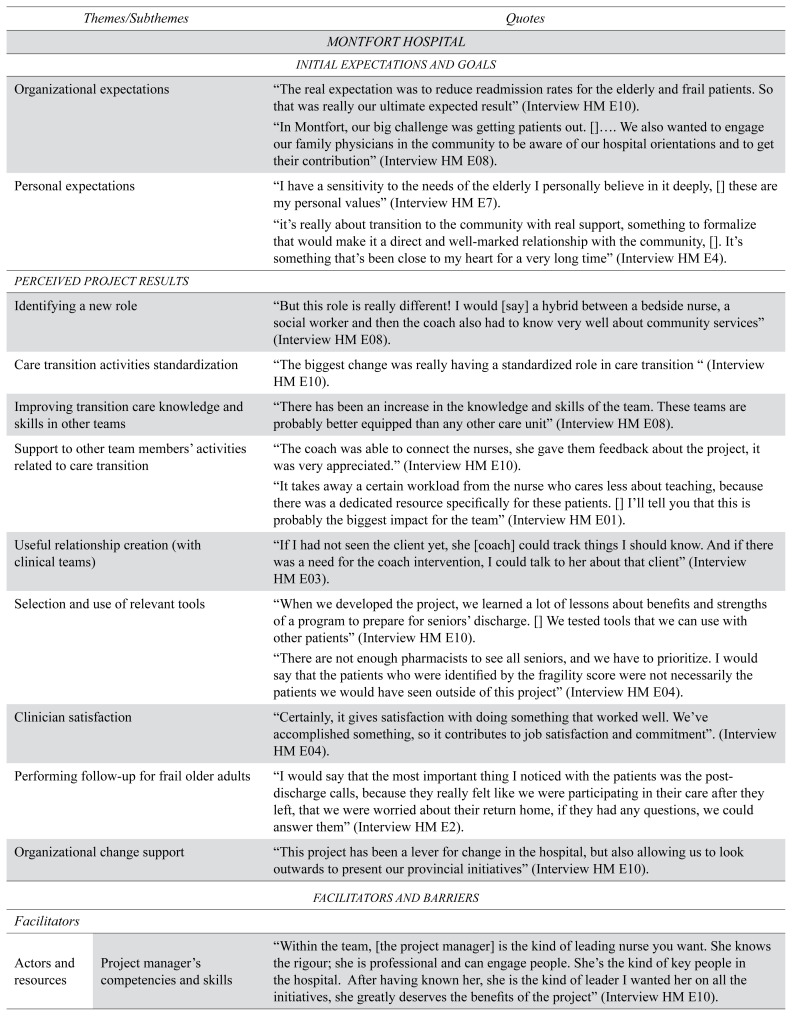
| Themes/Subthemes | Quotes | |
|---|---|---|
| MONTFORT HOSPITAL | ||
|
| ||
| INITIAL EXPECTATIONS AND GOALS | ||
|
| ||
| Organizational expectations | “The real expectation was to reduce readmission rates for the elderly and frail patients. So that was really our ultimate expected result” (Interview HM E10). | |
|
| ||
| “In Montfort, our big challenge was getting patients out. []…. We also wanted to engage our family physicians in the community to be aware of our hospital orientations and to get their contribution” (Interview HM E08). | ||
|
| ||
| Personal expectations | “I have a sensitivity to the needs of the elderly I personally believe in it deeply, [] these are my personal values” (Interview HM E7). | |
| “it’s really about transition to the community with real support, something to formalize that would make it a direct and well-marked relationship with the community, []. It’s something that’s been close to my heart for a very long time” (Interview HM E4). | ||
|
| ||
| PERCEIVED PROJECT RESULTS | ||
|
| ||
| Identifying a new role | “But this role is really different! I would [say] a hybrid between a bedside nurse, a social worker and then the coach also had to know very well about community services” (Interview HM E08). | |
|
| ||
| Care transition activities standardization | “The biggest change was really having a standardized role in care transition “ (Interview HM E10). | |
|
| ||
| Improving transition care knowledge and skills in other teams | “There has been an increase in the knowledge and skills of the team. These teams are probably better equipped than any other care unit” (Interview HM E08). | |
|
| ||
| Support to other team members’ activities related to care transition | “The coach was able to connect the nurses, she gave them feedback about the project, it was very appreciated.” (Interview HM E10). | |
| “It takes away a certain workload from the nurse who cares less about teaching, because there was a dedicated resource specifically for these patients. [] I’ll tell you that this is probably the biggest impact for the team” (Interview HM E01). | ||
|
| ||
| Useful relationship creation (with clinical teams) | “If I had not seen the client yet, she [coach] could track things I should know. And if there was a need for the coach intervention, I could talk to her about that client” (Interview HM E03). | |
|
| ||
| Selection and use of relevant tools | “When we developed the project, we learned a lot of lessons about benefits and strengths of a program to prepare for seniors’ discharge. [] We tested tools that we can use with other patients” (Interview HM E10). | |
| “There are not enough pharmacists to see all seniors, and we have to prioritize. I would say that the patients who were identified by the fragility score were not necessarily the patients we would have seen outside of this project” (Interview HM E04). | ||
|
| ||
| Clinician satisfaction | “Certainly, it gives satisfaction with doing something that worked well. We’ve accomplished something, so it contributes to job satisfaction and commitment”. (Interview HM E04). | |
|
| ||
| Performing follow-up for frail older adults | “I would say that the most important thing I noticed with the patients was the post-discharge calls, because they really felt like we were participating in their care after they left, that we were worried about their return home, if they had any questions, we could answer them” (Interview HM E2). | |
|
| ||
| Organizational change support | “This project has been a lever for change in the hospital, but also allowing us to look outwards to present our provincial initiatives” (Interview HM E10). | |
|
| ||
| FACILITATORS AND BARRIERS | ||
|
| ||
| Facilitators | ||
|
| ||
| Actors and resources | Project manager’s competencies and skills | “Within the team, [the project manager] is the kind of leading nurse you want. She knows the rigour; she is professional and can engage people. She’s the kind of key people in the hospital. After having known her, she is the kind of leader I wanted her on all the initiatives, she greatly deserves the benefits of the project” (Interview HM E10). |
|
| ||
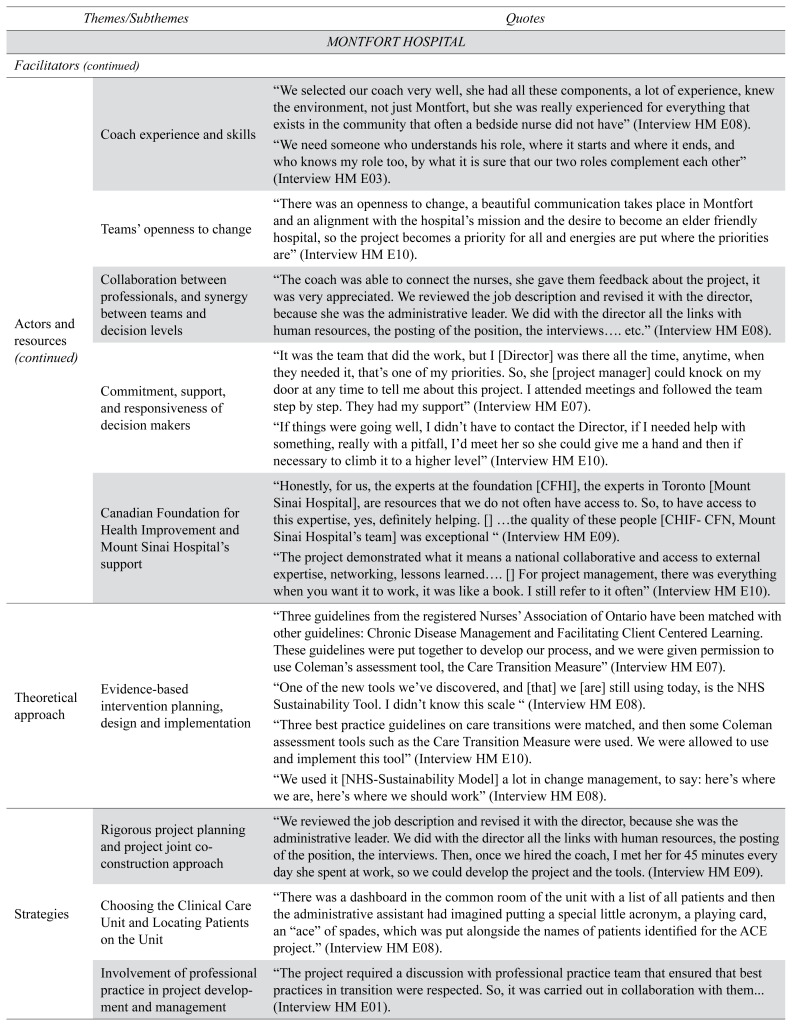
| Coach experience and skills | “We selected our coach very well, she had all these components, a lot of experience, knew the environment, not just Montfort, but she was really experienced for everything that exists in the community that often a bedside nurse did not have” (Interview HM E08). | |
| “We need someone who understands his role, where it starts and where it ends, and who knows my role too, by what it is sure that our two roles complement each other” (Interview HM E03). | ||
|
| ||
| Teams’ openness to change | “There was an openness to change, a beautiful communication takes place in Montfort and an alignment with the hospital’s mission and the desire to become an elder friendly hospital, so the project becomes a priority for all and energies are put where the priorities are” (Interview HM E10). | |
|
| ||
| Collaboration between professionals, and synergy between teams and decision levels | “The coach was able to connect the nurses, she gave them feedback about the project, it was very appreciated. We reviewed the job description and revised it with the director, because she was the administrative leader. We did with the director all the links with human resources, the posting of the position, the interviews…. etc.” (Interview HM E08). | |
|
| ||
| Commitment, support, and responsiveness of decision makers | “It was the team that did the work, but I [Director] was there all the time, anytime, when they needed it, that’s one of my priorities. So, she [project manager] could knock on my door at any time to tell me about this project. I attended meetings and followed the team step by step. They had my support” (Interview HM E07). | |
| “If things were going well, I didn’t have to contact the Director, if I needed help with something, really with a pitfall, I’d meet her so she could give me a hand and then if necessary to climb it to a higher level” (Interview HM E10). | ||
