Abstract
Background
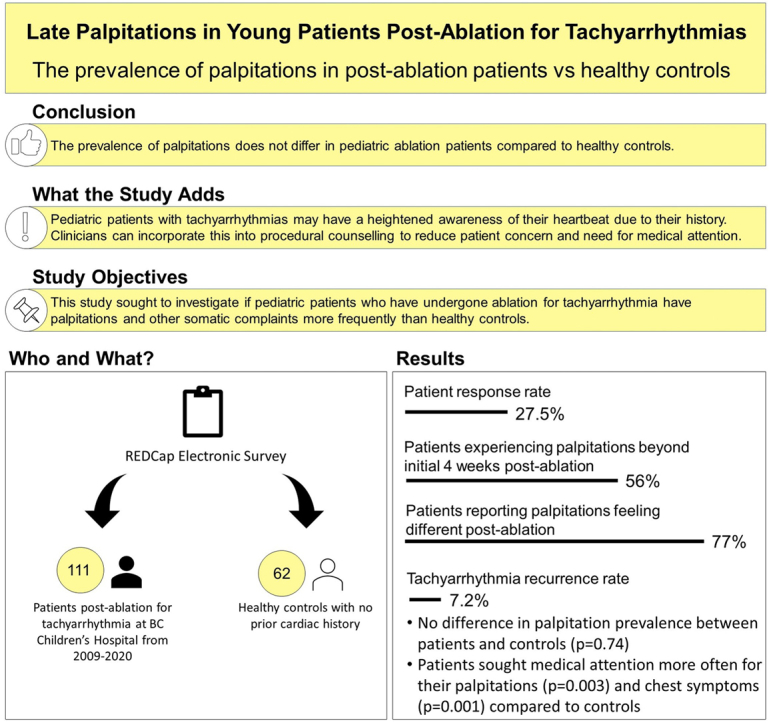
Patients after ablation for tachyarrhythmias may continue to experience palpitations in the setting of sinus rhythm. The objective of our study was to investigate if patients who have undergone ablation for tachyarrhythmia have palpitations and other somatic complaints more frequently than healthy controls.
Methods
Paediatric patients after ablation for tachyarrhythmia at BC Children’s Hospital from 2009 to 2020 and healthy controls were invited to participate in a survey about palpitations. Demographics, palpitation symptoms, frequency, duration, and need for medical attention were collected and compared between patients and controls.
Results
We received responses from 111 patients (response rate of 27.5%; mean age = 20.0 ± 4.6 years, 52% male) and 62 controls (age = 19.8 ± 5.7 years, 40% male). Sixty-two (56%) patients experienced palpitations beyond the initial 4 weeks after ablation, of whom 77% (n = 48/62) reported their palpitations feeling different. Tachyarrhythmia recurrence rate after ablation was 7.2%. There was no difference in the prevalence of palpitations experienced between patients and controls (P = 0.74). Patients after ablation sought medical attention more often for their palpitations (P = 0.003) and chest symptoms (P = 0.001) compared to controls.
Conclusion
The prevalence of palpitations did not differ in ablation patients compared to healthy controls. Patients reported that their palpitations felt different after ablation and were more likely to seek medical attention for their palpitations. Paediatric patients with tachyarrhythmias may have heightened awareness due to their history. Clinicians can incorporate this into procedural counselling to reduce patient concern and need for medical attention.
Graphical abstract
Résumé
Contexte
Après le traitement d’une tachyarythmie par ablation, les patients peuvent continuer de ressentir des palpitations en rythme sinusal. Notre étude avait pour objectif d’examiner si les patients ayant subi une ablation pour traiter une tachyarythmie présentaient plus fréquemment des palpitations et d’autres symptômes somatiques que des témoins en bonne santé.
Méthodologie
Une invitation à répondre à un sondage portant sur les palpitations a été transmise aux patients ayant subi une ablation au cours de leur enfance pour traiter une tachyarythmie au BC Children’s Hospital entre 2009 et 2020 ainsi qu’à des témoins en bonne santé. Des renseignements démographiques et des informations sur les symptômes de palpitation, leur fréquence, leur durée et le besoin de consulter un médecin ont été recueillis, puis des comparaisons ont été effectuées entre les patients et les témoins.
