Abstract
Background and Objectives
Previous studies have reported a substantial between-country variation in the case fatality rates (CFRs) of aneurysmal subarachnoid hemorrhage (SAH). However, contrary to comparisons among countries, nationwide comparisons within countries that focus on populations with equal access to health care and include out-of-hospital deaths in analyses are lacking. Thus, we aimed to investigate whether the SAH CFRs vary between geographic regions within Finland.
Methods
We identified all hospitalized and nonhospitalized (sudden-death) cases with aneurysmal SAH in Finland during 1998–2017 through 2 externally validated nationwide registers. According to the municipality of residence, we divided the cases with SAH into 5 geographic regions: Southern, Central, Western, Northern, and Eastern Finland, each served by a University Central Hospital with a neurosurgical service. In addition to overall 30-day CFRs, we computed sudden death rates and 30-day CFRs after hospitalization for each region. Using logistic and Poisson regression models, we calculated regional age-adjusted, sex-adjusted, and year-adjusted odds ratios and annual percent changes with 95% CIs for CFRs.
Results
During 1998–2017, we identified a total of 9,443 cases with SAH, of which 3,484 (36.9%) occurred in Southern Finland. In comparison with the overall 30-day CFR of Southern Finland (35.1%), the age-adjusted, sex-adjusted, and study year–adjusted odds of SAH death were 32% (16%–50%) higher in Central Finland (42.7%), 39% (23%–58%) higher in Eastern Finland (43.4%), and 52% (33%–74%) higher in Western Finland (47.1%). The regional differences were present among both sexes, in all age groups, in sudden death rates, and in 30-day CFRs after hospitalization. Between 1998 and 2017, the overall 30-day CFRs decreased in Central (2.4% [1.0%–3.8%] per year) and Southern (1.2% [0.2%–2.2%] per year) Finland, whereas CFRs remained stable in the other regions. In the last 4 years of the study period (2014–2017), Southern Finland had the lowest 30-day CFR (16.5%) among hospitalized patients.
Discussion
SAH CFRs seem to vary significantly even within a country with relatively equal access to health care. Future studies with detailed individual-level data are needed to explore whether health inequities explain the reported findings.
Introduction
Despite the improvements in early diagnostic and treatment modalities, it is estimated that approximately 40% of patients with subarachnoid hemorrhage (SAH) die within the first month after the event.1 However, the case fatality rate (CFR) estimations have varied from 13% to 67% between studies from different countries.1 Because most of this variation is likely attributed to differences in health care structures and study methodologies (e.g., variation in including out-of-hospital deaths that account for more than 50% of fatal SAHs),2 it has been challenging to provide reliable evidence about the true country-specific SAH CFRs and their within-country and between-country differences.
Within-country regional variation in the incidence of SAH is substantial.3-5 Consequently, population-based national incidence estimates extrapolated from studies based on small geographical areas do not represent nationwide figures. Similarly, many CFR estimates are based on small geographical areas,1,6 though it is not known whether these population-based CFRs correspond to nationwide estimates. Therefore, our epidemiologic understanding about SAH CFRs is somewhat compromised, which may lead to erroneous health care policy decisions. To investigate whether SAH CFRs differ in various geographical areas within a country, we conducted a nationwide study including both hospitalized and nonhospitalized sudden-death cases with SAH in Finland during 1998–2017. We hypothesized that substantial variation exists within Finland in SAH CFRs.
Methods
Standard Protocol Approvals, Registrations, and Patient Consents
This study was approved by the Finnish Institute for Health and Welfare (approval number: THL/3136/14.06.00/2021) and followed the ethical principles of the Declaration of Helsinki. According to the Finnish legislation, register-based studies that use pseudonymized datasets do not require informed consent from the patients.
Case Ascertainment
The register-based case ascertainment and its external validation have been described in detail in an earlier study.3 In brief, we used the national Care Register for Health Care (governed by the Finnish Institute for Health and Welfare) and the national Cause of Death Register (CDR) (governed by Statistics Finland) to identify all first-ever nonfatal and fatal cases with SAH in Finland during 1998–2017. We included cases with a primary diagnosis of aneurysmal SAH (ICD-10 I60.0–I60.6) and excluded cases with nonaneurysmal origin (ICD I60.7–I60.9) and cases with a secondary diagnosis of cerebral arteriovenous malformation (ICD-10 Q28.0–Q28.9) or intracranial injury (ICD-10 S06.0–S06.9). For hospitalized events, we extracted data on the type of hospital admission, the specialty of admission, the length of hospitalization, and 365-day all-cause mortality after SAH to improve the accuracy of our register-based search. In addition to deaths of hospitalized patients with SAH, we also included nonhospitalized cases with SAH who died outside of hospitals, in an ambulance, or in emergency departments (defined as sudden-death SAHs). According to Finnish legislation, such unexpected deaths occurring outside of hospital wards must undergo a thorough postmortem examination for the cause of death determination, which improves the identification coverage of sudden-death SAHs in Finland. For both hospitalized and nonhospitalized cases, we gathered information about sex, age, and residency (municipality code) during SAH. In comparison with an external hospital-based aneurysm register, governed manually by the Helsinki University Hospital since 1937,7 our register-based case ascertainment for hospitalized patients had a positive predictive value (PPV) of 99.8%,3 whereas the PPV for fatal SAH events of CDR have been estimated to be 97%.8
Outcome Measures and Geographical Regions of Finland
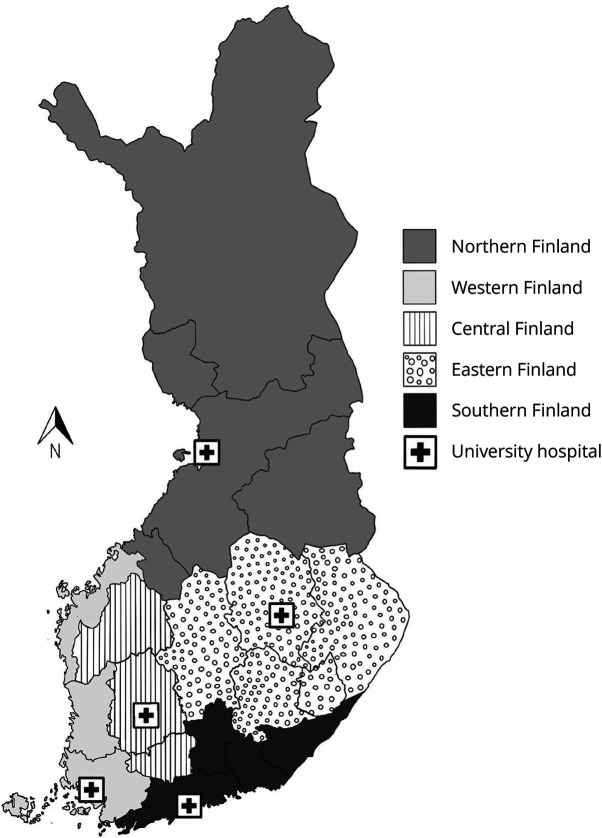
We defined the overall 30-day CFR as the proportion of cases with SAH dying before hospitalization or during the first 30 days after reaching hospital wards. To examine whether the possible within-country differences were attributed to the varying proportions of nonhospitalized or hospitalized SAH deaths, we also defined sudden-death SAHs and 30-day CFRs for hospitalized patients with SAH. All deaths were included in the 30-day case fatalities, regardless of their cause, representing the so-called all-cause CFRs. Based on the patient's residency (municipality code) during SAH, we divided the identified cases with SAH and CFRs into 5 geographical regions, corresponding to the 5 university hospital catchment areas (UHCAs) covering the whole country (in total, 309 municipalities and 21 hospital districts of Finland): (1) Southern Finland (Helsinki UHCA), (2) Central Finland (Tampere UHCA), (3) Western Finland (Turku UHCA), (4) Northern Finland (Oulu UHCA), and (5) Eastern Finland (Kuopio UHCA) (Figure 1). Cases with SAH without a municipality code (people not registered as residents in Finland, that is, short-term workers and visitors) were excluded.