|
| ||
| Canadian Foundation for Health Improvement and Mount Sinai Hospital’s support | “Honestly, for us, the experts at the foundation [CFHI], the experts in Toronto [Mount Sinai Hospital], are resources that we do not often have access to. So, to have access to this expertise, yes, definitely helping. [] …the quality of these people [CHIF-CFN, Mount Sinai Hospital’s team] was exceptional “ (Interview HM E09). | |
| “The project demonstrated what it means a national collaborative and access to external expertise, networking, lessons learned…. [] For project management, there was everything when you want it to work, it was like a book. I still refer to it often” (Interview HM E10). | ||
|
| ||
| Theoretical approach | Evidence-based intervention planning, design and implementation | “Three guidelines from the registered Nurses’ Association of Ontario have been matched with other guidelines: Chronic Disease Management and Facilitating Client Centered Learning. These guidelines were put together to develop our process, and we were given permission to use Coleman’s assessment tool, the Care Transition Measure” (Interview HM E07). |
| “One of the new tools we’ve discovered, and [that] we [are] still using today, is the NHS Sustainability Tool. I didn’t know this scale “ (Interview HM E08). | ||
| “Three best practice guidelines on care transitions were matched, and then some Coleman assessment tools such as the Care Transition Measure were used. We were allowed to use and implement this tool” (Interview HM E10). | ||
| “We used it [NHS-Sustainability Model] a lot in change management, to say: here’s where we are, here’s where we should work” (Interview HM E08). | ||
|
| ||
| Strategies | Rigorous project planning and project joint co-construction approach | “We reviewed the job description and revised it with the director, because she was the administrative leader. We did with the director all the links with human resources, the posting of the position, the interviews. Then, once we hired the coach, I met her for 45 minutes every day she spent at work, so we could develop the project and the tools. (Interview HM E09). |
|
| ||
| Choosing the Clinical Care Unit and Locating Patients on the Unit | “There was a dashboard in the common room of the unit with a list of all patients and then the administrative assistant had imagined putting a special little acronym, a playing card, an “ace” of spades, which was put alongside the names of patients identified for the ACE project.” (Interview HM E08). | |
|
| ||
| Involvement of professional practice in project development and management | “The project required a discussion with professional practice team that ensured that best practices in transition were respected. So, it was carried out in collaboration with them... (Interview HM E01). | |
|
| ||
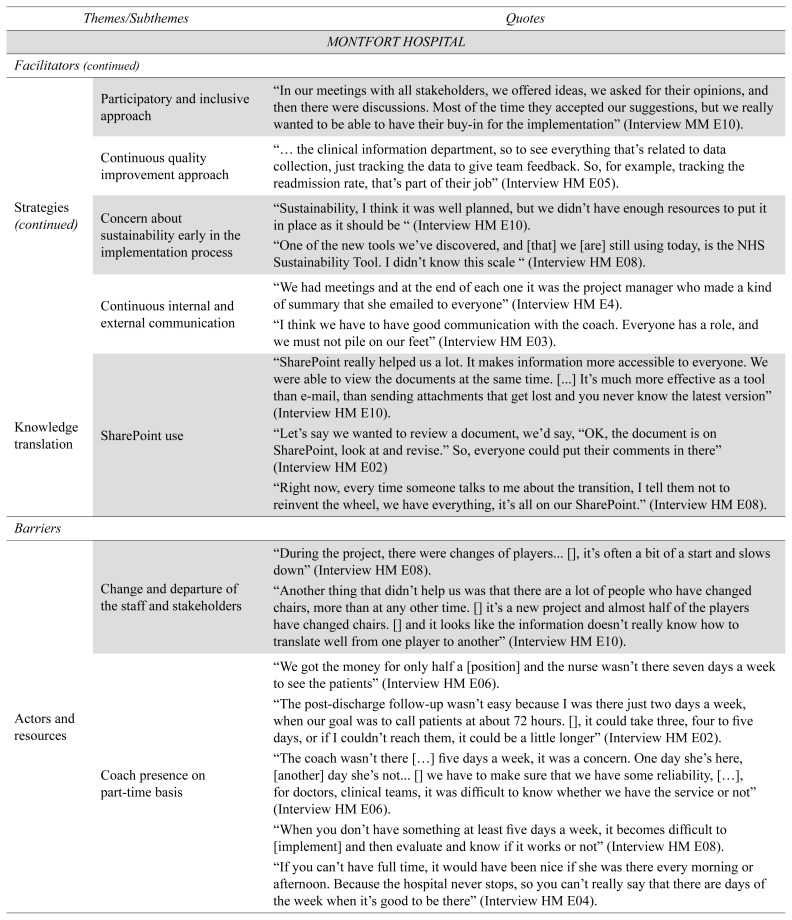
| Participatory and inclusive approach | “In our meetings with all stakeholders, we offered ideas, we asked for their opinions, and then there were discussions. Most of the time they accepted our suggestions, but we really wanted to be able to have their buy-in for the implementation” (Interview MM E10). | |
|
| ||
| Continuous quality improvement approach | “… the clinical information department, so to see everything that’s related to data collection, just tracking the data to give team feedback. So, for example, tracking the readmission rate, that’s part of their job” (Interview HM E05). | |
|
| ||
| Concern about sustainability early in the implementation process | “Sustainability, I think it was well planned, but we didn’t have enough resources to put it in place as it should be “ (Interview HM E10). | |
| “One of the new tools we’ve discovered, and [that] we [are] still using today, is the NHS Sustainability Tool. I didn’t know this scale “ (Interview HM E08). | ||
|
| ||
| Continuous internal and external communication | “We had meetings and at the end of each one it was the project manager who made a kind of summary that she emailed to everyone” (Interview HM E4). | |
| “I think we have to have good communication with the coach. Everyone has a role, and we must not pile on our feet” (Interview HM E03). | ||
|
| ||
| Knowledge translation | SharePoint use | “SharePoint really helped us a lot. It makes information more accessible to everyone. We were able to view the documents at the same time. [...] It’s much more effective as a tool than e-mail, than sending attachments that get lost and you never know the latest version” (Interview HM E10). |
| “Let’s say we wanted to review a document, we’d say, “OK, the document is on SharePoint, look at and revise.” So, everyone could put their comments in there” (Interview HM E02) | ||
| “Right now, every time someone talks to me about the transition, I tell them not to reinvent the wheel, we have everything, it’s all on our SharePoint.” (Interview HM E08). | ||
|
| ||
| Barriers | ||
|
| ||
| Actors and resources | Change and departure of the staff and stakeholders | “During the project, there were changes of players... [], it’s often a bit of a start and slows down” (Interview HM E08). |
| “Another thing that didn’t help us was that there are a lot of people who have changed chairs, more than at any other time. [] it’s a new project and almost half of the players have changed chairs. [] and it looks like the information doesn’t really know how to translate well from one player to another” (Interview HM E10). | ||
|
| ||
| Coach presence on part-time basis | “We got the money for only half a [position] and the nurse wasn’t there seven days a week to see the patients” (Interview HM E06). | |
| “The post-discharge follow-up wasn’t easy because I was there just two days a week, when our goal was to call patients at about 72 hours. [], it could take three, four to five days, or if I couldn’t reach them, it could be a little longer” (Interview HM E02). | ||
| “The coach wasn’t there […] five days a week, it was a concern. One day she’s here, [another] day she’s not... [] we have to make sure that we have some reliability, […], for doctors, clinical teams, it was difficult to know whether we have the service or not” (Interview HM E06). | ||
