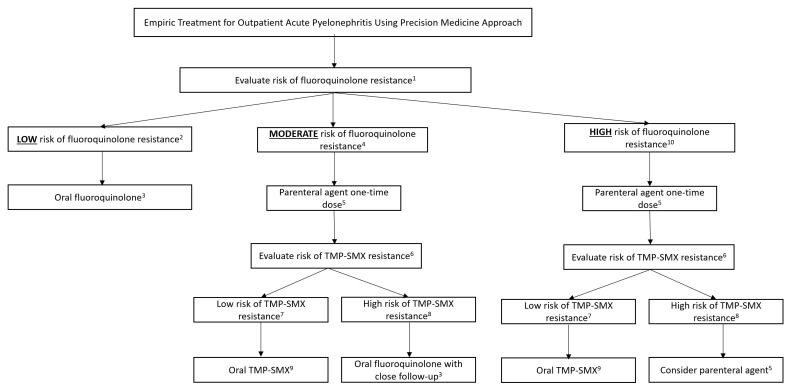
Figure 2.
Precision-medicine-based therapy of acute pyelonephritis. 1 See fluoroquinolone risk score in Table 1. 2 Low risk of fluoroquinolone resistance defined as fluoroquinolone resistance score < 2. 3 Levofloxacin 750 mg PO Q24 h or ciprofloxacin 500 mg PO Q12 h for 5–7 days. 4 Moderate risk of fluoroquinolone resistance defined as risk score of 2. 5 Parenteral agents to include: IV/IM ceftriaxone 1G or consolidated 24 h dose of tobramycin or amikacin. 6 See TMP-SMX risk score in Table 2. 7 Low risk of TMP-SMX resistance defined as risk score < 1. 8 High risk of TMP-SMX resistance defined as risk score ≥ 1. 9 1 Double-strength TMP-SMX PO Q12 h × 14 days. 10 High risk of fluoroquinolone resistance defined as fluoroquinolone resistance score > 2. If there is a high risk of fluoroquinolone resistance and a high risk of TMP-SMX resistance, consider evaluating for risk of ESBL (Table 3) and Pseudomonas aeruginosa. If there is concern for Pseudomonas aeruginosa, consider utilizing anti-pseudomonal agent such as meropenem, piperacillin/tazobactam, cefepime, tobramycin, or amikacin. If ESBL prediction score is <3, and there is no concern for P. aeruginosa, utilize IV/IM ceftriaxone. If ESBL prediction score is ≥3, utilize IV/IM ertapenem or an aminoglycoside. Tobramycin or amikacin are the only recommended aminoglycosides due to the recent change in recommendations by CLSI to not utilize gentamicin as a treatment option for P. aeruginosa [27].