Figure 1. The 5 Geographic Regions of Finland According to the UHCAs.
UHCAs are composed of several regional hospital districts, each with 1 central hospital responsible for specialized care. UHCA = university hospital catchment area.
Statistical Analyses
In addition to calculating the nationwide and regional sudden death rates, 30-day CFRs for hospitalized patients, and overall 30-day CFRs, we also computed the rates separately for men and women and by age classes (younger than 40 years; 40–64 years; 65 years or older). Furthermore, we used a logistic regression model to calculate age-adjusted, sex-adjusted, and year-adjusted odds ratios and 95% CIs for fatal SAHs by geographic regions. We used a Poisson regression model to calculate the average annual percent changes for the sudden death rates, 30-day CFRs of hospitalized patients, and overall 30-day CFRs to examine the age-adjusted and sex-adjusted time-dependent trends of regional case fatalities of SAH. Southern Finland, which has the largest population, served as the reference category in all analyses. Last, we reported the average subgroup-specific CFRs and their changes between the first (1998–2001) and last 4 years (2014–2017) of our study period by region, sex, and 10-year age group.
Data Availability
Due to legislative data transfer restrictions imposed by the European Union, the used dataset is not available for public use. However, qualified investigators can request access to the data from the Finnish Health and Social Data Permit Authority (findata.fi/en/).
Results
General Characteristics
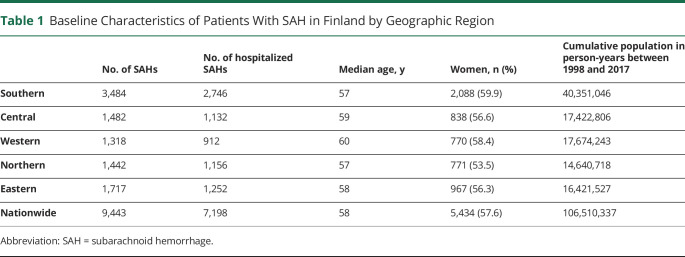
We identified a total of 9,443 cases with SAH between 1998 and 2017. Most of the cases with SAH occurred among women in all regions (range from 54% in Northern Finland to 60% in Southern Finland), whereas the median age during SAH was highest in Western Finland (age 60 years) and lowest in Southern and Northern Finland (age 57 years in both regions) (Table 1). The overall caseload in Southern Finland was more than 2-fold in comparison with that in other geographical regions and even 3-fold when compared with that in Western Finland, which had the lowest number of cases with SAH (Table 1). As also previously reported,3 Southern Finland consisted of 38% of the total Finnish population during our study period (Table 1), whereas the population was the smallest in Northern and Eastern Finland where the incidence rates of SAH were the highest.3
Table 1.
Baseline Characteristics of Patients With SAH in Finland by Geographic Region
| No. of SAHs | No. of hospitalized SAHs | Median age, y | Women, n (%) | Cumulative population in person-years between 1998 and 2017 | |
| Southern | 3,484 | 2,746 | 57 | 2,088 (59.9) | 40,351,046 |
| Central | 1,482 | 1,132 | 59 | 838 (56.6) | 17,422,806 |
| Western | 1,318 | 912 | 60 | 770 (58.4) | 17,674,243 |
| Northern | 1,442 | 1,156 | 57 | 771 (53.5) | 14,640,718 |
| Eastern | 1,717 | 1,252 | 58 | 967 (56.3) | 16,421,527 |
| Nationwide | 9,443 | 7,198 | 58 | 5,434 (57.6) | 106,510,337 |
Abbreviation: SAH = subarachnoid hemorrhage.
