Figure 7. Treatment with PAR1 antagonist reduces itch and skin damage during S. aureus exposure.
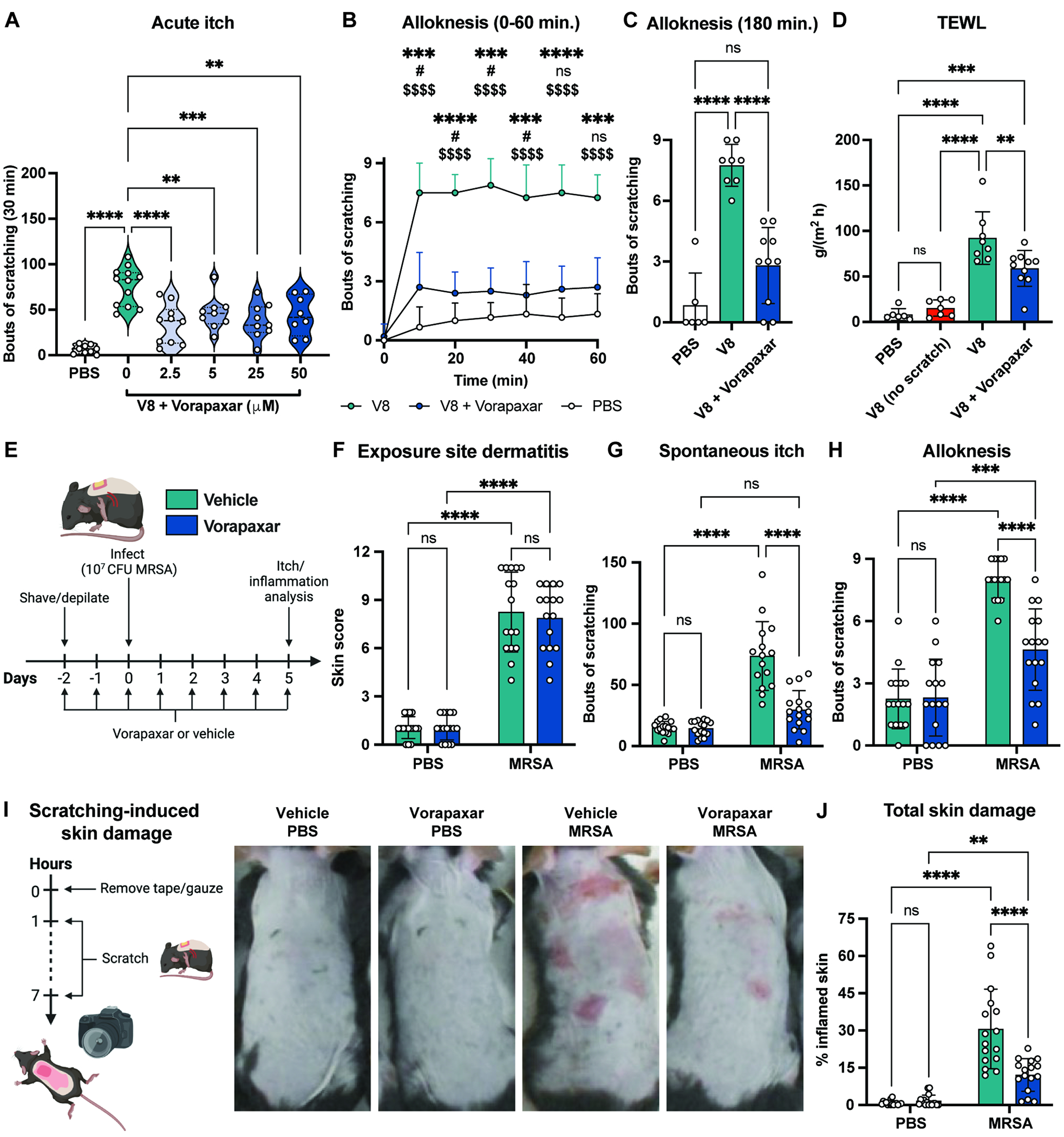
(A) Bouts of scratching following cheek injection with PBS or V8 with increasing doses of Vorapaxar (n=4-6 males, 4-6 females per group).
(B-C) Alloknesis measured every 10 min. for 1hr (B) and 3 hrs (C) after cheek injection with PBS, V8, or V8+Vorapaxar (n=3-5 males, 3-5 females per group).
(D) Mice injected with PBS, V8, or V8+Vorapaxar were allowed to scratch; TEWL measured 3 hrs post-injection. One group of V8-injected mice were wrapped in bandages to prevent scratching.
(E-J) Mice gavaged daily with vehicle or Vorapaxar from 2-days before exposure to PBS or MRSA. Dermatitis scores (F), spontaneous itch (G), alloknesis (H), scratch-induced skin damage (I-J) measured for control and MRSA-exposed mice treated with vehicle or Vorapaxar (n=7-8 males, 8 females per group)
For each panel, data combined from 2 independent experiments are shown. Data are represented as mean±SD.
Statistical analysis: (A, C, D) Mann-Whitney test (B) Two-way ANOVA with Tukey’s multiple comparisons: *V8 vs. V8+Vorapaxar; #V8+Vorapaxar vs. PBS; $V8 vs. PBS (F-H, J) Two-way ANOVA with Sidak’s multiple comparisons. *P<0.05; **P<0.01; ***P<0.001; ****P<0.0001; ns, not significant. See also Figure S9.
