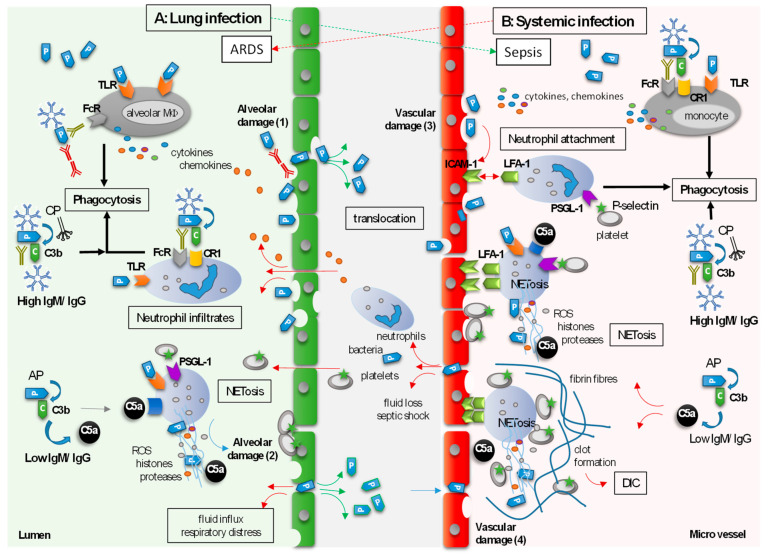
Figure 2.
Neutrophil and Ig actions at the epithelial/endothelial barrier of alveoli leading from lung infection to sepsis or from systemic infection to ARDS. (A) In the case of lung infection, bacteria (P) enter the lung alveoli (green area), where they are phagocytosed by alveolar macrophages. Due to infection-related damage of alveolar epithelium (1, green lining) and activation of macrophages, cytokines and chemokines (colored circles) are secreted. Neutrophils and platelets translocate from the vasculature (red lining) through the interstitium (gray area) into the alveoli. Neutrophils support phagocytosis, which is enhanced in the presence of polyvalent Igs (high IgM/IgG) and when bacteria are complement-opsonized (via CP). In the absence of Igs, particularly IgM (low IgM/IgG), complement is activated by the AP causing release of C5a (anaphylatoxin). Overactivation of neutrophils by bacteria (TLR stimulation), platelets, and C5a, leads to NETosis, which further damages the alveoli (2, green lining). Tissue damage facilitates translocation of bacteria into the blood stream (green arrows) causing sepsis. (B) When bacteria disseminate into the vasculature, they are phagocytosed by monocytes. Phagocytosis is enhanced in the presence of IgG, IgA, and IgM, and after additional complement deposition. If, however, bacterial load is too high, they cannot be sufficiently cleared and may damage endothelial cells (3, red lining). Platelets are activated and plug the damaged vessel wall. In addition, activated endothelial cells express adhesion molecules such as ICAM-1. Secretion of cytokines and chemokines attract and activate neutrophils that attach to the endothelium, e.g., via integrin LFA-1 to ligand ICAM-1. Activated platelets express P-selectin and engage with the P-selectin receptor (via the ligand PSGL-1) on neutrophils. In the absence of sufficient Ig levels (low IgM/IgG), neutrophils are overactivated by binding of PSGL-1 and C5a to their respective receptors and via TLR stimulation inducing NETosis of the attached neutrophils. C5a is generated via the AP and can induce NETs. This leads to activation of coagulation processes and ultimately to immunothrombosis, DIC, and to further vascular damage (4), thus facilitating translocation of bacteria into the interstitium and lung alveoli, causing ARDS (red arrows at the red and green lining). AP: alternative pathway; ARDS: acute respiratory distress syndrome; C: complement; C3b: complement factor C3b (anaphylatoxin); C5a: complement factor C5a (anaphylatoxin); CP: classical pathway; CR1: complement receptor 1; DIC: disseminated intravascular coagulation; FcR: Fc receptor; ICAM-1: intercellular adhesion molecule 1; Ig: immunoglobulin; LFA-1: lymphocyte function-associated antigen 1; MΦ: macrophage; NET: neutrophil extracellular trap; P: bacteria; PSGL-1: P-selectin glycoprotein ligand 1; ROS: reactive oxygen species; TLR: Toll-like receptor.