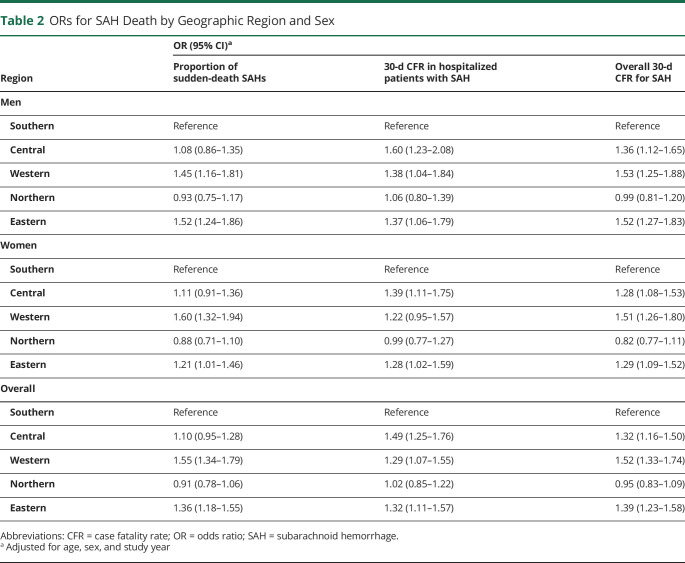
Case Fatality of SAH by Geographic Region
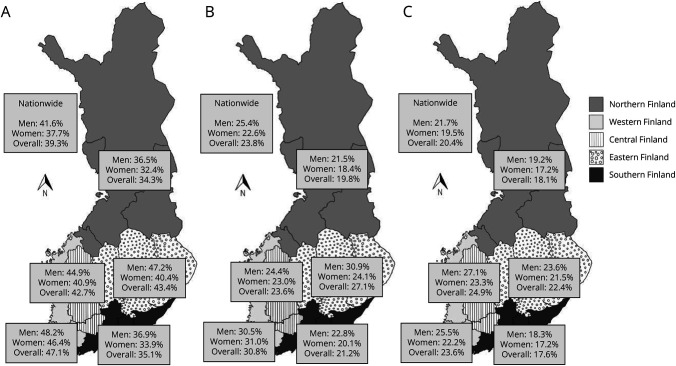
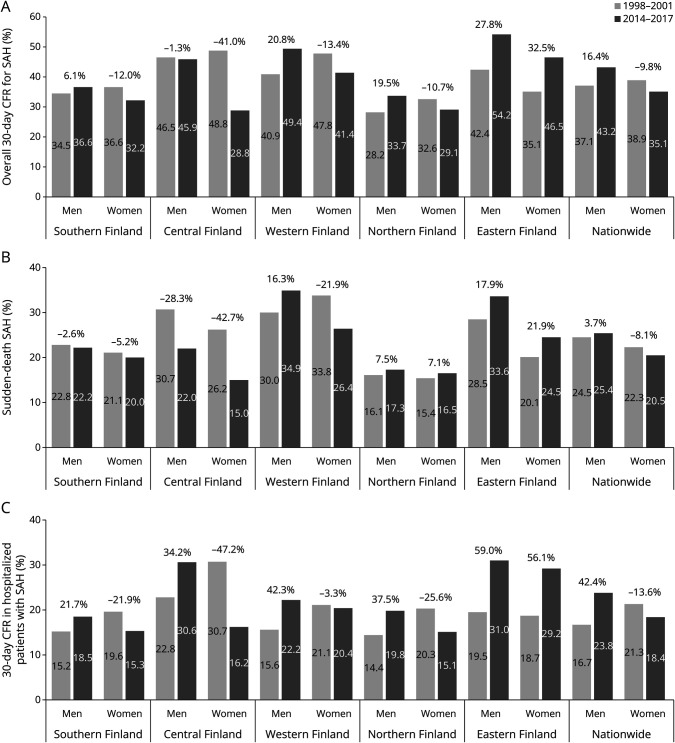
We found that the highest overall 30-day CFR (including both nonhospitalized and hospitalized cases) occurred in Western Finland (47.1%), while the lowest rates were found in Northern (34.3%) and Southern Finland (35.1%) (Figure 2A). After adjusting the rates for age, sex, and study year, the odds of SAH death within 30 days were 52% (33%–74%) higher in Western Finland, 32% (16%–50%) higher in Central Finland, and 39% (23%–58%) higher in Eastern Finland when compared with the rates of Southern Finland (Table 2, Figure 2A). When analyzing nonhospitalized and hospitalized cases separately, the highest proportions of sudden deaths were observed in Western Finland (30.8%), while the 30-day CFRs of hospitalized patients were the highest in Central Finland (24.9%); Southern and Northern Finland had the lowest rates for both categories of fatalities (Figure 2, B and C). Similar regional differences were observed in men and women (Table 2, Figure 2, B and C) and in all age groups (eTables 1 and 2, links.lww.com/WNL/D134).
Figure 2. CFRs of SAH by Geographic Region Between 1998 and 2017 in Finland.
(A) Overall 30-day CFR for SAH, (B) sudden-death SAHs, and (C) 30-day CFR in hospitalized patients with SAH. CFR = case fatality rate; SAH = subarachnoid hemorrhage.
Table 2.
ORs for SAH Death by Geographic Region and Sex
| Region | OR (95% CI)a | ||
| Proportion of sudden-death SAHs | 30-d CFR in hospitalized patients with SAH | Overall 30-d CFR for SAH | |
| Men | |||
| Southern | Reference | Reference | Reference |
| Central | 1.08 (0.86–1.35) | 1.60 (1.23–2.08) | 1.36 (1.12–1.65) |
| Western | 1.45 (1.16–1.81) | 1.38 (1.04–1.84) | 1.53 (1.25–1.88) |
| Northern | 0.93 (0.75–1.17) | 1.06 (0.80–1.39) | 0.99 (0.81–1.20) |
| Eastern | 1.52 (1.24–1.86) | 1.37 (1.06–1.79) | 1.52 (1.27–1.83) |
| Women | |||
| Southern | Reference | Reference | Reference |
| Central | 1.11 (0.91–1.36) | 1.39 (1.11–1.75) | 1.28 (1.08–1.53) |
| Western | 1.60 (1.32–1.94) | 1.22 (0.95–1.57) | 1.51 (1.26–1.80) |
| Northern | 0.88 (0.71–1.10) | 0.99 (0.77–1.27) | 0.82 (0.77–1.11) |
| Eastern | 1.21 (1.01–1.46) | 1.28 (1.02–1.59) | 1.29 (1.09–1.52) |
| Overall | |||
| Southern | Reference | Reference | Reference |
| Central | 1.10 (0.95–1.28) | 1.49 (1.25–1.76) | 1.32 (1.16–1.50) |
| Western | 1.55 (1.34–1.79) | 1.29 (1.07–1.55) | 1.52 (1.33–1.74) |
| Northern | 0.91 (0.78–1.06) | 1.02 (0.85–1.22) | 0.95 (0.83–1.09) |
| Eastern | 1.36 (1.18–1.55) | 1.32 (1.11–1.57) | 1.39 (1.23–1.58) |
Abbreviations: CFR = case fatality rate; OR = odds ratio; SAH = subarachnoid hemorrhage.