Résultats
Nous avons reçu une réponse au sondage de la part de 111 patients (taux de réponse de 27,5 %; âge moyen = 20,0 ± 4,6 ans, dont 52 % de sexe masculin) et de la part de 62 témoins (âge = 19,8 ± 5,7 ans, dont 40 % de sexe masculin). Soixante-deux patients (56 %) ont eu des palpitations au-delà de la période initiale de quatre semaines suivant l’ablation, et 77 % (n = 48 sur 62) d’entre eux ont mentionné ressentir des palpitations de nature différente. Le taux de récurrence de la tachyarythmie après l’ablation s’élevait à 7,2 %. Aucune différence n’a été observée entre la prévalence des palpitations chez les patients et chez les témoins (p = 0,74). Comparativement aux témoins, les patients ayant subi une ablation ont consulté plus souvent un médecin en raison de leurs palpitations (p = 0,003) et de leurs symptômes thoraciques (p = 0,001).
Conclusion
La prévalence des palpitations chez les patients ayant subi une ablation n’était pas différente de celle observée chez les témoins en bonne santé. Les patients ont rapporté ressentir des palpitations de nature différente après leur ablation, et ils étaient plus susceptibles que les témoins de consulter un médecin en raison de leurs palpitations. Il se pourrait que les patients atteints de tachyarythmie au cours de l’enfance se montrent plus vigilants en raison de leurs antécédents. Les cliniciens peuvent intégrer ces observations au processus de consultation afin de diminuer les inquiétudes des patients et le besoin de consulter un médecin.
Palpitations are among the most common symptoms reported by paediatric and adult patients presenting to primary care providers and cardiologists. Cardiac etiologies account for approximately 40% of all palpitation reports;1,2 among them, supraventricular tachycardias (SVT) are a frequent cause. Symptoms from SVT may impact daily life and the frequency for which medical care is sought. Catheter ablation (CA) is a safe and effective first-line therapy for SVT3, 4, 5, 6 and can greatly improve the symptom burden.
The CA success rate in paediatric populations is reported between 92 and 98%.7, 8, 9, 10 Despite this high procedural success rate in the modern era, patients may continue to experience palpitations in the absence of any abnormalities seen on electrophysiological restudy.4,11 Persistent palpitations in the setting of sinus rhythm are a common complaint among post-ablation patients in the outpatient cardiology clinic. Studies investigating this phenomenon in adult populations reveal that palpitations are frequently experienced after ablation but have a poor predictive value of arrhythmia recurrence.4,11 This suggests a possible increased awareness of a normal heartbeat. There is currently a limited understanding of the events that are responsible for heartbeat sensation, the involved afferent sensory pathways, and the higher-order processing responsible for filtering, modulating, and amplifying these stimuli.
We hypothesize that the brain-heart connection responsible for heartbeat awareness would be strengthened in paediatric patients with a history of symptomatic arrhythmia, resulting in a heightened awareness of cardiac symptoms. The aim of our study was to investigate if patients with ablated tachyarrhythmias complained of more palpitations compared to healthy controls.
Methods
Patients
Patients treated by radiofrequency ablation or cryoablation at BC Children’s Hospital between January 1, 2009, and December 31, 2020, who fulfilled the following inclusion criteria were enrolled in the study: (1) documented symptomatic or asymptomatic SVT inclusive of atrioventricular re-entrant tachycardia, atrioventricular nodal re-entry tachycardia, atrial tachycardia, and Wolff-Parkinson-White before the CA procedure; (2) had at least 1 year of follow-up in clinic after the CA procedure; (3) between 7 and 30 years of age at study entry but had a CA procedure performed at ≤19 years of age; (4) a structurally normal heart; and (5) ability to read in the English language.