| “When you don’t have something at least five days a week, it becomes difficult to [implement] and then evaluate and know if it works or not” (Interview HM E08). | ||
| “If you can’t have full time, it would have been nice if she was there every morning or afternoon. Because the hospital never stops, so you can’t really say that there are days of the week when it’s good to be there” (Interview HM E04). | ||
|
| ||
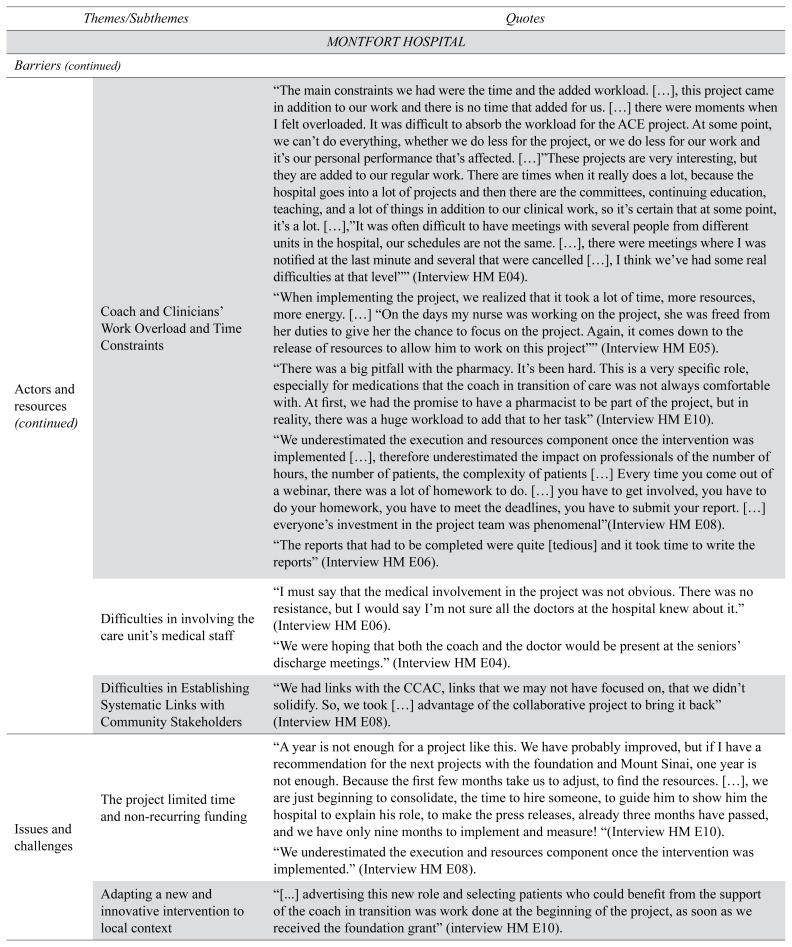
| Coach and Clinicians’ Work Overload and Time Constraints | “The main constraints we had were the time and the added workload. […], this project came in addition to our work and there is no time that added for us. […] there were moments when I felt overloaded. It was difficult to absorb the workload for the ACE project. At some point, we can’t do everything, whether we do less for the project, or we do less for our work and it’s our personal performance that’s affected. […]”These projects are very interesting, but they are added to our regular work. There are times when it really does a lot, because the hospital goes into a lot of projects and then there are the committees, continuing education, teaching, and a lot of things in addition to our clinical work, so it’s certain that at some point, it’s a lot. […],”It was often difficult to have meetings with several people from different units in the hospital, our schedules are not the same. […], there were meetings where I was notified at the last minute and several that were cancelled […], I think we’ve had some real difficulties at that level”“ (Interview HM E04). | |
| “When implementing the project, we realized that it took a lot of time, more resources, more energy. […] “On the days my nurse was working on the project, she was freed from her duties to give her the chance to focus on the project. Again, it comes down to the release of resources to allow him to work on this project”“ (Interview HM E05). | ||
| “There was a big pitfall with the pharmacy. It’s been hard. This is a very specific role, especially for medications that the coach in transition of care was not always comfortable with. At first, we had the promise to have a pharmacist to be part of the project, but in reality, there was a huge workload to add that to her task” (Interview HM E10). | ||
| “We underestimated the execution and resources component once the intervention was implemented […], therefore underestimated the impact on professionals of the number of hours, the number of patients, the complexity of patients […] Every time you come out of a webinar, there was a lot of homework to do. […] you have to get involved, you have to do your homework, you have to meet the deadlines, you have to submit your report. […] everyone’s investment in the project team was phenomenal”(Interview HM E08). | ||
| “The reports that had to be completed were quite [tedious] and it took time to write the reports” (Interview HM E06). | ||
|
| ||
| Difficulties in involving the care unit’s medical staff | “I must say that the medical involvement in the project was not obvious. There was no resistance, but I would say I’m not sure all the doctors at the hospital knew about it.” (Interview HM E06). | |
| “We were hoping that both the coach and the doctor would be present at the seniors’ discharge meetings.” (Interview HM E04). | ||
|
| ||
| Difficulties in Establishing Systematic Links with Community Stakeholders | “We had links with the CCAC, links that we may not have focused on, that we didn’t solidify. So, we took […] advantage of the collaborative project to bring it back” (Interview HM E08). | |
|
| ||
| Issues and challenges | The project limited time and non-recurring funding | “A year is not enough for a project like this. We have probably improved, but if I have a recommendation for the next projects with the foundation and Mount Sinai, one year is not enough. Because the first few months take us to adjust, to find the resources. […], we are just beginning to consolidate, the time to hire someone, to guide him to show him the hospital to explain his role, to make the press releases, already three months have passed, and we have only nine months to implement and measure! “(Interview HM E10). |
| “We underestimated the execution and resources component once the intervention was implemented.” (Interview HM E08). | ||
|
| ||
| Adapting a new and innovative intervention to local context | “[...] advertising this new role and selecting patients who could benefit from the support of the coach in transition was work done at the beginning of the project, as soon as we received the foundation grant” (interview HM E10). | |
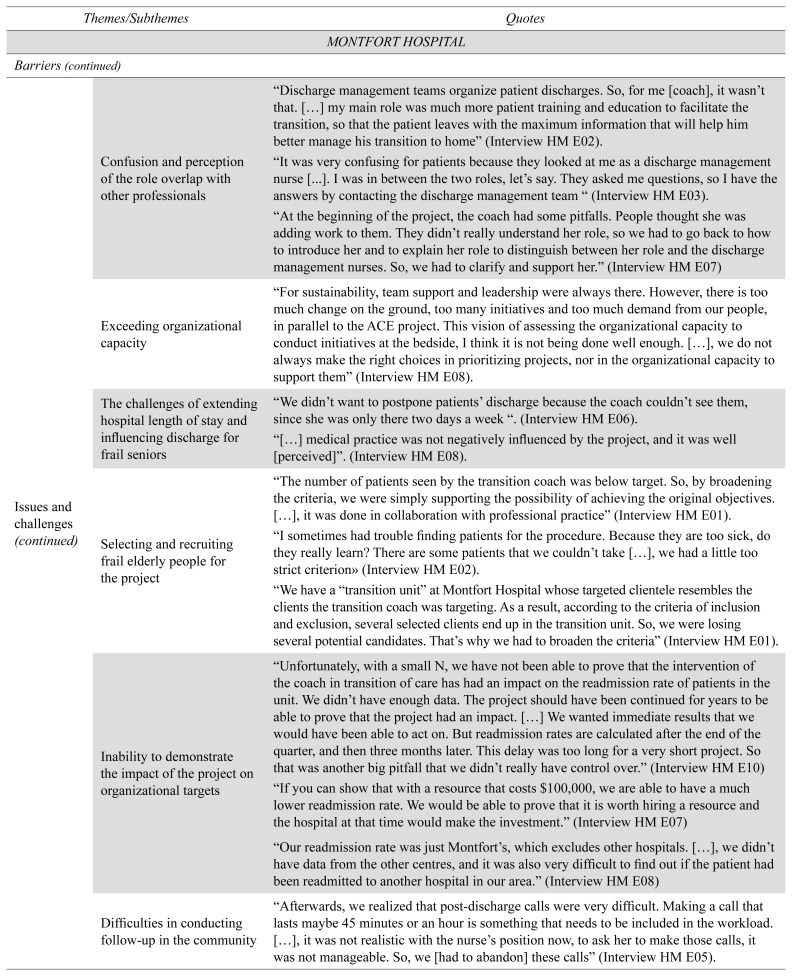
| Confusion and perception of the role overlap with other professionals | “Discharge management teams organize patient discharges. So, for me [coach], it wasn’t that. […] my main role was much more patient training and education to facilitate the transition, so that the patient leaves with the maximum information that will help him better manage his transition to home” (Interview HM E02). | |
| “It was very confusing for patients because they looked at me as a discharge management nurse [...]. I was in between the two roles, let’s say. They asked me questions, so I have the answers by contacting the discharge management team “ (Interview HM E03). | ||
| “At the beginning of the project, the coach had some pitfalls. People thought she was adding work to them. They didn’t really understand her role, so we had to go back to how to introduce her and to explain her role to distinguish between her role and the discharge management nurses. So, we had to clarify and support her.” (Interview HM E07) | ||
|
| ||
| Exceeding organizational capacity | “For sustainability, team support and leadership were always there. However, there is too much change on the ground, too many initiatives and too much demand from our people, in parallel to the ACE project. This vision of assessing the organizational capacity to conduct initiatives at the bedside, I think it is not being done well enough. […], we do not always make the right choices in prioritizing projects, nor in the organizational capacity to support them” (Interview HM E08). | |