Adjusted for age, sex, and study year
Time-Dependent Trends of Regional Case Fatality of SAH
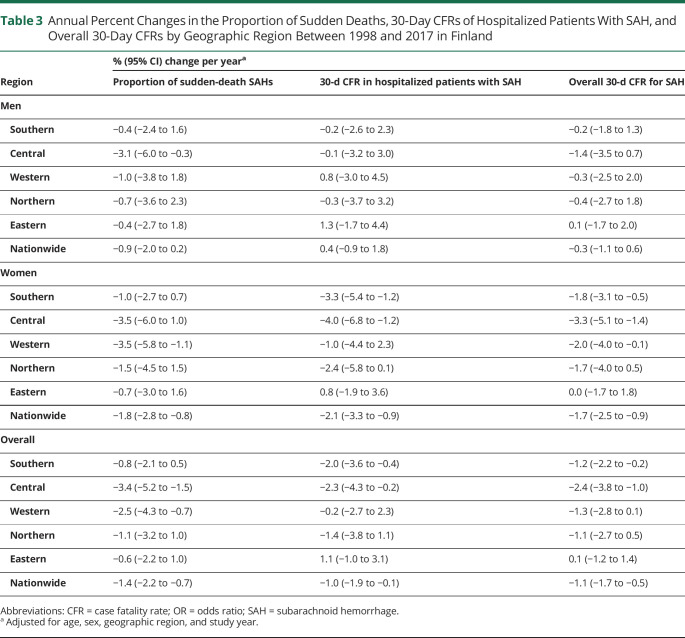
Among the 5 regions, the annual age-adjusted and sex-adjusted overall 30-day CFRs decreased the most in Southern (1.2% [0.2%–2.2%] per year) and Central Finland (2.4% [1.0%–3.8%] per year), while no obvious trend was observed for the other regions during 1998–2017 (Table 3). In hospitalized patients, decreasing 30-day CFRs were found among women in Southern (3.3% [1.2%–5.4%] per year) and Central Finland (4.0% [1.2%–6.8%] per year), while no significant change was observed for men in any region (Table 3). By age groups, the largest overall 30-day CFR decreases were reported in middle-aged cases in Central (3.1% [1.0%–5.2%] per year) and Southern Finland (1.6% [0.1%–2.9%] per year) (eTable 3, links.lww.com/WNL/D134).
Table 3.
Annual Percent Changes in the Proportion of Sudden Deaths, 30-Day CFRs of Hospitalized Patients With SAH, and Overall 30-Day CFRs by Geographic Region Between 1998 and 2017 in Finland
| Region | % (95% CI) change per yeara | ||
| Proportion of sudden-death SAHs | 30-d CFR in hospitalized patients with SAH | Overall 30-d CFR for SAH | |
| Men | |||
| Southern | −0.4 (−2.4 to 1.6) | −0.2 (−2.6 to 2.3) | −0.2 (−1.8 to 1.3) |
| Central | −3.1 (−6.0 to −0.3) | −0.1 (−3.2 to 3.0) | −1.4 (−3.5 to 0.7) |
| Western | −1.0 (−3.8 to 1.8) | 0.8 (−3.0 to 4.5) | −0.3 (−2.5 to 2.0) |
| Northern | −0.7 (−3.6 to 2.3) | −0.3 (−3.7 to 3.2) | −0.4 (−2.7 to 1.8) |
| Eastern | −0.4 (−2.7 to 1.8) | 1.3 (−1.7 to 4.4) | 0.1 (−1.7 to 2.0) |
| Nationwide | −0.9 (−2.0 to 0.2) | 0.4 (−0.9 to 1.8) | −0.3 (−1.1 to 0.6) |
| Women | |||
| Southern | −1.0 (−2.7 to 0.7) | −3.3 (−5.4 to −1.2) | −1.8 (−3.1 to −0.5) |
| Central | −3.5 (−6.0 to 1.0) | −4.0 (−6.8 to −1.2) | −3.3 (−5.1 to −1.4) |
| Western | −3.5 (−5.8 to −1.1) | −1.0 (−4.4 to 2.3) | −2.0 (−4.0 to −0.1) |
| Northern | −1.5 (−4.5 to 1.5) | −2.4 (−5.8 to 0.1) | −1.7 (−4.0 to 0.5) |
| Eastern | −0.7 (−3.0 to 1.6) | 0.8 (−1.9 to 3.6) | 0.0 (−1.7 to 1.8) |
| Nationwide | −1.8 (−2.8 to −0.8) | −2.1 (−3.3 to −0.9) | −1.7 (−2.5 to −0.9) |
| Overall | |||
| Southern | −0.8 (−2.1 to 0.5) | −2.0 (−3.6 to −0.4) | −1.2 (−2.2 to −0.2) |
| Central | −3.4 (−5.2 to −1.5) | −2.3 (−4.3 to −0.2) | −2.4 (−3.8 to −1.0) |
| Western | −2.5 (−4.3 to −0.7) | −0.2 (−2.7 to 2.3) | −1.3 (−2.8 to 0.1) |
| Northern | −1.1 (−3.2 to 1.0) | −1.4 (−3.8 to 1.1) | −1.1 (−2.7 to 0.5) |
| Eastern | −0.6 (−2.2 to 1.0) | 1.1 (−1.0 to 3.1) | 0.1 (−1.2 to 1.4) |
| Nationwide | −1.4 (−2.2 to −0.7) | −1.0 (−1.9 to −0.1) | −1.1 (−1.7 to −0.5) |
Abbreviations: CFR = case fatality rate; OR = odds ratio; SAH = subarachnoid hemorrhage.
Adjusted for age, sex, geographic region, and study year.
Subgroup-Specific CFRs and Their Changes Between 1998–2001 and 2014–2017
Between the first 4 (1998–2001) and last 4 years (2014–2017), the overall 30-day CFRs decreased in Southern (5.3%; from 35.7% to 33.8%) and Central Finland (25.1%; from 47.9% to 35.9%) and increased in Eastern Finland (30.2%; from 38.4% to 50.0%) (eFigure 1, links.lww.com/WNL/D132, Figure 3A). By sex, the proportion of sudden deaths decreased the most among women (42.7%; from 26.2% to 15.0%) and men (28.3%; from 30.7% to 22.0%) in Central Finland, while the largest increases were found among women (21.9%; from 20.1% to 24.5%) and men (17.9%; from 28.5% to 33.6%) in Eastern Finland (Figure 3B). The 30-day CFR of hospitalized patients declined among women in Southern (21.9%; from 19.6% to 15.3%), Northern (25.6%; from 20.3% to 15.1%), and Central Finland (47.2%; from 30.7% to 16.2%), whereas large increases were observed among men in all regions (42.4%; from 16.7% to 23.8%) and among women in Eastern Finland (56.1%; from 18.7% to 29.2%) (Figure 3C). By age, sudden death rates decreased mostly among those younger than 70 years in Southern, Central, and Northern Finland, while the largest increases were observed among those younger than 70 years in Eastern and Western Finland (eFigure 2). In hospitalized patients, the 30-day CFR decreased among those younger than 50 years in all regions, but increased among those aged 60 years or older in Western, Northern, and Eastern Finland (eFigure 3).
Figure 3. Four-Year Average CFR Changes of SAH Between 1998–2001 and 2014–2017 by Sex and Geographic Region.
(A) Overall 30-day CFR for SAH, (B) sudden-death SAHs, and (C) 30-day CFR in hospitalized patients with SAH. CFR = case fatality rate; SAH = subarachnoid hemorrhage.
