual, and transgender New Yorkers, National Gay and Lesbian Task Force Policy Institute, New York, 2004. [Google Scholar]
- [21].Herrmann WJ, Oeser P, Buspavanich P, Lech S, Berger M, Gellert P, Loneliness and depressive symptoms differ by sexual orientation and gender identity during physical distancing measures in response to COVID-19 pandemic in Germany, Article; Early Access, Appl. Psychol. Health Well Being (2022) 17, 10.1111/aphw.12376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Tun SM, Murman DL, Colenda CC, Concurrent validity of neuropsychiatric subgroups on caregiver burden in Alzheimer disease patients, Am. J. Geriatr. Psychiatry 16 (7) (Jul 2008) 594–602, 10.1097/JGP.0b013e318173f5fc. [DOI] [PubMed] [Google Scholar]
- [23].Kim HJ, Fredriksen-Goldsen K, Jung HH, Determinants of physical functioning and health-related quality of life among sexual and gender minority older adults with cognitive impairment, J. Aging Health (29 Jun 2022), 10.1177/08982643221108658,8982643221108658. [DOI] [PMC free article] [PubMed]
- [24].Teri L, McKenzie G, Logsdon RG, et al. , Translation of two evidence-based programs for training families to improve care of persons with dementia, Gerontologist. 52 (4) (Aug 2012) 452–459, 10.1093/geront/gnr132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Teri L, Truax P, Logsdon R, Uomoto J, Zarit S, Vitaliano PP, Assessment of behavioral problems in dementia: the revised memory and behavior problems checklist, Article. Psychol. Aging 7 (4) (Dec 1992) 622–631, 10.1037/0882-7974.7.4.622. [DOI] [PubMed] [Google Scholar]
- [26].Teri L, Logsdon RG, McCurry SM, Exercise interventions for dementia and cognitive impairment: the Seattle protocols, J. Nutr. Health Aging 12 (6) (2008) 391–394, 10.1007/bf02982672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Teri L, Logsdon RG, McCurry SM, Pike KC, McGough EL, Translating an evidence-based multicomponent intervention for older adults with dementia and caregivers, Gerontologist 60 (3) (2020) 548–557, 10.1093/geront/gny122,0402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Teri L, Gibbons LE, McCurry SM, et al. , Exercise plus behavioral management in patients with Alzheimer disease: a randomized controlled trial, JAMA. 290 (15) (15 Oct 2003) 2015–2022, 10.1001/jama.290.15.2015. [DOI] [PubMed] [Google Scholar]
- [29].McCurry SM, Logsdon RG, Pike KC, Lafazia DM, Teri L, Training area agencies on aging case managers to improve physical function, mood, and behavior in persons with dementia and caregivers: examples from the RDAD-northwest study, J. Gerontol. Soc. Work 61 (1) (2018) 45–60, 10.1080/01634372.2017.1400486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Glasgow RE, Emmons KM, How can we increase translation of research into practice? Types of evidence needed, Annu. Rev. Public Health 28 (2007) 413–433. [DOI] [PubMed] [Google Scholar]
- [31].Glasgow RE, Klesges LM, Dzewaltowski DA, Bull SS, Estabrooks P, The future of health behavior change research: what is needed to improve translation of research into health promotion practice? Ann. Behav. Med 27 (1) (2004) 3–12. [DOI] [PubMed] [Google Scholar]
- [32].Fredriksen-Goldsen KI, Simoni JM, Kim HJ, et al. , The health equity promotion model: reconceptualization of lesbian, gay, bisexual, and transgender (LGBT) health disparities, Am. J. Orthop 84 (6) (Nov 2014) 653–663, 10.1037/ort0000030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Romanelli M, Fredriksen Goldsen K, Kim H-J, Development of a multidimensional measure of health care access among LGBTQ older adults. Oral Presentation: 27th Annual Conference of the Society for Social Work and Research, 2023. Phoenix, AZ. [Google Scholar]
- [34].Bandura A, Social Learning Theory, General Learning Press, 1971. [Google Scholar]
- [35].Foglia MB, Fredriksen-Goldsen KI, Health disparities among LGBT older adults and the role of nonconscious bias, Hast. Cent. Rep 44 (5) (2014) S40–S44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Heinen C, Optimizing Communication with Gender Diverse Patients Using a Trauma Informed Approach and Medical Context and Management of Transgender and Gender Non-binary Patients, 2019.