Controls
Community controls were included if they were between 7 and 30 years of age, had no prior history of arrhythmia or other known heart disease, had never received treatment for a heart condition (including medications, surgery, or CA), and were able to read in the English language. The community control group was recruited through social media postings, physical posters, and email communication disseminated throughout the BC Children’s Hospital campus.
Survey
We developed an electronic survey using REDCap, a secure web application, to determine if patients and controls experienced any palpitation symptom burden and, if so, to characterize those palpitations. Survey questions targeted demographics, existing medical conditions, time of palpitation onset in relation to time since CA and frequency, duration, and sensation of palpitations (ie, “heart pounding,” “heart racing,” “skipped/extra beats,” and “heart fluttering”). In addition, questions about any chest symptoms experienced (ie, “chest pain/discomfort,” “chest tightness,” “chest pounding,” “flip-flopping within chest,” and “chest fluttering”) and whether or not medical attention was sought for chest or palpitation symptoms were included in the survey. A detailed summary of survey questions can be found in Supplemental Appendix S1.
Statistical analysis
Only complete survey responses from participants were included in data analysis. Data were analysed using SPSS version 25.0 software (IBM Corp, Armonk, NY). Nominal variables were expressed as counts (n) and percentages (%). Continuous variables were presented as mean with standard deviation. Descriptive statistics were reported for existing medical conditions for patients and controls. Palpitation symptoms, frequency, duration, and need for medical attention between patient and control groups were compared using a χ2 test. A χ2 test was used if >20% of expected cell counts were more than 5, and a Fisher’s exact test was used when >20% of expected cell counts were less than 5. Significance was considered when the 2-sided P value was <0.05.
Results
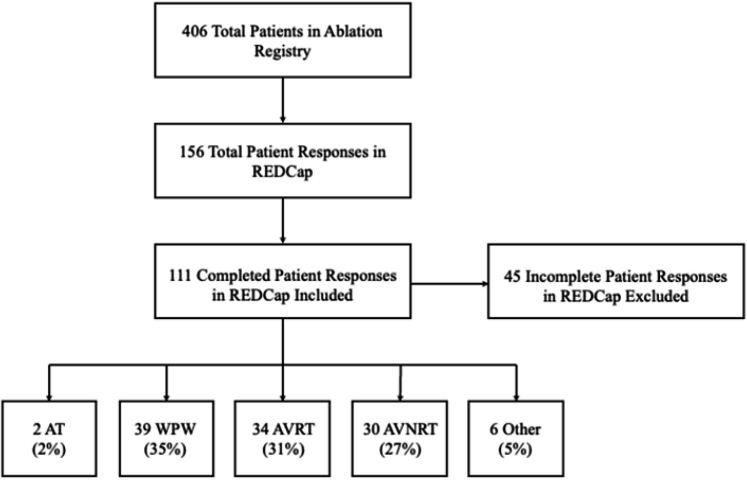
Of 403 ablation patients who were contacted to participate in the survey, 111 (27.5%) who completed responses were analysed (52% male, mean age 20.0 ± 4.6 years). The mean age of patients at the time of ablation was 13.6 ± 3.2 years. The mean time from the procedure to study participation was 6.1 ± 3.3 years. Of the 111 patients, ablation was indicated for Wolff-Parkinson-White in 39 patients (35%), followed by atrioventricular re-entrant tachycardia in 34 patients (31%), atrioventricular nodal re-entry tachycardia in 30 patients (27%), atrial tachycardia in 2 patients (2%), and other substrate for SVT (ie, empiric AV node modification and the Mahaim pathway) in 6 patients (5%) (Fig. 1). Tachyarrhythmia recurrence rate after ablation was 7.2%. A total of 62 (56%) patients continued to experience palpitations beyond the initial 4 weeks after their ablation. Thirty (48%) patients reported ongoing symptoms for years after the procedure, and 44 (40%) experienced them within 6 months of survey completion. Forty-eight (77%) patients who continued to experience palpitations after ablation reported that their palpitations felt different compared with those experienced before their procedure.
Figure 1.