Discussion
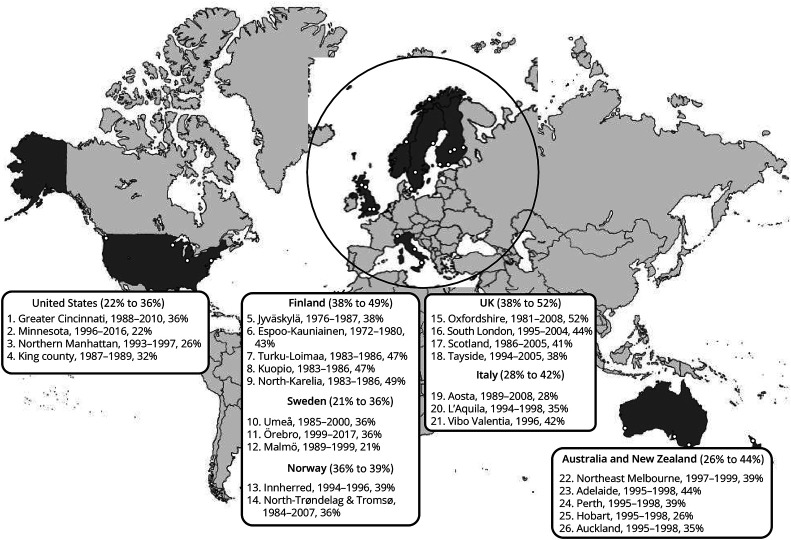
In this nationwide register-based study, we found that case fatality of SAH varied substantially by major geographic areas within Finland over 2 decades (1998–2017). Specifically, the odds of death within 30 days after SAH were 43% greater in Western, Central, and Eastern Finland (ranging from 43% to 47%) compared with those in Southern and Northern Finland (ranging from 34% to 35%) combined. Such substantial variation in a homogeneous population with relatively equal access to health care services is unexpected and highlights the importance of considering geographical differences when generalizing regional CFR to represent nationwide or worldwide figures. However, because the previously reported worldwide CFR variation is more than 4-fold (ranging from 13% to 67%)1 compared with the variation of our study (ranging from 34% to 47%), it is likely that a large proportion of previously reported differences can be attributed to the differences in study methodologies, not so much to the differences in true CFRs. Therefore, between-country comparisons of SAH CFRs should be performed with extreme caution, especially if used for evaluating the quality of treatment between different centers and regions.
In addition to regional differences in average CFRs, we observed substantial variation in the time-dependent trends of case fatality of SAH. Between 1998 and 2017, overall CFRs decreased in Southern and Central Finland, particularly among women, while stable trends were seen in other geographical regions. Notably, the SAH CFRs of hospitalized women decreased by 25% (from 20% to 15%) in Southern Finland, and this trend was even more pronounced in women younger than 60 years who experienced a 39% decrease (from 18% to 11%) during the study period. When compared with more historical hospital-based CFRs reported in Southern Finland in the 1950s9 (46% CFR) and 1970s10 (40% CFR), the CFRs of hospitalized patients with SAH have decreased by approximately two-thirds; currently, they are only approximately 17% in Southern Finland. Notably, these patients also include those who have been admitted to the intensive care unit as possible organ donors (very poor prognosis). The reported CFRs among hospitalized patients with SAH in Southern Finland seem to be lower in comparison with previously reported nationwide hospital-based figures from Australia (25%, 2017–2018),11 Czech Republic (18%, 2013–2015),12 Norway (22%, 2008–2014), France (19%, 2015),13 and the United Kingdom (25%, 2008–2010).14 The percentage of hospitalized patients with SAH who were organ donors in each country is unknown. Taken together, case fatality of SAH has decreased, especially among hospitalized patients with SAH in Southern and Central Finland. In fact, currently less than one-fifth of hospitalized patients with SAH die within 30 days after hospitalization.
Several factors related to patient characteristics and SAH care may contribute to the geographical variation and time-dependent changes in SAH CFRs.15 For instance, the regions with the highest CFRs—Western, Central, and Eastern Finland—also had the highest median age during SAH (Spearman correlation ρ = 0.60, p = 0.01) (eTable 4, links.lww.com/WNL/D134). Similarly, the mean age of hospitalized patients with SAH and the proportion of people who live alone16 (significant risk factors of fatal SAH17,18) increased the least in Southern and Central Finland during the study period (eFigure 4, links.lww.com/WNL/D132). Moreover, CFRs after hospitalization were the lowest in the regions with the highest hospital caseload (Spearman correlation ρ = −0.80, p = 0.13) (eTable 4). Previous studies have reported a similar inverse relationship between hospital caseload and SAH CFR.19,20 In terms of modifiable risk factors of SAH death, the prevalence of daily smokers21,22 and the proportion of adults entitled to special refunds for hypertension medication23 decreased the most in Southern and Central Finland, while the decline was more modest in the other regions (eFigure 4). In addition, part of the differences may attribute to regional differences in the availability of neurocritical care, SAH diagnostics, or other aspects of SAH patient management though the treatment of patients with SAH should be based on general guidelines24 in each of the 5 university hospitals in Finland. Moreover, because each Finnish neurosurgical unit has its own specialized cerebrovascular neurosurgeon(s) and interventional neuroradiologist(s), acute-phase referrals to another Finnish neurosurgical unit are rarely done.
Because no previous nationwide study has investigated the within-country differences of overall SAH case fatality (also including sudden-death SAHs), direct comparison with published studies is not feasible. Nevertheless, the difference in the odds of SAH death between regions with the largest and smallest overall CFRs in this study (70%; Western vs Northern Finland) was relatively similar compared with the CFR variation in previous Nordic regional studies from Finland,25-27 Sweden,28-30 and Norway31,32 (ranging from 14% to 112%) (Figure 4). In comparison with the Nordic countries, the within-country variations in region-specific studies from larger countries such as the United Kingdom,33-36 the United States,37-40 Australia and New Zealand,41,42 and Italy43-47 have understandably been greater (ranging from 70% to 124%) (Figure 4). Besides these population-based studies, some hospital-based studies have reported within-country differences in the in-hospital mortality of SAH.15,48 Notably, a recent US study15 reported that differences in the admission severity of illness, nimodipine use, and aneurysm repair may have contributed to the modest regional variation in in-hospital mortality. Similar to our findings, within-country differences in CFRs have also been observed for other cardiovascular diseases, such as acute myocardial infarction,49 intracerebral hemorrhage,50 and ischemic stroke.50
Figure 4. Regional Differences in 1-Month Case Fatality Rates of Subarachnoid Hemorrhage in Population-Based Studies in the CT Scan Era.
References are presented in the supplement (links.lww.com/WNL/D133).
