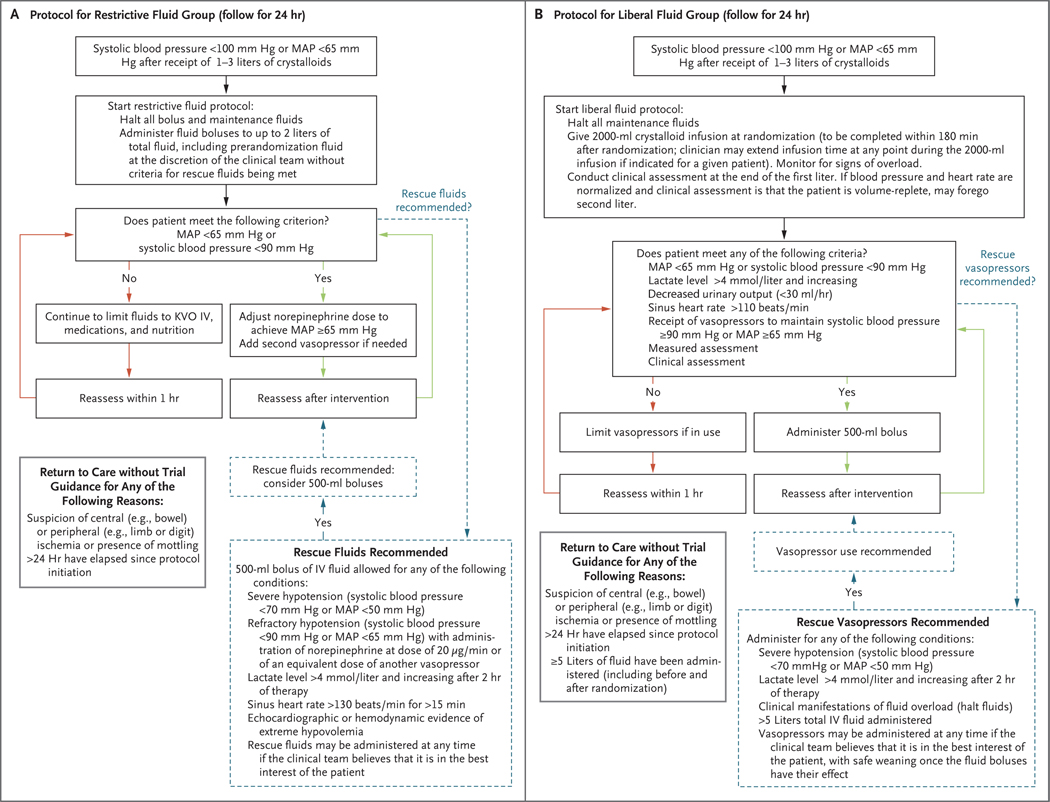
Figure 1. Fluid and Vasopressor Administration Protocols in the Restrictive Fluid Group and the Liberal Fluid Group.
Panel A shows the instructions for intravenous (IV) fluid and vasopressor administration in the restrictive fluid group, and Panel B the instructions in the liberal fluid group. In both trial groups, all protocol assessments, such as frequency of vital-sign monitoring, lactic acid measurements, and echocardiographic interventions, were performed at the discretion of the clinical team. The restrictive fluid protocol suggested norepinephrine as the primary vasopressor and epinephrine as a second vasopressor; neither was required. The restrictive fluid protocol defined “echocardiographic or hemodynamic evidence of extreme hypovolemia” as a maximal diameter of the inferior vena cava (IVC) of less than 5 mm, an empty left ventricle on echocardiography (e.g. left ventricular end diastolic area index, <5.5 cm2 per square meter of body-surface area), or stroke-volume increase of more than 30% in response to a passive leg raise, fluid challenge, or positive-pressure breaths. KVO denotes keep vein open, and MAP mean arterial pressure. The liberal fluid protocol instructed that patients receiving vasopressors should have the dose adjusted down or vasopressors discontinued, as feasible. The protocol included an instruction that care team members could use any available “measured assessment” they chose (e.g. echocardiography, IVC measurement, or central venous pressure measurement) or any type of “clinical assessment” of volume status to trigger use of additional fluids. If a patient had manifestations of fluid overload, fluids were to be halted. The liberal fluid protocol also expressly permitted the use of vasopressors after the administration of 5 liters of total fluid.