- [37].Livingston NA, Berke D, Scholl J, Ruben M, Shiphered JC, Addressing diversity in PTSD treatment: clinical considerations and guidance for the treatment of PTSD in LGBTQ populations, Curr. Treat Options Psychiat. 7 (2) (2020) 53–69, 10.1007/s40501-020-00204-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Hawkins NG, Sanson-Fisher RW, Shakeshaft A, D’Este C, Green LW, The multiple baseline design for evaluating population-based research, Am. J. Prev. Med 33 (2) (Aug 2007) 162–168, 10.1016/j.amepre.2007.03.020. [DOI] [PubMed] [Google Scholar]
- [39].Samsa G, Edelman D, Rothman ML, Williams GR, Lipscomb J, Matchar D, Determining clinically important differences in health status measures: a general approach with illustration to the health utilities index mark II, Pharmacoeconomics. 15 (2) (Feb 1999) 141–155. [DOI] [PubMed] [Google Scholar]
- [40].Knopman DS, Petersen RC, Mild cognitive impairment and mild dementia: a clinical perspective, Mayo Clin. Proc 89 (10) (Oct 2014) 1452–1459, 10.1016/j.mayocp.2014.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Teng E, Becker BW, Woo E, Knopman DS, Cummings JL, Lu PH, Utility of the functional activities questionnaire for distinguishing mild cognitive impairment from very mild Alzheimer disease, Alzheimer Dis. Assoc. Disord 24 (4) (Oct-Dec 2010) 348–353, 10.1097/WAD.0b013e3181e2fc84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Altman DG, How to randomize, BMJ. 319 (1999) 703–704, 10.1136/bmj.319.7211.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Folstein MF, Folstein SE, McHugh PR, “Mini-mental state” a practical method for grading the cognitive state of patients for the clinician, J. Psychiatr. Res 12 (1975) 189–198. [DOI] [PubMed] [Google Scholar]
- [44].Andresen EM, Malmgren JA, Carter WB, Patrick DL, Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale), Am. J. Prev. Med 10 (2) (Mar-Apr 1994) 77–84. [PubMed] [Google Scholar]
- [45].Stewart M, The medical outcomes study 36-item short-form health survey (SF-36), Aust. J. Physiother 53 (3) (2007) 208. [DOI] [PubMed] [Google Scholar]
- [46].Logsdon RG, Gibbons LE, McCurry SM, Teri L, Quality of life in Alzheimer’s disease: patient and caregiver reports, J. Ment. Health Aging 5 (1999) 21–32. [Google Scholar]
- [47].Sherbourne CD, Stewart AL, The MOS social support survey, Soc. Sci. Med. 32 (6) (1991) 705–714. [DOI] [PubMed]
- [48].Berndt DJ, How valid are the subscales of the multiscore depression inventory? J. Clin. Psychol 37 (3) (1981) 564–570. [DOI] [PubMed] [Google Scholar]
- [49].Cohen S, Kamarck T, Mermelstein R, A global measure of perceived stress, J. Health Soc. Behav. 24 (4) (Dec 1983) 385–396. [PubMed] [Google Scholar]
- [50].Miller WR, Rollnick S, Motivational interviewing: Helping people change, 3rd edition, in: Motivational Interviewing: Helping People Change, 3rd edition, Guilford Press, 2013. xii, 482–xii, 482. [Google Scholar]
- [51].Burke BL, Dunn CW, Atkins DC, Phelps JS, The emerging evidence for motivational interviewing: a meta-analytic and qualitative inquiry, J. Cogn. Psychother 18 (4) (2004) 309–322. [Google Scholar]
- [52].Hettema J, Steele J, Miller WR, Motivational interviewing, Annu. Rev. Clin. Psychol 1 (2005) 91–111. [DOI] [PubMed] [Google Scholar]
- [53].Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke BL, A meta-analysis of motivational interviewing: twenty-five years of empirical studies, Res. Soc. Work. Pract 65 (11) (2010) 1232–1245. [Google Scholar]
- [54].Goffman E, Stigma: Notes on the Management of Spoiled Identity, Simon and Schuster, 1963.