In comparison with previous literature, this study has some strengths. First, because all sudden and unexpected out-of-hospital deaths in Finland must undergo an autopsy for accurate determination of cause of death, we were able to comprehensively include sudden-death SAHs (covering more than half of the SAH deaths). Second, due to a long study period of 20 years, we were able to identify nearly 10,000 SAH events, which in turn enabled us to perform regional analyses in detailed subgroups. Third, because Finland has a taxation-based health care system that provides an equal tertiary care for its inhabitants, it is unlikely that our findings are strongly distorted by patients' socioeconomic status.
In addition to these possible strengths, this study also has shortcomings. Although we had access to nationwide registers containing information on population demographics and risk factors (eTable 4, links.lww.com/WNL/D134, eFigure 4, links.lww.com/WNL/D132),16,23 we had no individual-level data, and therefore, we were not able to address whether the regional CFR variation was attributed to the differences in patient characteristics, environmental risk factors, or diagnostics and treatment modalities of SAH. For the same reason, we did not have detailed data about all the hospitals involved in the diagnostics and treatment of each patient with SAH or the exact location of where patients with SAH were deceased. Thus, we decided to divide patients with SAH according to their municipality of residence, which may, however, limit the generalizability of our findings for hospital comparison. On the contrary, because even 90% of the hospitalized patients were first admitted and therefore most likely treated in the same UHCA as their residence (eFigure 5), and the regional differences of CFRs among hospitalized patients did not differ when stratifying the patients by their initial treatment unit (eTable 5) and by their residence (Figure 2, Tables 2 and 3), our findings may also reflect SAH outcome differences between different Finnish hospitals. Nevertheless, future studies with detailed individual-level data are needed to determine which factors explain the geographic differences of SAH CFRs in Finland. Last, the hospital district of Vaasa was transferred from Central Finland to Western Finland in 2013, so the results may have been subject to some slight error. However, because residents of the Vaasa district contributed only 220 (2.3%) of all cases with SAH, the regional change probably has a negligible effect on our conclusions.
In conclusion, our findings suggest that SAH CFRs and their trends vary substantially between different geographic regions within a country. Therefore, we do not recommend using regional SAH CFR averages and trends to represent nationwide figures or to compare the quality of treatment or patient morbidity between countries. Future studies with individual-level data are needed to investigate whether changes in modifiable risk factors, hospital care, or health inequities would contribute to the regional differences.
Disclosure
A. Asikainen has been supported by the Juho Vainio Foundation, the Päivikki and Sakari Sohlberg Foundation, the Finnish Brain Foundation, the Finnish Medical Foundation, the Biomedicum Helsinki Foundation, the Maire Taponen Foundation, and the Paulo Foundation. M. Korja reports no disclosures relevant to the manuscript. J. Kaprio has been supported by the Academy of Finland (grant number 352792). I. Rautalin has received personal research grants from the Sigrid Juselius Foundation, the Finnish Medical Foundation, the Sakari Alhopuro Foundation, the Finnish Foundation for Cardiovascular Research, and the Maud Kuistila Foundation. Go to Neurology.org/N for full disclosures.
Acknowledgment
The authors thank Jacquelin De Faveri for the language revision.
Glossary
- CDR
Cause of Death Register
- CFR
case fatality rate
- ICD-10
International Classification of Diseases, 10th Revision
- PPV
positive predictive value
- SAH
subarachnoid hemorrhage
- UHCA
university hospital catchment area
Appendix. Authors
| Name | Location | Contribution |
| Aleksanteri Asikainen, BM | Department of Neurosurgery, University of Helsinki and Helsinki University Hospital; Department of Public Health, University of Helsinki, Finland | Drafting/revision of the article for content, including medical writing for content; study concept or design; and analysis or interpretation of data |
| Miikka Korja, MD, PhD | Department of Neurosurgery, University of Helsinki and Helsinki University Hospital, Finland | Drafting/revision of the article for content, including medical writing for content; major role in the acquisition of data; study concept or design; and analysis or interpretation of data |
| Jaakko Kaprio, MD, PhD | Institute for Molecular Medicine FIMM, University of Helsinki, Finland | Drafting/revision of the article for content, including medical writing for content; major role in the acquisition of data; study concept or design; and analysis or interpretation of data |
| Ilari Rautalin, MD, PhD | Department of Neurosurgery, University of Helsinki and Helsinki University Hospital, Finland; National Institute for Stroke and Applied Neurosciences, Auckland University of Technology, New Zealand | Drafting/revision of the article for content, including medical writing for content; major role in the acquisition of data; study concept or design; and analysis or interpretation of data |
Footnotes
Editorial, page 869
Study Funding
No targeted funding reported.