Patient survey responses and indications for ablation therapy. The survey response rate was 27.5%, and only complete responses were analysed. Substrate for supraventricular tachycardia listed as “Other” included empiric AV node modification and Mahaim pathway. AT, atrial tachycardia; AVNRT, atrioventricular nodal re-entry tachycardia; AVRT, atrioventricular re-entrant tachycardia; WPW, Wolff-Parkinson-White.
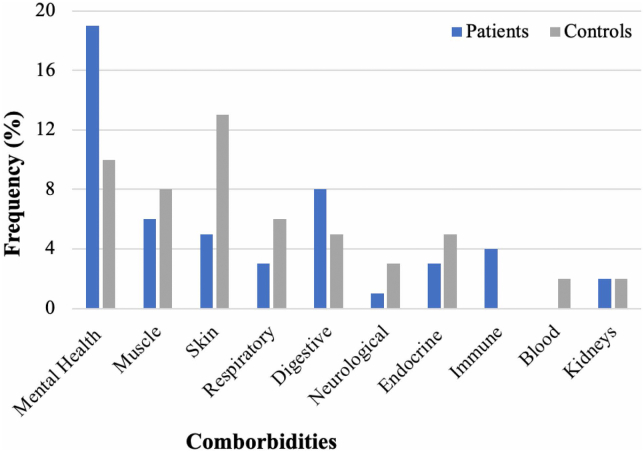
Sixty-two control responses were collected (40% male, mean age 19.8 ± 5.7 years). There was no difference in the prevalence of palpitations experienced between post-ablation patients and controls (56% [n = 62] for patients compared with 53% [n = 33] for controls, P = 0.74). Patients experienced significantly more skipped/extra beats, heart fluttering/racing, and were more likely to describe multiple palpitation-related symptoms compared with controls (P < 0.001). Most patients experienced palpitations on a monthly frequency with episodes lasting for seconds, whereas most controls experienced palpitations on a daily frequency with episodes also lasting for seconds (Table 1). Controls (85%, n = 53) reported more chest symptoms compared with patients (63%, n = 70) (P = 0.001). However, patients sought medical attention more often than controls for their palpitations (patients: 43%; controls: 12%; P = 0.003) and chest symptoms (patients: 44%; controls: 13%; P = 0.001). Mental health (35%, n = 21) conditions were the most reported comorbidity among patients, whereas skin conditions (13%, n = 8) were the most common among controls (Fig. 2). Among controls and patients who reported palpitations, there was no difference in palpitation prevalence between those who had greater than 1 comorbidity versus a singular comorbidity (P = 0.23).
Table 1.
Symptoms, frequency, and duration of palpitations between post-ablation patients and controls who reported palpitations
| Patients (n = 44) | Controls (n = 33) | P value | |
|---|---|---|---|
| Symptoms | |||
| Heart pounding | 17 (39) | 23 (70) | 0.007 |
| Heart racing | 19 (43) | 12 (36) | 0.546 |
| Skipped beats/extra beats | 31 (71) | 6 (18) | <0.001 |
| Heart fluttering | 21 (48) | 2 (6) | <0.001 |
| Heart about to start racing | 17 (39) | 2 (6) | 0.001 |
| Other | 2 (5) | 0 (0) | 0.215 |
| Frequency of palpitations | |||
| Hourly | 2 (5) | 7 (21) | 0.033 |
| Daily | 3 (7) | 11 (33) | 0.006 |
| Weekly | 9 (20) | 6 (18) | 0.803 |
| Monthly | 19 (43) | 6 (18) | 0.020 |
| Yearly | 11 (25) | 3 (9) | 0.084 |
| Duration of palpitations | |||
| Seconds | 29 (66) | 21 (64) | 0.836 |
| Minutes | 13 (30) | 11 (33) | 0.722 |
| Hours | 2 (5) | 0 (0) | 0.215 |
| Days | 0 (0) | 0 (0) | N/A |
| Unknown | 0 (0) | 1 (3) | 0.429 |
Data are expressed as n (%).
N/A, not applicable.
Figure 2.