- [55].Emlet CA, Stigma in an aging context, Interdiscip. Top Gerontol. Geriatr 42 (2017) 144–158, 10.1159/000448560. [DOI] [PubMed] [Google Scholar]
- [56].Emlet CA, Brennan-Ing M, Is there no place for us? The psychosocial challenges and rewards of aging with HIV, J. Elder Pol 1 (1) (2020) 69–95, 10.18278/jep.1.1.4. [DOI] [Google Scholar]
- [57].Fredriksen-Goldsen KI, Emlet CA, Kim HJ, et al. , The physical and mental health of lesbian, gay male, and bisexual (LGB) older adults: the role of key health indicators and risk and protective factors, Gerontologist. 53 (4) (Aug 2013) 664–675, 10.1093/geront/gns123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Fredriksen-Goldsen KI, Cook-Daniels L, Kim HJ, et al. , Physical and mental health of transgender older adults: an at-risk and underserved population, Gerontologist. 54 (3) (Jun 2014) 488–500, 10.1093/geront/gnt021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Lynch C, World Alzheimer report 2019: attitudes to dementia, a global survey, Alzheimers Dement. 16 (2020), e038255, 10.1002/alz.038255. [DOI] [Google Scholar]
- [60].Semlyen J, Dementia and the lesbian, gay, bisexual and trans (LGBT) population, Dementia Action Alliance, September 26, 2016. Accessed March 20, 2021. https://www.dementiaaction.org.uk/news/19643_dementia_and_the_lesbian_gay_bisexual_and_trans_lgbt_population. [Google Scholar]
- [61].Dovidio JF, Penner LA, Albrecht TL, Norton WE, Gaertner SL, Shelton JN, Disparities and distrust: the implications of psychological processes for understanding racial disparities in health and health care, Soc. Sci. Med 67 (3) (Aug 2008) 478–486, 10.1016/j.socscimed.2008.03.019. [DOI] [PubMed] [Google Scholar]
- [62].Devine PG, Stereotypes and prejudice: their automatic and controlled components, J. Pers. Soc. Psychol 56 (1) (1989) 5–18. [Google Scholar]
- [63].Chapman EN, Kaatz A, Carnes M, Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities, J. Gen. Intern. Med 28 (11) (Nov 2013) 1504–1510, 10.1007/s11606-013-2441-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Hall WJ, Chapman MV, Lee KM, et al. , Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review, Am. J. Public Health 105 (12) (Dec 2015) e60–e76, 10.2105/AJPH.2015.302903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Maina IW, Belton TD, Ginzberg S, Singh A, Johnson TJ, A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test, Soc. Sci. Med 02 (199) (2018) 219–229, 10.1016/j.socscimed.2017.05.009. [DOI] [PubMed] [Google Scholar]
- [66].Understanding Alzheimer’’s, Alzheimer’s Disease Research Center, University of Washington Department of Psychosocial and Community Health, Northwest Research Group on Aging, 2010. [Google Scholar]
- [67].Aging with Pride, Innovations in Dementia Empowerment and Action Coach Manual, 2018. [DOI] [PMC free article] [PubMed]
- [68].Barrera M, Castro FG, Strycker LA, Toobert DJ, Cultural adaptations of behavioral health interventions: a progress report, J. Consult. Clin. Psychol 81 (2) (2013) 196–205, 10.1037/a0027085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Parker LJ, Marx KA, Nkimbeng M, et al. , It’s more than language: cultural adaptation of a proven dementia care intervention for Hispanic/Latino caregivers, The Gerontologist (2022), 10.1093/geront/gnac120. [DOI] [PMC free article] [PubMed]
- [70].Gonyea JG, Lopez LM, Velasquez EH, The effectiveness of a culturally sensitive cognitive behavioral group intervention for Latino Alzheimer’s caregivers, Article. Gerontol 56 (2) (Apr 2016) 292–302, 10.1093/geront/gnu045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Owen A, Brown B, Deragon K, et al. , Developing an integrated cognitive behavioral therapy and motivational interviewing intervention for African Americans with mild cognitive impairment: a pilot study, Pract. Innov 7 (3) (2022) 241–254, 10.1037/pri0000182. [DOI] [Google Scholar]
- [72].National Institute on Minority Health and Health Disparities, Sexual and gender minorities formally designated as a health disparity population for research purposes, October 6, 2016. Updated June 27, 2022. Accessed July 6, 2022, https://www.nimhd.nih.gov/about/directors-corner/messages/message_10-06-16.html.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data was used for the research described in the article.