|
| ||
| The challenges of extending hospital length of stay and influencing discharge for frail seniors | “We didn’t want to postpone patients’ discharge because the coach couldn’t see them, since she was only there two days a week “. (Interview HM E06). | |
| “[…] medical practice was not negatively influenced by the project, and it was well [perceived]”. (Interview HM E08). | ||
|
| ||
| Selecting and recruiting frail elderly people for the project | “The number of patients seen by the transition coach was below target. So, by broadening the criteria, we were simply supporting the possibility of achieving the original objectives. […], it was done in collaboration with professional practice” (Interview HM E01). | |
| “I sometimes had trouble finding patients for the procedure. Because they are too sick, do they really learn? There are some patients that we couldn’t take […], we had a little too strict criterion» (Interview HM E02). | ||
| “We have a “transition unit” at Montfort Hospital whose targeted clientele resembles the clients the transition coach was targeting. As a result, according to the criteria of inclusion and exclusion, several selected clients end up in the transition unit. So, we were losing several potential candidates. That’s why we had to broaden the criteria” (Interview HM E01). | ||
|
| ||
| Inability to demonstrate the impact of the project on organizational targets | “Unfortunately, with a small N, we have not been able to prove that the intervention of the coach in transition of care has had an impact on the readmission rate of patients in the unit. We didn’t have enough data. The project should have been continued for years to be able to prove that the project had an impact. […] We wanted immediate results that we would have been able to act on. But readmission rates are calculated after the end of the quarter, and then three months later. This delay was too long for a very short project. So that was another big pitfall that we didn’t really have control over.” (Interview HM E10) | |
| “If you can show that with a resource that costs $100,000, we are able to have a much lower readmission rate. We would be able to prove that it is worth hiring a resource and the hospital at that time would make the investment.” (Interview HM E07) | ||
| “Our readmission rate was just Montfort’s, which excludes other hospitals. […], we didn’t have data from the other centres, and it was also very difficult to find out if the patient had been readmitted to another hospital in our area.” (Interview HM E08) | ||
|
| ||
| Difficulties in conducting follow-up in the community | “Afterwards, we realized that post-discharge calls were very difficult. Making a call that lasts maybe 45 minutes or an hour is something that needs to be included in the workload. […], it was not realistic with the nurse’s position now, to ask her to make those calls, it was not manageable. So, we [had to abandon] these calls” (Interview HM E05). | |
|
| ||
| HÔTEL-DIEU DE LÉVIS HOSPITAL | ||
|
| ||
| INITIAL EXPECTATIONS AND GOALS | ||
|
| ||
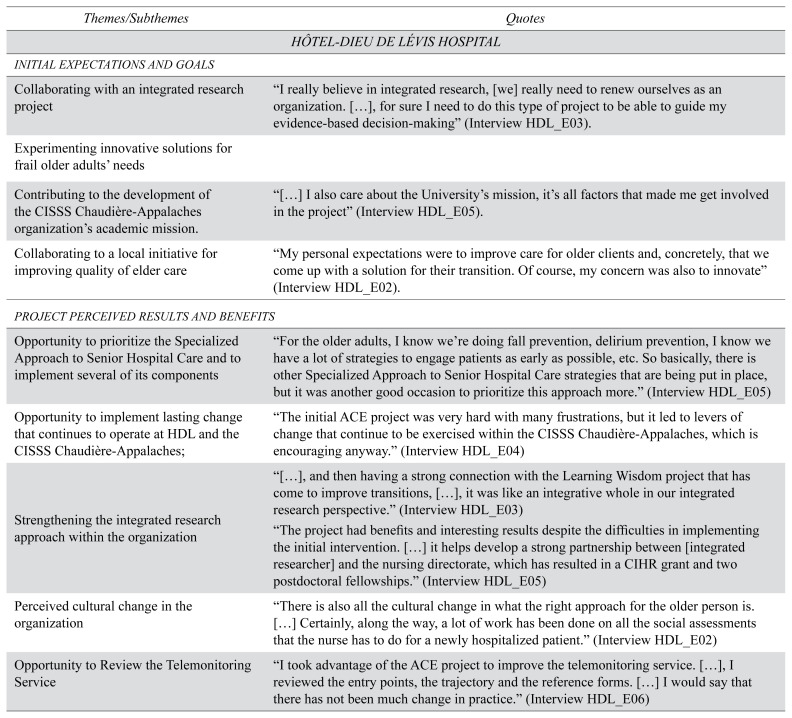
| Collaborating with an integrated research project | “I really believe in integrated research, [we] really need to renew ourselves as an organization. […], for sure I need to do this type of project to be able to guide my evidence-based decision-making” (Interview HDL_E03). | |
|
| ||
| Experimenting innovative solutions for frail older adults’ needs | ||
|
| ||
| Contributing to the development of the CISSS Chaudière-Appalaches organization’s academic mission. | “[…] I also care about the University’s mission, it’s all factors that made me get involved in the project” (Interview HDL_E05). | |
|
| ||
| Collaborating to a local initiative for improving quality of elder care | “My personal expectations were to improve care for older clients and, concretely, that we come up with a solution for their transition. Of course, my concern was also to innovate” (Interview HDL_E02). | |
|
| ||
| PROJECT PERCEIVED RESULTS AND BENEFITS | ||
|
| ||
| Opportunity to prioritize the Specialized Approach to Senior Hospital Care and to implement several of its components | “For the older adults, I know we’re doing fall prevention, delirium prevention, I know we have a lot of strategies to engage patients as early as possible, etc. So basically, there is other Specialized Approach to Senior Hospital Care strategies that are being put in place, but it was another good occasion to prioritize this approach more.” (Interview HDL_E05) | |
|
| ||
| Opportunity to implement lasting change that continues to operate at HDL and the CISSS Chaudière-Appalaches; | “The initial ACE project was very hard with many frustrations, but it led to levers of change that continue to be exercised within the CISSS Chaudière-Appalaches, which is encouraging anyway.” (Interview HDL_E04) | |
|
| ||
| Strengthening the integrated research approach within the organization | “[…], and then having a strong connection with the Learning Wisdom project that has come to improve transitions, […], it was like an integrative whole in our integrated research perspective.” (Interview HDL_E03) | |
| “The project had benefits and interesting results despite the difficulties in implementing the initial intervention. […] it helps develop a strong partnership between [integrated researcher] and the nursing directorate, which has resulted in a CIHR grant and two postdoctoral fellowships.” (Interview HDL_E05) | ||
|
| ||
| Perceived cultural change in the organization | “There is also all the cultural change in what the right approach for the older person is. […] Certainly, along the way, a lot of work has been done on all the social assessments that the nurse has to do for a newly hospitalized patient.” (Interview HDL_E02) | |
|
| ||