References
- 1.Mahlamaki K, Rautalin I, Korja M. Case fatality rates of subarachnoid hemorrhage are decreasing with substantial between-country variation: a systematic review of population-based studies between 1980 and 2020. Neuroepidemiology. 2022;56(6):402-412. doi: 10.1159/000526983 [DOI] [PubMed] [Google Scholar]
- 2.Korja M, Kaprio J. Controversies in epidemiology of intracranial aneurysms and SAH. Nat Rev Neurol. 2016;12(1):50-55. doi: 10.1038/nrneurol.2015.228 [DOI] [PubMed] [Google Scholar]
- 3.Rautalin I, Lindbohm JV, Kaprio J, Korja M. Substantial within-country variation in the incidence of subarachnoid hemorrhage: a nationwide Finnish study. Neurology. 2021;97(1):e52-e60. doi: 10.1212/WNL.0000000000012129 [DOI] [PubMed] [Google Scholar]
- 4.Koffijberg H, Buskens E, Granath F, et al. Subarachnoid haemorrhage in Sweden 1987-2002: regional incidence and case fatality rates. J Neurol Neurosurg Psychiatry. 2008;79(3):294-299. doi: 10.1136/jnnp.2007.123901 [DOI] [PubMed] [Google Scholar]
- 5.Lindekleiv HM, Njølstad I, Ingebrigtsen T, Mathiesen EB. Incidence of aneurysmal subarachnoid hemorrhage in Norway, 1999-2007. Acta Neurol Scand. 2011;123(1):34-40. doi: 10.1111/j.1600-0404.2010.01336.x [DOI] [PubMed] [Google Scholar]
- 6.Nieuwkamp DJ, Setz LE, Algra A, Linn FHH, de Rooij NK, Rinkel GJE. Changes in case fatality of aneurysmal subarachnoid haemorrhage over time, according to age, sex, and region: a meta-analysis. Lancet Neurol. 2009;8(7):635-642. doi: 10.1016/S1474-4422(09)70126-7 [DOI] [PubMed] [Google Scholar]
- 7.Korja M, Kivisaari R, Jahromi BR, Lehto H. Size and location of ruptured intracranial aneurysms: consecutive series of 1993 hospital-admitted patients. J Neurosurg. 2017;127(4):748-753. doi: 10.3171/2016.9.JNS161085 [DOI] [PubMed] [Google Scholar]
- 8.Tolonen H, Salomaa V, Torppa J, Sivenius J, Immonen-Räihä P, Lehtonen A. The validation of the Finnish Hospital Discharge Register and Causes of Death Register data on stroke diagnoses. Eur J Prev Cardiol. 2007;14(3):380-385. doi: 10.1097/01.hjr.0000239466.26132.f2 [DOI] [PubMed] [Google Scholar]
- 9.Pakarinen S. Incidence, aetiology, and prognosis of primary subarachnoid haemorrhage. A study based on 589 cases diagnosed in a defined urban population during a defined period. Acta Neurol Scand. 1967;43(suppl 29):1-28. [PubMed] [Google Scholar]
- 10.Tilvis R, Autio L, Mähönen Y, Mäntylä J, Heinonen M, Brommels M. The incidence and prognosis of cerebrovascular disease in hospital patients in Helsinki, Finland, in the decade 1970-1980. Acta Med Scand. 1987;221(3):267-273. doi: 10.1111/j.0954-6820.1987.tb00893.x [DOI] [PubMed] [Google Scholar]
- 11.Huang H, Lai LT. Incidence and case-fatality of aneurysmal subarachnoid hemorrhage in Australia, 2008-2018. World Neurosurg. 2020;144:e438-e446. doi: 10.1016/j.wneu.2020.08.186 [DOI] [PubMed] [Google Scholar]
- 12.Bryndziar T, Sedova P, Brown RD Jr, et al. Trends in one month and one year hemorrhagic stroke case fatality rates in the Czech Republic between 1998 and 2015. J Stroke Cerebrovasc Dis. 2020;29(6):104762. doi: 10.1016/j.jstrokecerebrovasdis.2020.104762 [DOI] [PubMed] [Google Scholar]
- 13.Gabet A, Grimaud O, de Peretti C, Béjot Y, Olié V. Determinants of case fatality after hospitalization for stroke in France 2010 to 2015. Stroke. 2019;50(2):305-312. doi: 10.1161/strokeaha.118.023495 [DOI] [PubMed] [Google Scholar]
- 14.González-Pérez A, Gaist D, Wallander MA, McFeat G, García-Rodríguez LA. Mortality after hemorrhagic stroke: data from general practice (The Health Improvement Network). Neurology. 2013;81(6):559-565. doi: 10.1212/WNL.0b013e31829e6eff [DOI] [PubMed] [Google Scholar]
- 15.Shah VA, Kazmi SO, Damani R, et al. Regional variability in the care and outcomes of subarachnoid hemorrhage patients in the United States. Front Neurol. 2022;13:908609. doi: 10.3389/fneur.2022.908609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.StatFin: Statistics Finland's free-of-charge statistical databases. Accessed February 28, 2023. pxdata.stat.fi/PxWeb/pxweb/en/StatFin/.
- 17.Rosengart AJ, Schultheiss KE, Tolentino J, Macdonald RL. Prognostic factors for outcome in patients with aneurysmal subarachnoid hemorrhage. Stroke. 2007;38(8):2315-2321. doi: 10.1161/STROKEAHA.107.484360 [DOI] [PubMed] [Google Scholar]
- 18.Lindbohm JV, Kaprio J, Jousilahti P, Salomaa V, Korja M. Risk factors of sudden death from subarachnoid hemorrhage. Stroke. 2017;48(9):2399-2404. doi: 10.1161/STROKEAHA.117.018118 [DOI] [PubMed] [Google Scholar]
- 19.Lindgren A, Burt S, Bragan Turner E, et al. Hospital case-volume is associated with case-fatality after aneurysmal subarachnoid hemorrhage. Int J Stroke. 2019;14(3):282-289. doi: 10.1177/1747493018790073 [DOI] [PubMed] [Google Scholar]
- 20.McNeill L, English SW, Borg N, Matta BF, Menon DK. Effects of institutional caseload of subarachnoid hemorrhage on mortality: a Secondary analysis of administrative data. Stroke. 2013;44(3):647-652. doi: 10.1161/STROKEAHA.112.681254 [DOI] [PubMed] [Google Scholar]
- 21.Aromaa A. Health and functional capacity in Finland: basic results of the Health 2000 survey (in Finnish). 2002. Accessed February 28, 2023. urn.fi/URN:ISBN:951-740-262-7.
- 22.Koponen P, Borodulin K, Lundqvist A, Sääksjärvi K, Koskinen S. Health, functional capacity and well-being in Finland: FinHealth 2017 study (In Finnish). 2018. Accessed February 28, 2023. urn.fi/URN:ISBN:978-952-343-105-8.
- 23.Sotkanet: statistical information on welfare and health in Finland. Accessed February 28, 2023. sotkanet.fi/sotkanet/en/index?.
