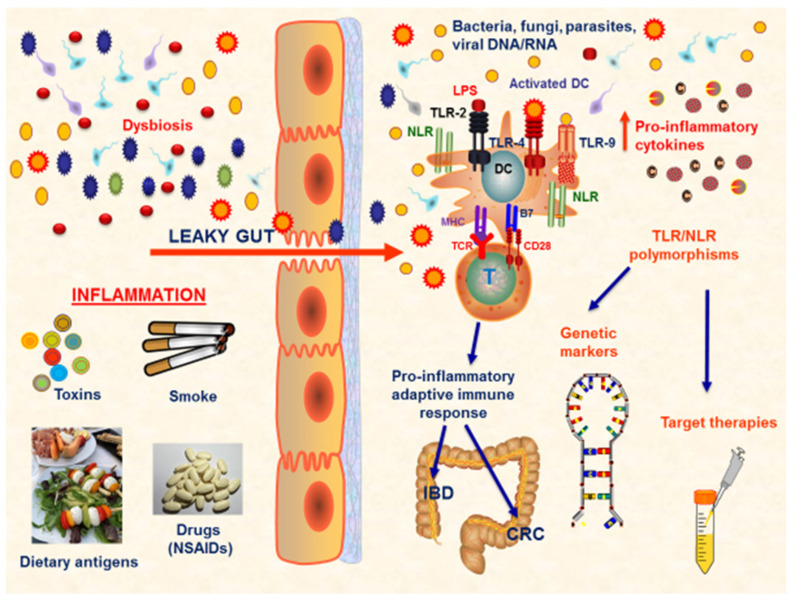
Figure 1.
TLR response at gut mucosa in IBD and CRC. IBD and CRC are both characterized by the presence of a persistent chronic inflammatory status that heavily affects the gut mucosa homeostasis. Several conditions are implicated in the development of mucosal damage, such as dysbiosis, smoke, toxins, dietary antigens, and drugs. The most important factor is represented by the alteration in the gut permeability. In the condition of ‘leaky gut’, a disequilibrium between the immune system and microbiota exists and several inflammatory pathways are activated, leading to the proliferation of pro-inflammatory cells, such as Th1, Th2, and Th17 cells, with a corresponding downregulation of the anti-inflammatory Tregs, and the production of pro-inflammatory mediators. In this scenario of impaired gut mucosa homeostasis, the gut microbiota composition is altered, and pro-inflammatory bacteria, known as ‘pathobionts’, proliferate and further enhance the immune response. This complex pathological mechanism is driven by the presence of specific receptors on immune cells, able to be activated by microbial components, such as TLRs and NLRs. Several TLR/NLR polymorphisms have been evaluated to be linked to specific pathological patterns, both in IBD and CRC. Thus, these polymorphisms may be considered as disease-related genetic markers and may guide the development of personalized target therapies. Abbreviations: NSAIDs (non-steroidal anti-inflammatory drugs); TLR (Toll-like receptors); NLR (NOD-like receptors); DC (dendritic cell); IBD (inflammatory bowel disease); CRC (colorectal cancer); LPS (lipopolysaccharide).