Reported comorbidities among post-ablation patients and controls.
Discussion
To our knowledge, this is the first study to report and compare to healthy controls the prevalence of palpitations in patients who have undergone successful ablation. Our results show that 56% of paediatric patients who undergo ablation for tachyarrhythmia continue to experience palpitations beyond the initial 4 weeks after their ablation. The prevalence of palpitations in patients may not differ from healthy controls who have never had a history of an arrhythmia or undergone ablation. These results suggest that our initial hypothesis that patients after ablation would report a higher prevalence of palpitations compared with healthy controls was incorrect. Previous studies in paediatric cohorts report a palpitation prevalence between 35% and 43%.12, 13, 14
Similarly, we found that 53% of our control population reported palpitations. A previous study reported palpitations associated with sinus rhythm in up to 39% of individuals.15 Given the limited number of studies of palpitations in healthy paediatric controls, it is difficult to interpret whether the prevalence of palpitations reported in our control population is consistent with the normal population.
The etiology of persistent palpitations despite successful arrhythmia ablation remains unclear. It is possible that the more attention individuals devote to cardiac activity, the more accurate it becomes.11,16,17 Patients with longstanding documented arrhythmias who have not undergone ablation therapy demonstrate superior performance on heartbeat detection testing compared with their sinus rhythm and healthy control counterparts.11,16 Patients learn to discriminate rhythm irregularities from normal heartbeats and label them as palpitations.4 In our study, the majority of patients (77%) felt a difference in their palpitations before and after successful ablation, which may reflect their heightened ability to detect subtle differences in heart rhythm activity. Although the prevalence of palpitations did not significantly differ between patients and controls, patients with a history of tachyarrhythmias may have been more likely to seek medical attention for their palpitations out of concern for recurrence of their arrhythmia.
Adrenergic environments and situations are also known to play a role in promoting brain-heart connections. Through heartbeat detection tasks, patients with greater beta-adrenergic sympathetic cardiac activation and inotropic activity have better ability to perceive their heartbeat at rest and during emotional activation.18,19 This is supported by the fact that heartbeat perception is improved during or immediately after physical exercise.20 Patients with anxiety disorders are known to have increased beta-adrenergic receptor sensitivity compared with the normal population;21 these patients are more vigilant to cardiorespiratory symptoms relative to other body symptoms.22,23 Mental health conditions including anxiety were the most reported comorbidities within our patient cohort; however, we did not identify any associations between individual or multiple comorbid health conditions and the odds of post-ablation palpitations.
Clinicians should consider the post-ablation prevalence of palpitations when counselling patients and their families about the procedure to appropriately manage expectations. Patients can be informed that not all post-ablation palpitations represent SVT. Rather, emphasis should be placed on being aware of the dangerous signs and symptoms that should necessitate presentation to medical attention.
Further investigation of the brain-heart connection and cardiac interoception should be pursued. Prospective studies should also focus on the effect of environmental influences in the form of verbal discussion and suggestion on the brain-heart connection and perception of palpitations.
Study limitations
This was a single-centre retrospective study, and our sample size of post-ablation patients was relatively small. Responses from patients and controls were subject to recall bias because those with a longer duration between the procedure and study entry may have had difficulty recalling their symptoms compared with participants who had their procedure recently. Participating healthy controls may have been subject to selection bias. The recruitment invitations had described the purpose of the study and included the term “palpitations”. Individuals with palpitations may have been more inclined to participate compared with those without palpitations or those who did not understand the term; however, it is necessary to adequately describe the purpose of the study to potential participants in order to adhere to ethical research standards. For instance, some control participants may have had palpitations in the past and wished to learn more about their symptoms; others may have wanted to contribute to medical research regardless of their history of palpitations. It is difficult to differentiate controls in these types of research studies. Limited data is available in the literature surrounding the prevalence of palpitations in healthy controls, thus making it difficult to ascertain if our results are representative of the normal population. We could not confirm if controls participating in our study were truly healthy individuals as the comorbid health conditions listed in the survey were not well defined. The experience of palpitations is subjective and varies substantially between individuals.