- 24.Maher M, Schweizer TA, Macdonald RL. Treatment of spontaneous subarachnoid hemorrhage: guidelines and gaps. Stroke. 2020;51(4):1326-1332. doi: 10.1161/strokeaha.119.025997 [DOI] [PubMed] [Google Scholar]
- 25.Fogelholm R, Hernesniemi J, Vapalahti M. Impact of early surgery on outcome after aneurysmal subarachnoid hemorrhage: a population-based study. Stroke. 1993;24(11):1649-1654. doi: 10.1161/01.STR.24.11.1649 [DOI] [PubMed] [Google Scholar]
- 26.Kotila M. Declining incidence and mortality of stroke? Stroke. 1984;15(2):255-259. doi: 10.1161/01.STR.15.2.255 [DOI] [PubMed] [Google Scholar]
- 27.Sarti C, Tuomilehto J, Sivenius J, et al. Stroke mortality and case-fatality rates in three geographic areas of Finland from 1983 to 1986. Stroke. 1993;24(8):1140-1147. doi: 10.1161/01.STR.24.8.1140 [DOI] [PubMed] [Google Scholar]
- 28.Stegmayr B, Eriksson M, Asplund K. Declining mortality from subarachnoid hemorrhage: changes in incidence and case fatality from 1985 through 2000. Stroke. 2004;35(9):2059-2063. doi: 10.1161/01.STR.0000138451.07853.b6 [DOI] [PubMed] [Google Scholar]
- 29.Appelros P. Secular trends of stroke epidemiology in Örebro, Sweden, 2017 compared to the trends in 1999: a population-based study. Cerebrovasc Dis. 2020;48(3-6):149-156. doi: 10.1159/000504082 [DOI] [PubMed] [Google Scholar]
- 30.Khan FA, Engstrom G, Jerntorp I, Pessah-Rasmussen H, Janzon L. Seasonal patterns of incidence and case fatality of stroke in Malmö, Sweden: the STROMA study. Neuroepidemiology. 2005;24(1-2):26-31. doi: 10.1159/000081046 [DOI] [PubMed] [Google Scholar]
- 31.Ellekjær H, Holmen J, Indredavik B, Terent A. Epidemiology of stroke in innherred, Norway, 1994 to 1996: incidence and 30-day case-fatality rate. Stroke. 1997;28(11):2180-2184. doi: 10.1161/01.str.28.11.2180 [DOI] [PubMed] [Google Scholar]
- 32.Sandvei MS, Mathiesen EB, Vatten LJ, et al. Incidence and mortality of aneurysmal subarachnoid hemorrhage in two Norwegian cohorts, 1984-2007. Neurology. 2011;77(20):1833-1839. doi: 10.1212/WNL.0b013e3182377de3 [DOI] [PubMed] [Google Scholar]
- 33.Lovelock CE, Rinkel GJE, Rothwell PM. Time trends in outcome of subarachnoid hemorrhage: population-based study and systematic review. Neurology. 2010;74(19):1494-1501. doi: 10.1212/WNL.0b013e3181dd42b3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smeeton NC, Heuschmann PU, Rudd AG, et al. Incidence of hemorrhagic stroke in black Caribbean, black African, and white populations: the South London Stroke Register, 1995-2004. Stroke. 2007;38(12):3133-3138. doi: 10.1161/STROKEAHA.107.487082 [DOI] [PubMed] [Google Scholar]
- 35.Macpherson KJ, Lewsey JD, Jhund PS, et al. Trends in incidence and in short term survival following a subarachnoid haemorrhage in Scotland, 1986-2005: a retrospective cohort study. BMC Neurol. 2011;11:38. doi: 10.1186/1471-2377-11-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Flynn RW, MacDonald TM, Murray GD, Ferguson C, Shah K, Doney AS. The Tayside Stroke Cohort: exploiting advanced regional medical informatics to create a region-wide database for studying the pharmacoepidemiology of stroke. Pharmacoepidemiol Drug Saf. 2010;19(7):737-744. doi: 10.1002/pds.1958 [DOI] [PubMed] [Google Scholar]
- 37.Mackey J, Khoury JC, Alwell K, et al. Stable incidence but declining case-fatality rates of subarachnoid hemorrhage in a population. Neurology. 2016;87(21):2192-2197. doi: 10.1212/WNL.0000000000003353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Giordan E, Graffeo CS, Rabinstein AA, et al. Aneurysmal subarachnoid hemorrhage: long-term trends in incidence and survival in Olmsted County, Minnesota. J Neurosurg. 2021;134(3):878-883. doi: 10.3171/2019.12.JNS192468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Labovitz DL, Halim AX, Brent B, Boden-Albala B, Hauser WA, Sacco RL. Subarachnoid hemorrhage incidence among whites, blacks and caribbean hispanics: the Northern Manhattan Study. Neuroepidemiology. 2006;26(3):147-150. doi: 10.1159/000091655 [DOI] [PubMed] [Google Scholar]
- 40.Longstreth WT Jr, Nelson LM, Koepsell TD, van Belle G. Clinical course of spontaneous subarachnoid hemorrhage: a population-based study in King County, Washington. Neurology. 1993;43(4):712-718. doi: 10.1212/wnl.43.4.712 [DOI] [PubMed] [Google Scholar]
- 41.Thrift AG, Dewey HM, Sturm JW, et al. Incidence of stroke subtypes in the North East Melbourne Stroke Incidence Study (NEMESIS): differences between men and women. Neuroepidemiology. 2008;32(1):11-18. doi: 10.1159/000170086 [DOI] [PubMed] [Google Scholar]
- 42.Epidemiology of aneurysmal subarachnoid hemorrhage in Australia and New Zealand. Stroke. 2000;31(8):1843-1850. doi: 10.1161/01.str.31.8.1843 [DOI] [PubMed] [Google Scholar]
- 43.D'Alessandro G, Bottacchi E, Di Giovanni M, et al. Temporal trends of stroke in valle d'Aosta, Italy. Incidence and 30-day fatality rates. Neurol Sci. 2000;21(1):13-18. doi: 10.1007/s100720070113 [DOI] [PubMed] [Google Scholar]
- 44.Corso G, Bottacchi E, Giardini G, et al. Epidemiology of stroke in Northern Italy: the Cerebrovascular Aosta Registry, 2004-2008. Neurol Sci. 2013;34(7):1071-1081. doi: 10.1007/s10072-012-1185-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lauria G, Gentile M, Fassetta G, et al. Incidence and prognosis of stroke in the Belluno province, Italy. First-year results of a community-based study. Stroke. 1995;26(10):1787-1793. doi: 10.1161/01.str.26.10.1787 [DOI] [PubMed] [Google Scholar]
- 46.Sacco S, Totaro R, Toni D, Marini C, Cerone D, Carolei A. Incidence, case-fatalities and 10-year survival of subarachnoid hemorrhage in a population-based registry. Eur Neurol. 2009;62(3):155-160. doi: 10.1159/000226617 [DOI] [PubMed] [Google Scholar]
- 47.Di Carlo A, Inzitari D, Galati F, et al. A prospective community-based study of stroke in Southern Italy: the Vibo Valentia incidence of stroke study (VISS). Methodology, incidence and case fatality at 28 days, 3 and 12 months. Cerebrovasc Dis. 2003;16(4):410-417. doi: 10.1159/000072565 [DOI] [PubMed] [Google Scholar]
- 48.Dijkland SA, Jaja BNR, van der Jagt M, et al. Between-center and between-country differences in outcome after aneurysmal subarachnoid hemorrhage in the Subarachnoid Hemorrhage International Trialists (SAHIT) repository. J Neurosurg. 2019:1-9. doi: 10.3171/2019.5.Jns19483 [DOI] [PubMed] [Google Scholar]
- 49.Kjærulff TM, Bihrmann K, Zhao J, et al. Acute myocardial infarction: does survival depend on geographical location and social background? Eur J Prev Cardiol. 2019;26(17):1828-1839. doi: 10.1177/2047487319852680 [DOI] [PubMed] [Google Scholar]
- 50.Sacco S, Stracci F, Cerone D, Ricci S, Carolei A. Epidemiology of stroke in Italy. Int J Stroke. 2011;6(3):219-227. doi: 10.1111/j.1747-4949.2011.00594.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to legislative data transfer restrictions imposed by the European Union, the used dataset is not available for public use. However, qualified investigators can request access to the data from the Finnish Health and Social Data Permit Authority (findata.fi/en/).