| Opportunity to Review the Telemonitoring Service | “I took advantage of the ACE project to improve the telemonitoring service. […], I reviewed the entry points, the trajectory and the reference forms. […] I would say that there has not been much change in practice.” (Interview HDL_E06) | |
|
| ||
| FACILITATORS AND BARRIERS | ||
|
| ||
| Facilitators | ||
|
| ||
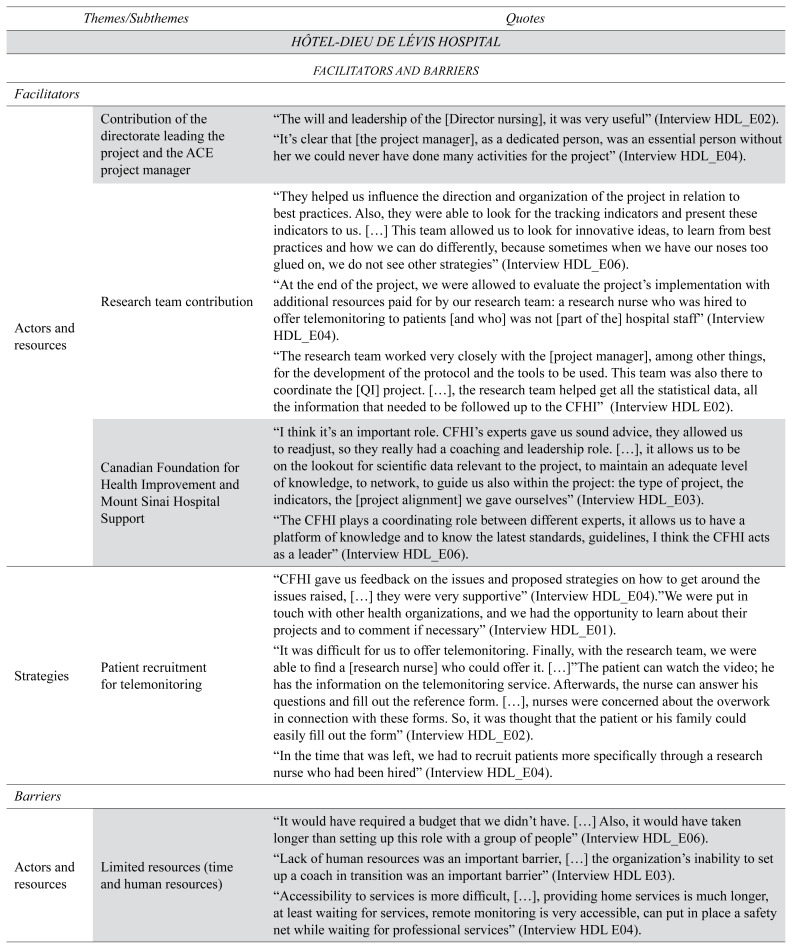
| Actors and resources | Contribution of the directorate leading the project and the ACE project manager | “The will and leadership of the [Director nursing], it was very useful” (Interview HDL_E02). |
| “It’s clear that [the project manager], as a dedicated person, was an essential person without her we could never have done many activities for the project” (Interview HDL_E04). | ||
|
| ||
| Research team contribution | “They helped us influence the direction and organization of the project in relation to best practices. Also, they were able to look for the tracking indicators and present these indicators to us. […] This team allowed us to look for innovative ideas, to learn from best practices and how we can do differently, because sometimes when we have our noses too glued on, we do not see other strategies” (Interview HDL_E06). | |
| “At the end of the project, we were allowed to evaluate the project’s implementation with additional resources paid for by our research team: a research nurse who was hired to offer telemonitoring to patients [and who] was not [part of the] hospital staff” (Interview HDL_E04). | ||
| “The research team worked very closely with the [project manager], among other things, for the development of the protocol and the tools to be used. This team was also there to coordinate the [QI] project. […], the research team helped get all the statistical data, all the information that needed to be followed up to the CFHI” (Interview HDL E02). | ||
|
| ||
| Canadian Foundation for Health Improvement and Mount Sinai Hospital Support | “I think it’s an important role. CFHI’s experts gave us sound advice, they allowed us to readjust, so they really had a coaching and leadership role. […], it allows us to be on the lookout for scientific data relevant to the project, to maintain an adequate level of knowledge, to network, to guide us also within the project: the type of project, the indicators, the [project alignment] we gave ourselves” (Interview HDL_E03). | |
| “The CFHI plays a coordinating role between different experts, it allows us to have a platform of knowledge and to know the latest standards, guidelines, I think the CFHI acts as a leader” (Interview HDL_E06). | ||
|
| ||
| Strategies | Patient recruitment for telemonitoring | “CFHI gave us feedback on the issues and proposed strategies on how to get around the issues raised, […] they were very supportive” (Interview HDL_E04).”We were put in touch with other health organizations, and we had the opportunity to learn about their projects and to comment if necessary” (Interview HDL_E01). |
| “It was difficult for us to offer telemonitoring. Finally, with the research team, we were able to find a [research nurse] who could offer it. […]”The patient can watch the video; he has the information on the telemonitoring service. Afterwards, the nurse can answer his questions and fill out the reference form. […], nurses were concerned about the overwork in connection with these forms. So, it was thought that the patient or his family could easily fill out the form” (Interview HDL_E02). | ||
| “In the time that was left, we had to recruit patients more specifically through a research nurse who had been hired” (Interview HDL_E04). | ||
|
| ||
| Barriers | ||
|
| ||
| Actors and resources | Limited resources (time and human resources) | “It would have required a budget that we didn’t have. […] Also, it would have taken longer than setting up this role with a group of people” (Interview HDL_E06). |
| “Lack of human resources was an important barrier, […] the organization’s inability to set up a coach in transition was an important barrier” (Interview HDL E03). | ||
| “Accessibility to services is more difficult, […], providing home services is much longer, at least waiting for services, remote monitoring is very accessible, can put in place a safety net while waiting for professional services” (Interview HDL E04). | ||
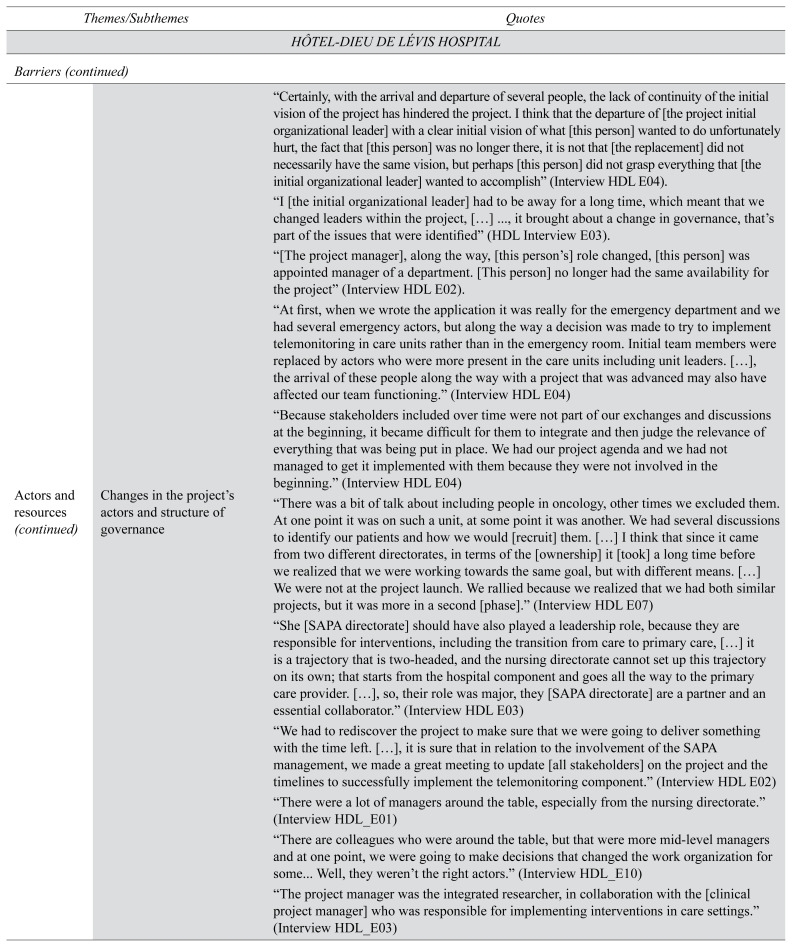
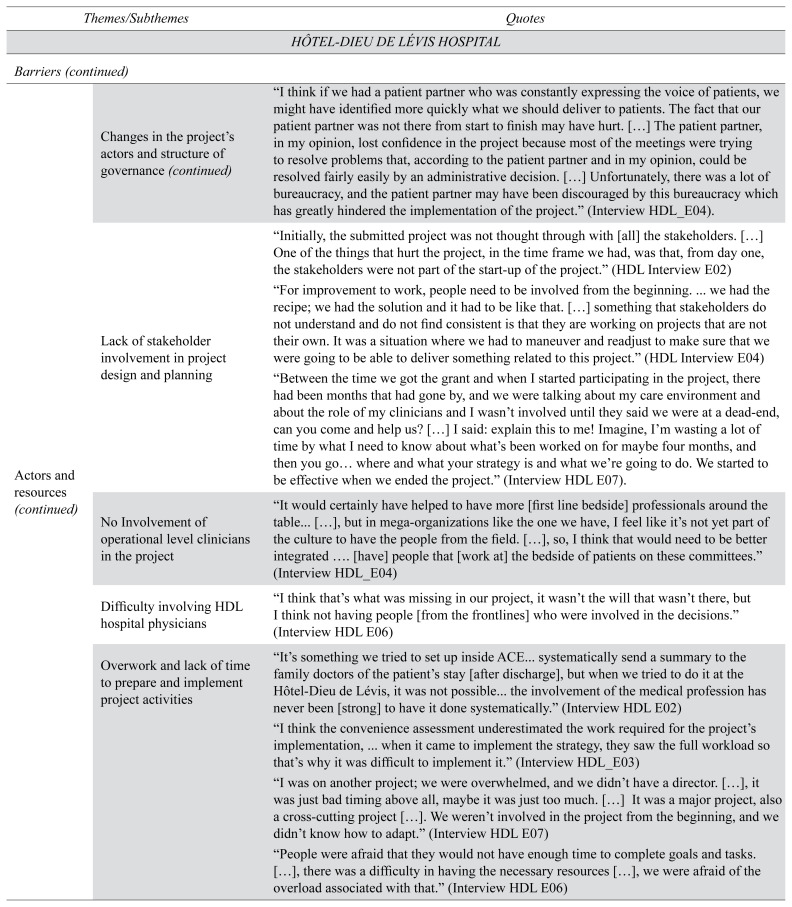
| Changes in the project’s actors and structure of governance | “Certainly, with the arrival and departure of several people, the lack of continuity of the initial vision of the project has hindered the project. I think that the departure of [the project initial organizational leader] with a clear initial vision of what [this person] wanted to do unfortunately hurt, the fact that [this person] was no longer there, it is not that [the replacement] did not necessarily have the same vision, but perhaps [this person] did not grasp everything that [the initial organizational leader] wanted to accomplish” (Interview HDL E04). | |
| “I [the initial organizational leader] had to be away for a long time, which meant that we changed leaders within the project, […] ..., it brought about a change in governance, that’s part of the issues that were identified” (HDL Interview E03). | ||
| “[The project manager], along the way, [this person’s] role changed, [this person] was appointed manager of a department. [This person] no longer had the same availability for the project” (Interview HDL E02). | ||
| “At first, when we wrote the application it was really for the emergency department and we had several emergency actors, but along the way a decision was made to try to implement telemonitoring in care units rather than in the emergency room. Initial team members were replaced by actors who were more present in the care units including unit leaders. […], the arrival of these people along the way with a project that was advanced may also have affected our team functioning.” (Interview HDL E04) | ||
| “Because stakeholders included over time were not part of our exchanges and discussions at the beginning, it became difficult for them to integrate and then judge the relevance of everything that was being put in place. We had our project agenda and we had not managed to get it implemented with them because they were not involved in the beginning.” (Interview HDL E04) | ||