Conclusion
Patients reported their palpitations as feeling different after ablation and were more likely to seek medical attention for their palpitations. Although the prevalence of palpitations does not differ in paediatric patients who have undergone a successful ablation procedure compared with healthy controls, paediatric patients with tachyarrhythmias may have a heightened awareness or vigilance of their heartbeat. Clinicians can consider incorporating these findings into procedural counselling to reduce the concern and need for medical attention.
Acknowledgments
Ethics Statement
Ethical approval for the study was obtained from the University of British Columbia Children’s and Women’s Research Ethics Board (H20-02530).
Patient Consent
The authors confirm that a patient consent form(s) has been obtained for this article.
Funding Sources
No funding was received for this study.
Disclosures
The author has no conflicts of interest to disclose.
Footnotes
To access the supplementary material accompanying this article, visit CJC Pediatric and Congenital Heart Disease at https://www.cjcpc.ca// and at https://doi.org/10.1016/j.cjcpc.2022.12.004.
Supplementary Material
References
- 1.Weber B.E., Kapoor W.N. Evaluation and outcomes of patients with palpitations. Am J Med. 1996;100:138–148. doi: 10.1016/s0002-9343(97)89451-x. [DOI] [PubMed] [Google Scholar]
- 2.Crawford M.H., Bernstein S.J., Deedwania P.C., et al. ACC/AHA guidelines for ambulatory electrocardiography. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the Guidelines for Ambulatory Electrocardiography). Developed in collaboration with the North American Society for Pacing and Electrophysiology. J Am Coll Cardiol. 1999;34:912–948. doi: 10.1016/s0735-1097(99)00354-x. [DOI] [PubMed] [Google Scholar]
- 3.Tung R., Boyle N.G., Shivkumar K. Catheter ablation of ventricular tachycardia. Circulation. 2010;122:e389–e391. doi: 10.1161/CIRCULATIONAHA.110.963371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mann D.E., Kelly P.A., Adler S.W., Fuenzalida C.E., Reiter M.J. Palpitations occur frequently following radiofrequency catheter ablation for supraventricular tachycardia, but do not predict pathway recurrence. Pacing Clin Electrophysiol. 1993;16:1645–1649. doi: 10.1111/j.1540-8159.1993.tb01034.x. [DOI] [PubMed] [Google Scholar]
- 5.Calkins H., Kumar V.K., Francis J. Radiofrequency catheter ablation of supraventricular tachycardia. Indian Pacing Electrophysiol J. 2002;2:45–49. [PMC free article] [PubMed] [Google Scholar]
- 6.Joseph J.P., Rajappan K. Radiofrequency ablation of cardiac arrhythmias: past, present and future. QJM. 2012;105:303–314. doi: 10.1093/qjmed/hcr189. [DOI] [PubMed] [Google Scholar]
- 7.Van Hare G.F., Carmelli D., Smith W.M., et al. Prospective assessment after pediatric cardiac ablation: design and implementation of the multicenter study. Pacing Clin Electrophysiol. 2002;25:332–341. doi: 10.1046/j.1460-9592.2002.00332.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Hare G.F., Javitz H., Carmelli D., et al. Prospective assessment after pediatric cardiac ablation: demographics, medical profiles, and initial outcomes. J Cardiovasc Electrophysiol. 2004;15:759–770. doi: 10.1046/j.1540-8167.2004.03645.x. [DOI] [PubMed] [Google Scholar]
- 9.Kugler J.D., Danford D.A., Houston K., Felix G. Radiofrequency catheter ablation for paroxysmal supraventricular tachycardia in children and adolescents without structural heart disease. Pediatric EP Society, Radiofrequency Catheter Ablation Registry. Am J Cardiol. 1997;80:1438–1443. doi: 10.1016/s0002-9149(97)00736-4. [DOI] [PubMed] [Google Scholar]