| “There was a bit of talk about including people in oncology, other times we excluded them. At one point it was on such a unit, at some point it was another. We had several discussions to identify our patients and how we would [recruit] them. […] I think that since it came from two different directorates, in terms of the [ownership] it [took] a long time before we realized that we were working towards the same goal, but with different means. […] We were not at the project launch. We rallied because we realized that we had both similar projects, but it was more in a second [phase].” (Interview HDL E07) | ||
| “She [SAPA directorate] should have also played a leadership role, because they are responsible for interventions, including the transition from care to primary care, […] it is a trajectory that is two-headed, and the nursing directorate cannot set up this trajectory on its own; that starts from the hospital component and goes all the way to the primary care provider. […], so, their role was major, they [SAPA directorate] are a partner and an essential collaborator.” (Interview HDL E03) | ||
| “We had to rediscover the project to make sure that we were going to deliver something with the time left. […], it is sure that in relation to the involvement of the SAPA management, we made a great meeting to update [all stakeholders] on the project and the timelines to successfully implement the telemonitoring component.” (Interview HDL E02) | ||
| “There were a lot of managers around the table, especially from the nursing directorate.” (Interview HDL_E01) | ||
| “There are colleagues who were around the table, but that were more mid-level managers and at one point, we were going to make decisions that changed the work organization for some... Well, they weren’t the right actors.” (Interview HDL_E10) | ||
| “The project manager was the integrated researcher, in collaboration with the [clinical project manager] who was responsible for implementing interventions in care settings.” (Interview HDL_E03) | ||
| “I think if we had a patient partner who was constantly expressing the voice of patients, we might have identified more quickly what we should deliver to patients. The fact that our patient partner was not there from start to finish may have hurt. […] The patient partner, in my opinion, lost confidence in the project because most of the meetings were trying to resolve problems that, according to the patient partner and in my opinion, could be resolved fairly easily by an administrative decision. […] Unfortunately, there was a lot of bureaucracy, and the patient partner may have been discouraged by this bureaucracy which has greatly hindered the implementation of the project.” (Interview HDL_E04). | ||
|
| ||
| Lack of stakeholder involvement in project design and planning | “Initially, the submitted project was not thought through with [all] the stakeholders. […] One of the things that hurt the project, in the time frame we had, was that, from day one, the stakeholders were not part of the start-up of the project.” (HDL Interview E02) | |
| “For improvement to work, people need to be involved from the beginning. … we had the recipe; we had the solution and it had to be like that. […] something that stakeholders do not understand and do not find consistent is that they are working on projects that are not their own. It was a situation where we had to maneuver and readjust to make sure that we were going to be able to deliver something related to this project.” (HDL Interview E04) | ||
| “Between the time we got the grant and when I started participating in the project, there had been months that had gone by, and we were talking about my care environment and about the role of my clinicians and I wasn’t involved until they said we were at a dead-end, can you come and help us? […] I said: explain this to me! Imagine, I’m wasting a lot of time by what I need to know about what’s been worked on for maybe four months, and then you go… where and what your strategy is and what we’re going to do. We started to be effective when we ended the project.” (Interview HDL E07). | ||
|
| ||
| No Involvement of operational level clinicians in the project | “It would certainly have helped to have more [first line bedside] professionals around the table... […], but in mega-organizations like the one we have, I feel like it’s not yet part of the culture to have the people from the field. […], so, I think that would need to be better integrated …. [have] people that [work at] the bedside of patients on these committees.” (Interview HDL_E04) | |
|
| ||
| Difficulty involving HDL hospital physicians | “I think that’s what was missing in our project, it wasn’t the will that wasn’t there, but I think not having people [from the frontlines] who were involved in the decisions.” (Interview HDL E06) | |
|
| ||
| Overwork and lack of time to prepare and implement project activities | “It’s something we tried to set up inside ACE... systematically send a summary to the family doctors of the patient’s stay [after discharge], but when we tried to do it at the Hôtel-Dieu de Lévis, it was not possible... the involvement of the medical profession has never been [strong] to have it done systematically.” (Interview HDL E02) | |
| “I think the convenience assessment underestimated the work required for the project’s implementation, … when it came to implement the strategy, they saw the full workload so that’s why it was difficult to implement it.” (Interview HDL_E03) | ||
| “I was on another project; we were overwhelmed, and we didn’t have a director. […], it was just bad timing above all, maybe it was just too much. […] It was a major project, also a cross-cutting project […]. We weren’t involved in the project from the beginning, and we didn’t know how to adapt.” (Interview HDL E07) | ||
| “People were afraid that they would not have enough time to complete goals and tasks. […], there was a difficulty in having the necessary resources […], we were afraid of the overload associated with that.” (Interview HDL E06) | ||
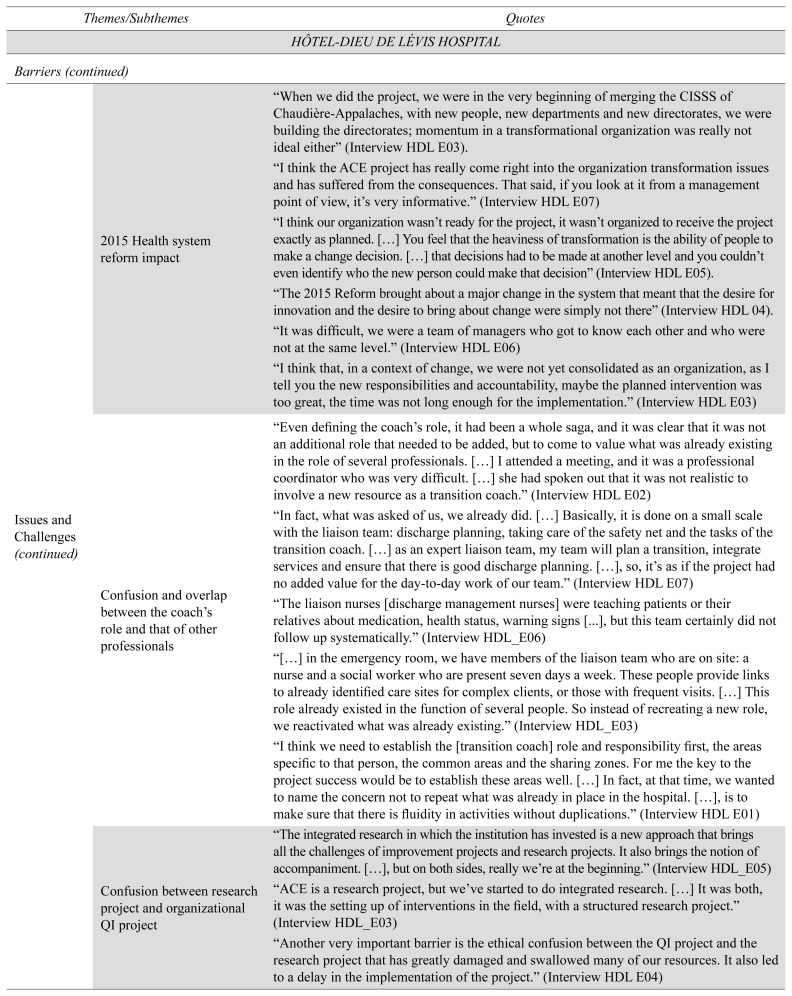
| Issues and Challenges | 2015 Health system reform impact | “When we did the project, we were in the very beginning of merging the CISSS of Chaudière-Appalaches, with new people, new departments and new directorates, we were building the directorates; momentum in a transformational organization was really not ideal either” (Interview HDL E03). |
| “I think the ACE project has really come right into the organization transformation issues and has suffered from the consequences. That said, if you look at it from a management point of view, it’s very informative.” (Interview HDL E07) | ||
| “I think our organization wasn’t ready for the project, it wasn’t organized to receive the project exactly as planned. […] You feel that the heaviness of transformation is the ability of people to make a change decision. […] that decisions had to be made at another level and you couldn’t even identify who the new person could make that decision” (Interview HDL E05). | ||
| “The 2015 Reform brought about a major change in the system that meant that the desire for innovation and the desire to bring about change were simply not there” (Interview HDL 04). | ||
| “It was difficult, we were a team of managers who got to know each other and who were not at the same level.” (Interview HDL E06) | ||
| “I think that, in a context of change, we were not yet consolidated as an organization, as I tell you the new responsibilities and accountability, maybe the planned intervention was too great, the time was not long enough for the implementation.” (Interview HDL E03) | ||
|
| ||
| Confusion and overlap between the coach’s role and that of other professionals | “Even defining the coach’s role, it had been a whole saga, and it was clear that it was not an additional role that needed to be added, but to come to value what was already existing in the role of several professionals. […] I attended a meeting, and it was a professional coordinator who was very difficult. […] she had spoken out that it was not realistic to involve a new resource as a transition coach.” (Interview HDL E02) | |
| “In fact, what was asked of us, we already did. […] Basically, it is done on a small scale with the liaison team: discharge planning, taking care of the safety net and the tasks of the transition coach. […] as an expert liaison team, my team will plan a transition, integrate services and ensure that there is good discharge planning. […], so, it’s as if the project had no added value for the day-to-day work of our team.” (Interview HDL E07) | ||
| “The liaison nurses [discharge management nurses] were teaching patients or their relatives about medication, health status, warning signs [...], but this team certainly did not follow up systematically.” (Interview HDL_E06) | ||
| “[…] in the emergency room, we have members of the liaison team who are on site: a nurse and a social worker who are present seven days a week. These people provide links to already identified care sites for complex clients, or those with frequent visits. […] This role already existed in the function of several people. So instead of recreating a new role, we reactivated what was already existing.” (Interview HDL_E03) | ||
| “I think we need to establish the [transition coach] role and responsibility first, the areas specific to that person, the common areas and the sharing zones. For me the key to the project success would be to establish these areas well. […] In fact, at that time, we wanted to name the concern not to repeat what was already in place in the hospital. […], is to make sure that there is fluidity in activities without duplications.” (Interview HDL E01) | ||
|
| ||
| Confusion between research project and organizational QI project | “The integrated research in which the institution has invested is a new approach that brings all the challenges of improvement projects and research projects. It also brings the notion of accompaniment. […], but on both sides, really we’re at the beginning.” (Interview HDL_E05) | |
| “ACE is a research project, but we’ve started to do integrated research. […] It was both, it was the setting up of interventions in the field, with a structured research project.” (Interview HDL_E03) | ||
| “Another very important barrier is the ethical confusion between the QI project and the research project that has greatly damaged and swallowed many of our resources. It also led to a delay in the implementation of the project.” (Interview HDL E04) | ||
|
| ||
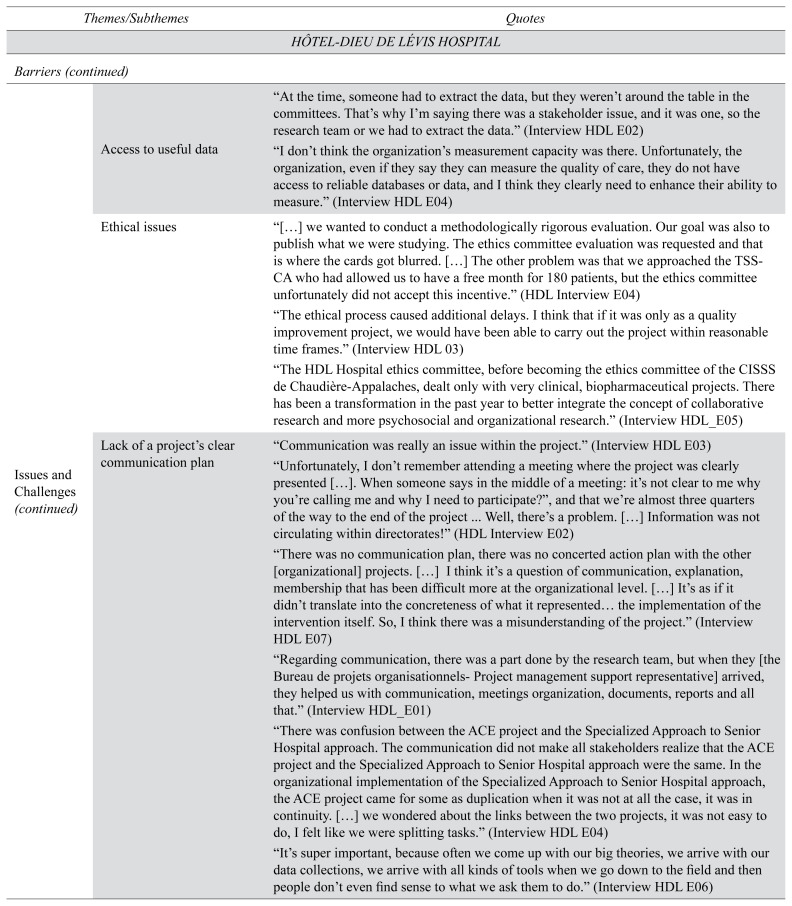
| Access to useful data | “At the time, someone had to extract the data, but they weren’t around the table in the committees. That’s why I’m saying there was a stakeholder issue, and it was one, so the research team or we had to extract the data.” (Interview HDL E02) | |
| “I don’t think the organization’s measurement capacity was there. Unfortunately, the organization, even if they say they can measure the quality of care, they do not have access to reliable databases or data, and I think they clearly need to enhance their ability to measure.” (Interview HDL E04) | ||
|
| ||
| Ethical issues | “[…] we wanted to conduct a methodologically rigorous evaluation. Our goal was also to publish what we were studying. The ethics committee evaluation was requested and that is where the cards got blurred. […] The other problem was that we approached the TSS-CA who had allowed us to have a free month for 180 patients, but the ethics committee unfortunately did not accept this incentive.” (HDL Interview E04) | |
| “The ethical process caused additional delays. I think that if it was only as a quality improvement project, we would have been able to carry out the project within reasonable time frames.” (Interview HDL 03) | ||
| “The HDL Hospital ethics committee, before becoming the ethics committee of the CISSS de Chaudière-Appalaches, dealt only with very clinical, biopharmaceutical projects. There has been a transformation in the past year to better integrate the concept of collaborative research and more psychosocial and organizational research.” (Interview HDL_E05) | ||