- 10.Kugler J.D., Danford D.A., Houston K.A. Pediatric Radiofrequency Ablation Registry of the Pediatric Radiofrequency Ablation Registry of the Pediatric Electrophysiology Society. Pediatric radiofrequency catheter ablation registry success, fluoroscopy time, and complication rate for supraventricular tachycardia: comparison of early and recent eras. J Cardiovasc Electrophysiol. 2002;13:336–341. doi: 10.1046/j.1540-8167.2002.00336.x. [DOI] [PubMed] [Google Scholar]
- 11.Oddsson H., Walfridsson H., Edvardsson N. Perception and documentation of arrhythmias after successful radiofrequency catheter ablation of accessory pathways. Ann Noninvasive Electrocardiol. 2001;6:216–221. doi: 10.1111/j.1542-474X.2001.tb00111.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fremed M.A., Silver E.S., Joong A., Liberman M., Liberman L. Long-term patient experience following acutely successful ablation of supraventricular tachycardia substrate in children. Pediatr Cardiol. 2021;42:109–115. doi: 10.1007/s00246-020-02459-z. [DOI] [PubMed] [Google Scholar]
- 13.Carberry T., Balmert L.C., Stanley S., et al. Persistence of palpitations after slow pathway modification for AVNRT in young people. Pediatr Cardiol. 2021;42:590–596. doi: 10.1007/s00246-020-02519-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kimman G.J., Theuns D.A., Janse P.A., et al. One-year follow-up in a prospective, randomized study comparing radiofrequency and cryoablation of arrhythmias in Koch's triangle: clinical symptoms and event recording. Europace. 2006;8:592–595. doi: 10.1093/europace/eul051. [DOI] [PubMed] [Google Scholar]
- 15.Zimetbaum P., Kim K.Y., Ho K.K., et al. Utility of patient-activated cardiac event recorders in general clinical practice. Am J Cardiol. 1997;79:371–372. doi: 10.1016/s0002-9149(96)00766-7. [DOI] [PubMed] [Google Scholar]
- 16.Barsky A.J., Ahern D.K., Brener J., et al. Palpitations and cardiac awareness after heart transplantation. Psychosom Med. 1998;60:557–562. doi: 10.1097/00006842-199809000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Barsky A.J., Cleary P.D., Barnett M.C., Christiansen C.L., Ruskin J.N. The accuracy of symptom reporting by patients complaining of palpitations. Am J Med. 1994;97:214–221. doi: 10.1016/0002-9343(94)90003-5. [DOI] [PubMed] [Google Scholar]
- 18.Eichler S., Katkin E.S. The relationship between cardiovascular reactivity and heartbeat detection. Psychophysiology. 1994;31:229–234. doi: 10.1111/j.1469-8986.1994.tb02211.x. [DOI] [PubMed] [Google Scholar]
- 19.Katkin E.S., Morell M.A., Goldband S., Bernstein G.L., Wise J.A. Individual differences in heartbeat discrimination. Psychophysiology. 1982;19:160–166. doi: 10.1111/j.1469-8986.1982.tb02538.x. [DOI] [PubMed] [Google Scholar]
- 20.Schandry R., Bestler M., Montoya P. On the relation between cardiodynamics and heartbeat perception. Psychophysiology. 1993;30:467–474. doi: 10.1111/j.1469-8986.1993.tb02070.x. [DOI] [PubMed] [Google Scholar]
- 21.Kang E.H., Yu B.H. Anxiety and beta-adrenergic receptor function in a normal population. Prog Neuropsychopharmacol Biol Psychiatry. 2005;29:733–737. doi: 10.1016/j.pnpbp.2005.04.027. [DOI] [PubMed] [Google Scholar]
- 22.White K.S., Craft J.M., Gervino E.V. Anxiety and hypervigilance to cardiopulmonary sensations in non-cardiac chest pain patients with and without psychiatric disorders. Behav Res Ther. 2010;48:394–401. doi: 10.1016/j.brat.2010.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Katon W., Lin E.H., Kroenke K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen Hosp Psychiatry. 2007;29:147–155. doi: 10.1016/j.genhosppsych.2006.11.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.