|
| ||
| Lack of a project’s clear communication plan | “Communication was really an issue within the project.” (Interview HDL E03) | |
| “Unfortunately, I don’t remember attending a meeting where the project was clearly presented […]. When someone says in the middle of a meeting: it’s not clear to me why you’re calling me and why I need to participate?”, and that we’re almost three quarters of the way to the end of the project … Well, there’s a problem. […] Information was not circulating within directorates!” (HDL Interview E02) | ||
| “There was no communication plan, there was no concerted action plan with the other [organizational] projects. […] I think it’s a question of communication, explanation, membership that has been difficult more at the organizational level. […] It’s as if it didn’t translate into the concreteness of what it represented… the implementation of the intervention itself. So, I think there was a misunderstanding of the project.” (Interview HDL E07) | ||
| “Regarding communication, there was a part done by the research team, but when they [the Bureau de projets organisationnels-Project management support representative] arrived, they helped us with communication, meetings organization, documents, reports and all that.” (Interview HDL_E01) | ||
| “There was confusion between the ACE project and the Specialized Approach to Senior Hospital approach. The communication did not make all stakeholders realize that the ACE project and the Specialized Approach to Senior Hospital approach were the same. In the organizational implementation of the Specialized Approach to Senior Hospital approach, the ACE project came for some as duplication when it was not at all the case, it was in continuity. […] we wondered about the links between the two projects, it was not easy to do, I felt like we were splitting tasks.” (Interview HDL E04) | ||
| “It’s super important, because often we come up with our big theories, we arrive with our data collections, we arrive with all kinds of tools when we go down to the field and then people don’t even find sense to what we ask them to do.” (Interview HDL E06) | ||
| An emphasis on planning instead of implementation | “It’s multifactorial obviously, but maybe having clear, precise mandates, with specific timelines, and with the establishment of very specific roles and responsibilities for the actors. And perhaps target the necessary actors, the actors who would be most relevant by their role, their function, etc.” (Interview HDL E01) | |
| “On project planning; I want to say that there would have been place for improvement, it was more at the “now that I’ve heard, now that I’ve consulted, I do what with it and I use it in what way?” (Interview HDL E07) | ||
| “We wanted to set up a project that was too perfect to start with. However, it is important to start somewhere with small steps that are easy to implement, measure and study changes, and act: do simple and fast PDSA cycles, evaluate and move forward!” (Interview HDL E04) | ||
|
| ||
| Lack of project planning | “I think we should have had a more operational committee to help us implement the strategy […], people are more there, and we talk more in the how with the teams. […] Of course, it’s important to have the leaders be able to make policy decisions, but the operational part should have really been there.” (Interview HDL E03) | |
| “There were a department head who was in the project, but [the person] didn’t understand that [the person] had to make the connection with the director, and I realized after a few weeks, a few months, that the director was not aware of the project, so I don’t know if the role of the people who were on the committee was clear to them and their responsibility and accountability within the project.” (HDL Interview E05) | ||
|
| ||
| Competition with other projects | “Since there were several projects simultaneously running in the CISSS surrounding the Specialized Approach to Senior Hospital approach, confusion also developed, namely what was one project versus another.” (HDL Interview E02) | |
| “We all had a common goal, but sometimes it lacked a bit of clarity. We often gathered the same actors around the different tables for each of the “pieces”, I would say different projects. […] I find that there was a lot of confusion between our project and the ACE project, although everyone agreed on the objective.” (Interview HDL E07) | ||
|
| ||
| Attempting to Implement Telemonitoring as a “Complex” Technological Innovation | “It had several organizational barriers … we thought that remote monitoring would be easy to install, finally it was not so easy. […] …for telemonitoring reference, who was going to do the screening? Who will show, discuss and present this service to patients? After that, who’s going to make the reference? There were really a lot of questions as people thought it still took time to present and offer the service.” (HDL Interview E06) | |
|
| ||
| Telemonitoring service cost | “Unfortunately, most of the patients who were offered telemonitoring refused it because it cost [money]. There were several reasons in fact that the research nurse documented. […] 3 out of 29 patients who were approached finally accepted it, so a large refusal rate.” (Interview HDL E04) | |
|
| ||
| Google Site’s knowledge-sharing platform security issues | “Even just wanting to use a new platform to improve communication was difficult. […] because there were a lot of technological barriers to sharing and access to the platform that was blocked by the hospital firewall that prevented people from having access to the platform. […] It was necessary to bring in the Information Technology (IT) Department to see how to develop the tool.” (Interview HDL E04) | |
ACE = Acute Care for Elders; CCAC = Community Care Access Centre; CFHI = Canadian Foundation for Healthcare Improvement; CFN = Canadian Frailty Network; CISSS = Centre Intégré de Santé et de services sociaux; PDSA = Plan, Do, Study, Act; SASHA = Specialized Approach to Senior Hospital (Quebec).